Abstract
Background
Total joint arthroplasty (TJA) registries traditionally have focused on implant longevity and rates of revision surgery. Registries would benefit from the addition of standardized patient-reported outcomes (PROs) such as pain relief and improved physical function. However, PROs have not been routinely adopted, and their incorporation into TJA registries presents challenges.
Questions/purposes
We review current PRO use by existing national registries, challenges to integrating PROs in national registries, lessons from national registries that have integrated PROs, and suggestions to guide future adoption of PROs.
Methods
We conducted a literature search of papers addressing PRO use in national knee and hip arthroplasty registries, resulting in 15 articles. These publications were supplemented by discussions with thought leaders from international registries.
Where Are We Now?
Some national TJA registries are collecting PROs and valuable research is emerging. However, challenges exist, such as selecting suitable PROs, selection bias in countries without government-mandated participation for all hospitals, and challenges with missing data.
Where Do We Need to Go?
The ideal system will incorporate PROs into TJA registries. In so doing, it will be important to choose suitable PROs and develop innovative methods to collect PROs to ensure complete data and sustainability.
How Do We Get There?
New methods are required to meet the challenges related to registry design, logistics of PRO collection, and registry cost and sustainability. Modifications to the traditional hospital- and implant-centric design and new procedures to collect complete data from both patients and clinicians may be necessary. For instance, England and Wales, New Zealand, and Sweden developed methods to collect PROs after TJA directly from patients and a US TJA registry collects PROs as the primary outcome. Finally, to assure long-term sustainability, PRO data must be valuable to multiple stakeholders, including patients, clinicians, researchers, and policy makers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total joint arthroplasty (TJA) provides pain relief and improves physical function for many patients with advanced arthritis whose symptoms failed to improve using nonsurgical interventions. In the United States, approximately one million patients had a knee or hip replaced in 2009 [4]. With the number of TJAs and associated costs growing annually, a new emphasis on improving the “value” of TJA has emerged. To achieve this goal, surgeons must continue to improve functional and pain-related outcomes after TJA, while reducing the numbers of postoperative complications and poor clinical results.
Traditional TJA registries monitor the frequency of revision surgery and define success based on a low number of revisions. Such an approach has its limitations, as revision-oriented registries cannot determine whether unrevised implants are functioning well or poorly or whether the patient achieved satisfactory pain relief and functional gain. This limitation is underscored by the recent recall of metal-on-metal hip implants where significant numbers of patients experienced unusual pain due to soft tissue pathology associated with the metal ions [14, 18]. On the other hand, patient-reported outcomes (PROs) that measure pain relief and improved function could be an important addition to a registry by quantifying optimal outcomes from TJA procedures as defined by the patient. PROs also capture presence of persistent pain and unsatisfactory functional gains in patients who fail to achieve the desired outcome. Some of the international TJA registries now incorporate PROs that emphasize the patient’s perception of pain and physical function [20], and recent evidence-based research has called attention to the value of incorporating PROs in national joint registries [19].
The addition of PROs to TJA registries introduces challenges related to the registry design, logistics of PRO collection, cost, and sustainability. Each of these challenges necessitates modifications to the traditional hospital- and implant-centric design of many registries. Beyond these issues that affect all registries, the United States faces unique barriers due to the sheer volume of annual TJA procedures, the lack of a single national payer to capture all procedures, and stringent privacy regulations that constrain secondary uses of patient health information.
In this paper, we review the current use of PROs by national registries, the challenges to integrating PROs in national implant registries, and lessons from the subset of national registries that have integrated PROs. Future opportunities to systematically collect PROs in TJA registries to quantify both patient- and implant-centric outcomes will be discussed.
Where Are We Now?
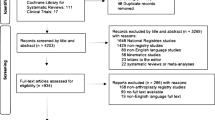
To assess the current use of PROs in TJA registries, we searched PubMed for the terms “joint registry and patient reported outcome”; 132 articles were identified. An additional, similar search was conducted in Google Scholar. Only the papers addressing the use of PROs in a national knee and hip arthroplasty registry were reviewed in detail, resulting in the review of 15 articles (Appendix 1; supplemental materials are available with the online version of CORR®). These publications, as well as presentations and discussions with thought leaders from international registries, form the basis for this review.
The New Zealand registry was an early adopter of postoperative PROs for hip and knee procedures, beginning at its inception in 1998. Other long-standing European implant registries have more recently added PRO measurement: the Swedish hip registry in 2002, the England and Wales registry in 2009, and the Norwegian hip fracture registry in 2005 [20]. In the United States, the Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement (FORCE-TJR), which was funded in 2010 and represents a national sample of 121 diverse orthopaedic surgeons in 22 states performing TJA [8], is collecting PROs before and after surgery on 100% of participants.
Traditional TJA registries were designed to collect data useful to monitoring implant survival and failure, defined by revision rates. National registries typically attempt to enroll 100% of patients from all hospitals to assure complete capture of data at the time of surgery and data from subsequent revision surgeries. The dates of both the initial surgery and revision are necessary to quantify the time to revision and failure rate. In this model, national registries incorporate large numbers of surgeries to identify relatively low annual failure rates. For example, New Zealand reports post-TKA implant failure rates of approximately 0.5%/year in the first 12 years [16].
In contrast to failure rates that concern a minority of patients, pain relief and improved physical function are relevant to all patients. A recent review of the use of PROs in registries concluded: “omitting patient-reported outcomes precludes us [surgeons] from having a full understanding of the factors that contribute to pain relief, restoration of function, and patient satisfaction” [20].
The Value of PROs
The PROs collected by a subset of TJA registries are contributing new information, spurring growing interest in the value of incorporating PROs in TJA registries. Beyond clinical care, PROs are increasingly used in the allocation of healthcare resources and comparative effectiveness research. Beginning in April 2009, the UK Department of Health mandated collection of generic and condition-specific PROs from patients before and after four surgical procedures, including TKA and THA [6]. Goodfellow et al. [10] analyzed data from the New Zealand Joint Registry to compare the effectiveness of TKA and unicompartmental knee arthroplasty (UKA) and found that PROs were a more sensitive outcome than revision. Thus, PROs may be useful as a measure of positive outcomes (such as pain relief and improved function) and as a marker of risk for negative outcomes (such as persistent pain or higher risk for implant failure).
Challenges of Selecting Suitable PROs
One of the challenges in selecting suitable PROs comes from the lack of consensus as to the ideal PRO measure(s) to include. The UK required both global health status and condition-specific outcomes for each of four surgical procedures [6]. Generic measures are required to compare across surgical procedures, while condition-specific data are useful for evaluating outcomes associated with varied techniques within a single procedure. The UK and Sweden also emphasize collecting pre- and postoperative data so that individual change can be detected. In contrast, New Zealand mandates postoperative PROs. In the United States, FORCE-TJR selected joint-specific function and pain surveys that allow knee or hip pain relief to be quantified independent of functional gains. For example, the WOMAC [3] and Hip Disability and Osteoarthritis Outcome Score (HOOS)/Knee Injury and Osteoarthritis Outcome Score (KOOS) [5] provide subscores for joint pain, stiffness, activities of daily living, and function. Other joint-specific PROs such as the Oxford are shorter, but its items integrate both pain and function domains and separate scores are not calculated [5]. While global function surveys such as the SF-36 [23] and EQ-5D™ [7] enable measurement of general health and well-being and facilitate outcome comparisons with other medical and surgical interventions, they are unable to attribute specific postoperative health changes to the TJA procedure or other health interventions.
Assuring Representative and Complete Data
Another challenge faced by registries is that most collect data at the hospital operating room at the time the patient undergoes the TJA procedure. This process has proven effective in countries with national health insurance or government mandates for all hospitals to participate in the TJA registry but inadequate in countries lacking these attributes. In the United States in particular, if a patient chooses a different surgeon or hospital for postoperative care due to dissatisfaction or a change of residence, followup information (eg, key postoperative events such as revision or infection) will be missed. Similarly, in the case of US registries based on a single insurance plan, valuable followup data elements will be lost if the patient changes to a different insurance plan. The missing data from these analyses are not random and may result in underreporting of implant failures. Finally, US registries relying on the Medicare beneficiary files would not be representative of the current US TJA population as almost 45% of current patients are younger than 65 years, introducing an age bias to the outcome measurement. Such challenges in the United States and other countries without a centralized healthcare system must be met with creativity in registry design to avoid systematic bias. Of note, these concerns apply to both the collection of implant survival data and the addition of PROs.
Where Do We Need to Go?
The ideal system by which PROs are incorporated into TJA registries involves choosing suitable PROs and developing innovative methods to collect PROs to ensure complete data and sustainability. Finally, registries must address the technical challenges of extracting data from electronic health records, as possible, to enhance sustainability and outcome measurement.
Broadening Registry Data to Include PROs
Data on relative implant longevity and implant revision rates will always be important clinical information; however, as implant designs, materials mature, and survival times lengthen, patient factors, such as younger age at time of surgery, greater BMI, and greater demands on the joint, are emerging as key factors in predicting implant survivorship among the growing total population of patients with TJA. In addition, existing outcome research on TKA and THA have demonstrated variation in functional outcome after surgery correlated to patient attributes such as greater BMI, older age, female sex, poorer emotional health, and higher number of medical and musculoskeletal comorbidities [9, 15, 17]. Other risk factors for suboptimal postoperative function include poorer self-care skills and self-efficacy [1, 22]. Thus, these patient attributes, as well as PROs related to pain relief and functional gains, will be important to future TJA registry design.
Collecting Electronic PRO and Clinical Data
To minimize patient burden and to assure PRO sustainability, brief, electronic, computer-adapted PRO measures may be preferable. Ongoing research, such as the Patient-reported Outcomes Measurement Information System, PROMIS® initiative in the United States, will refine computerized adaptive testing (CAT) outcome measures. PROMIS® was funded by the NIH to define valid, reliable, consistent measures to be used in research and delivered through a variety of methods, including CAT. CAT measures are web-accessible, to deliver surveys in surgeon offices and at patient homes, incorporate independent pain and function measures and minimize patient response burden by tailoring questions to individual responses. Further psychometric research is needed to define summary scores specific to TJA, to determine outcome norms for patients with TJA at specific time intervals after TJA, and to map these new scores to legacy measures currently in use. When these research goals are met, electronic, CAT PROs may greatly improve the ease and sustainability of PRO administration by TJA registries.
Because TJA requires a hospital stay, the key preoperative patient risk factors and postoperative adverse events and PRO data may be best captured in the surgeons’ office records. With the adoption of electronic health records, the possibility for registries to extract key clinical factors electronically may support expanding the scope of registry data. However, current electronic health records support clinician data entry and rarely include capture of patient-entered data, such as PROs. In the future, surgeon office electronic health records may be an optimal source of clinical data and electronic health record software may be modified to capture PROs. With these modifications, registries will benefit by systematic office-based data capture. In addition, direct-to-patient collection of PROs will be supported by web-based software and use of mobile phones and other technology. The integration of electronic data across time will assure complete longitudinal followup data.
Assuring Representative and Complete Data
The International Society of Arthroplasty Registries defines a full member registry as one that captures more than 90% of all cases and clinically validates the data [13]. This standard supports stable measures of low prevalent events such as revision or infection. As discussed previously, the 100% enrollment model is more feasible in a country with a single payer and a moderate volume of surgeries. In contrast to countries performing 10,000 to 20,000 annual procedures, the Unites States performs more than one million TJA procedures each year and no all-payer database exists to define the total population of patients with TJA. Capturing more than 90% of all US patients is a daunting task. In this situation, the registry must follow the patient over time to assure complete longitudinal outcomes independent of site, insurance, or provider. The challenges to followup of US patients with TJA has been highlighted by Greenbaum et al. [11] in a study conducted at a major referral center, in which 65% of confirmed post-THA complications were from hospitals other than the site of the original surgery. In summary, to assure complete followup data, new methods to monitor all TJA care over time must follow the individual patient to diverse hospitals, surgeons, and geographic regions.
Sustainability
Before dedicating efforts to redesign registries to incorporate PROs, TJA registry leaders must be confident that representative PRO collection can be sustained, and that the data will enhance the knowledge obtained from the registry and benefit multiple stakeholders, including patients and surgeons. For instance, integration of implant registry data with comprehensive clinical data from medical records can generate tailored outcome analyses for diverse patient subgroups with varied clinical profiles at the time of surgery, as illustrated in recent analysis from the UK registry data [2].
To assure sustainability, PRO data must be valuable to multiple stakeholders to justify the incremental costs of their collection. For instance, patient-centric outcomes are valuable to public health leaders and policy makers when the “value” of TJA is defined in relation to healthcare costs. The Institute of Medicine calls for patient-centered care where the patients’ preferences and values are included in healthcare decisions [12]. PROs are one method for including the patient’s voice in assessing TJA outcomes. At the clinical level, surgeons and hospitals can use summary PRO data to monitor postdischarge outcomes (including quality of care as measured by pain relief and functional gain or unexpected postdischarge adverse events) and to identify subgroups of patients with persistent pain who may be at risk for future implant failure. Comparative effectiveness research based on PROs and comprehensive TJA outcome data are valuable to guiding the orthopaedic community to define best practices. Finally, postmarketing surveillance based on registry PROs and implant data is valuable to regulatory agencies and orthopaedic implant manufacturers. In summary, while the addition of PROs to a TJA registry is time-consuming, if stakeholders value and use the data, the PROs will gain broader use and dissemination.
How Do We Get There?
Selecting Suitable PROs
To date, the orthopaedic community has not defined a national or international standard for optimal measure of PROs after TJA. However, general PRO preferences can be identified from early PRO users. Many TJA registries, such as the UK registry and FORCE-TJR, include both general health status measures (eg, EQ-5D™, SF-36) and joint-specific measures (eg, Oxford, HOOS/KOOS). General health measures assure that TJA outcomes can be compared to other healthcare interventions while changes in joint-specific measures are more easily attributable to the TJA procedure. The second decision is whether to include independent measures of pain relief and functional gain. Sweden uses both a VAS pain score and a brief functional assessment, and FORCE-TJR uses the pain and function subscores of the HOOS/KOOS. In contrast, the UK and New Zealand selected a measure that, while quicker to complete, integrates the two outcomes. Research demonstrates, while almost all patients receive pain relief after TJA, functional gain varies widely and is related to nonsurgical factors [9]. Thus, surgeons may prefer PROs that can discriminate the two outcomes of pain and function.
Assuring Representative and Complete Data
New methods are emerging to address some of the challenges of collecting consistent and complete longitudinal data after TJA. For instance, England and Wales, New Zealand, and Sweden have developed methods to collect PROs directly from patients at specific intervals after TJA. In addition, FORCE-TJR developed a unique registry design to collect PROs as the primary registry outcome directly from patients across settings [8]. Direct-to-patient PRO collection is not dependent on surgeon office visits. Because surgeon office visits can vary in timing, depending on clinical need and surgeon preference, direct-to-patient PRO administration allows annual assessments that do not require the patient to visit the surgeon’s office. Additional benefits include minimizing the burden on office staff and assuring consistent measurement intervals. Lessons learned from these direct-to-patient models will guide future registry adoption of PROs.
Other design modifications to assure complete PRO capture include patient consent-based enrollment at the time TJA surgery is scheduled, well in advance of the surgery date. The FORCE-TJR design assures time to collect preoperative PROs and minimizes surgeon burden. To that effect, office systems and patient consent procedures are simplified and supported by a telephone-based registry coordinator. Followups are centralized and patients receive reminders and postoperative PRO surveys by mail or email at prearranged times. In addition to PROs on pain and functional status, patients report any post-TJA events that required surgical or medical treatment. Events that occur at settings other than that of the initial procedure are captured and medical records are reviewed to verify diagnoses and procedures. In aggregate, these PRO collection methods assure complete patient followup independent of surgeon, hospital, patient geography, timing, or insurer.
A challenge with the collection of PROs is the variation in survey completion rates, which requires focused efforts to manage consistent patient response. To engage patients over time, the FORCE-TJR registry adapted principles from the US Women’s Health Initiative [24] because this national cohort study successfully followed more than 90% of patients for 10 years. This high level of ongoing participation is important to assure credible conclusions and can only be achieved by actively engaging the patient as partner in the registry efforts. From the start, the patient is engaged as partner during the consent process. If the patient fails to return the PRO, a FORCE-TJR registry coordinator contacts the patient directly to encourage participation. Patients have convenient options for PRO completion, such as email/password-protected simple web surveys with “save and complete later” options or scannable paper surveys available in multiple languages (eg, English/Spanish). This patient-focused protocol can be adapted in countries where 100% of patients receive the survey. For instance, the region or hospital could manage the process to assure adequate data are obtained to be able to quantify and compare PROs across settings.
In a country with such a large number of annual procedures as the United States, the 100% enrollment model might be difficult to achieve. FORCE-TJR is instead using a representative sample of surgeons and patients across the country. The potential of a selection bias at enrollment is minimized by inviting sites from a random sample of orthopaedic practices with attention to diverse settings (ie, size, payers, hospital, geographic location). For example, a country with a 100% implant tracking system could choose to adopt PROs for a representative subset of its patients to focus resources on complete data, but on fewer patients.
Demonstrate Value of Long-term Sustained PRO Collection
To assure longevity of national TJA registries, the data infrastructure and data collection procedures must support a complete and accurate database so that analyses will inform best practices in TJA implant selection and patient care. To engage surgeons and hospitals, registry procedures must be simplified to ensure continued participation. In addition, returning registry data to the surgeon encourages ongoing commitment to complete data collection. Surgeons value benchmarks by which to compare individual outcomes. In the UK and FORCE-TJR, surgeon-specific web reports present a summary of postoperative PROs over time to inform practice management. In an era of public reporting, this feedback is increasingly important to surgeons and hospitals for quality monitoring, contract negotiations, and patient care.
The unfortunate metal-on-metal THA implant recall highlights the potential public health importance of detecting early persistent pain in a large cohort of patients. Systematic analysis of pain trends across patients may have allowed earlier detection of implant-associated morbidity and facilitated earlier warnings to clinicians, manufacturers, and regulatory agencies. While this experience may be unique, it highlights a potential public health role for PRO collection in TJA registries.
Discussion
Some national registries have started collecting PROs and the added value is evident from the research that is emerging from these data [2, 19, 21]. Broader PRO adoption by TJA registries will require modified registry designs that include judicious selection of PRO measures and careful attention to complete data capture to assure valid analyses. Lessons learned from the early PRO implementation in a subset of international registries will inform future adoption.
Financial models to support PRO collection in TJA registries will vary across countries. To date, direct-to-patient collection methods have proven successful. This process operates in parallel to the hospital-reported implant data required by registries. It is possible that the two mechanisms will be integrated in the future if all data are captured in electronic medical records. Before this is feasible, incremental funding will be required for PRO capture. Whether government-funded or supported by orthopaedists, manufacturers, or research agencies, the costs of registry data collection must be justified by the value of the knowledge gained from the analyses. Innovative efforts to minimize data costs, including web and smart phone-based surveys, may also accelerate PRO data collection in the future.
In summary, the addition of PROs to TJA registries introduces challenges related to the registry design, logistics of PRO collection, and cost and sustainability. Each of these challenges requires modifications to the traditional hospital- and implant-centric design of many registries. Beyond these issues that affect all registries, the United States faces unique barriers owing to the volume of TJA procedures performed each year, the lack of a single national payer, and stringent data privacy regulations. Innovative, unbiased, and clinically refined TJA registries designed to evaluate the relative contributions of patient, clinical, and device factors to patient-reported function and pain relief, postoperative adverse events, and device failure hold great promise to guide best practices in TJA care. Implementation of lessons learned from comprehensive registries that include PROs will assure patients achieve optimal pain relief and functional gain with minimal adverse events and implant failures.
References
Ayers DC, Franklin PD, Trief PM, Ploutz-Snyder R, Freund D. Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty. 2004;19(7 suppl 2):125–130.
Baker P, Petheram T, Jameson S, Reed M, Gregg P, Deehan D. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2012;94:1501–1508.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
Centers for Disease Control and Prevention. National Hospital Discharge Survey: 2009 table, procedures by selected patient characteristics - number by procedure category and age. May 2012. Available at: http://www.cdc.gov/nchs/fastats/insurg.htm. Accessed February 2013.
Collins NJ, Roos EM. Patient-reported outcomes for total hip and knee arthroplasty: commonly used instruments and attributes of a “good” measure. Clin Geriatr Med. 2012;28:367–394.
Devlin NJ, Parkin D, Browne J. Patient-reported outcome measures in the NHS: new methods for analysing and reporting EQ-5D data. Health Economics. 2010;19:886–905.
EuroQol—a new facility for the measurement of health-related quality of life: the EuroQol Group. Health Policy. 1990;16:199–208.
Franklin PD, Allison JJ, Ayers DC. Beyond joint implant registries: a patient-centered research consortium for comparative effectiveness in total joint replacement. JAMA. 2012;308:1217–1218.
Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award. Functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–2604.
Goodfellow JW, O’Connor JJ, Murray DW. A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br. 2010;92:1628–1631.
Greenbaum JN, Bornstein LJ, Lyman S, Alexiades MM, Westrich GH. The validity of self-report as a technique for measuring short-term complications after total hip arthroplasty in a joint replacement registry. J Arthroplasty. 2012;27:1310–1315.
Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
International Society of Arthroplasty Registries. Statements (revised February 2007). Available at: http://www.isarhome.org/statements. Accessed May 21, 2013.
Jameson SS, Baker PN, Mason J, Rymaszewska M, Gregg PJ, Deehan DJ, Reed MR. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. Bone Joint J. 2013;95:747–757.
Lingard EA, Riddle DL. Impact of psychological distress on pain and function following knee arthroplasty. J Bone Joint Surg Am. 2007;89:1161–1169.
New Zealand Orthopaedic Association. The New Zealand Joint Registry Thirteen Year Report: January 1999 to December 2011. Wellington, New Zealand: New Zealand Orthopaedic Association; 2012.
Nilsdotter AK, Petersson IF, Roos EM, Lohmander LS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–930.
Rising JP, Reynolds IS, Sedrakyan A. Delays and difficulties in assessing metal-on-metal hip implants. N Engl J Med. 2012;367:e1.
Rolfson O, Karrholm J, Dahlberg LE, Garellick G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br. 2011;93:867–875.
Rolfson O, Rothwell A, Sedrakyan A, Chenok KE, Bohm E, Bozic KJ, Garellick G. Use of patient-reported outcomes in the context of different levels of data. J Bone Joint Surg Am. 2011;93(suppl 3):66–71.
Rothwell AG, Hooper GJ, Hobbs A, Frampton CM. An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br. 2010;92:413–418.
van den Akker-Scheek I, Stevens M, Groothoff JW, Bulstra SK, Zijlstra W. Preoperative or postoperative self-efficacy: which is a better predictor of outcome after total hip or knee arthroplasty? Patient Educ Couns. 2007;66:92–99.
Ware JE, Kosinski M, Bjomer JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36v2 Health Survey. 2nd ed. Lincoln, RI: QualityMetric Inc; 2007.
Wilcox S, Shumaker SA, Bowen D J, Naughton MJ, Rosal MC, Ludlam SE, Dugan E, Hunt JR, Stevens S. Promoting adherence and retention to clinical trials in special populations: a Women’s Health Initiative workshop. Control Clin Trials. 2001;22:279–289.
Acknowledgments
The authors acknowledge the broad team of investigators who have contributed to the design and implementation of the FORCE-TJR model, including Jeroan J. Allison MD, Wenjun Li PhD, Milagros C. Rosal PhD, Bruce Barton PhD, Sharina Person PhD, John E. Ware PhD, Courtland Lewis MD, Philip Noble PhD, Regis O’Keefe MD, PhD, and Vincent Pellegrini MD. In addition, FORCE-TJR is dependent on the ongoing collaboration of more than 100 surgeons who willingly allow enrollment of their patients. We also acknowledge Sylvie Puig PhD for her editorial contributions.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of the authors has received, during the study period, funding from the Agency for Healthcare Research and Quality (Grant P50HS018910). Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Franklin, P.D., Harrold, L. & Ayers, D.C. Incorporating Patient-reported Outcomes in Total Joint Arthroplasty Registries: Challenges and Opportunities. Clin Orthop Relat Res 471, 3482–3488 (2013). https://doi.org/10.1007/s11999-013-3193-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3193-2