Abstract
Background
Controversy persists regarding the safety of same-day bilateral TKAs, and indications for same-day versus staged bilateral surgery need to be clarified.
Questions/purposes
We compared the (1) 30-day mortality, (2) rates of in-hospital complications, (3) in-hospital charges, and (4) risk factors for complications among patients undergoing same-day and staged bilateral TKAs at two separate admissions within 1 year either less than 3 months apart (staged 0–3) or more than 3 months apart (staged 3–12) at an institution where same-day bilateral TKAs were discouraged in patients with more severe medical comorbidities.
Methods
We analyzed institutional data from 3960 same-day, 172 staged 0–3, and 1533 staged 3–12 bilateral TKAs performed between 1998 and 2011. Patient demographics, comorbidities, and 30-day mortality were tabulated. Same-day patients were younger and healthier. Outcomes of interest included complications, blood transfusions, transfer to rehabilitation, and in-hospital charges. Regression models were conducted to identify independent risk factors for major morbidity or mortality.
Results
There were no differences in 30-day mortality among groups. The same-day group experienced more acute postoperative anemia, blood transfusions, and transfers to rehabilitation, but otherwise had complications comparable to those of the staged groups. In-hospital charges were lower in the same-day group. Congestive heart failure and pulmonary hypertension were the most significant factors associated with morbidity and mortality in the same-day group.
Conclusions
In a high-volume subspecialty setting in which patients undergoing same-day bilateral TKAs were generally much healthier and younger, we found that same-day bilateral TKAs appeared to be safe.
Level of Evidence
Level III, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many patients present with symptomatic bilateral knee osteoarthritis, and many of these patients opt to have bilateral TKAs [23]. In 2007, approximately 7% of all TKAs performed in the United States were same-day bilateral [12] and 15% were staged bilateral (two sequential unilateral TKAs performed within 1 year) [1]. It has been predicted that by 2030 there will be a 456% increase in TKAs performed each year [12].
Given the potential cost benefits and overall shorter hospitalization time [23], the resulting financial and clinical burden might be dramatically reduced just by performing more same-day bilateral TKAs in those with bilateral joint disease. Data have shown a decrease in 30-day mortality after same-day bilateral TKAs from 0.99% in 1990 [24] to 0.38% in 2007 [14]. However, despite potential advantages of the same-day approach, including exposure to the risks of anesthetic only once, one postoperative course of pain, reduced rehabilitation, and an earlier return to baseline function [10, 11, 23], the safety of same-day procedures has been questioned because of higher morbidity and mortality when compared with unilateral TKAs [15, 22]. Several studies have attempted to compare the incidence of complications after same-day bilateral TKAs, staged bilateral TKAs, and unilateral TKAs using single institution databases, large administrative datasets, or meta-analyses [1, 6, 7, 9, 14, 15, 18, 22, 26–28]. However, there are no randomized trials comparing the safety of these surgical strategies. Because of the diversity of study settings and designs, it is difficult to draw definitive conclusions [1, 6, 7, 9, 14, 15, 18, 22, 26–28].
We therefore compared the (1) 30-day mortality, (2) rates of in-hospital complications, (3) in-hospital charges, and (4) risk factors for complications among patients undergoing same-day bilateral TKAs, staged bilateral TKAs during two separate admissions fewer than 3 months apart (staged 0–3), and staged bilateral TKAs where the two admissions were from 3 to 12 months apart (staged 3–12) at an institution where same-day bilateral TKAs were discouraged for patients with more severe medical comorbidities.
Patients and Methods
Data Collection and Patient Selection
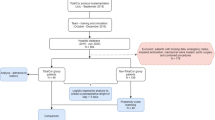
This study involved retrospective data collection from a large computerized patient database based on hospital discharge data and medical records. Hospital and physicians’ clinical records were also reviewed for eligible patients, as were death records for in-hospital mortalities. Data collected for this study included patient demographics (age, sex, and race), length of hospital stay (LOS), and discharge disposition (rehabilitation center, discharge to higher level of care, and other [eg, home]). Total charges for the hospitalization (including the cost associated with 12–24 hours in the postanesthesia care unit [PACU]) were only available and collected for patients having surgery in 2003 and later. ICD-9-CM [8] codes stored in the database were used to identify patient diagnosis group (osteoarthritis, inflammatory arthritis, or other) and to determine patient comorbidities and complications. The Charlson Comorbidity Index was calculated using the modification of Deyo et al. [4, 5] for administrative data to estimate the overall comorbidity burden. Specific comorbidities of interest identified via ICD-9-CM coding were hypertension, diabetes mellitus, obesity, hypercholesterolemia, pulmonary disease, renal disease, coronary artery disease (CAD), congestive heart failure (CHF), sleep apnea, pulmonary hypertension, liver disease, and coagulopathy [8]. The study was approved by our institutional review board.
All patients who underwent at least one primary TKA (ICD-9-CM procedure code 81.54) between January 1, 1998, and December 31, 2011, were identified. Patients classified as having same-day bilateral TKAs had two primary TKA procedure codes during a single admission with the same procedure date, as defined by discharge coding rules. The same-day group underwent bilateral TKAs performed by a single surgical team during a single anesthetic session with sequential inflation of the tourniquets. Patients undergoing staged bilateral TKAs had two separate admissions within 365 days with a single primary TKA procedure code entered for each admission. This group was further divided into two subgroups: the staged 0–3 group, when the second TKA procedure date was less than 92 days after the first TKA procedure date; and the staged 3–12 group, when the second TKA was performed 92 to 365 days after the first TKA. Patients who had a second primary TKA more than 365 days after the first TKA, those who underwent staged bilateral TKAs during a single hospitalization (separate anesthetic sessions), and those who underwent unilateral TKAs were excluded.
Our hospital has established guidelines to limit same-day bilateral TKAs to healthier and younger patients whenever possible, with adherence to these guidelines increasing over time. If the patient was deemed unstable intraoperatively, the second arthroplasty was performed electively at a later hospitalization. All patients underwent arthroplasty in a laminar airflow room, and the vast majority of them received regional anesthetics. All patients were admitted to the PACU immediately postoperatively. Patients undergoing same-day bilateral TKAs spent the first 12 to 24 hours after surgery in the PACU for monitoring and were discharged from the unit to the floor only when their pain was controlled, they had a stable hemodynamic profile, and their urine output was deemed acceptable. All patients received postoperative thromboembolic prophylaxis for 4 to 6 weeks.
Study Population
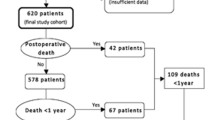
Between January 1998 and December 2011, 3960 patients underwent same-day bilateral TKAs, 172 underwent staged 0–3 bilateral TKAs, and 1533 underwent staged 3–12 TKAs (Table 1). The mean (± SD) age of the same-day bilateral TKA group (65 ± 9 years) was lower than that of the staged 3–12 bilateral TKA group (69 ± 9 years) (p < 0.001) but similar to that of the staged 0–3 bilateral TKA group (67 ± 9 years) (p = 0.1). The same-day group was more likely to be male and healthier, with a mean Charlson-Deyo comorbidity index of 0.3 ± 0.8 compared to 0.6 ± 1.1 and 0.5 ± 1.0 for the staged 0–3 and staged 3–12 groups, respectively (p < 0.001 for both comparisons) (Table 1). Idiopathic osteoarthritis was the most prevalent diagnosis for all groups (Table 1). There were moderate differences in the prevalence of many comorbidities among groups (Table 1). In particular, hypertension, hypercholesteremia, pulmonary disease, diabetes mellitus, and CAD were less prevalent in the same-day group.
Outcome Evaluation
Protected information of the study subjects was submitted to the Social Security Death Index (SSDI) to obtain data on patient survivorship through September 2012 to calculate 30-day mortality. Information for patients not matched to the SSDI was gathered from the individual physician’s office charts where detailed clinical followup was recorded.
Procedure-related complications were identified using ICD-9-CM diagnosis codes for complications of surgical and medical care (997.XX–999.XX) [8]. The list of specific procedure-related complications (cardiac and central nervous system [CNS] complications included in major complications; postoperative infection/cellulitis included in minor complications) and ICD-9-CM codes are provided in Appendix 1 (supplemental materials are available with the online version of CORR®). An additional 16 complications were identified using ICD-9-CM codes (Appendix 1; supplemental materials are available with the online version of CORR®). These acute systemic and local complications during the hospitalization period were classified as minor or major. Minor complications included (1) minor cardiac events (hypotension, syncope and collapse, angina, and tachycardia), (2) delirium, (3) urinary tract infection, (4) urinary retention, (5) postoperative infection/cellulitis, (6) thromboembolism/deep vein thrombosis, (7) paralytic ileus; and (8) pleural effusion. Major complications included (1) CNS infarction (ischemic stroke), (2) pulmonary compromise, (3) sepsis, (4) shock/cardiorespiratory arrest, (5) acute myocardial infarction, (6) major cardiac (except myocardial infarction), (7) pneumonia, and (8) pulmonary embolism. For this study, all adverse events were evaluated at the patient level; thus, a patient in either of the staged bilateral TKA groups was considered to have had a specific complication if the complication occurred during either or both surgical admissions.
Statistical Methods
Descriptive statistics were calculated to examine patient characteristics and complication rates by group. Patient demographic and comorbidity status at the time of the first surgery were used for the staged 0–3 and staged 3–12 groups. Means and SDs are reported for continuous variables, while frequencies and percentages by patient are reported for categorical variables. Medians and interquartile ranges (IQRs) are reported for charges. Post hoc multiple pairwise comparisons between groups were performed for selected outcomes of interest. Fisher’s exact test was used for categorical variables with the Bonferroni adjustment for multiple comparisons. Continuous variables were analyzed using an ANOVA model on the rank-transformed data, also using the Bonferroni adjustment for multiple comparisons.
A multivariable logistic regression analysis was conducted for the same-day group alone to identify predictors of major morbidity or mortality in this population. Covariates in the model included age (categorized as < 55, 56–65, 66–75, and > 75 years), sex, race, diagnosis, and individual comorbidities. For each predictor variable, the odds ratio (OR), 95% CI, and p value were computed. Results are presented for a simple logistic model (Model 1) with the only independent variable being surgery group and a multivariable logistic regression model (Model 2) with age, sex, race, specific comorbidity indicators, number of allogenic blood units received, and time period of surgery (1998–2005 versus 2006–2011) as additional covariates. The time period variable is included to address temporal changes in LOS and other factors such as surgical technique, perioperative pain control, mobilization and rehabilitation, and change in patients’ expectations across the study period. All analyses were performed using SAS® software (Version 9.2; SAS Institute Inc, Cary, NC, USA). Statistical significance was set at a p value of less than 0.05.
Results
There was no significant difference in mortality among the three groups. Thirty-day mortality was 0.03% for the same-day group, 0% for the staged 0–3 group, and 0.07% for the staged 3–12 group (p = 0.75).
The mean LOS was significantly lower in the same-day group (5.4 ± 2 days) than in the staged 0–3 (8.9 ± 3 days) and staged 3–12 group (9.2 ± 2.8 days) (Table 2). The incidences of acute posthemorrhagic anemia, overall blood units transfused, and allogenic blood units transfused were higher in the same-day group (p < 0.001) (Table 2). However, a higher proportion of patients required mechanical ventilation (reflecting acute pulmonary dysfunction or decreased ventilation) in the staged 0–3 (0.58%) and staged 3–12 (0.59%) groups than in the same-day group (0.38%) (Table 2). Patients in the same-day group were more likely to be discharged to a rehabilitation center than patients in the staged 0–3 or staged 3–12 groups (72.1% versus 39.5% versus 45.9%, respectively; p < 0.001) (Table 2). The overall rates of procedure-related complications were similar among groups (1.72% versus 1.16% versus 2.74%; p = 0.037); however, there was a trend toward lower complication rate in the same-day group compared to the staged 3–12 group (1.7% versus 2.7%; p = 0.054) (Table 3). The rates for most minor complications were comparable among groups. Interestingly, the rates of syncope and collapse, urinary tract infection, and in-hospital surgical site infection (including both superficial and deep) were significantly lower in the same-day group than in the staged 3–12 group (Table 4). Similarly, the rates of the various major complications were similar among groups; however, there was a trend of lower pulmonary compromise in the same-day group compared to the staged 3–12 group (3.5% versus 4.9%; p = 0.059) (Table 4). Major morbidity or mortality was not significantly different among groups (5.2% versus 2.9% versus 6.4%; p = 0.071) (Table 4).
Charges associated with in-hospital care were lower in the same-day group than in the staged 0–3 and staged 3–12 groups. Median in-hospital charges were USD 63,045 (IQR, USD 56,941–70,869), USD 88,160 (IQR, USD 79,583–100,450, both hospitalizations), and USD 88,618 (IQR, USD 81,657–97,974, both hospitalizations) for the same-day, staged 0–3, and staged 3–12 groups, respectively (p < 0.001).
CHF and pulmonary hypertension were associated with a greater risk of major morbidity and mortality in patients who underwent same-day bilateral TKAs. The multivariable logistic regression model showed that patients with CHF were five times more likely to have major morbidity or to die (OR: 5.21; 95% CI: 2.46–11.04; p < 0.001), while patients with pulmonary hypertension had two times the risk (OR: 2.34; 95% CI: 1.08–5.08; p = 0.032). The covariates included for model adjustment are listed in Table 5. Same-day patients having surgery in 2006 or later were less likely to develop major morbidity or to die (OR: 0.64, 95% CI: 0.48–0.86; p = 0.003). The simple regression Model 1 (Table 6) showed similar risk among groups, except for a trend toward higher risk in the staged 3–12 group compared to the same-day group (OR: 1.24; 95% CI: 0.97–1.59; p = 0.084). Model 2 (Table 6) similarly showed that risk was comparable among groups after adjusting for differences in patient characteristics among groups.
Discussion
Despite the potential advantages of same-day over staged bilateral TKAs, controversy persists regarding the safety of same-day procedures. If candidates for same-day bilateral TKAs who have higher risk for perioperative complications can be effectively identified and counseled away from this more invasive surgery, same-day bilateral TKA may be the preferred surgical strategy for an appropriate subset of patients. Therefore, we compared 30-day mortality and perioperative morbidity in a large series of same-day and staged bilateral TKAs performed at a high-volume institution where a selective preoperative screening process has been adopted that tends to drive practice away from same-day bilateral TKAs in patients with more severe medical complications.
There are limitations inherent to our study design. Firstly, there is selection bias in retrospectively constructing the three groups. The same-day group was younger and healthier based on the selection protocol utilized in our institution. This could account for the low perioperative morbidity and mortality and therefore the decreased cost of care in this group. However, the risk of major morbidity or mortality was comparable among groups after adjustment for these types of patient factors, which indicates that same-day procedures are safe in appropriately selected patients. Secondly, in this study, we could not account for patients who were planned for one type of bilateral surgery and experienced a major complication or died after the first arthroplasty or electively delayed or declined the second procedure. Patients in the two staged groups are also subject to an immortal time bias for the duration of time between their two arthroplasty admissions (up to 12 months) because patients must not have died during this time interval or delayed the second surgery to more than 12 months after their first surgery. The staged groups also have two hospitalizations during which a complication could occur, while the same-day group has only one hospitalization. However, we believe that this an inherent reason for our analysis, which aims to evaluate the risks of same-day surgery compared to the risk of an additional hospitalization. Thirdly, this study lacks specific clinical data that may be of interest such as the impact of specific surgeon or anesthesiologist. However, since this study spans a period of 14 years and encompasses 5665 patients and 7370 TKA admissions, we believe that the diversity in practice of multiple orthopaedic surgeons may provide a more accurate estimate of events surrounding bilateral TKAs than various prospective studies that have limited sample size and cannot capture low-incidence outcomes.
Further limitations include the reliance on administrative data and the SSDI to provide complete 30-day followup. However, we identified each outcome using these databases in an identical fashion in all cohorts, minimizing the likelihood that data errors would bias the findings differently in each group. In addition, ICD-9-CM coding has been accepted as a valid method to identify and analyze these variables and is associated with a high predictive value [2, 3, 29]. Finally, the clinical decision-making process may have changed over the study period and various unmeasured confounders may exist that have influenced the operative plan (same-day versus staged) and consequently the perioperative outcomes. Although our institutional criteria are meant to guide and not dictate the selection pattern of patients, it is likely that strong social, economic, and other patient-related factors, as well as surgeon preferences and considerations, might have played an important role in the decision-making process. This could justify why we still found patients with comorbidities such as pulmonary disease, CAD, and CHF in the same-day group.
This study showed that patients undergoing same-day bilateral TKAs had a low 30-day mortality rate, which was similar to the rates in the patients undergoing staged 0–3 and staged 3–12 bilateral TKAs. The risk for major morbidity or mortality was comparable among the cohorts after adjustment for significant patient-related factors, which is similar to other studies using large databases finding no significant differences between same-day and staged bilateral TKAs regarding in-hospital [18] and 90-day mortality [28]. However, two meta-analyses [7, 22] and the Swedish Knee Arthroplasty Register [26] showed a higher rate of mortality in same-day compared to staged bilateral TKAs. Another study [21] identified same-day bilateral TKA as a significant risk factor for perioperative mortality and concluded that same-day bilateral TKAs should be avoided in sick or elderly patients and that the medical condition of patients who have a history of cardiac or pulmonary problems should be optimized preoperatively [21]. This is precisely what the guidelines implemented by our institution for patient selection aim to do and our data show that use of this selective preoperative screening process can reduce the risk of mortality.
In our cohort, the overall rates of procedure-related complications were similar among the bilateral TKA groups, while same-day TKA was associated with lower in-hospital infection rate. Prior research has shown that the overall incidence of procedure-related complications was lower after same-day compared to staged bilateral TKAs during a single hospitalization [18]. Likewise, a recent analysis [14] suggested, after risk adjustment, the odds of developing hematoma and infection were lower in patients undergoing same-day bilateral TKAs than in patients undergoing staged bilateral TKAs.
The overall minor or major complication rates were also similar among groups. Interestingly, both minor and major cardiac, pulmonary, and thrombotic events were comparable among groups. Two meta-analyses have demonstrated higher rates for neurologic, cardiac, and respiratory complications in same-day compared to staged bilateral TKAs [7, 22]. Similarly, same-day bilateral TKAs were found to be associated with a moderately higher adjusted risk of adverse cardiovascular outcomes and pulmonary embolism within 30 days compared with staged bilateral TKAs [14].
In-hospital charges were lower for same-day bilateral TKAs despite an extended stay in the PACU for the first 12 to 24 hours after surgery. All patients undergoing same-day bilateral TKAs received this higher level of monitoring, which is equivalent to one overnight stay in the intensive care unit. Despite the extended stay in the PACU, in-hospital charges were lower for the same-day group. Our results agree with previously published studies, which showed that the average in-hospital costs for one-stage TKA were significantly lower (by 24%) than for two-stage TKA [13]. Similarly, another study demonstrated that the hospitalization cost of same-day bilateral TKAs was 36% less than two unilateral TKAs [23].
We identified pulmonary hypertension and CHF as significant risk factors for major morbidity or mortality in the same-day bilateral TKA cohort. The preexisting decreased vascular reserve of the lungs, specifically the load-dependent response and capacity of the lungs to absorb the embolic insult, has been previously documented in healthy patients undergoing bilateral TKAs [19]. The ability of the pulmonary vascular bed to compensate may be overwhelmed by the larger embolic load of two consecutively performed arthroplasties. The significant association of pulmonary hypertension with increased rates of perioperative morbidity and mortality has also been documented [17]. In this context, a history of CHF suggests reduced end organ reserve and thus decreased ability to compensate for the stresses of surgery [20]. Therefore, physicians should be cautioned against worsening of cardiopulmonary function, especially in the setting of same-day bilateral TKAs, because these procedures are associated with significant metabolic injury, fluid shifts, and other insults exposing various organ systems to significant stresses [15, 16, 18, 25].
In conclusion, this study represents one of the largest institutional investigations evaluating perioperative morbidity and mortality in patients undergoing bilateral TKAs using modern anesthetic and surgical techniques. Our data suggest, in a high-volume subspecialty center, a selective preoperative screening process for candidates for same-day bilateral TKAs that tends to exclude patients with CHF and pulmonary hypertension can lead to safe use of same-day bilateral TKAs as a treatment option. As the diagnosis of occult diseases such as pulmonary hypertension may be difficult, further screening may be indicated in those at high risk for the disease, ie, patients with sleep apnea, obesity, and chronic obstructive pulmonary disease.
References
Barrett J, Baron JA, Losina E, Wright J, Mahomed NN, Katz JN. Bilateral total knee replacement: staging and pulmonary embolism. J Bone Joint Surg Am. 2006;88:2146–2151.
Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485.
Bozic KJ, Chiu VW, Takemoto SK, Greenbaum JN, Smith TM, Jerabek SA, Berry DJ. The validity of using administrative claims data in total joint arthroplasty outcomes research. J Arthroplasty. 2010;25(6 suppl):58–61.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619.
Fabi DW, Mohan V, Goldstein WM, Dunn JH, Murphy BP. Unilateral vs bilateral total knee arthroplasty risk factors increasing morbidity. J Arthroplasty. 2011;26:668–673.
Hu J, Liu Y, Lv Z, Li X, Qin X, Fan W. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2011;131:1291–1298.
International Classification of Diseases, 9th Revision, Clinical Modification, 6th ed, 2008. Available at: http://icd9cm.chrisendres.com/. Accessed September 19, 2008.
Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91:64–68.
Kovacik MW, Singri P, Khanna S, Gradisar IA. Medical and financial aspects of same-day bilateral total knee arthroplasties. Biomed Sci Instrum. 1997;33:429–434.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Levit K, Wier L, Stranges E, Ryan K, Elixhauser A. HCUP facts and figures: statistics on hospital-based care in the United States 2007. Available at: http://www.hcup-us.ahrq.gov/reports/factsandfigures/2007/exhibit3_1.jsp. Accessed March 17, 2011.
Macario A, Schilling P, Rubio R, Goodman S. Economics of one-stage versus two-stage bilateral total knee arthroplasties. Clin Orthop Relat Res. 2003;414:149–156.
Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH. A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am. 2011;93:2203–2213.
Memtsoudis SG, Gonzalez Della Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res. 2008;466:2617–2627.
Memtsoudis SG, Ma Y, Chiu YL, Poultsides L, Gonzalez Della Valle A, Mazumdar M. Bilateral total knee arthroplasty: risk factors for major morbidity and mortality. Anesth Analg. 2011;113:784–790.
Memtsoudis SG, Ma Y, Chiu YL, Walz JM, Voswinckel R, Mazumdar M. Perioperative mortality in patients with pulmonary hypertension undergoing major joint replacement. Anesth Analg. 2010;111:1110–1116.
Memtsoudis SG, Ma Y, Gonzalez Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206–1216.
Memtsoudis SG, Salvati EA, Go G, Ma Y, Sharrock NE. Perioperative pulmonary circulatory changes during bilateral total hip arthroplasty under regional anesthesia. Reg Anesth Pain Med. 2010;35:417–421.
Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32.
Parvizi J, Sullivan TA, Trousdale RT, Lewallen DG. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg Am. 2001;83:1157–1161.
Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2007;89:1220–1226.
Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13:172–179.
Ritter M, Mamlin LA, Melfi CA, Katz BP, Freund DA, Arthur DS. Outcome implications for the timing of bilateral total knee arthroplasties. Clin Orthop Relat Res. 1997;345:99–105.
Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty: a survival analysis. J Bone Joint Surg Am. 2003;85:1532–1537.
Stefansdottir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: results from the Swedish Knee Arthroplasty Register. Clin Orthop Relat Res. 2008;466:3066–3070.
Urban MK, Chisholm M, Wukovits B. Are postoperative complications more common with single-stage bilateral (SBTKR) than with unilateral knee arthroplasty? Guidelines for patients scheduled for SBTKR. HSS J. 2006;2:78–82.
Walmsley P, Murray A, Brenkel IJ. The practice of bilateral, simultaneous total knee replacement in Scotland over the last decade: data from the Scottish Arthroplasty Project. Knee. 2006;13:102–105.
White RH, Garcia M, Sadeghi B, Tancredi DJ, Zrelak P, Cuny J, Sama P, Gammon H, Schmaltz S, Romano PS. Evaluation of the predictive value of ICD-9-CM coded administrative data for venous thromboembolism in the United States. Thromb Res. 2010;126:61–67.
Acknowledgments
We thank Andres Gleich MBA, Christopher Ferrandina BA, and David Staum BA for their expertise with the data collection and management.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Poultsides, L., Memtsoudis, S., Gonzalez Della Valle, A. et al. Perioperative Morbidity and Mortality of Same-day Bilateral TKAs: Incidence and Risk Factors. Clin Orthop Relat Res 472, 111–120 (2014). https://doi.org/10.1007/s11999-013-3156-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3156-7