Abstract
Background
Trapeziometacarpal (TMC) arthritis of the thumb is a common source of hand pain and disability. TMC ligamentous instability may play a role in TMC degeneration. However, the relative importance of the TMC ligaments in the etiology of degeneration and the use of surgery to treat instability in early-stage arthritis are unclear.
Questions/purposes
In this review, we addressed several questions: (1) What are the primary ligamentous stabilizers of the thumb TMC joint? (2) What is the evidence for ligament reconstruction or ligament imbrication in the treatment of thumb TMC joint osteoarthritis? And (3) what is the evidence for thumb metacarpal osteotomy in the treatment of thumb TMC joint osteoarthritis?
Methods
We performed a systematic review of the literature using PubMed (MEDLINE®) and Scopus® (EMBASE®) for peer-reviewed articles published until November 2012. Fifty-two studies fit the inclusion criteria. Twenty-four studies were anatomic, biomechanical, or histopathologic studies on TMC joint ligamentous anatomy, 16 studies were clinical studies concerning ligament reconstruction, and 12 studies were clinical studies on thumb metacarpal osteotomy.
Results
Over the past two decades, increasing evidence suggests the dorsoradial ligament is the most important stabilizer of the TMC joint. Other ligaments consistently identified are the superficial anterior oblique, deep anterior oblique, intermetacarpal, ulnar collateral, and posterior oblique ligaments. Ligament reconstruction and metacarpal osteotomy relieve pain and improve grip strength based on Level IV studies.
Conclusions
The dorsal ligaments are the primary stabilizers of the TMC joint. Ligament reconstruction and metacarpal osteotomy ameliorate ligamentous laxity and relieve pain based on Level IV studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) of the thumb trapeziometacarpal (TMC) joint can be a debilitating disorder, resulting in hand pain and reduced strength and motion during activities of daily living [2, 15]. The disease is also exceedingly common. The prevalence of TMC OA is reportedly 7% for men and 15% for women 30 years or older [20]. As many as 1/3 of all postmenopausal women have radiographic evidence of arthritic changes, with 1/3 of these women experiencing basal joint pain [1].
The underlying etiology of TMC OA is poorly understood. Many investigators have theorized that ligamentous laxity of the TMC joint leads to an incongruous relationship between the joint surfaces [10, 15, 42]. This incongruity is thought to lead to smaller contact areas and thus greater contact stresses in certain areas of the joint, leading to degradation and OA [2, 14, 15].
However, controversy exists regarding both the number and relative importance of the TMC ligaments. The anterior oblique ligament (AOL) [26, 27, 42, 43], the intermetacarpal ligament (IML) [40], and the dorsoradial ligament (DRL) [4, 31, 37, 50, 54] have all been proposed as primary stabilizers of the TMC joint. Moreover, the use of ligament reconstruction or metacarpal osteotomy in the setting of ligamentous laxity and early-stage OA is also controversial.
In this review, we addressed the following questions: (1) What are the primary ligamentous stabilizers of the TMC joint? (2) What is the evidence for ligament reconstruction or ligament imbrication in the treatment of OA of the TMC joint? And (3) what is the evidence for thumb metacarpal osteotomy in the treatment of OA of the TMC joint?
Search Strategy and Criteria
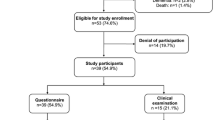
We searched MEDLINE® (through PubMed) and EMBASE® (through Scopus®) up to November 2012. Articles were identified using the following query: “trapeziometacarpal joint” OR ((“thumb” OR “first”) AND (“carpometacarpal joint” OR “basal joint”)). The search was performed under the guidance of our departmental librarian. We also performed a hand search of the following journals for articles published between January 2012 and November 2012: Clinical Orthopaedics and Related Research ®, Journal of Bone and Joint Surgery, and Journal of Hand Surgery. We identified a total of 2112 articles. The results were then entered into EndNote® (Thomas Reuters, Carlsbad, CA, USA) for removal of duplicate entries, resulting in a total of 1334 articles for title and abstract review (Fig. 1).
Articles were included in the systematic review based on the following criteria: (1) published in English and (2) an anatomic, biomechanical, or histopathologic study on ligamentous stability of the thumb TMC joint or (3) a clinical study with a Level I, II, III, or IV study design or a biomechanical study on metacarpal extension osteotomy or (4) a clinical study with a Level I, II, III, or IV study design or biomechanical study on ligament reconstruction or ligament imbrication independent of arthroplasty. We excluded articles on ligament reconstruction in the setting of arthroplasty or fractures, trapezial osteotomy, review articles, and conference proceedings. Articles where full text was unavailable were excluded.
Two of us (JDL, RJS) independently reviewed the titles and abstracts of each article for inclusion and exclusion criteria. If an article was identified by one author and not another, it was included for full-text review. Forty-six articles were identified for potential inclusion in the systematic review, and full-text articles were obtained and further reviewed by two of us (JDL, RJS). The bibliographies of included articles were searched for additional references and six additional references were identified.
On completion of the search, 52 articles were included in the systematic review. Twenty-four articles were anatomic, biomechanical, or histopathologic studies on ligamentous anatomy [4, 5, 7, 11, 12, 15, 21–23, 26–28, 31, 34, 37–40, 42, 43, 45, 50, 52, 54], 12 articles were clinical studies on metacarpal osteotomy [3, 18, 19, 25, 30, 36, 41, 44, 48, 53, 57, 58], and 16 articles were on ligament reconstruction [6, 8, 9, 13, 16, 17, 24, 29, 32, 33, 35, 39, 47, 49, 51, 55]. No articles were on ligament imbrication.
Results
What Are the Primary Ligamentous Stabilizers of the TMC Joint?
In 1944, Haines [22] described five ligaments of the TMC joint: the radial ligament, AOL, posterior oblique ligament (POL), anterior IML, and posterior IML; essentially supporting Weitbrecht’s [56] original descriptions in 1742. There have been further elucidations of ligamentous anatomy since then, with varying importance placed on the contributions of individual ligaments to TMC stability (Table 1). The role of the AOL, originally believed by Eaton and Littler [15] and Pellegrini [42, 43] to be the primary stabilizer of the TMC joint, has been questioned by biomechanical and anatomic studies performed over the past 20 years, indicating the DRL is the primary restraint to dorsal translation. Specifically, Strauch et al. [50], Najima et al. [37], Van Brenk et al. [54], Bettinger et al. [4, 5], Colman et al. [11], Tan et al. [52], Hagert et al. [21], and Ladd et al. [31], to varying degrees, found the DRL (or other nearby dorsal ligaments) to be the primary ligament resisting dorsal joint translation, as well as the most robust and well-innervated ligament. (See Appendix 1 for more detail on the individual studies. Supplemental materials are available with the online version of CORR.)
What Is the Evidence for Ligament Reconstruction or Ligament Imbrication in the Treatment of Thumb TMC Joint OA?
This systematic review produced 16 articles detailing ligamentous reconstruction of the TMC joint [6, 8–10, 13, 16, 17, 24, 29, 32, 33, 35, 47, 49, 51, 55]. These articles reflect a wide array of surgical procedures utilizing different grafts and reconstructing different ligaments around the TMC joint. The palmaris longus [8, 49], extensor carpi radialis longus [6, 16], abductor pollicis longus [9, 10, 29], extensor pollicis brevis [29], fascia lata [35], and flexor carpi radialis (FCR) [13] have been used by authors in a variety of reconstructions involving the volar ligament [10, 13, 24, 51], dorsal ligament [13, 29, 35, 49], or IMLs [6, 8, 9, 16].
The Eaton-Littler procedure is by far the most studied procedure, with five of 16 articles identified reporting on its outcomes, virtually all of which demonstrate that the procedure relieves pain and improves grip strength (Table 2). All studies reported are Level IV studies. On close inspection, the Eaton-Littler procedure, using a strip of the FCR through an extraarticular drill hole in the thumb metacarpal base and secured to the FCR tendon, actually reconstructs both the AOL and the DRL. We did not find any clinical studies on techniques of ligament reefing or imbrication to stabilize the TMC joint; however, Koff et al. [30], in a cadaveric biomechanical study, found the dorsal limb of the Eaton-Littler ligament reconstruction reduced laxity in the dorsovolar direction only, the volar limb of the reconstruction reduced laxity in both the dorsovolar and radioulnar directions, and the total ligament reconstruction reduced laxity in the dorsovolar, radioulnar, and pronation-supination directions. (See Appendix 2 for further detail on the individual studies. Supplemental materials are available with the online version of CORR.)
What Is the Evidence for Thumb Metacarpal Osteotomy in the Treatment of Thumb TMC Joint OA?
The metacarpal extension osteotomy procedure was first reported by Wilson [57] in 1973 as a treatment for TMC OA to improve pain and thumb position. Since then, the indications have expanded to patients with minimal arthritic changes and TMC instability, although all studies are Level IV case series (Table 3). These studies consistently demonstrate that metacarpal osteotomy results in pain relief at short- to medium-term followup (2–12 years). The biomechanical rationale for the clinical success of the procedure has been attributed to shifting of joint contact areas to nonarthritic cartilage [44] and improving dynamic joint stability in the position of lateral pinch by altering the tension arc of the dorsal TMC ligaments [30]. Typically, a 30° extension osteotomy is created at the metacarpal base, although experimentally Koff et al. [30] found a 15° osteotomy was equally effective in reducing joint laxity. (See Appendix 3 for a detailed description of osteotomy studies. Supplemental materials are available with the online version of CORR.)
Discussion
TMC OA of the thumb is a common source of hand pain and disability, and TMC ligamentous instability may play a role in TMC degeneration. However, controversy exists regarding both the number and relative importance of the TMC ligaments. Similarly, the use of ligament reconstruction or metacarpal osteotomy in the setting of ligamentous laxity and early-stage OA is also controversial. In this review, we addressed the following questions: (1) What are the primary ligamentous stabilizers of the TMC joint? (2) What is the evidence for ligament reconstruction or ligament imbrication in the treatment of OA of the TMC joint? And (3) what is the evidence for thumb metacarpal osteotomy in the treatment of OA of the TMC joint?
There are several limitations to this study. First, only English literature articles were included in our systematic review. Translation of non-English literature would have been cost-prohibitive and may have introduced bias by the translator. In addition, our search was limited to indexed peer-reviewed articles. This type of search excludes original texts and book chapters, but this is the accepted methodology for a systematic review and we believe the results to be comprehensive. Second, biomechanical and anatomic studies are generally reported in an inconsistent manner, and therefore this review may reflect the bias of the authors in synthesizing the results. However, we believe the comprehensive and systematic nature of this review accurately conveys the evolution in and our current understanding of TMC ligamentous stability and the associated surgical procedures.
The six thumb TMC ligaments consistently identified in the literature are the DRL, superficial AOL, deep AOL, IML, ulnar collateral ligament, and POL. Other ligaments identified include a dorsocentral ligament [21, 31], dorsal TMC [31], intermediate (dorsal) [7], and distinct dorsal and volar IMLs. Controversy exists over the primary stabilizer of the TMC joint, but over the past two decades, the DRL has emerged as the most likely candidate to limit dorsal translation of the TMC joint. Various authors have shown the DRL not only is the primary biomechanical restraint to subluxation [11, 50, 54] but also is anatomically thick [4], mechanically robust [5], highly cellular [31], and well innervated [21, 31]. Nevertheless, the role that each TMC ligament plays in the development of TMC OA remains incompletely defined. It is likely all the TMC ligaments act in a coordinated fashion to maintain thumb TMC stability across a large ROM and joint forces. Our understanding of TMC ligamentous anatomy continues to evolve.
The Eaton-Litter ligament reconstruction is the most common and most studied procedure identified in this review and reconstructs the function of both the AOL and DRL. However, many authors [6, 9, 10, 16, 29, 35] have published other techniques that utilize different grafts to reconstruct different TMC ligaments. While ligament reconstruction stabilizes the TMC joint [30], there is currently no evidence that joint stabilization can prevent or retard the development of TMC OA. The Eaton-Littler reconstruction appears to have excellent and durable outcomes in most patients. Authors have consistently shown this procedure reduces pain and improves strength and function in patients with early-stage TMC OA. However, the highest level of clinical evidence for ligament reconstruction is Level IV case series. During our systematic review, we identified no papers discussing DRL reefing as an alternative and isolated treatment for instability or early-stage TMC OA. However, after submission of this manuscript, a surgical technique paper was published on DRL reefing [46]. This is a potential area where future research is needed. Tightening or advancing the DRL on either the metacarpal or trapezial side is an intriguing method of improving joint stability without complicated tendon weaves and grafts. Whether this procedure will relieve pain and improve function depends on the outcome of pending clinical studies.
Thumb metacarpal osteotomy appears to have excellent and durable outcomes. The mechanism by which it works is believed to be a combination of shifting the contact area and tightening of the dorsal ligaments when the thumb is placed into the lateral pinch position.
Over the past two decades, our understanding of TMC ligamentous anatomy has evolved, with most recent authors designating the dorsal ligaments as the primary stabilizers of the TMC joint. Ligament reconstruction and metacarpal osteotomy ameliorate TMC ligamentous laxity and relieve pain based on Level IV studies.
References
Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19:340–341.
Aune S. Osteo-arthritis in the first carpo-metacarpal joint; an investigation of 22 cases. Acta Chir Scand. 1955;109:449–456.
Badia A, Khanchandani P. Treatment of early basal joint arthritis using a combined arthroscopic debridement and metacarpal osteotomy. Tech Hand Up Extrem Surg. 2007;11:168–173.
Bettinger PC, Linscheid RL, Berger RA, Cooney WP 3rd, An KN. An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint. J Hand Surg Am. 1999;24:786–798.
Bettinger PC, Smutz WP, Linscheid RL, Cooney WP 3rd, An KN. Material properties of the and trapeziometacarpal ligaments. J Hand Surg Am. 2000;25:1085–1095.
Biddulph SL. The extensor sling procedure for an unstable carpometacarpal joint. J Hand Surg Am. 1985;10:641–645.
Bojsen-Moller F. Osteoligamentous guidance of the movements of the human thumb. Am J Anat. 1976;147:71–80.
Botelheiro JC. Trapeziometacarpal instability treated with modified Brunelli ligamentoplasty. J Hand Surg Br. 2001;26:145–147.
Brunelli G, Monini L, Brunelli F. Stabilisation of the trapezio-metacarpal joint. J Hand Surg Br. 1989;14:209–212.
Cho KO. Translocation of the abductor pollicis longus tendon: a treatment for chronic subluxation of the thumb carpometacarpal joint. J Bone Joint Surg Am. 1970;52:1166–1170.
Colman M, Mass DP, Draganich LF. Effects of the deep anterior oblique and dorsoradial ligaments on trapeziometacarpal joint stability. J Hand Surg Am. 2007;32:310–317.
Doerschuk SH, Hicks DG, Chinchilli VM, Pellegrini VD Jr. Histopathology of the palmar beak ligament in trapeziometacarpal osteoarthritis. J Hand Surg Am. 1999;24:496–504.
Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9:692–699.
Eaton RG, Littler JW. A study of the basal joint of the thumb: treatment of its disabilities by fusion. J Bone Joint Surg Am. 1969;51:661–668.
Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655–1666.
Eggers GW. Chronic dislocation of the base of the metacarpal of the thumb. J Bone Joint Surg. 1945;27:500–501.
Freedman DM, Eaton RG, Glickel SZ. Long-term results of volar ligament reconstruction for symptomatic basal joint laxity. J Hand Surg Am. 2000;25:297–304.
Futami T, Kobayashi A, Ukita T, Fujita T. Abduction-opposition wedge osteotomy of the base of the first metacarpal for thumb basal joint arthritis. Tech Hand Up Extrem Surg. 1998;2:110–114.
Futami T, Nakamura K, Shimajiri I. Osteotomy for trapeziometacarpal arthrosis: 4 (1–6) year follow-up of 12 cases. Acta Orthop Scand. 1992;63:462–464.
Haara MM, Heliövaara M, Kroger H, Arokoski JP, Manninen P, Kärkkäinen A, Knekt P, Impivaara O, Aromaa A. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86:1452–1457.
Hagert E, Lee J, Ladd AL. Innervation patterns of thumb trapeziometacarpal joint ligaments. J Hand Surg Am. 2012;37:706–714.e1.
Haines RW. The mechanism of rotation at the first carpo-metacarpal joint. J Anat. 1944;78:44–46.
Harvey FJ, Bye WD. Bennett’s fracture. Hand. 1976;8:48–53.
Hirata H, Nakao E. Anatomical ligament reconstruction for trapeziometacarpal osteroarthritis. Nagoya J Med Sci. 2007;69:1–7.
Hobby JL, Lyall HA, Meggitt BF. First metacarpal osteotomy for trapeziometacarpal osteoarthritis. J Bone Joint Surg Br. 1998;80:508–512.
Imaeda T, An KN, Cooney WP 3rd, Linscheid R. Anatomy of trapeziometacarpal ligaments. J Hand Surg Am. 1993;18:226–231.
Imaeda T, Niebur G, An KN, Cooney WP 3rd. Kinematics of the trapeziometacarpal joint after sectioning of ligaments. J Orthop Res. 1994;12:205–210.
Imaeda T, Niebur G, Cooney WP, Linscheid RL, An KN. Ligament length during circumduction of the trapeziometacarpal joint. J Orthop Sci. 1997;2:319–327.
Kestler OC. Recurrent dislocation of the first carpometacarpal joint repaired by functional tenodesis. J Bone Joint Surg Am. 1946;28:858–861.
Koff MF, Shrivastava N, Gardner TR, Rosenwasser MP, Mow VC, Strauch RJ. An in vitro analysis of ligament reconstruction or extension osteotomy on trapeziometacarpal joint stability and contact area. J Hand Surg Am. 2006;31:429–439.
Ladd AL, Lee J, Hagert E. Macroscopic and microscopic analysis of the thumb carpometacarpal ligaments: a cadaveric study of ligament anatomy and histology. J Bone Joint Surg Am. 2012;94:1468–1477.
Lane LB, Eaton RG. Ligament reconstruction for the painful “prearthritic” thumb carpometacarpal joint. Clin Orthop Relat Res. 1987;220:52–57.
Lane LB, Henley DH. Ligament reconstruction of the painful, unstable, nonarthritic thumb carpometacarpal joint. J Hand Surg Am. 2001;26:686–691.
Lubahn J, Ivance D, Konieczko E, Cooney T. Immunohistochemical detection of relaxin binding to the volar oblique ligament. J Hand Surg Am. 2006;31:80–84.
Michele AA, Skinner HL, Krueger FJ. Repair and stabilization of the first carpometacarpal joint. Am J Surg. 1950;79:348, illust.
Molitor PJ, Emery RJ, Meggitt BF. First metacarpal osteotomy for carpo-metacarpal osteoarthritis. J Hand Surg Br. 1991;16:424–427.
Najima H, Oberlin C, Alnot JY, Cadot B. Anatomical and biomechanical studies of the pathogenesis of trapeziometacarpal degenerative arthritis. J Hand Surg Br. 1997;22:183–188.
Nanno M, Buford WL Jr, Patterson RM, Andersen CR, Viegas SF. Three-dimensional analysis of the ligamentous attachments of the first carpometacarpal joint. J Hand Surg Am. 2006;31:1160–1170.
Napier JR. The form and function of the carpo-metacarpal joint of the thumb. J Anat. 1955;89:362–369.
Pagalidis T, Kuczynski K, Lamb DW. Ligamentous stability of the base of the thumb. Hand. 1981;13:29–35.
Parker WL, Linscheid RL, Amadio PC. Long-term outcomes of first metacarpal extension osteotomy in the treatment of carpal-metacarpal osteoarthritis. J Hand Surg Am. 2008;33:1737–1743.
Pellegrini VD Jr. Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. J Hand Surg Am. 1991;16:967–974.
Pellegrini VD Jr, Olcott CW, Hollenberg G. Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament. J Hand Surg Am. 1993;18:238–244.
Pellegrini VD Jr, Parentis M, Judkins A, Olmstead J, Olcott C. Extension metacarpal osteotomy in the treatment of trapeziometacarpal osteoarthritis: a biomechanical study. J Hand Surg Am. 1996;21:16–23.
Pieron AP. The mechanism of the first carpometacarpal (CMC) joint: an anatomical and mechanical analysis. Acta Orthop Scand Suppl. 1973;148:1–104.
Rayan G, Do V. Dorsoradial capsulodesis for trapeziometacarpal joint instability. J Hand Surg Am. 2013;38:382–387.
Roberts SN, Brown JN, Hayes MG, Saies A. The early results of the Brunelli procedure for trapeziometacarpal instability. J Hand Surg Br. 1998;23:758–761.
Shrivastava N, Koff MF, Abbot AE, Mow VC, Rosenwasser MP, Strauch RJ. Simulated extension osteotomy of the thumb metacarpal reduces carpometacarpal joint laxity in lateral pinch. J Hand Surg Am. 2003;28:733–738.
Slocum DB. Stabilization of the articulation of the greater multangular and the first metacarpal. J Bone Joint Surg. 1943;25:626–630.
Strauch RJ, Behrman MJ, Rosenwasser MP. Acute dislocation of the carpometacarpal joint of the thumb: an anatomic and cadaver study. J Hand Surg Am. 1994;19:93–98.
Takwale VJ, Stanley JK, Shahane SA. Post-traumatic instability of the trapeziometacarpal joint of the thumb: diagnosis and the results of reconstruction of the beak ligament. J Bone Joint Surg Br. 2004;86:541–545.
Tan J, Xu J, Xie RG, Deng AD, Tang JB. In vivo length and changes of ligaments stabilizing the thumb carpometacarpal joint. J Hand Surg Am. 2011;36:420–427.
Tomaino MM. Treatment of Eaton Stage I trapeziometacarpal disease with thumb metacarpal extension osteotomy. J Hand Surg Am. 2000;25:1100–1106.
Van Brenk B, Richards RR, Mackay MB, Boynton EL. A biomechanical assessment of ligaments preventing dorsoradial subluxation of the trapeziometacarpal joint. J Hand Surg Am. 1998;23:607–611.
Van Giffen N, Van Ransbeeck H, De Smet L. Stabilization of the pre-arthritic trapeziometacarpal joint using ligament reconstruction. Chir Main. 2002;21:277–281.
Weitbrecht J. Syndesmology (1742). Philadelphia: WB Saunders; 1969.
Wilson JN. Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal joint of the thumb. Br J Surg. 1973;60:854–858.
Wilson JN, Bossley CJ. Osteotomy in the treatment of osteoarthritis of the first carpometacarpal joint. J Bone Joint Surg Br. 1983;65:179–181.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Lin, J.D., Karl, J.W. & Strauch, R.J. Trapeziometacarpal Joint Stability: The Evolving Importance of the Dorsal Ligaments. Clin Orthop Relat Res 472, 1138–1145 (2014). https://doi.org/10.1007/s11999-013-2879-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2879-9