Abstract
Background
Several strategies for the treatment of pathologic proximal femur fractures are practiced but treatment outcomes have not been rigorously compared.
Questions/purposes
Major variations in the use of intramedullary fixation, extramedullary/plate-screw fixation, and endoprosthetic reconstruction techniques for pathologic proximal femur fractures in patients with skeletal metastases are reported. The clinical and surgical variables that influence this choice differ among treating surgeons. To characterize the technique preferences and to identify areas of consensus regarding specific clinical presentations, we administered an online survey to the Musculoskeletal Tumor Society (MSTS) membership. We also tested whether responses correlated with the respondents’ years in practice and asked about the indications for wide tumor resection and the role of tumor debulking and adjuvant cementation.
Methods
A 10-minute, web-based survey was sent via email to 244 MSTS members. The survey queried participants’ musculoskeletal oncology training and experience and presented case scenarios illustrating different combinations of four variables that influence decision-making: cancer type, estimated patient survival, fracture displacement, and anatomic region of involvement.
Results
Forty-one percent (n = 98) of MSTS members completed the survey. Intramedullary nail fixation (IMN; 45%) and proximal femur resection and reconstruction (34%) were the most commonly recommended techniques followed by long-stem cemented hemiarthroplasty/cemented hemiarthroplasty (15%) and open reduction and internal fixation (7%). Most respondents (56%) recommended use of cementation with IMN. Differences of opinion on recommended treatment were associated with variations in cancer type, fracture displacement, and anatomic region of involvement.
Conclusions
Our online survey showed a trend among MSTS members for selecting IMN and arthroplasty-related techniques to treat pathologic fractures of the proximal femur, but major differences in preferred operative technique exist. Prospective studies are needed to develop consistent, evidence-based treatment recommendations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathologic proximal femur fractures are a leading cause of morbidity in patients with skeletal metastases [16]. Operative strategies for the treatment of pathologic proximal femur fractures include the use of intramedullary fixation (IMN) [13, 19], extramedullary, plate-screw fixation (open reduction and internal fixation [ORIF]) [5], and endoprosthetic reconstruction (proximal femur resection reconstruction [PFRR] or long-stem cemented hemiarthroplasty/cemented hemiarthroplasty [LSCH/CH]) [9, 19]. Retrospective data support the use of each approach, but few attempts have been made to rigorously compare treatment outcomes [15, 19]. An extensive list of patient- or treatment-related factors often is considered when selecting an operative strategy and includes estimated patient survival, the necessity of a separate tumor resection procedure, the method of tumor resection (eg, intralesional versus wide resection), sensitivity of the lesion to radiation therapy or chemotherapy, baseline health and performance status, type of cancer, the extent of osseous and/or visceral metastasis, anatomic region(s) of femoral involvement, and the perceived risk of procedure-specific complications.
Given the substantial number of factors that must be considered when treating pathologic proximal femur fractures, it is not surprising that clinical and surgical variables are prioritized differently among treating surgeons. In fact, major variations in practice currently exist among members of the Musculoskeletal Tumor Society (MSTS). The lack of prospective analyses makes it impossible to take an evidence-based decision-making approach. Improving patient outcomes through the conduct of comparative effectiveness research continues to be a stated research priority of the MSTS. Thus, we aimed to characterize the opinions of the MSTS membership with respect to the surgical treatment of pathologic proximal femur fractures through administration of an online survey. The analysis of qualitative data on current practices among MSTS members can inform the development of future research priorities and establish evidence-based recommendations on the treatment of pathologic proximal femur fractures.
The purposes of our survey study were to determine where consensus lies with respect to specific clinical presentations and examine whether treatment preferences correlated with the extent of the respondent’s surgical oncology experience. We also tested whether responses correlated with the respondent’s years in practice and asked about the indications for wide tumor resection and the role of tumor debulking and adjuvant cementation.
Patients and Methods
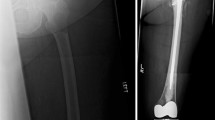
We constructed an online survey using a commercial, web-based application (QuestionPro®; QuestionPro Inc, Seattle, WA, USA). Aggregated data were stored electronically by the authors (MS, JHH) using the website’s proprietary software. The first four survey questions asked for information regarding surgeon demographics (eg, years of experience, fellowship training, practice setting). The following 20 questions elicited recommendations for optimal surgical treatment of hypothetical clinical scenarios. (Survey questions are presented in the Appendix; supplemental materials are available with the online version of CORR ®.) Responses were indicated for each question using a mouse-based, point-and-click format. All multiple-choice questions were presented on two scroll-down pages. We performed completeness checks before and after survey submission to the MSTS membership. The first 18 individual case scenarios were constructed by combining four categorical variables selected by the working group as having a major influence on surgical decision-making: cancer type, estimated patient survival, fracture displacement, and anatomic region of involvement (Table 1). The first variable, cancer type, included two cancers considered to have a differential response to radiation therapy: breast carcinoma metastasis (BrCA), which typically responds favorably to radiation therapy, and conventional renal cell carcinoma metastasis (RCC), which exhibits an intermediate response to radiation therapy. The second variable, estimated survival, was defined as a period greater than or less than 6 months. The third variable, fracture displacement, was categorized as no or minimal radiographic evidence of displacement (ie, impending fracture) versus overt fracture displacement. To ensure that the survey respondents interpreted fracture displacement correctly, we explicitly stated the degree of displacement in the case narrative and showed it in corresponding radiographs. The fourth variable, anatomic region of involvement, was shown radiographically, and lesions were classified according to their location in either the intertrochanteric/pertrochanteric region or the subtrochanteric/pertrochanteric region. Lesions occupying portions of the femoral neck or isolated diaphyseal lesions were not presented. We included two additional questions to gauge survey responders’ management of pathologic proximal femur fractures associated with soft tissue masses and to characterize the use of adjunctive tumor excision and cement augmentation procedures when treating pathologic proximal femur fractures with intramedullary fixation. Open-text fields for user feedback on the content and design were included at the end of the survey.
We performed a preliminary field test to validate the feasibility of the survey format and to ensure that participants could complete the survey in 10 minutes or less. Two requests for participation were sent via email to the 244 active members of MSTS. No other means of advertising the survey were used. During the course of 8 weeks, 98 respondents completed the survey in an average of 9 minutes. We collected data in a deidentified manner and reported the data in the aggregate from completed surveys only. Baseline information regarding the practice setting and experience of the survey responders are included (Table 2).
Results
An overall trend toward selection of intramedullary fixation and arthroplasty-related surgical techniques was found (Fig. 1A). Individual variables also were associated with specific treatment preferences. With respect to cancer type, IMN and LSCH/CH were recommended more frequently in the context of BrCA versus RCC (p < 0.05) (Fig. 1B). For patients with estimated survival less than 6 months, respondents favored IMN over other methods, but the consensus was less clear for patients with longer estimated survival (Fig. 1C). For the variable fracture displacement, a significant increase (p < 0.05) in the recommended use of IMN and ORIF was seen for impending pathologic fractures, whereas PFRR was recommended more often for a displaced fracture (Fig. 1D). With respect to anatomic region of involvement, IMN was recommended more often for lesions of the subtrochanteric/pertrochanteric region (p < 0.05), whereas LSCH/CH was recommended more often for the treatment of intertrochanteric/pertrochanteric lesions (Fig. 1E). Despite individual differences in the recommended operative strategies for each survey variable, the overall trend favoring intramedullary fixation and arthroplasty-related techniques was consistent on the whole.
(A) Completed survey responses were combined with respect to the frequency of operative strategy selection and recorded as percentages. Shown are the percentages for breakdown of total responses by (B) cancer type, (C) estimated survival, (D) fracture displacement, and (E) anatomic region of involvement. An asterisk indicates a statistically significant difference (p < 0.05) for individual group comparisons (Mann-Whitney U test).
Next, we attempted to determine whether the experience of the survey responder influenced corresponding treatment recommendations (Table 3). Looking specifically at the variable fracture displacement, relative concordance among responders was observed for treatment recommendations in the setting of RCC regardless of experience (Table 3). Conversely, surgeons with less than 10 years of experience were more likely to recommend IMN (61%) versus PFRR (34%) for BrCA-related fractures, whereas surgeons with greater than 10 years of experience were more likely to recommend PFRR (51%) versus IMN (29%).
In a separate series of questions, a clinical scenario was proposed describing a patient with widespread metastases and a large, associated soft tissue mass. Survey participants were instructed to recommend (1) an optimal operative strategy in light of varied estimated survival (< 6 months or > 6 months) (Fig. 2); and (2) assign a size threshold above which wide resection should be performed assuming an estimated survival greater than 6 months. IMN was the preferred method of surgical treatment when estimated survival was less than 6 months (IMN = 76%; PFRR = 25%; ORIF = 2%; LSCH = 1%). With an estimated survival greater than 6 months, IMN and PFRR were recommended equally (49% and 48%, respectively) (ORIF = 3%; LSCH = 0%). The minimum size threshold for wide resection varied substantially among respondents with approximately equal distribution of responses given for lesions of 3 cm, 5 cm, 8 cm, and greater than 10 cm (Fig. 3). This question also provided an option of selecting a technique other than wide resection. Fifty-three percent of respondents selected an alternative strategy (Fig. 3).
Survey responders were asked to select an operative strategy for treating an impending pathologic fracture associated with a large soft tissue mass. In this scenario, the patient had a diagnosis of widely metastatic renal cell carcinoma. Responses were recorded for an estimated survival of (A) less than 6 months and (B) greater than 6 months.
Survey participants were asked to make specific recommendations regarding the use of adjunctive tumor excision and cement augmentation procedures (Table 4). In approximately 1/3 of the responses (35%), intramedullary fixation was performed alone without adjunctive procedures. Use of cementation after tumor excision was reported by 56% of respondents, whereas the use of tumor excision without cementation was infrequent (3%). Survey participants also indicated a preference for application of cement after intramedullary nail insertion (44% of total responses) over preinjection of cement just before nail insertion (11% of total responses).
Discussion
Investigation of optimal treatment strategies for pathologic proximal femur fractures continues to be a stated research priority of the MSTS. To foster progress toward this goal, we used a survey-based approach to characterize opinions of the MSTS membership regarding current practice. These opinions are critically important for developing much-needed prospective studies in this area. Our survey results confirm that MSTS surgeons currently use a diversity of surgical approaches to treat pathologic proximal femur fractures and that the four factors included in the survey influence surgeons’ decision-making.
Our study has some potential limitations. The survey results do not necessarily support claims of efficacy regarding individual operative strategies, but rather reflect the opinions of MSTS members regarding use of these strategies in the context of a limited number of simplified clinical scenarios. For this reason, the survey responses specific to presentations of breast and kidney cancer should not be extrapolated to treatment scenarios for less common diagnoses such as thyroid and prostate cancer. More thorough information about the indications for and variations of adjunctive treatments would be desirable. We chose to minimize responder burden to maximize the quantity and quality of responses. It gives only superficial answers to the question about how these methods are used in current practice. Further work is needed to draw definitive conclusions about the role of these techniques in the management of metastatic bone disease. The optimal surgical treatment of pathologic proximal femur fractures requires nuanced clinical judgment, taking into account multiple patient- and treatment-related factors. It also is dependent on an adequate body of supporting literature that allows for an evidence-based, decision-making approach. Additionally, only 41% (n = 98 of 244) of the membership provided complete responses. Our survey response rate is comparable to those reported in the survey literature at large. In a review of 1607 studies published in 17 peer-reviewed academic journals during a 5-year period (2000–2005), 490 different studies used surveys. Survey responses were recorded from more than 400,000 individuals representing the research interests of more than 100,000 organizations. The average response rate among these studies was 35.7% (SD, ± 18.8) [1]. One inherent problem in the validity of analyses of Internet-based surveys is the possibility that the surveys never reach the intended recipients. Failure to properly transmit survey invitations often can result from the use of conservative filtering software settings by recipients or account inactivity. These factors and others affect the denominator estimates used to calculate the percent survey response [6]. To disseminate our survey, we obtained email addresses from the MSTS membership directory, but we did not attempt to confirm the activity status of each email account. Because we presumed 100% success in email transmission of the surveys, our percent survey response may be understated.
We reviewed the peer-reviewed literature from 1980 through 2011 and found 14 articles describing outcomes for IMN, PFRR, LSCH/CH, and ORIF in patients treated for femoral metastases. Notably, few studies examined proximal femur fractures specifically, and 14 of 15 studies were retrospective, citing either a retrospective cohort (Level of Evidence IV) or retrospective comparison design (Level of Evidence III) (Table 5) [2, 4, 5, 7–15, 18–20]. A single, prospective study (Level I) was found that showed functional improvement in patients undergoing surgery for nonspinal bone metastases [17], but outcomes specific to the proximal femur were not reported. Furthermore, detailed reporting of treatment covariates (eg, use of radiation therapy, cement augmentation of IMN) in these studies was inconsistent as was the incorporation of validated assessment tools from which study-to-study comparisons could be drawn. Thus, quality data are severely lacking for comparisons of operative strategies (IMN, PFRR, LSCH/CH, and ORIF).
Survey responder demographics, including years of experience, fellowship training, and percentage of practice dedicated to orthopaedic oncology, were representative of the MSTS as a whole and suggest that our study respondents comprise a relevant sample for our analysis. Accordingly, we report a consistent trend among survey respondents for selecting IMN and arthroplasty-related techniques (PFRR and LSCH/CH) for the treatment of pathologic proximal femur fractures. ORIF was recommended less frequently but was consistently chosen in each clinical scenario. The variables cancer type, estimated patient survival, fracture displacement, and anatomic region of involvement were selected by the working group as factors that heavily influence surgical decision-making. Consistent with this observation, statistically significant differences in operative strategy selection were noted in each of the variable-specific analyses with the exception of estimated survival. Survival estimate did, however, appear to influence responses for a displaced fracture in which IMN was recommended more often when estimated survival was less than 6 months and equaled PFRR when estimated survival was greater than 6 months. The results of this study may have differed if we sampled opinions regarding the treatment of patients with other durations of predicted survival. Furthermore, opinions regarding treatment strategies might change significantly if new therapies substantively change the prognosis of patients with breast or renal metastases to bone.
The barriers to performing research on patients with skeletal metastases are well characterized [3, 17]. Many of these barriers are intrinsic to the patient population being studied. However, several factors in the collective reach of the MSTS have not been addressed adequately, particularly with respect to the development of validated outcome measurement tools for pathologic fracture research, refinement of current methodologic approaches, and establishing multicenter collaborative teams through which high-quality prospective investigations can be performed.
Pathologic proximal femur fractures are a common presentation in orthopaedic oncology, for which an evidence-based treatment approach is lacking. A major difference of opinion currently exists among members of the MSTS in determining the optimal surgical strategy. Despite the heterogeneity of the patient population affected by pathologic proximal femur fractures, the MSTS, through its research initiatives and the participation of its members, can provide the appropriate and much-needed prospective data to determine the optimal use of IMN, PFRR, LSCH/CH, and ORIF.
References
Baruch Y, Haltom BC. Survey response rate levels and trends in organizational research. Hum Relations. 2008;61:1139–1160.
Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108–112.
Cheng EY. Prospective quality of life research in bony metastatic disease. Clin Orthop Relat Res. 2003;415(suppl):S289–S297.
Clarke HD, Damron TA, Sim FH. Head and neck replacement endoprosthesis for pathologic proximal femoral lesions. Clin Orthop Relat Res. 1998;353:210–217.
Dijstra S, Wiggers T, van Geel BN, Boxma H. Impending and actual pathological fractures in patients with bone metastases of the long bones: a retrospective study of 233 surgically treated fractures. Eur J Surg. 1994;160:535–542.
Dobrow MJ, Orchard MC, Golden B, Holowaty E, Paszat L, Brown AD, Sullivan T. Response audit of an Internet survey of health care providers and administrators: implications for determination of response rates. J Med Internet Res. 2008;10:e30.
Finstein JL, King JJ, Fox EJ, Ogilvie CM, Lackman RD. Bipolar proximal femoral replacement prostheses for musculoskeletal neoplasms. Clin Orthop Relat Res. 2007;459:66–75.
Harvey N, Ahlmann ER, Allison DC, Wang L, Menendez LR. Endoprostheses last longer than intramedullary devices in proximal femur metastases. Clin Orthop Relat Res. 2012;470:684–691.
Lane JM, Sculco TP, Zolan S. Treatment of pathological fractures of the hip by endoprosthetic replacement. J Bone Joint Surg Am. 1980;62:954–959.
Manoso MW, Frassica DA, Lietman ES, Frassica FJ. Proximal femoral replacement for metastatic bone disease. Orthopedics. 2007;30:384–388.
Potter BK, Chow VE, Adams SC, Letson GD, Temple HT. Endoprosthetic proximal femur replacement: metastatic versus primary tumors. Surg Oncol. 2009;18:343–349.
Randall RL, Aoki SK, Olson PR, Bott SI. Complications of cemented long-stem hip arthroplasties in metastatic bone disease. Clin Orthop Relat Res. 2006;443:287–295.
Sarahrudi K, Greitbauer M, Platzer P, Hausmann JT, Heinz T, Vecsei V. Surgical treatment of metastatic fractures of the femur: a retrospective analysis of 142 patients. J Trauma. 2009;66:1158–1163.
Selek H, Başarir K, Yildiz Y, Sağlik Y. Cemented endoprosthetic replacement for metastatic bone disease in the proximal femur. J Arthroplasty. 2008;23:112–117.
Steensma M, Boland PJ, Morris CD, Athanasian E, Healey JH. Endoprosthetic treatment is more durable for pathologic proximal femur fractures. Clin Orthop Relat Res. 2012;470:920–926.
Swanson KC, Pritchard DJ, Sim FH. Surgical treatment of metastatic disease of the femur. J Am Acad Orthop Surg. 2000;8:56–65.
Talbot M, Turcotte RE, Isler M, Normandin D, Iannuzzi D, Downer P. Function and health status in surgically treated bone metastases. Clin Orthop Relat Res. 2005;438:215–220.
Ward WG, Holsenbeck S, Dorey FJ, Spang J, Howe D. Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res. 2003;415(suppl):S230–S244.
Wedin R, Bauer HC. Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail? J Bone Joint Surg Br. 2005;87:1653–1657.
Yazawa Y, Frassica FJ, Chao EY, Pritchard DJ, Sim FH, Shives TC. Metastatic bone disease: a study of the surgical treatment of 166 pathologic humeral and femoral fractures. Clin Orthop Relat Res. 1990;251:213–219.
Acknowledgments
We thank Richard Terek MD, Edward Chang MD, members of the MSTS Research Committee, and the volunteers who answered the pilot and definitive questionnaires. We thank Jesse Galle for structuring and collating the questionnaire and Rosalind Simmons for editorial assistance at each stage of manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors received funding from the Orthopaedic Research and Education Fund (MS, JHH) and from a major donor to Memorial Sloan-Kettering Cancer Center, New York, NY, USA (MS).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Steensma, M., Healey, J.H. Trends in the Surgical Treatment of Pathologic Proximal Femur Fractures Among Musculoskeletal Tumor Society Members. Clin Orthop Relat Res 471, 2000–2006 (2013). https://doi.org/10.1007/s11999-012-2724-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2724-6