Abstract
Background
Developing a high-efficiency operating room (OR) for total joint arthroplasty (TJA) in an academic setting is challenging given the preexisting work cultures, bureaucratic road blocks, and departmental silo mentalities. Also, academic institutions and aligned surgeons must have strategies to become more efficient and productive in the rapidly changing healthcare marketplace to ensure future financial viability.
Questions/purposes
We identified specific resources and personnel dedicated to our OR for TJA, assessed the typical associated work process delays, and implemented changes and set goals to improve OR efficiencies, including more on-time starts and shorter turnover times, to perform more TJA cases per OR. We then compared these variables before and after project initiation to determine whether our goals were achieved.
Methods
We gathered 1 year of retrospective TJA OR time data (starting, completion, turnover times) and combined these data with 1 month of prospective observations of the workflow (patient check-in, patient processing and preparation, OR setup, anesthesia, surgeon behaviors, patient pathway). The summarized information, including delays and inefficiencies, was presented to a multidisciplinary committee of stakeholders; recommendations were formulated, implemented, and revised quarterly. Key strategies included dedicated OR efficiency teams, parallel processing, dedicated hospital resources, and modified physician behavior. OR data were gathered and compared 3 years later.
Results
After project changes, on-time OR starts increased from less than 60% to greater than 90% and average turnover time decreased from greater than 60 minutes to 35 minutes. Our average number of TJA cases per OR increased by 29% during the course of this project.
Conclusions
Our project achieved improved OR efficiency and productivity using strategies such as process and resource analysis, improved communication, elimination of silo mentalities, and team work.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Given the current US healthcare environment of unsustainable growth and escalating costs, surgeons and their respective hospitals are under heightened pressure and scrutiny to document and implement evidence-based care with efficient, reproducible, safe, high-value, uncomplicated results for patients. Within this context, the operating room (OR) represents an important hospital resource for increased clinical productivity, but with high associated costs [2, 9]. Traditionally, academic medical centers, with their inherent additional missions of education and research, have been branded as unnecessarily expensive, inefficient healthcare organizations with known difficulties in adapting to a hypercompetitive market [6]. Within the current healthcare market, THA and TKA procedures have documented increasing demands (demographically and technologically driven), increasing volumes and costs, and decreasing reimbursements, but with positive hospital profit margins when they are performed with standardized processes by expert surgeons in high-volume institutions [1, 5, 10–13]. Thus, a model for a high-efficiency OR for total joint arthroplasty (TJA) is critical for aligning surgeons and hospitals in planning for future growth, increasing market share, and the overall financial viability of this service line particularly at an academic medical center.
Other academic institutions have recognized the need for improved OR efficiency and have successfully implemented applicable strategies [2–4, 7–9, 12]. In pursuing greater efficiency, we considered and embraced many of the published techniques, eg, detailed process and resource assessment, parallel processing, and high-efficiency teams, to achieve our goals.
We then analyzed our TJA OR work flow, determined the potentially correctable inefficiencies, discussed and agreed on our strategies for improvement, and then implemented the changes, with ongoing reviews to document our progress, successes, and failures. We compared the following data before and 3 years after project initiation to determine whether our goals were achieved: (1) starting time, (2) number of TJA procedures completed per OR block of time, (3) turnover time, (4) number of TJA cases per OR, (5) length of hospital stay, and (6) number of inpatients discharged before 1 PM.
Materials and Methods
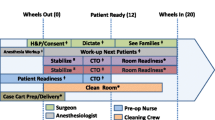
Our project started in 2007 with detailed analyses utilized at other academic institutions of the specific personnel, resources, and processes directly and indirectly involved with an average block of time in our TJA OR (10–12 hours; 7 AM to 7 PM on weekdays except for Wednesdays, 8:30 AM to 7 PM), so we could fully understand our starting point [2, 9]. This required an interdisciplinary assessment team, consisting of TJA physicians, anesthesiologists, OR nurses, and support personnel, sterile processing, postanesthesia and intermediate care, and hospital administrators. The team was led by hospital personnel trained as Six Sigma Black Belts (ie, professionals who can explain the Six Sigma business philosophies and principles and apply the DMAIC [define, measure, analyze, improve, control] model) to approach this challenge using change management tools including lean management (ie, streamlining processes by eliminating unnecessary or wasteful steps) [2]. The group gathered all of the initial workflow and performance data and then provided summary analyses for the efficiency committee. The efficiency committee then made suggestions and asked all stakeholders for recommendations on the setting of goals. They also identified essential assets (eg, personnel, recovery room beds) to achieve the goals and obtained data on those assets to initiate and implement the project. The committee collected data on an ongoing basis to implement further efficiencies. We collected 1 year of retrospective OR time stamp data (nurse in OR, patient in OR, procedure start time and completion time, patient out of OR, nurse out of OR), as well as real-time OR observation and patient flow, for the dedicated TJA surgeons. The workflow processes were detailed, summarized, and presented to a multidisciplinary TJA OR efficiency committee with representatives from hospital administration, anesthesiology, nursing (preoperative holding and preparation, OR, recovery room, inpatient ward), and the TJA surgeons (Table 1). Several meetings were required to digest and discuss the findings. The first review of the data outlined the opportunities that existed for us to improve our efficiency and case throughput.
Our initial analysis demonstrated our starting point (Table 2): (1) surgeons were completing two to three primary or one to two revision TJA procedures during a complete block of OR time; (2) on-time starts (patient in the room) occurred less than 60% of the time; (3) the average time for room turnover (from patient to patient) was highly variable, ranging from 60 to 90 minutes and occasionally up to 2 hours; (4) the TJA surgeons averaged 2.35 TJA cases (primary and/or revisions) per OR; (5) more than 60% of the inpatients receiving TJA were not discharged from the hospital until after 1:00 PM; and (6) the average length of stay for patients receiving primary and revision TJA was 3.5 and 4.4 days, respectively.
The primary inefficiency categories for the on-time OR starts were (1) patient related, (2) nurse related, (3) OR related, (4) surgeon related, and (5) anesthesia related (Table 3). The inefficiencies identified in the OR also included variations in the OR support team, variations in room setup, lack of parallel processing, incomplete OR tray processing, and instrumentation availability. OR turnover times were slowed by several factors, including unavailable surgical attendants, delayed movement of the patient from the OR table to the hospital bed, and the holding of recovery rooms. The same inefficiencies described for on-time starts also contributed to longer turnover times. Competition for limited resources with other orthopaedic and nonorthopaedic service lines proved to be a negative contributing factor.
With a microscopic understanding of our typical TJA OR, the stakeholder OR efficiency committee established specific transparent goals and constructive rules of conduct for the implementation of a high-efficiency OR. The desired benchmarks were (1) the creation of scheduling templates for more efficient utilization of the ORs, eg, separation of primary and revision ORs; (2) greater than 90% on-time starts; (3) an average turnover time of less than 45 minutes and decreasing to 30 minutes over time; (4) four to five primary TJAs being performed in an OR more than 50% of the time; and (5) three TJA cases per OR, even with revision surgery, at least ½ of the time, with an overall goal to increase the number of cases by 20% within the designated ORs. Surgeon-specific data were collected and reported to all stakeholders on a monthly basis and then analyzed and discussed by the committee each quarter up to the present time.
One of our first tactics was to implement a scheduling template for each surgeon by using their specific historical OR performance data. This set the stage for increasing OR volume by creating predictable combinations of TJA procedures that could be completed in the allotted amount of block time for each surgeon. The second strategy was the creation of A teams for the high-efficiency TJA OR, with the same OR team (nurse-circulator, scrub technician, room attendant, and additional person for turnover) assigned to individual surgeons, as well as identified anesthesiology teams specifically committed to the success of the project [7, 9, 11, 12]. The third strategy helped establish the culture of parallel processing, which replaced the existing perfunctory serial steps; eg, the patient was not allowed in the OR until the OR team was ready, anesthesia did not start until the surgeon was available, the subsequent patient was not sent for and prepared unless the OR called the request, etc [4]. Steps were also taken to reduce and standardize trays of instruments for primary THA and TKA procedures to cut costs, reduce related preparation times, and avoid unnecessary delays associated with incorrect postings or missing instruments sets. Our fourth priority was to introduce an efficient check-in process at the admissions office, followed by on-time preparation in the preoperative holding area. Patients were contacted the day before and reminded of the time and location at which to report (at least 2 hours before the OR case start time). Hospital personnel and resources were also committed to the project by adding dedicated nursing support and recovery room beds (adjusted to the day’s schedule). Furthermore, efforts were made on the inpatient ward to discharge patients before 11:00 AM to facilitate patient flow through the system, thereby avoiding delays in the recovery room, which could also delay the treatment of patients coming out of the OR. Finally, each attending TJA surgeon, along with his or her assigned orthopaedic resident or fellow, participated in and supported all aspects of the efficiency project by (1) ensuring the completion of paperwork and marking the first patient at least 45 minutes before start; (2) briefing the OR and anesthetic teams about the plans for the day, as well as any potential problems; (3) being in the OR at least 10 minutes before the patient entering the OR; and (4) helping the in-OR processes whenever necessary (moving the patient to the OR table, starting a Foley catheter, helping to position the patient, etc) [8, 11, 12]. Once these initiatives were in place, the committee met monthly to share surgeon-specific reports that included metrics related to each facet of the project. The committee also used this time to openly discuss project successes and new opportunities for process improvement.
We compared the following data before (2007) and 3 years after project initiation (2011) to determine whether our goals were achieved: (1) starting time, (2) number of TJA procedures completed per OR block of time, (3) average turnover time, (4) average number of TJA cases per OR, (5) average length of hospital stay, and (6) number of inpatients discharged before 1 PM.
Results
Our total joint OR efficiency project was able to achieve (1) more on-time starts (> 90% versus < 60%), (2) the completion of four and occasionally five primary TJA procedures per OR block more often (30% versus 0%), (3) a shorter average turnover time (≤ 35 minutes versus 60–120 minutes); (4) a 29% increase in average number of TJA cases per OR (3.04 versus 2.35), (5) shorter average lengths of stay (3.1 days and 3.4 days versus 3.5 days and 4.4 days for primary and revision TJA, respectively), and (6) more inpatients receiving TJA discharged before 1 PM (70% versus 40%) (Table 2). Today, data and project milestones continue to be shared at a quarterly orthopaedic OR efficiency/improvement meeting, as well as at our monthly Total Joint Coordination of Care committee meeting. Many of the process improvements and successes have been shared and translated to other OR service lines within our hospital.
Discussion
Developing a high-efficiency OR for TJA in an academic setting is challenging given the preexisting work cultures, bureaucratic road blocks, and departmental silo mentalities. Also, academic institutions and aligned surgeons must have strategies to become more efficient and productive in the rapidly changing healthcare marketplace to ensure future financial viability. We developed a higher-efficiency TJA OR at our hospital by using constructive team work by all stakeholders; conducting a detailed analysis of our OR workflow, personnel, and processes; and subsequently implementing various strategies successfully used at other similar institutions.
We are aware of limitations to our study and data collection processes. First, this paper reports surgeon-specific observational data only in achieving predefined goals but without any statistical analyses. Second, our experience, while similar to published projects at various academic institutions, may not be entirely applicable to other OR environments or cultures. Third, even though we achieved more on-time OR starts, shorter turnover times, more total TJA cases per OR, and apparent shorter average length of stay, it is not clear these accomplishments were more cost-effective or provided equal or improved results for our patients.
Our project confirms previously published efforts in improving OR efficiency through process and resource analysis [2, 9], improved communication, elimination of silo mentalities, team work [3, 8, 11], and high-efficiency OR teams adapting parallel processing [4, 7].
From a practical standpoint, establishing a high-efficiency TJA OR in our academic setting was dependent on the TJA surgeons aligning with the hospital and its various parts or players in a constructive, fully engaged manner. The surgeons initiated and implemented the proposed changes by bringing the various stakeholders together, requesting the collection and analyses of data, transparently sharing and discussing the information, while respectfully establishing mutually beneficial goals, and then demonstrating an ongoing commitment to the project’s success. More than anything else, the surgeons led by example and followed all of the established rules; failure in this regard would have potentially resulted in project participant apathy and disrespect. The surgeons advocated for success by (1) restating the goals and relevance of the project on a regular basis, (2) transparently sharing and discussing the ongoing collected data, (3) proposing constructive solutions to identified problems, (4) expressing sincere gratitude to the team players every day, (5) decreasing or eliminating barriers to hiring and rewarding high-achieving employees, (6) promoting and participating in alignment projects with the hospital, and (7) looking for new ideas for creating potential value for patients, staff, surgeons, residents, fellows, and the hospital.
References
Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652.
Cima RR, Brown MJ, Hebl JR, Moore R, Rogers JC, Kollengode A, Amstutz GJ, Weisbrod CA, Narr BJ, Deschamps C; Surgical Process Improvement Team, Mayo Clinic, Rochester. Use of lean and Six Sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center. J Am Coll Surg. 2011;213:83–92.
Dexter F, Epstein RH, Traub RD, Xiao Y. Making management decisions on the day of surgery based on operating room efficiency and patient waiting times. Anesthesiology. 2004;101:1444–1453.
Friedman DM, Sokal SM, Chang Y, Berger DL. Increasing operating room efficiency through parallel processing. Ann Surg. 2006;243:10–14.
Healy WL, Rana AJ, Iorio R. Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin Orthop Relat Res. 2011;469:87–94.
Hwang CS, Wichterman KA, Alfrey EJ. The cost of resident education. J Surg Res. 2010;163:18–23.
Leach LS, Myrtle RC, Waver FA, Dasu S. Assessing the performance of surgical teams. Health Care Manage Rev. 2009;34:29–41.
Nundy S, Mukherjee A, Sexton JB, Pronovost PJ, Knight A, Rowen LC, Duncan M, Syin D, Makary MA. Impact of preoperative briefings on operating room delays: a preliminary report. Arch Surg. 2008;143:1068–1072.
Overdyk FJ, Harvey SC, Fishman RL, Shippey F. Successful strategies for improving operating room efficiency at academic institutions. Anesth Analg. 1998;86:896–906.
Rana AJ, Iorio R, Healy WL. Hospital economics of primary THA decreasing reimbursement and increasing cost, 1990–2008. Clin Orthop Relat Res. 2011;469:355–361.
Scott WN, Booth RE Jr, Dalury DF, Healy WL, Lonner JH. Efficiency and economics in joint arthroplasty. J Bone Joint Surg Am. 2009;91(suppl 5):33–36.
Smith MP, Sandberg WS, Foss J, Massoli K, Kanda M, Barsoum W, Schubert A. High-throughput operating room system for joint arthroplasties durably outperforms routine processes. Anesthesiology. 2008;109:25–35.
Tomek IM, Sabel AL, Froimson MI, Muschler G, Jevsevar DS, Koenig KM, Lewallen DG, Naessens JM, Savitz LA, Westrich JL, Weeks WB, Weinstein JN. A collaborative of leading health systems finds wide variations in total knee replacement delivery and takes steps to improve value. Health Affairs (Millwood). 2012;31:1–10.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
About this article
Cite this article
Attarian, D.E., Wahl, J.E., Wellman, S.S. et al. Developing a High-efficiency Operating Room for Total Joint Arthroplasty in an Academic Setting. Clin Orthop Relat Res 471, 1832–1836 (2013). https://doi.org/10.1007/s11999-012-2718-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2718-4