Abstract
Background
Successful treatment of pathologic femur fractures can preserve a patient’s independence and quality of life. The choice of implant depends on several disease- and patient-specific variables; however, its durability must generally match the patient’s estimated life expectancy. Failures do occur, however, it is unclear which implants are associated with greater risk of failure.
Questions/Purposes
We evaluated patients with femoral metastases in whom implants failed to determine (1) the rate of reoperation; (2) the timing of and most common causes for failure; and (3) incidence of perioperative complications and death.
Methods
From a prospectively collected registry, we identified 93 patients operated on for failed treatment of femoral metastases from 1990 to 2010. We excluded five patients who subsequently underwent amputations leaving 88 who underwent salvage procedures. These included intramedullary nails (n = 11), endoprostheses (n = 61), and plate fixation (n = 16). The primary outcome was reoperation after salvage treatment.
Results
Seventeen of the 88 patients (19%) required subsequent reoperation a median of 10 months (interquartile range, 4–14) from the time of salvage surgery: 15 for material failure, one for local progression of tumor, and one for a combination of these. Five patients died within 4 weeks of surgery. Although perioperative complications were higher in the endoprosthesis group and dislocations occurred, overall treatment failures after salvage surgery were lower in the that group (four of 61) compared the group with plate fixation (eight of 16) and intramedullary nail groups (five of 11).
Conclusions
Despite relatively common perioperative complications, salvage using endoprostheses may be associated with fewer treatment failures as compared with internal fixation.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Successful surgical treatment of femoral metastases requires careful consideration of patient- and disease-specific variables [18]. Initial treatment of femoral metastases can relieve pain and maintain quality of life [4, 7]; however, implant durability must be matched with both the biomechanical requirements posed by the lesion as well as the patient’s estimated longevity [19]. Failure (reoperation) rates range from 3.1% to 42% for the few patients with cancer who survive more than 1 year after fixation for pathological fracture [16–18]. As more patients with skeletal metastases live longer [1, 14], more implants are at risk for failure [19]. The causes for and treatment options available to failed cases have received some attention in the literature [11, 13, 16, 19]. However, these studies do not describe the subsequent course of these patients.
The purpose of this study was to evaluate patients with femoral metastases in whom constructs failed to determine (1) the rate of reoperation for any reason; (2) the timing of and most common causes for failure; and (3) incidence of other complications, not requiring surgery, and perioperative death.
Patients and Methods
From the prospectively collected Karolinska Skeletal Metastasis Registry, we identified 93 patients who underwent surgery for failed treatment of femoral metastases between 1990 and 2010. Five patients declined salvage reconstruction and underwent palliative amputations and were excluded, leaving 88 patients who underwent limb salvage procedures. The indications for repeat surgery were: (1) material failure; (2) implant malposition; (3) progression of disease, including local recurrence; and (4) a combination of these.
The contraindications were: (1) patients deemed too ill to undergo surgery; and (2) patients in whom death was imminent. However, during the study time, all patients were surgical candidates and no patients were treated nonoperatively. No patients were lost to followup. At the time of last followup, most (82) patients had died and the remainder were alive with disease, five patients died within the perioperative period, defined as within 4 weeks of surgery (two in the endoprosthesis [EP] group, one in the intramedullary nail [IMN] group, and two in the PLATE group). There were no intraoperative deaths. The minimum followup was 18 days (median, 8 months; interquartile range, 3–22 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Ethical permission was not required to use these registry data.
The most common oncologic diagnoses were breast, kidney, and myeloma, and the majority of patients had generalized skeletal metastases (Table 1). The type of salvage treatment was characterized by one of three general techniques. These included IMNs (n = 11), EPs (n = 61), and plate fixation (PLATE) (n = 16), which also included screw and side-plate devices. We compared age, sex, location within the femur, the type of initial, and final implant used (Table 2). The proportion of perioperative deaths was similar (p = 0.32) across groups.
The index surgical procedure was performed at the Karolinska University Hospital in 49 patients, whereas 39 were referred after failure. All salvage procedures were performed at Karolinska University Hospital. At our center, we approached skeletal metastases of the femur in the manner(s) previously described [18]. Briefly, if en bloc resection was indicated, reconstruction was performed using a modular tumor prosthesis. Lesions confined to the femoral neck were treated with standard or long-stem hemiarthroplasty components. Most cases, however, underwent intralesional curettage before stabilization. We preferred to use antibiotic-impregnated polymethylmethacrylate cement, whenever possible, to augment the construct. A variety of implants and surgical techniques were used in these patients at the discretion of the treating surgeon. We preferred the following implants as a result of availability at our center. In the IMN group, unreamed, locked femoral nails or cephalomedullary devices (both Synthes Stratec Medical, Oberdorf, Switzerland) were used. When plate fixation was performed, a dynamic hip screw or limited contact dynamic compression plate (Synthes Stratec Medical) was used. For those who underwent EP replacement, the Austin Moore hemiarthroplasty (Corin Medical, Cirencester, UK), the Charnley (DePuy, Leeds, UK), and Spectron (Smith & Nephew, Memphis, TN, USA) hip prostheses were used. Modular tumor prostheses (METS; Stanmore, Middlesex UK, and HMRS; Stryker Nordic, Malmo, Sweden) were used after en bloc resections of the distal femur and in cases with massive bone destruction.
Postoperative radiotherapy was used routinely after the index surgical treatment of skeletal metastases; therefore, most patients in this study would have been treated, but detailed information regarding timing, dose, and location was not available in the current registry.
After surgery, patients were discharged from the hospital when clinically appropriate. Each was then seen (either at the Karolinska University Hospital or their referring hospital) at 6 weeks after surgery for physical and radiographic examination. Long-term followup was conducted at regular intervals in conjunction with the patient’s regularly scheduled medical oncology visits in which radiographs were ordered if indicated. In addition, the orthopaedic team performed regular chart reviews to determine if and when patients had complications or required a reoperation.
Outcomes included surgical complications as classified by Dindo et al. [5]. The primary outcome was reoperation after salvage treatment (Grade IIIb). Secondary outcomes were perioperative death (Class V), defined as death within 1 month of surgery, other minor complications not requiring surgery or general anesthesia (Class I, II, or IIIa), and overall survival across treatment groups. We compared means between groups using the Mann-Whitney U test, because continuous variables (age, time to failure after salvage treatment, and the duration of followup) were not normally distributed. Proportions of categorical variables between groups were compared using Fisher’s exact test for variables in which the expected frequency on contingency analysis was less than four (initial fixation method for index procedure, reoperations after salvage treatment) and the chi-square test for the balance of categorical variables (sex, location, and perioperative death). We used logistic regression to evaluate the effect of the type of implant on treatment failure (reoperation after salvage treatment) while controlling for possible confounding variables. We performed survival analysis, censored records at the date of last followup or death, then compared differences between groups using the log-rank assessment. We used JMP© Version 9.0.2 (SAS Institute, Inc, Cary, NC, USA) and two-tailed tests for all statistical analyses.
Results
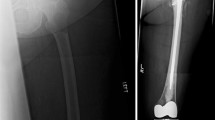
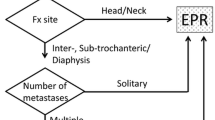
Of the 88 patients requiring salvage treatment after failed reconstructions, 17 required reoperation (Table 2). The median age, duration of followup, and sex distribution were similar between groups. EPs were most commonly performed for proximal (neck, peri- and subtrochanteric) lesions; plate fixation was most commonly performed for distal femoral (metaphyseal and diaphyseal) lesions; and IMNs were performed most commonly in the diaphyseal and subtrochanteric regions. We found a difference (p < 0.001) in the proportion of failures across treatment groups: EP (7%), IMN, (45%), and PLATE (50%) (Fig. 1). There was no correlation between failure and the oncologic diagnosis (p = 0.7). Using logistic regression, we observed an effect of the salvage implant on treatment failure after controlling for age, diagnosis, and location (chi-square = 7.92, DF = 2, p = 0.019) Specifically, the EP group had a lower chance of treatment failure than the PLATE (OR, 0.10; 95% CI, < 0.001 to 0.27) group. The observed odds ratios between EP and IMN and between IMN and PLATE with regard to treatment failure were 0.08 (0.01–1.11) and 0.13 (0.006–2.17), respectively.
Failure occurred at a median time of 10 months (interquartile range, 2–14) from the time of salvage surgery. The most common cause for reoperation was material failure (n = 15) followed by local progression of tumor (n = 1) and a combination of these (n = 1). Failures were most common in the diaphysis (n = 8) followed by subtrochanteric (n = 5), peritrochanteric (n = 2), and distal femoral (n = 2). There were no failures after salvage in the femoral neck region. There were no reoperations for dislocations or infections and no pathologic fractures.
Seventeen patients had perioperative complications that did not require surgery. These included dislocation (n = 6), superficial wound infections (n = 8) as well as systemic (medical) illness (n = 2) or a combination of these (n = 1). The proportion of perioperative complications was higher (p = 0.04) in the EP group.
Discussion
Surgical treatment of femoral metastases can be highly successful in terms of pain relief, maintenance of function, and quality of life. Ideally, implants used should be sufficiently durable to outlast the patient. However, patients with cancer are surviving longer, largely as a result of more effective surgical and adjuvant treatment strategies. The result is a growing population of patients whose femoral implants are at risk for failure. With this in mind, we sought to evaluate patients with femoral metastases in whom constructs failed to determine (1) the rate of reoperation for any reason; (2) the timing of and most common causes for failure; and (3) incidence of other complications, not requiring surgery, and perioperative death.
Readers should be aware of the limitations of our study. First, our review, although retrospective, was performed using a large, prospectively collected registry. In an effort to minimize selection bias, no patient was excluded from analysis. Second, because all salvage surgery was performed at a single institution, by one of nine surgeons, referral, treatment, and institutional biases exist, particularly when one considers the subjective, surgeon-specific component implant selection. As such, these findings may not be applicable to other centers with differing referral bases and treatment philosophies. Nevertheless, the surgical indications for these procedures were quite clear. Third, information regarding the use and timing of radiotherapy was not available nor were data regarding pain relief, functional status, or quality of life. Finally, the duration of followup for the EP group was somewhat shorter when compared with the other two groups (95% CI, −2.1 to 38.0 [EP versus PLATE] and −10.6 to 36.2 [EP versus IMN]). This may underrepresent the number of failures observed in the EP group. These potential confounders and sources of bias are potentially as important as the data reported herein.
We observed a fairly low reoperation rate after salvage of failed femoral implants. Specifically, only four of 61 patients in the EP group required reoperation. Endoprosthetic reconstruction is reportedly more durable than other treatment methods during the initial treatment of femoral metastases [16, 19], although few have described results of salvage treatment in this setting. A notable exception is an article by Jacofsky et al. [8], who reported the results of salvage arthroplasty for failed proximal femoral lesions. The authors reported 90% implant survivorship at 5 years; however, their results apply only to the proximal femur. Our data regarding implant survivorship are comparable, because we observed only two failures in this location (at or proximal to the peritrochanteric region) during the study period. In the EP group, considering all locations within the femur, we observed 85% (95% CI, 62%–94%) survivorship at 5 years, further highlighting the durability of endoprosthetic reconstruction in this patient population.
We observed a median time to failure of 10 months from the time of salvage surgery. This is similar to the results published by Jacofsky et al. [8], who stated “all reoperations occurred within 1 year of the [salvage] procedure.” The authors did not report a median time to failure or perform Kaplan-Meier analysis. Although the observed proportion of failures was much higher, we observed a relatively long median time to failure of 12 months in the IMN group compared with 7 months in the EP group. These results are similar to those previously reported, by our group and others [13, 16], in the primary (not salvage) setting. As such, given the relatively long time to failure, IMNs may be sufficiently durable and, as such, be an acceptable alternative to EP in selected patients with short life expectancies. With this in mind, we observed the expected association between postoperative survival and oncologic diagnosis when grouped in a manner previously described [6]. In the context of diagnoses encountered in this study, breast, renal, myeloma, and prostate (diagnosis Group III) were associated with a median survival of 10 months (interquartile range 4–29) compared with lung (diagnosis Group I) and others (diagnosis Group II) that were associated with 3 months (2–5) and 3 months (2–21), respectively (Table 1).
The rate of perioperative complications was highest in the EP group. Six dislocations (10%) were all treated with closed reduction (Class IIIa). The observed dislocation rate is slightly higher than previously reported 0% to 7% [3, 9, 12, 16, 17]; however, the reported values were after initial and not salvage treatment of femoral lesions and included a subset of patients also treated for primary as opposed to metastatic disease. The dislocation rate in the revision or salvage setting is generally higher even in the nonmetastatic setting [15]. All eight perioperative infections occurred in the EP group and were treated conservatively with antibiotic suppression. There was only one deep infection necessitating débridement without removal of the implant (Class IIIb). The observed infection rate is comparable with several published series in which the overall infection rate was reported as 1% to 10% [8, 17, 19, 20]. We believe local delivery of antibiotics is important to mitigate the risk of infection in these patients.
The majority of these salvage procedures was performed at the end of life. This is evidenced by a median overall survival after surgery of only 8 months (interquartile range, 3–22). Although there were no intraoperative deaths, five patients died during the perioperative period within 30 days of surgery (Fig. 2). When one considers the goal of treating patients with skeletal metastases is to relieve pain and preserve function (and thus quality of life) for the greatest amount of time, careful attention must be paid to each patient’s estimated survival [19]. Endoprosthetic replacement is reportedly more durable [16, 18]; however, less invasive techniques have value. This is especially true in the sick patient in which operative time, blood loss, physiological insult, and rehabilitation requirements should be minimized. As such, we believe that methods to estimate life expectancy in these patients should be used whenever possible [2, 6, 10].
Our data support the use of EPs as a salvage treatment, even at the end of life. With these observations in mind, surgeons must continue to balance the risk of perioperative complications with the benefits that are predicated on each patient’s estimated life expectancy and functional goals. There remains little question regarding the durability of endoprostheses; however, future studies should focus on pain relief, functional status, and quality of life, which are also major considerations in these patients.
References
American Cancer Society global cancer facts and figures. Available at: www.cancer.org/Research/CancerFactsFigures/GlobalCancerFactsFigures/global-facts-figures-2nd-ed. Accessed January 2012.
Bauer HC, Wedin R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop Scand. 1995;66:143–146.
Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009;91:108–112.
Clohisy DR, Le CT, Cheng EY, Dykes DC, Thompson RCJ. Evaluation of the feasibility of and results of measuring health-status changes in patients undergoing surgical treatment for skeletal metastases. J Orthop Res. 2000;18:1–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205.
Forsberg JA, Eberhardt J, Boland PJ, Wedin R, Healey JH. Estimating survival in patients with operable skeletal metastases: an application of a Bayesian belief network. PloS One. 2011;6:e19956.
Harrington KD, Sim FH, Enis JE, Johnston JO, Diok HM, Gristina AG. Methylmethacrylate as an adjunct in internal fixation of pathological fractures. Experience with three hundred and seventy-five cases. J Bone Joint Surg Am. 1976;58:1047–1055.
Jacofsky DJ, Haidukewych GJ, Zhang H, Sim FH. Complications and results of arthroplasty for salvage of failed treatment of malignant pathologic fractures of the hip. Clin Orthop Relat Res. 2004;427:52–56.
Lane JM, Sculco TP, Zolan S. Treatment of pathological fractures of the hip by endoprosthetic replacement. J Bone Joint Surg Am. 1980;62:954–959.
Nathan SS, Healey JH, Mellano D, Hoang B, Lewis I, Morris CD, Athanasian EA, Boland PJ. Survival in patients operated on for pathologic fracture: implications for end-of-life orthopedic care. J Clin Oncol. 2005;23:6072–6082.
Nilsson J, Gustafson P. Surgery for metastatic lesions of the femur: good outcome after 245 operations in 216 patients. Injury. 2008;39:404–410.
Potter BK, Chow VE, Adams SC, Letson GD, Temple HT. Endoprosthetic proximal femur replacement: metastatic versus primary tumors. Surg Oncol. 2009;18:343–349.
Sarahrudi K, Greitbauer M, Platzer P, Hausmann JT, Heinz T, Vecsei V. Surgical treatment of metastatic fractures of the femur: a retrospective analysis of 142 patients. J Trauma. 2009;66:1158–1163.
Schulman KL, Kohles J. Economic burden of metastatic bone disease in the US. Cancer. 2007;109:2334–2342.
Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;467:166–173.
Steensma M, Boland PJ, Morris CD, Athanasian E, Healey JH. Endoprosthetic treatment is more durable for pathologic proximal femur fractures. Clin Orthop Relat Res. 2011;470:920–926.
Ward WG, Holsenbeck S, Dorey FJ, Spang J, Howe D. Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res. 2003;415(Suppl):S230–244.
Wedin R, Bauer HC. Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail? J Bone Joint Surg Br. 2005;87:1653–1657.
Wedin R, Bauer HC, Wersall P. Failures after operation for skeletal metastatic lesions of long bones. Clin Orthop Relat Res. 1999;128–139.
Wedin R, Hansen BH, Laitinen M, Trovik C, Zaikova O, Bergh P, Kalen A, Schwarz-Lausten G, von Steyern FV, Walloe A, Keller J, Weiss RJ. Complications and survival after surgical treatment of 214 metastatic lesions of the humerus. J Shoulder Elbow Surg. 2012;21:1045–1055.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at the Karolinska University Hospital, Stockholm, Sweden.
About this article
Cite this article
Forsberg, J.A., Wedin, R. & Bauer, H. Which Implant Is Best After Failed Treatment for Pathologic Femur Fractures?. Clin Orthop Relat Res 471, 735–740 (2013). https://doi.org/10.1007/s11999-012-2558-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2558-2