Abstract
Background
Accurate reproduction of the preoperative plan at the time of surgery is critical for wide resection of primary bone tumors. Robotic technology can potentially help the surgeon reproduce a given preoperative plan, but yielding control of cutting instruments to a robot introduces potentially serious complications. We developed a novel passive (“haptics”) robot-assisted resection technique for primary bone sarcomas that takes advantage of robotic accuracy while still leaving control of the cutting instrument in the hands of the surgeon.
Questions/Purposes
We asked whether this technique would enable a preoperative resection plan to be reproduced more accurately than a standard manual technique.
Methods
A joint-sparing hemimetaphyseal resection was precisely outlined on the three-dimensionally reconstructed image of a representative Sawbones femur. The indicated resection was performed on 12 Sawbones specimens using the standard manual technique on six specimens and the haptic robotic technique on six specimens. Postresection images were quantitatively analyzed to determine the accuracy of the resections compared to the preoperative plan, which included measuring the maximum linear deviation of the cuts from the preoperative plan and the angular deviation of the resection planes from the target planes.
Results
Compared with the manual technique, the robotic technique resulted in a mean improvement of 7.8 mm of maximum linear deviation from the preoperative plan and 7.9° improvement in pitch and 4.6° improvement in roll for the angular deviation from the target planes.
Conclusions
The haptic robot-assisted technique improved the accuracy of simulated wide resections of bone tumors compared with manual techniques.
Clinical Relevance
Haptic robot-assisted technology has the potential to enhance primary bone tumor resection. Further bench and clinical studies, including comparisons with recently introduced computer navigation technology, are warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Most primary bone sarcomas can be surgically treated with a limb-sparing operation [16, 27, 30]. It is recommended that these tumors be removed by uncontaminated wide resection, in which the entire tumor is removed en bloc along with a surrounding cuff of normal tissue [34]. For uncontaminated wide resection to be successful, an accurate knowledge of the exact extent of tumor involvement before surgery is needed. MRI allows accurate definition of the tumor extent [11, 22, 28, 29]. Thus, based on the preoperative MRI, the surgeon can outline a precise preoperative plan that satisfies the principles of uncontaminated wide resection.
However, the surgeon’s ability to accurately reproduce the preoperative plan at the time of surgery is limited by the tools (eg, flexible metal rulers) and techniques (eg, identification of anatomic landmarks, use of fluoroscopy) that are typically available in the operating room [7, 35]. Consequently, during resection, the surgeon may inadvertently compromise surgical margins or unnecessarily remove large areas of unaffected tissue such as joint surfaces or ligament attachments. Either error is associated with negative consequences: on the one hand, positive surgical margins substantially increase the local recurrence rate [4, 5], which, in turn, dramatically increases the mortality rate [21], and on the other hand, resection of large amounts of normal tissue such as uninvolved joint surfaces requires joint-replacing reconstructions (either prosthetic or allograft) that have limited durability compared with nonjoint-replacing (ie, intercalary) reconstructions [3].
For example, for a patient with a high-grade osteogenic sarcoma that involves the distal femoral metaphysis but avoids the joint surface (Fig. 1), the ideal resection would be a joint-sparing hemimetaphyseal resection. Because this resection is difficult to perform using traditional manual techniques, rather than risk a positive or contaminated margin, many surgeons would opt for a more aggressive, joint-sacrificing resection such as a hemicondylar resection [18] or even a distal femur resection [6]. Whether an osteoarticular allograft or an endoprosthesis is used to reconstruct such resections, the construct typically fails with time, requiring substantial revision surgery [10, 12, 14, 15, 17, 19, 20, 26, 33, 37]. In contrast, if a patient underwent a joint-sparing resection (Fig. 2), an intercalary allograft could be used for the reconstruction; if successfully united to host bone, this could offer a lifelong solution [3]. In practice, performing an intercalary resection is possible if the surgeon could accurately reproduce the preoperative plan.
Robot-assisted technology, which has recently been introduced into knee arthroplasty procedures [24], may help improve the accuracy of reproducing the preoperative plan. The surgeon can precisely outline an ideal bone resection block on the MRI preoperatively that corresponds to an actual uncontaminated wide resection. The preoperative plan can then be programmed into a robotic system, which helps the surgeon exactly reproduce this ideal resection at the time of surgery.
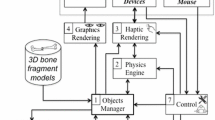
However, serious risks could occur if a surgeon yielded complete control of a saw to a robot that actively performs the resections. Although the robot may make accurate bone cuts, it may inadvertently injure deformable soft tissue structures such as major blood vessels and nerves. For this reason, we developed a passive, rather than an active, robotic technology for this application, in which the surgeon truly has full control of a saw that is attached to a robotic arm. The robot’s function is simply to enforce the predefined spatial boundaries (haptic boundaries) of the plane within which movement of the saw blade should occur. If the surgeon accidentally attempts to move the saw blade outside these boundaries during the saw cut, the robotic arm exerts mechanical resistance to prevent the surgeon from doing so, thereby avoiding an errant cut. The mechanical resistance serves as tactile, or haptic, feedback that guides the surgeon’s positioning of the saw blade throughout the procedure. Thus, haptic robot-assisted surgery is designed to maintain the accuracy afforded by robotic technology while avoiding soft-tissue injury or other complications that could result if the surgeon yielded complete control of the saw to the robot.
We asked whether this novel technique would substantially improve the surgeon’s ability to accurately reproduce a well-defined preoperative resection plan compared with a traditional manual technique. In particular, we determined whether the robotic technique would improve the mean values of various parameters of accuracy compared with the manual technique and whether the robotic technique would decrease the percentage of times that a violation greater than certain magnitudes occurred.
Materials and Methods
We used six pairs of identical Sawbones® femurs (Pacific Research Laboratories, Inc, Vashon, WA, USA). We imaged one representative Sawbones specimen with a high-resolution laser scanner (FaroArm Platinum; FARO Technologies, Inc, Lake Mary, FL, USA), which is highly accurate at imaging the cut surfaces of a Sawbones femur [2]. The preoperative images were used to generate a three-dimensional surface model of the Sawbones specimen using reverse engineering software (Version 12.0; Studio, Geomagic, Inc, Research Triangle Park, NC, USA). We then outlined a hypothetical joint-sparing hemimetaphyseal resection (Fig. 2) on the Sawbones femur using the reverse engineering software. We chose a distal femur sarcoma as the bone tumor model because it is the most common site of the most common primary bone cancer [23].
In each pair, one Sawbones specimen was resected using the haptic robot-assisted technique (robotic group) and the other was resected using the standard manual technique (manual group).
We used a standard procedure for wide resection in orthopaedic oncology to perform the manual resections [3, 35]. When an orthopaedic surgeon performs a manual resection, the surgeon typically draws (eg, on an MRI scan) the osteotomy planes, which would enable en bloc removal of tumor with a surrounding cuff of normal bone (and soft tissue) in all directions. The surgeon then records the location of each of these osteotomy planes from key palpable and/or visible anatomic landmarks. The surgeon uses this guide at the time of surgery to mark the location of the osteotomy planes on the patient’s femur so as to reproduce the preoperative plan as closely as possible. Typically, the surgeon either uses the cautery or a surgical marking pen to draw on the patient’s femur. Similarly, the dimensions of each plane of the osteotomy were measured from key anatomic landmarks (ie, the distal medial joint line, the medial epicondyle, the lateral epicondyle, and the front of the intercondylar notch) and printed out as a visual aid for the surgeon. One orthopaedic oncology fellowship-trained surgeon (FAK) then identified these landmarks on the Sawbones specimen and, using a standard surgical (flexible metal) ruler and marking pen, carefully outlined the three osteotomy planes on the specimen (Fig. 3). The surgeon then carefully cut the bone along the indicated planes with an oscillating saw.
The ideal resection is drawn manually on a Sawbones femoral model. The surgeon carefully reviewed the preoperative plan and attempted to reproduce the corresponding resection on an actual Sawbones femur using a surgical (flexible metal) ruler and marking pen. The surgeon focused on the distances of each osteotomy line from visible and palpable anatomic landmarks such as the medial and lateral epicondyles and the intercondylar notch.
We used a surface matching technique that takes into account the preoperative imaging [25] to register the Sawbones femurs before resection. Because, to our knowledge, registration software for the distal femoral metaphysis has not yet been developed, we used knee arthroplasty registration software designed for the distal femur articular surface in a manner consistent with other published studies in which surface matching for computer-navigated (but nonrobotic) extremity tumor surgery was performed [9, 32]. To quantify the accuracy of our registration, we placed the registration pointer on the surface of the bone. Ideally, the computer navigation software would recognize the pointer as actually touching the surface of bone with zero distance between the pointer and the surface of bone. If the pointer is actually touching the bone and the computer navigation software interprets the pointer as located off the surface of bone, then this constitutes a registration error. The magnitude of the discrepancy (that is, what distance the computer reads that the pointer is off the bone surface when it is actually on the bone surface) served as our quantitative measure of registration accuracy. The accuracy of the registration technique was measured by placing a registration pointer on the surface of the bone in six different locations within the vicinity of the bone resection and recording the distance between the registration pointer and the surface of the bone as estimated by the registration software. If the inaccuracy was greater than 1.0 mm, we repeated the registration process.
The RIO Robotic Arm Interactive Orthopedic System (MAKO Surgical Corp, Ft Lauderdale, FL, USA) was used to perform the haptic robot-assisted resections. The RIO system is currently used to implant unicompartmental knee arthroplasties. In this application, a round burr is used to remove a volume of arthritic bone [24]. However, as mentioned, the appropriate treatment for a primary bone sarcoma is wide excision, so volumetric intralesional removal with a round burr is not an acceptable technique for this resection.
Thus, our team of surgeons collaborated with industry robotic engineers (MAKO Surgical Corp) to develop a robotic saw that could be used to perform three (perpendicular) osteotomies just beyond the limits of the tumor (as shown in Figs. 1, 2) to appropriately effect a bone- and joint-conserving wide resection. An oscillating saw with a 1.47-mm blade was used. A greater blade thickness than what is typically required for this procedure was chosen to minimize errors that might result from blade flexion (that is, to reduce undesired up–down rather than side-to-side oscillations). The saw driver had a design similar to that of manual saw drivers currently used in the operating room, complete with an activation trigger, which ensures that only the surgeon (and not the robot) can activate and control the saw blade. The key difference from a standard manual saw is that a robotic arm was also attached to the saw (behind and away from the surgeon’s hands).
The robotic arm, which itself is attached to the RIO system, ensures that the surgeon does not deviate from the preoperative plan while performing the actual resection. For a given osteotomy plane (eg, the superior limb of the osteotomy in Fig. 2), the surgeon first introduces the (inactivated) saw blade into the plane of the cut. The robotic arm then makes the necessary adjustments to ensure that the saw blade is truly coplanar with the planned osteotomy and locks the saw in this plane, thereby establishing the haptic boundaries. The surgeon then has the freedom to move the saw within this plane but is prevented by the robot from positioning the saw blade to produce a cut beyond the predefined resection. The robot does not inactivate the saw (only the surgeon can do this by releasing the trigger), but, rather, enforces the haptic boundaries. In other words, the surgeon is prevented from deviating from the preoperative plan by a virtual boundary wall, also called a haptic boundary wall, produced by the robotic system (Fig. 4). Using this haptic robotic technique, the surgeon performed the desired bone resections indicated in Figure 2, first in three trial specimens (for the learning curve; mean deviation from preoperative plan for these nine cuts in three specimens was 1.7 mm with 2.6 mm as the single greatest deviation from the plan noted) and then in six experimental Sawbones specimens after each bone model was registered using the surface matching technique. No procedure in the robotic group had to be aborted because of registration or robotic system failures.
Screen shot was taken during haptic robot-assisted joint-sparing distal femur resection on a Sawbones femoral model, illustrating the proximal limb of the osteotomy. The yellow plane represents a virtual boundary beyond which the haptic robotic arm will not allow the saw to move. Although the surgeon has full control of the saw and is the only one who can activate it and keep it activated, the surgeon will be prevented from transgressing these preoperatively defined boundaries by a constraining robotic arm that is also physically attached to the saw. Thus, the surgeon is constrained to work within a very precisely defined plane and cannot inadvertently make cuts beyond the preoperatively defined region. The extension of the plane lateral to the edge of the bone was intentionally planned to allow the saw to be introduced into the surgical field and can be easily modified to accommodate a given surgical exposure.
After resection, each specimen was imaged using the laser scanner (FaroArm Platinum). We then created a three-dimensional image of each resected specimen using the reverse engineering software (Geomagic Studio). For all calculation purposes, the reverse engineering software converts the three-dimensional image of the femur into closely spaced, but discrete (rather than continuous), points, including those points on the cut surface of the bone. Because the voids in the cancellous bone make it very difficult, even impossible, to satisfactorily identify points on the cut surface, we only used points on the outer cortices of each cut in the accuracy calculations (see the Appendix). After these points on each limb of the osteotomy were outlined, the absolute coordinate position in space (relative to the reference coordinate system) was recorded for every point. We then generated a best-fit plane through the data points for each of the three osteotomies.
For each limb of the osteotomy, the relative position of the points and the best-fit plane for the actual surgical cuts were compared with the target plane as defined in the preoperative plan. We accounted for the kerf of the saw blade in all of the accuracy calculations. For the individual points of the actual resection, we recorded the maximum absolute deviation from the preoperative plan (ie, the location error according to International Organization for Standardization [ISO] guidelines, ISO1101:2004 [13]). For the best-fit plane through the actual resection points, two Euler angles (pitch and roll) measuring the angular deviation with respect to the target plane and the flatness of each surgical cut were measured. We also measured the parallelism between the superior and inferior planar cuts and the overall flatness of each of the cuts. The exact definition of these terms, their calculation, and their correspondence with ISO standards are described in detail in the Appendix.
We calculated the mean of the mentioned parameters of accuracy for the robotic and manual groups, treating all three cuts in each specimen together. For instance, for the maximum deviation from the preoperative plan, we took the single greatest maximum deviation noted in each specimen among any of the three osteotomies and averaged the resulting six values in the robotic group with an identical calculation repeated for the manual group. For angular deviation, parallelism, and flatness, the average value per specimen was recorded and then the average of the resulting six values taken for each the robotic and the manual groups. Assuming the data for each group to have an approximate normal distribution and not paired, differences were compared using an unpaired two-sided Student’s t-test. The percentage of times that the manual and robotic resection techniques resulted in a maximum deviation that exceeded various distance values, called threshold values, was also calculated by dividing the number of planes that contained a point with a maximum deviation exceeding the specified threshold value by the total number of planes in each group. The threshold values can be interpreted as the surgeon’s accepted error in the resection. For example, if the surgeon performing a wide resection desired an absolute minimum 5-mm margin in every direction surrounding a tumor, the surgeon, understanding the limitations in accuracy of any resection technique, might deliberately plan a resection that is 5 + 3 = 8 mm away from the tumor in every direction; in this case, the surgeon plans a resection with a tolerated, or accepted error, of 3 mm. Because the (side-to-side) oscillatory motion of the saw also results in small (but nonzero) vertical oscillations of the saw blade, some degree of deviation of the cuts from the target planes is expected even under the most ideal circumstances. To allow for some deviation from the target plane as a result of the cutting device, we chose to begin our threshold values at 2 mm and then continued to analyze at 3 mm, 4 mm, and so on. The statistical analysis was performed with SPSS software (Version 15.0; IBM Corp, Armonk, NY, USA).
Results
Compared with the manual group, the robotic group demonstrated improvements in all parameters used to determine the accuracy of the resections with respect to the preoperative plan. The robotic technique improved (p = 0.001) the mean maximum deviation from the preoperative plan by 7.8 mm. Similarly, the best-fit planes taken through the cuts more closely approximated the target planes in the robotic group than in the manual group with a mean improvement of 7.9° in pitch (p < 0.001) and 4.6° in roll (p < 0.001). The superior and inferior planes deviated from perfectly parallel (as outlined in the preoperative plan) by an average of 3.5° for the manual group and 0.9° for the robotic group (p ≤ 0.001). There was a small improvement (p = 0.02) in the flatness of the two cuts with the robotic group having a deviation from flatness (with a value of zero considered perfectly flat) of 0.4 versus 0.6 for the manual group. To provide a direct, visual representation of the data, we used the reverse engineering software (Geomagic Studio) to create three-dimensional reconstructed images for a representative manually resected specimen (Fig. 5) and for a representative robotically resected specimen (Fig. 6) with the target planes superimposed on the postresection images.
There was a marked difference in the percentage of violations from the preoperative plan between the robotic and manual groups (Table 1). At the 2-mm threshold, 100% of the manually resected planes had a maximum deviation from the preoperative plan that exceeded this threshold, whereas only 28% of the robotically resected planes did so (Table 2). At thresholds of 3 mm and greater, the robotically resected planes did not have any violations, whereas the manually resected planes had violations 100% of the time at 3 mm, 73% of the time at 4 mm, and 40% of the time at 5 mm. Only when the threshold value was increased to 13 mm were no violations noted in the manual group.
Discussion
Inaccuracy in reproducing the preoperative plan during surgery can substantially increase the rate of local recurrence, which can compromise patient survival or push the surgeon to resect more normal tissue than is oncologically necessary, which can compromise patient function [4, 5, 20]. In this study, we demonstrate using a preliminary Sawbones model that a novel technique using haptic robotic technology can accurately allow the surgeon to reproduce a preoperative plan, especially as compared with a traditional, manual technique.
This preliminary study has several limitations. First, for this initial, pilot study, only one fellowship-trained surgeon performed the resections. Although the data reported here clearly illustrate the potential for this technology to improve the accuracy of bone tumor resections, larger studies involving multiple surgeons and larger numbers of specimens are required before any definitive conclusions can be made. Nevertheless, we note that the deviations from the preoperative plan for the manual resections are of a similar nature and magnitude as those obtained in other studies. In one study that examined the accuracy of manual resections of pelvic Sawbones models, performed by four surgeons, a violation beyond 5 mm of the preoperative plan occurred in 48% of cases [7], a rate that compares similarly to our rate of 40% for manual resections that violated the preoperative plan by more than 5 mm (Table 1). In another study comparing manual resections with computer-navigated resections and with robotic resections performed by an industrial robot (without haptic technology), the location error (which is analogous to the maximum deviation from the preoperative plan) averaged 5.19 ± 3.44 mm for the manual resections [8]; in that study, the surgeons performed a single planar cut in a rectangular block of material and, therefore, did not confront the complexity of performing three cuts in an irregular but anatomically shaped distal femur, like in our study. Second, this version of the haptic robotic system is still considered experimental and thus is not ready for clinical use. In our case, the resection involved a nonarticular region of bone proximal to the knee despite using a surface matching algorithm designed to identify a resection at the knee. The use of surface matching algorithms in anatomic areas other than those for which it was designed yields less accurate resections [32]. Our team is currently working to incorporate more accurate bone registration modalities using fluoro-CT matching and intraoperative CT scanning. Other modifications to the robotic system are focused on improving the ease of use of the robot, improving the accuracy of the cuts, and using the robot for cuts of greater complexity such as multiplanar osteotomies. After these modifications are incorporated into future iterations of the haptic robotic system, further studies are required to reassess accuracy and the extra time required for haptic robot-assisted surgeries. Third, idealized Sawbones rather than cadavers were used. The presence of soft tissues could affect the accuracy results as well as the ability of the surgeon to introduce the saw (and the attached robotic arm) into the wound. Cadaveric studies are clearly warranted. Fourth, although this study used laser-scanned data, the system could have easily been adapted for CT images. Even so, this means that each patient would require a CT scan in addition to the usual MRI. A CT-based system will still have to incorporate MRI findings in one form or another, because MRI is more sensitive at showing tumor extent than CT [27]. Existing modern MRI/CT fusion software [1, 31, 36] would be ideal for this purpose. Fifth, computer navigation has been recently introduced into orthopaedic oncology as a means to help surgeons reproduce preoperative plans [9, 32]. A limitation of this study is that it did not compare the accuracy of computer-navigated (but nonrobotic) resections with that of haptic robot-assisted resections. We surmise that the haptic robotic technique will produce more accurate resections than a computer-navigated technique, because this robotic system, in addition to orienting the surgeon as to where to start the cut (which computer navigation systems do), ensures that the surgeon maintains a given trajectory for the entire cut (which computer navigation systems do not do). Finally, industrial robotic systems are accurate but are far from clinically realistic. Their physical dimensions and limited degrees of freedom make it difficult for the surgeon to introduce their cutting instruments into the wound. Moreover, the lack of haptic technology introduces substantial potential dangers to adjacent soft tissues. In tumor surgery, major blood vessels and nerves are commonly exposed in the vicinity of the bone that is to be resected. Conventional tracking systems can accurately track (rigid) bony structures but have difficulty tracking (deformable) soft tissues such as vessels and nerves. To avoid disastrous complications to the neurovascular structures, it is therefore greatly advantageous to give final control of the cutting device to the surgeon. The haptic robotic technology used in this study perfectly meets this requirement while maintaining high levels of accuracy.
From a clinical standpoint, the percentage of times that each resection group violated each threshold was the most important outcome variable. For the manual group, violations occurred at every integral threshold value below 13 mm. In contrast, for the robotic group, no violations occurred at or above the 3-mm threshold. These findings suggest that to avoid inadvertently cutting into the tumor, the surgeon should aim to produce cuts that are at least 13 mm away from the ideal resection lines when using the manual technique. However, when using the haptic robotic technique, the surgeon can aim to produce cuts that are only approximately 3 mm away from the ideal resection lines. In practice, given the relatively close proximity of metaphyseal tumors to the joint, performing a resection 13 mm beyond the ideal resection line may leave little to no possibility of sparing the epiphysis, whereas performing a resection approximately 3 mm beyond the ideal resection line would likely still allow for a satisfactory joint-sparing resection and reconstruction [3]. The extra centimeter may be critical to save the joint.
In conclusion, this study has shown that a novel haptic robot-assisted technique can produce preplanned bone cuts in a distal femur Sawbones model more reliably than a manual technique. Substantial work is still required to make the robotic system developed here ready for clinical use, and further studies are warranted to evaluate the use and accuracy of this haptic robotic technique in more realistic clinical scenarios before its acceptance as a surgical tool.
References
Alyafei S, Inoue T, Zhang H, Ahmed K, Oriuchi N, Sato N, Suzuki H, Endo K. Image fusion system using PACS for MRI, CT, and PET images. Clin Positron Imaging. 1999;2:137–143.
Anstey JB, Smith EJ, Rasquinha B, Rudan JF, Ellis RE. On the use of laser scans to validate reverse engineering of bony anatomy. Stud Health Technol Inform. 2011;163:18–24.
Avedian RS, Haydon RC, Peabody TD. Multiplanar osteotomy with limited wide margins: a tissue preserving surgical technique for high-grade bone sarcomas. Clin Orthop Relat Res. 2010;468:2754–2764.
Bacci G, Ferrari S, Mercuri M, Bertoni F, Picci P, Manfrini M, Gasbarrini A, Forni C, Cesari M, Campanacci M. Predictive factors for local recurrence in osteosarcoma: 540 patients with extremity tumors followed for minimum 2.5 years after neoadjuvant chemotherapy. Acta Orthop Scand. 1998;69:230–236.
Bacci G, Forni C, Longhi A, Ferrari S, Mercuri M, Bertoni F, Serra M, Briccoli A, Balladelli A, Picci P. Local recurrence and local control of non-metastatic osteosarcoma of the extremities: a 27-year experience in a single institution. J Surg Oncol. 2007;96:118–123.
Bickels J, Wittig JC, Kollender Y, Henshaw RM, Kellar-Graney KL, Meller I, Malawer MM. Distal femur resection with endoprosthetic reconstruction: a long-term followup study. Clin Orthop Relat Res. 2002;400:225–235.
Cartiaux O, Docquier PL, Paul L, Francq BG, Cornu OH, Delloye C, Raucent B, Dehez B, Banse X. Surgical inaccuracy of tumor resection and reconstruction within the pelvis: an experimental study. Acta Orthop. 2008;79:695–702.
Cartiaux O, Paul L, Docquier PL, Raucent B, Dombre E, Banse X. Computer-assisted and robot-assisted technologies to improve bone-cutting accuracy when integrated with a freehand process using an oscillating saw. J Bone Joint Surg Am. 2010;92:2076–2082.
Cho HS, Oh JH, Han I, Kim HS. Joint-preserving limb salvage surgery under navigation guidance. J Surg Oncol. 2009;100:227–232.
Gebhardt MC, Flugstad DI, Springfield DS, Mankin HJ. The use of bone allografts for limb salvage in high-grade extremity osteosarcoma. Clin Orthop Relat Res. 1991;270:181–196.
Hoffer FA, Nikanorov AY, Reddick WE, Bodner SM, Xiong X, Jones-Wallace D, Gronemeyer SA, Rao BN, Kauffman WM, Laor T. Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol. 2000;30:289–298.
Horowitz SM, Glasser DB, Lane JM, Healey JH. Prosthetic and extremity survivorship after limb salvage for sarcoma. How long do the reconstructions last? Clin Orthop Relat Res. 1993;293:280–286.
International Standard, ISO 1101:2004(E). Geometrical Product Specifications (GPS)—Geometrical Tolerancing—Tolerances of Form, Orientation, Location and Run-out. 2nd ed. Geneva, Switzerland: International Organization for Standardization; 2004.
Kawai A, Lin PP, Boland PJ, Athanasian EA, Healey JH. Relationship between magnitude of resection, complication, and prosthetic survival after prosthetic knee reconstructions for distal femoral tumors. J Surg Oncol. 1999;70:109–115.
Kawai A, Muschler GF, Lane JM, Otis JC, Healey JH. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur. Medium to long-term results. J Bone Joint Surg Am. 1998;80:636–647.
Marcove RC, Sheth DS, Healey J, Huvos A, Rosen G, Meyers P. Limb-sparing surgery for extremity sarcoma. Cancer Invest. 1994;12:497–504.
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Abalo E, Farfalli G. Unicondylar osteoarticular allografts of the knee. J Bone Joint Surg Am. 2007;89:2137–2142.
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Abalo E, Farfalli G. Unicondylar osteoarticular allografts of the knee. Surgical technique. J Bone Joint Surg Am. 2008;90(Suppl 2):206–217.
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Use of distal femoral osteoarticular allografts in limb salvage surgery. J Bone Joint Surg Am. 2005;87:2449–2455.
Nagarajan R, Neglia JP, Clohisy DR, Robison LL. Limb salvage and amputation in survivors of pediatric lower-extremity bone tumors: what are the long-term implications? J Clin Oncol. 2002;20:4493–4501.
Nathan SS, Gorlick R, Bukata S, Chou A, Morris CD, Boland PJ, Huvos AG, Meyers PA, Healey JH. Treatment algorithm for locally recurrent osteosarcoma based on local disease-free interval and the presence of lung metastasis. Cancer. 2006;107:1607–1616.
Onikul E, Fletcher BD, Parham DM, Chen G. Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR Am J Roentgenol. 1996;167:1211–1215.
Ottaviani G, Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13.
Pearle AD, O’Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty. 2010;25:230–237.
Raabe A, Krishnan R, Seifert V. Actual aspects of image-guided surgery. Surg Technol Int. 2003;11:314–319.
Renard AJ, Veth RP, Schreuder HW, van Loon CJ, Koops HS, van Horn JR. Function and complications after ablative and limb-salvage therapy in lower extremity sarcoma of bone. J Surg Oncol. 2000;73:198–205.
Rougraff BT, Simon MA, Kneisl JS, Greenberg DB, Mankin HJ. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. J Bone Joint Surg Am. 1994;76:649–656.
Saifuddin A. The accuracy of imaging in the local staging of appendicular osteosarcoma. Skeletal Radiol. 2002;31:191–201.
San-Julian M, Aquerreta JD, Benito A, Cañadell J. Indications for epiphyseal preservation in metaphyseal malignant bone tumors of children: relationship between image methods and histological findings. J Pediatr Orthop. 1999;19:543–548.
Shin DS, Choong PF, Chao EY, Sim FH. Large tumor endoprostheses and extracortical bone-bridging: 28 patients followed 10–20 years. Acta Orthop Scand. 2000;71:305–311.
Shin M, Penholate MF, Lefaucheur JP, Gurruchaga JM, Brugieres P, Nguyen JP. Assessing accuracy of the magnetic resonance imaging-computed tomography fusion images to evaluate the electrode positions in subthalamic nucleus after deep-brain stimulation. Neurosurgery. 2010;66:1193–1202.
So TYC, Lam YL, Mak KL. Computer-assisted navigation in bone tumor surgery: seamless workflow model and evolution of technique. Clin Orthop Relat Res. 2010;468:2985–2991.
Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res. 2001;392:283–291.
Springfield DS, Schmidt R, Graham-Pole J, Marcus RB Jr, Spanier SS, Enneking WF. Surgical treatment for osteosarcoma. J Bone Joint Surg Am. 1988;70:1124–1130.
Sugarbaker PH, Malawer MM. Musculoskeletal Surgery for Cancer: Principles and Techniques. New York, NY, USA: Thieme Medical Publishers; 1992.
Yamanaka Y, Kamogawa J, Katagi R, Kodama K, Misaki H, Kamada K, Okuda S, Morino T, Ogata T, Yamamoto H. 3-D MRI/CT fusion imaging of the lumbar spine. Skeletal Radiol. 2010;39:285–288.
Zatsepin ST, Burdygin VN. Replacement of the distal femur and proximal tibia with frozen allografts. Clin Orthop Relat Res. 1994;303:95–102.
Acknowledgments
We thank Mako Surgical Corporation for providing the robot and required robotic engineering support used in this study at no cost to the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (AP, PJB, JHH) has received funding from MAKO Surgical Corporation (Ft Lauderdale, FL, USA). One author (CL) is an employee of MAKO Surgical Corp.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at Memorial Sloan-Kettering Cancer Center, New York, NY, USA; the Hospital for Special Surgery, New York, NY, USA; and Mako Surgical Corporation.
Appendix
Appendix
Calculation of various parameters of accuracy
We used reverse engineering software (Version 12.0; Studio, Geomagic, Inc, Research Triangle Park, NC, USA) to analyze the pre- and postresection three-dimensionally reconstructed laser scan images. The preoperative image contained the three target planes of the resection, ie, the three planes that were defined as part of the preoperative plan as the superior, inferior, and vertical cut planes. For each specimen, the standard best alignment function of the software was used to perfectly superimpose the preoperative and postoperative images of the Sawbones specimen; this placed the preoperative and postoperative scans in a common coordinate system. We then used the software to highlight the cortical rim of each of the three cuts, deliberately excluding the cancellous surfaces to avoid the analysis problems associated with the cancellous voids of the cancellous surface. (These voids resulted in the software selecting points not only on the surface of the cancellous bone, but also in the depths of the voids, the latter of which were clearly not in the plane of the cut.) We believed this technique was well justified, because it was unlikely that a horizontal saw blade would produce cuts in the cancellous surface that deviated wildly from the plane of the cuts defined by just the cortical rims. The small values recorded for the deviation from flatness for both the robotic and manual cuts (see Results section) support this assumption.
The cortical rims of each of the three cuts—superior, inferior, and vertical—were exported as discrete points (relative to the common coordinate system created after the preoperative and postoperative images were superimposed) and imported into a technical computing software program (Matlab; MathWorks, Natick, MA, USA) for further analysis. This software was used to help analyze the various geometric relationships between points on the resection plane (and the best-fit plane) and the target planes. Using this software, the perpendicular distance between each point and the corresponding target plane was calculated. Additionally, the angular deviations between the target plane and best-fit planes were calculated.
The data were reported in a form that was consistent with the standards of the International Organization of Standardization (ISO) (Fig. A-1) [13]. According to these standards, the location error is defined as the perpendicular distance from the target plane to the point on the cut surface furthest from the target plane. For simplicity, in the text we usually refer to location error as the maximum deviation from the preoperative plan. Although it is not an ISO standard, we also calculated the mean deviation of the points from the target plane by calculating the mean of the (absolute) distance of each point from the target plane. The flatness was calculated by measuring the amplitude, or peak-to-peak distance, of the cut surface.
The pitch and roll errors were defined as angular deviations between the best-fit plane and the target plane along the axis of the blade and the front edge of the blade, in that order. Specifically, the roll error refers to a rotation about the AP axis of the bone; the pitch error refers to a rotation about the superoinferior axis for the medial cut and the mediolateral axis for the superior and inferior cuts. For the best-fit planes through the superior and inferior limbs of the cuts, the deviation from parallel was defined as the angle between these two planes.
About this article
Cite this article
Khan, F., Pearle, A., Lightcap, C. et al. Haptic Robot-assisted Surgery Improves Accuracy of Wide Resection of Bone Tumors: A Pilot Study. Clin Orthop Relat Res 471, 851–859 (2013). https://doi.org/10.1007/s11999-012-2529-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2529-7