Abstract
Background
Recently, the authors of two prospective multicenter observational studies recommended surgery to improve head sphericity in older children, whereas large retrospective observational studies suggest that surgery does not improve head sphericity in older children. Thus, the treatment for Legg-Calvé-Perthes disease (LCPD) remains controversial.
Questions/purposes
Using a meta-analysis we asked whether femoral varus osteotomy (FVO) or Salter innominate osteotomy (SIO) resulted in better radiographic head sphericity at the end of the disease process as compared with nonsurgical modalities.
Methods
We systematically searched the literature using the key concepts LCPD, operative treatment, and nonoperative treatment. Of 160 abstracts, 57 full-text studies were reviewed and 14 papers chosen for meta-analysis. Subgroup analyses were performed to assess the impact of age and stage of disease. The odds of a spherical head after operative compared with nonoperative treatment were calculated to measure effect size for each study and a pooled odds ratio (OR) calculated.
Results
Head sphericity improved (OR, 1.29; 95% CI, 1.05–1.60) by FVO or SIO as compared with patients treated nonoperatively. In children younger than 6 years, it did not alter femoral head sphericity (OR, 1.02; 95% CI, 0.45–2.36); children 6 years of age and older were more likely to have better femoral head sphericity from surgical treatment than nonoperative treatment (OR, 2.05; 95% CI, 1.28–3.26).
Conclusions
The data suggest FVO or SIO in patients with LCPD disease who are older than 6 years of age during or before the fragmentation phase should be considered.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
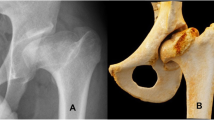
Legg-Calvé-Perthes disease (LCPD) is a childhood hip disorder characterized by idiopathic osteonecrosis of the femoral epiphysis that is likely related to its tenuous blood supply. Attributed to Waldenström [48], the stages of LCPD include necrosis/initial, fragmentation, reossification/healing, and residual. LCPD is associated with substantial hip pain and dysfunction both during the disease process as well as later in adulthood in 39% to 70% of patients at 22 to 47 years followup [36, 41, 46]. Although morbidity appears to be related to the morphologic changes that are present in the final and healed stage of the disease [15], emphasis is on radiographic features that may predict asphericity of the femoral head [6, 16, 25, 44]. Whereas the Catterall [6], Salter-Thompson [44], modified Elizabethtown [25], and lateral pillar [16, 19] classification schemes are used during the disease process, classifications by Stulberg et al. [46] and Mose et al. [38, 39] are generally used to describe the final femoral head shape. The Stulberg classification has become the primary method of quantifying end-result radiographic outcomes at skeletal maturity. It consists of five classes that can be categorized into three groups: spherical congruency (Classes I and II), aspherical congruency (Classes III and IV), and aspherical incongruency (Class V). Although the ultimate goal is to maintain spherical congruency, the optimal treatment remains elusive.
The natural history of LCPD in very young children (younger than 6 years) appears to be less severe with 65% of them going on to develop spherical femoral heads as compared with the natural history in older children (older than 8 years) in whom only 12% develop spherical femoral heads [24]. Catterall [5] suggested age and head-at-risk signs were the keys to predicting head sphericity at skeletal maturity in patients with LCPD. This view has since been challenged and several studies have reported that age and lateral subluxation are more important [22, 40, 42]. More recently it has been suggested that age along with amount of head collapse as judged by the modified lateral pillar classification are better prognostic indicators of head sphericity at skeletal maturity [18]. In addition, many authors suggest the stage at which surgery is undertaken directly affects femoral head sphericity [2, 6, 14, 16, 20, 21, 23, 26, 27, 31, 33, 35, 37, 47]. Although multiple treatment modalities are available, their effects on the natural history of the disease are unclear.
Several retrospective studies [4, 5, 13], one of which included 371 patients and specifically addressed patients older than 8 years of age [1], have found no clear benefit to operative versus nonoperative treatment groups with respect to head sphericity. However, recently two large (> 300 patients in each study) prospective multicenter observational studies [18, 50] have recommended surgery for older patients. Despite this, the role of surgery in treating older patients still remains unclear.
We therefore asked whether (1) either a femoral varus osteotomy or Salter innominate osteotomy results in better radiographic head sphericity at the end of the disease process as compared with nonoperative treatment modalities; and (2) age of onset of LCPD or stage of disease process at surgery affected the risk of having an aspherical head.
Search Strategy and Criteria
Medline and EMBASE databases were searched using the key concepts of “operative treatment”, “nonoperative treatment”, and “Perthes”. All three search results were merged using the AND function to minimize nonapplicable studies (Appendices A, B). The Journal of Children’s Orthopaedics was searched using the PubMed database for the term “Perthes”. All searches were performed in March 2010. All abstracts were reviewed and studies that were non-LCPD-related or were nontreatment-related were eliminated yielding a set of studies that was obtained and reviewed for the inclusion and exclusion criteria. All searches were limited to English language publications and an age limit of 0 to 18 years. Any studies that included children with neuromuscular, metabolic, or other hip disorders were also excluded. Publication dates were not restricted. The Medline (Appendix A) and EMBASE (Appendix B) searches yielded 141 potential studies after duplicates were removed. A PubMed search of the Journal of Children’s Orthopaedics for the keyword “LCPD” yielded an additional 19 studies for a total of 160 papers (Fig. 1).
Title, abstract, and article reviews were conducted in a nonblinded fashion by two independent reviewers (NS, RV) both of whom are fellowship-trained pediatric orthopaedic surgeons. Disagreement in final article selection was resolved by consensus. Data sets with multiple publications were removed such that only the single largest data set was included. Levels of evidence were assigned based on the schema used by The Journal of Bone and Joint Surgery (www.ejbjs.org) with a modification to the Level II (prospective observational studies) and Level III (case-comparative or case-control) studies. The Level II and III studies were further divided into a and b in which the former included studies in which a nonclinical process was used to decide on the type of intervention in all patients treated during the study period. This yielded a group of studies (IIa and IIIa) that is quasirandomized for treatment based on period, referral center, or center of treatment. The rationale for this is to minimize selection bias usually present in retrospective studies.
Of the 160 abstracts reviewed, 57 articles were reviewed in full, and of these, 18 reported the use of either a femoral varus osteotomy (FVO) or a Salter innominate osteotomy (SIO) with respect to radiographic outcomes including the Stulberg classification, Mose sphericity, or Mose concentric templates and a comparative nonoperative group (Table 1). Four of these 18 were eliminated to remove duplicated data sets secondary to multiple publications leaving 14 studies for the overall analysis (Fig. 1). However, the duplicated data sets were maintained for subgroup analysis in the event that the chosen study did not provide stratification as is the case for Cooperman and Stulberg [7] and Evans et al. [9].
The primary outcome measure collected was radiographic sphericity at final followup. A spherical head was represented by Stulberg I and II, Mose spherical, and Mose concentric templates within 2-mm classifications, whereas an aspherical head was represented by Stulberg III, IV, and V; Mose flattened and irregular; and Mose concentric templates > 2 mm classifications. Where multiple classifications were used, the Stulberg classification was chosen over the Mose classification system. All count data were collected by two independent reviewers (NS, RV). Disagreements in counts were resolved by consensus.
There were three Level IIa and two Level IIIa studies leaving five studies for subgroup analysis of Level IIa and IIIa studies only. The primary analysis of Level IIa and IIIa studies with patients treated during or before the fragmentation phase included three studies. Because each of these three studies presented data in various age groupings, multiple meta-analyses were performed to assess not only the overall effect of operative versus nonoperative treatment on radiographic head sphericity, but also the effects of intervention within certain age groupings. Considering that the study by Lahdes-Vasama et al. [32] was a Level III study, the analyses were performed with and without its incorporation. We excluded patients with < 50% head necrosis from the study by Wiig et al. [50] in the meta-analysis because the Stulberg outcomes for these patients were not tabulated by treatment type.
An odds ratio with 95% CI was calculated comparing FVO and SIO groups. Heterogeneity was tested using the chi-square and I2 tests. A pooled odds ratio (OR) was calculated using an inverse variance, fixed-effect model and a Z-test was performed to assess for an overall effect using Review Manager 5 (The Cochrane Collaboration, Copenhagen, Denmark). The primary analysis was done for Level II and III studies. Subgroup analyses were performed using the same statistical tests on all Level IIa and IIIa studies. Additional subgroup analyses were performed to assess for effect on sphericity by various age groupings as well as on patients treated during or before the fragmentation phase. The pooled OR represents the odds of having a spherical head at the end of treatment in patients treated by operative means (either FVOs or SIOs) as compared with those treated nonoperatively.
Results
Surgery appeared more likely to be associated with a spherical head at skeletal maturity than nonoperative treatment in patients with LCPD when pooling all data without stratifying for risk factors such as age of onset or stage of disease. Analysis of the 14 Level II and III studies yielded a pooled OR for a spherical head at skeletal maturity in operative versus nonoperative cases of 1.29 (p = 0.02; 95% CI, 1.05–1.60) (Fig. 2).
The forest plot of odds ratios for all Level II and III studies with a table of summarized data and tests for heterogeneity shows that operative treatment results in a higher likelihood of femoral head sphericity. Events = number of cases in treatment group that resulted in a spherical femoral head; Total = number of cases in the treatment group.
Surgery does not appear to be more likely associated with a spherical head at maturity than nonoperative treatment when analyzing patients treated during or before fragmentation (OR, 1.29; p = 0.06; 95% CI, 0.99–1.68) (Fig. 3); however, when a subgroup of the patients treated during or before fragmentation consisting of only Level II and IIIa studies is performed, surgery does appear to be more likely associated with a spherical head at maturity than nonoperative treatment (OR, 1.46; p = 0.02; 95% CI, 1.06–2.01) (Fig. 4). We substituted data from the Evans et al. [9] study for the data from the Cooperman and Stulberg [7] study because the Cooperman and Stulberg [7] study did not contain necessary data for subgroup analysis.
Forest plot of odds ratios for Level II and III studies with data on cases treated during or before fragmentation stage with a table of summarized data and tests for heterogeneity reveals operative treatment does not increase likelihood of femoral head sphericity. Events = number of cases in treatment group that resulted in a spherical femoral head; Total = number of cases in the treatment group.
Forest plot of odds ratios for Level II and IIIa studies with data on cases treated during or before fragmentation stage with a table of summarized data and tests for heterogeneity shows that operative treatment results in a higher likelihood of femoral head sphericity. Events = number of cases in treatment group that resulted in a spherical femoral head; Total = number of cases in the treatment group.
Age-stratified analysis of the Level II and IIIa studies shows that surgery does not appear to be more likely associated with a spherical head at maturity than nonoperative treatment in patients younger than age 6 years (Table 2; see Appendix C for forest plots). Although there is clearly no improved femoral head sphericity after surgery in those younger than age 6 years, the interval from 6 to 8 years of age is a gray zone with only a trend toward benefit, whereas when analyzing all children older than 6 years or older than 8 years, there is clearly an improvement in head sphericity after surgery.
Discussion
The best treatment of LCPD remains unknown, although in two recent prospective studies, surgery in certain subgroups yielded a higher likelihood of a spherical head than nonoperative treatment [18, 50]. The goals of our meta-analysis were to determine whether (1) either a FVO or SIO results in better radiographic head sphericity at the end of the disease process as compared with nonoperative treatment modalities; and (2) age of onset of LCPD or stage of disease at the time of treatment affected the risk of having an aspherical head.
Limitations of this meta-analysis are severalfold. First, only English language papers were used and the search was limited to the Cochrane databases, Medline, and EMBASE. Although some recommend including other databases, a recent publication [45] examining meta-analyses in orthopaedics suggests that searching the Cochrane databases, Medline, and EMBASE provides a 97% recall rate and that expansion to Web of Science or Cumulative Index to Nursing and Allied Health Literature does not improve the recall rate. Second, the analysis is based solely on nonrandomized studies. This is a major limitation but as a result of the relatively low incidence of LCPD, such trials become extremely difficult. Third, it is difficult to take into account the various effect modifiers and confounders such as age at onset, age at treatment, preoperative ROM, stage of the disease process at the time of treatment, extent of head involvement, extent of head collapse at the time of treatment, sex, femoral head extrusion, and subluxation on the effect of the treatment type. The ideal situation would include having deidentified raw data sets available such that more extensive subgroup analyses would be feasible. Despite the lack of such data sets, a subgroup analysis on the effect of age, one of the greatest effect modifiers for femoral head sphericity in LCPD, was possible and is presented in this review. Fourth, nonblinded retrospective data can often contain bias information skewing the findings of such an analysis. The creation of the “a” type study is an attempt to minimize different forms of bias including selection bias, confounding by severity, and confounding by indication. This could also account for the moderate to high amount of heterogeneity seen in the analyses. The heterogeneity is low when the “a” type studies were analyzed alone perhaps indicating that the results of the final subgroup analysis (Level II and IIIa only) may be most relevant. Fifth, only published data were used for this analysis and as such, such stratification by age or stage of disease at the time of surgery was not possible in all of the studies. As a result of this, the subgroup analyses involve a limited number of patients. For this reason also, we were unable to assess the effect of surgery on head sphericity in patients older than 8 years. The 6- to 8-year age range appears to be a gray zone and additional data may have provided a more suiting conclusion on the effect of surgery on femoral head sphericity in this age range. Furthermore, multiple comparisons were not adjusted for; however, we believe the questions asked were relevant and the conclusions of this study are in keeping with current thoughts on LCPD [17, 29]. Also, this study uses femoral head sphericity as a surrogate for long-term health of the hip. Although Stulberg et al. [46] and McElwain et al. [37] demonstrated a clear correlation between femoral head sphericity and radiographic and functional outcomes, long-term functional outcome studies comparing operative and nonoperative treatments would yield a more direct answer to this question. Finally, head involvement, whether by the Catterall [6] or the modified lateral pillar [19] classification, was not incorporated into this study. Although it is possible that they have substantial bearing on femoral head sphericity, it was not possible to perform a subgroup analysis based on this factor.
Although the overall pooled ORs when all studies are included show that surgery increases the likelihood of femoral head sphericity, the subgroup analyses performed based on age yields more relevant findings with patients older than age 6 years showing a higher likelihood of femoral head sphericity when treated surgically and those aged 6 to 8 years showing only a trend toward improved femoral head sphericity. Based on the lack of an effect size in those younger than 6 years as well as those between 6 and 8 years, it would seem that children older than 8 years would have the largest effect size on femoral head sphericity from surgery. Age appears to be an important factor in terms of altering the natural history of LCPD. Long-term radiographic outcome studies have stressed the importance of age at onset as an important prognostic factor [5, 35, 44] and multiple therapeutic studies [8, 12, 17, 50] have alluded to the importance of age at onset and treatment. It would appear that the older children (older than 6–8 years) are less likely to have a spherical femoral head [7, 10, 12, 17, 50] and it is this same cohort that appears to benefit from surgery. Wiig et al. [50] showed that surgery in the form of a proximal FVO was better than physiotherapy or bracing in patients 6 years of age or older with greater than 50% head involvement, whereas children younger than 6 years with greater than 50% head involvement did not appear to benefit from the surgery. Meanwhile, Herring et al. [18] reported improved femoral head sphericity by FVO or SIO in patients older than 8 years of age who were classified with a lateral pillar B or B/C border hip in comparison to those treated by bracing, ROM, or no treatment.
The Level IIa and IIIa studies revealed patients undergoing FVO or SIO during or before the fragmentation phase have better femoral head sphericity at the end stage of LCPD than those undergoing nonoperative treatment (OR, 1.46; p = 0.02; 95% CI, 1.06–2.01). The primary analyses (all Level II and III studies and all patients despite stage at treatment) revealed similar results (OR, 1.29; p = 0.02; 95% CI, 1.05–1.60). Interestingly, when analyzing all Level II and III studies treated during or before fragmentation, the beneficial effect of surgery was lost (OR, 1.29; p = 0.06; 95% CI, 0.99–1.68). This would imply that the stage at treatment is not an important prognostic factor. Axer et al. [2] reported on 70 patients undergoing varus osteotomy and showed that of patients who had surgery in the early/necrotic phase, only 9% had poor femoral head sphericity as per the Mose methods, whereas 14% of those during the intermediate/fragmentation phase had poor sphericity and 56% of those treated in the late/reossification/regeneration phase had poor sphericity. Jani and Dick [23] reported a better Catterall [6] outcome distribution in patients treated immediately with a varus derotation osteotomy (VDRO) as opposed to waiting for risk factors to appear. Joseph et al. [26] reported a multivariate logistic regression analysis on 97 patients undergoing a VDRO. They found that if surgery was performed during or after late fragmentation, the OR of femoral head asphericity was 16.58 (p < 0.01; 95% CI, 2.6–103.13) as compared with surgery performed during or before early fragmentation. These and multiple other studies [2, 6, 14, 16, 20, 21, 23, 26, 27, 30, 31, 33, 35, 47] have found better femoral head sphericity when surgery has been performed at an earlier stage. Despite our findings, we also believe stage at treatment is crucial in terms of altering the natural history of the disease. One possible explanation for why the inclusion of all Level II and III studies resulted in a loss of effect is that the “b”-type studies incorporated some level of confounding by indication or confounding by severity in that the surgically treated patients were older [5, 11] or had more severe disease [12], both of which are factors associated with aspherical femoral heads.
The data from this meta-analysis suggest a FVO or SIO improves femoral head sphericity in children older than 8 years. Although surgery does not appear to alter the natural history of the disease in those younger than 6 years, children aged 6 to 8 years remain in a gray zone in which the role for surgery is less obvious. Herring et al. [18] included a skeletal age analysis that revealed a cutoff of skeletal age of 6 years for improvement by surgery. It is quite possible that skeletal age rather than chronological age is a more important or consistent prognostic factor for improved radiographic outcomes. Further studies should incorporate skeletal age correlations with their findings. Furthermore, it is important that future studies include skeletal age at presentation and at surgery, pertinent active radiographic classification systems that can differentiate disease stage (modified Elizabethtown and modified lateral pillar), quantification of head involvement (modified Catterall or Salter-Thompson), end-stage radiographic classification systems that can be correlated to long-term outcomes (Mose and Stulberg), and validated functional outcome scores to better understand the physical impact or effects of our interventions.
Appendix A
Database: Ovid MEDLINE® 1950 to the present with daily update search strategy
-
1.
osteotomy.mp.
-
2.
operat$.mp.
-
3.
shelf.mp.
-
4.
distract$.mp.
-
5.
surg$.mp.
-
6.
arthrodiastasis.mp.
-
7.
arthrodiatasis.mp.
-
8.
fixat$.mp.
-
9.
1 or 2 or 3 or 4 or 5 or 6 or 8 or “9”.mp.
-
10.
nonoperative.mp.
-
11.
nonsurgical.mp.
-
12.
non-operative.mp.
-
13.
non-surgical.mp.
-
14.
abduction.mp.
-
15.
bedrest.mp.
-
16.
splint.mp.
-
17.
brace.mp.
-
18.
orthosis.mp.
-
19.
orthoses.mp.
-
20.
physical therapy.mp.
-
21.
physiotherapy.mp.
-
22.
10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21
-
23.
9 and 22
-
24.
perthes.mp.
-
25.
coxa plana.mp.
-
26.
24 or 25
-
27.
23 and 26
-
28.
limit 27 to English language
-
29.
limit 28 to “all child (0 to 18 years)”
Appendix B
Database: Ovid EMBASE search strategy
-
1.
osteotomy.mp.
-
2.
operat$.mp.
-
3.
shelf.mp.
-
4.
distract$.mp.
-
5.
surg$.mp.
-
6.
arthrodiastasis.mp.
-
7.
arthrodiatasis.mp.
-
8.
fixat$.mp.
-
9.
1 or 2 or 3 or 4 or 5 or 6 or 8 or “9”.mp.
-
10.
nonoperative.mp.
-
11.
nonsurgical.mp.
-
12.
non-operative.mp.
-
13.
non-surgical.mp.
-
14.
abduction.mp.
-
15.
bedrest.mp.
-
16.
splint.mp.
-
17.
brace.mp.
-
18.
orthosis.mp.
-
19.
orthoses.mp.
-
20.
physical therapy.mp.
-
21.
physiotherapy.mp.
-
22.
10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21
-
23.
9 and 22
-
24.
perthes.mp.
-
25.
coxa plana.mp.
-
26.
24 or 25
-
27.
23 and 26
-
28.
limit 27 to English language
-
29.
limit 28 to “all child (0 to 18 years)”
Appendix C
Forest plots of subgroup analyses for age groups and levels of evidence suggest that operative treatment may result in more spherical heads in children older than 6 years
All ages Levels IIa and IIIa 
All ages, Level IIa only 
6 + , Levels IIa and IIIa 
6 + , Level IIa only 
< 8, Levels IIa and IIIa 
< 8, Level IIa only 
< 6, Levels IIa and IIIa 
< 6, Level IIa only 
6–8, Level IIIa study 
References
Arkader A, Sankar WN, Amorim RM. Conservative versus surgical treatment of late-onset Legg-Calve-Perthes disease: a radiographic comparison at skeletal maturity. J Child Orthop. 2009;3:21–25.
Axer A, Gershuni DH, Hendel D, Mirovski Y. Indications for femoral osteotomy in Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1980;150:78–87.
Barer M. Role of innominate osteotomy in the treatment of children with Legg-Perthes disease. Clin Orthop Relat Res. 1978;135:82–89.
Bowen JR, Foster BK, Hartzell CR. Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1984;185:97–108.
Castaneda P, Haynes R, Mijares J, Quevedo H, Cassis N. Varus-producing osteotomy for patients with lateral pillar type B and C Legg-Calve-Perthes disease followed to skeletal maturity. J Child Orthop. 2008;2:373–379.
Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971;53:37–53.
Cooperman DR, Stulberg SD. Ambulatory containment treatment in Perthes’ disease. Clin Orthop Relat Res. 1986;203:289–300.
Denton JR. Experience with Legg-Calve-Perthes disease (LCPD) 1968–1974 at the New York Orthopaedic Hospital. Clin Orthop Relat Res. 1980;150:36–42.
Evans IK, Deluca PA, Gage JR. A comparative study of ambulation-abduction bracing and varus derotation osteotomy in the treatment of severe Legg-Calve-Perthes disease in children over 6 years of age. J Pediatr Orthop. 1988;8:676–682.
Fulford GE, Lunn PG, Macnicol MF. A prospective study of nonoperative and operative management for Perthes’ disease. J Pediatr Orthop. 1993;13:281–285.
Glard Y, Katchburian MV, Jacquemier M, Guillaume JM, Bollini G. Genu valgum in Legg-Calve-Perthes disease treated with femoral varus osteotomy. Clin Orthop Relat Res. 2009;467:1587–1590.
Grasemann H, Nicolai RD, Patsalis T, Hovel M. The treatment of Legg-Calve-Perthes disease. To contain or not to contain. Arch Orthop Trauma Surg. 1997;116:50–54.
Grzegorzewski A, Bowen JR, Guille JT, Glutting J. Treatment of the collapsed femoral head by containment in Legg-Calve-Perthes disease. J Pediatr Orthop. 2003;23:15–19.
Hardcastle PH, Ross R, Hamalainen M, Mata A. Catterall grouping of Perthes’ disease. An assessment of observer error and prognosis using the Catterall classification. J Bone Joint Surg Br. 1980;62:428–431.
Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33.
Heikkinen E, Puranen J. Evaluation of femoral osteotomy in the treatment of Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1980;150:60–8.
Herring JA. Legg-Calve-Perthes disease at 100: a review of evidence-based treatment. J Pediatr Orthop. 2011;31:S137–S140.
Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: Classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004;86:2103–2120.
Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86:2121–2134.
Hoikka V, Lindholm TS, Poussa M. Intertrochanteric varus osteotomy in Legg-Calve-Perthes disease: a report of 112 hips. J Pediatr Orthop. 1986;6:600–604.
Hoikka V, Poussa M, Yrjonen T, Osterman K. Intertrochanteric varus osteotomy for Perthes’ disease. Radiographic changes after 2-16-year follow-up of 126 hips. Acta Orthop Scand. 1991;62:549–553.
Ippolito E, Tudisco C, Farsetti P. The long-term prognosis of unilateral Perthes’ disease. J Bone Joint Surg Br. 1987;69:243–250.
Jani LF, Dick W. Results of three different therapeutic groups in Perthes’ disease. Clin Orthop Relat Res. 1980;150:88–94.
Joseph B, Mulpuri K, Varghese G. Perthes’ disease in the adolescent. J Bone Joint Surg Br. 2001;83:715–720.
Joseph B, Nair NS, Narasimha Rao KL, Mulpuri K, Varghese G. Optimal timing for containment surgery for Perthes disease. J Pediatr Orthop. 2003;23:601–606.
Joseph B, Rao N, Mulpuri K, Varghese G, Nair S. How does a femoral varus osteotomy alter the natural evolution of Perthes’ disease? J Pediatr Orthop B. 2005;14:10–15.
Joseph B, Varghese G, Mulpuri K, Narasimha Rao KL, Nair NS. Natural evolution of Perthes disease: a study of 610 children under 12 years of age at disease onset. J Pediatr Orthop. 2003;23:590–600.
Kamegaya M, Saisu T, Ochiai N, Hisamitsu J, Moriya H. A paired study of Perthes’ disease comparing conservative and surgical treatment. J Bone Joint Surg Br. 2004;86:1176–1181.
Kim HK. Legg-Calve-Perthes disease. J Am Acad Orthop Surg. 2010;18:676–686.
Klisic PJ. Treatment of Perthes’ disease in older children. J Bone Joint Surg Br. 1983;65:419–427.
Lack W, Feldner-Busztin H, Ritschl P, Ramach W. The results of surgical treatment for Perthes’ disease. J Pediatr Orthop. 1989;9:197–204.
Lahdes-Vasama TT, Marttinen EJ, Merikanto JE. Outcome of Perthes’ disease in unselected patients after femoral varus osteotomy and splintage. J Pediatr Orthop B. 1997;6:229–234.
Laurent LE, Poussa M. Intertrochanteric varus osteotomy in the treatment of Perthes’ disease. Clin Orthop Relat Res. 1980;150:73–77.
Leitch JM, Paterson DC, Foster BK. Growth disturbance in Legg-Calve-Perthes disease and the consequences of surgical treatment. Clin Orthop Relat Res. 1991;262:178–184.
Lloyd-Roberts GC, Catterall A, Salamon PB. A controlled study of the indications for and the results of femoral osteotomy in Perthes’ disease. J Bone Joint Surg Br. 1976;58:31–36.
McAndrew MP, Weinstein SL. A long-term follow-up of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1984;66:860–869.
McElwain JP, Regan BF, Dowling F, Fogarty E. Derotation varus osteotomy in Perthes disease. J Pediatr Orthop. 1985;5:195–198.
Mose K. Methods of measuring in Legg-Calve-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;150:103–109.
Mose K, Hjorth L, Ulfeldt M, Christensen ER, Jensen A. Legg Calve Perthes disease. The late occurence of coxarthrosis. Acta Orthop Scand Suppl. 1977;169:1–39.
Mukherjee A, Fabry G. Evaluation of the prognostic indices in Legg-Calve-Perthes disease: statistical analysis of 116 hips. J Pediatr Orthop. 1990;10:153–158.
Norlin R, Hammerby S, Tkaczuk H. The natural history of Perthes’ disease. Int Orthop. 1991;15:13–16.
O’Hara JP, Davis ND, Gage JR, Sundberg AB, Winter RB. Long-term follow-up of Perthes’ disease treated nonoperatively. Clin Orthop Relat Res. 1977;125:49–56.
Rowe SM, Moon ES, Song EK, Yoon TR, Kim MS, Cho SB. Residual shortening after Legg-Calve-Perthes disease, focusing on the response of the ipsilateral tibia. J Pediatr Orthop. 2005;25:296–299.
Salter RB, Thompson GH. Legg-Calve-Perthes disease. The prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. J Bone Joint Surg Am. 1984;66:479–489.
Slobogean GP, Verma A, Giustini D, Slobogean BL, Mulpuri K. MEDLINE, EMBASE, and Cochrane index most primary studies but not abstracts included in orthopedic meta-analyses. J Clin Epidemiol. 2009;62:1261–1267.
Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108.
Vila Verde VM, Gomes Peres JF, Costa BA. Value of the head-at-risk concept in assessing the prognosis in Legg-Calve-Perthes disease. J Pediatr Orthop. 1985;5:422–427.
Waldenström H. The Classic. The first stages of coxa plana by Henning Waldenström. 1938. Clin Orthop Relat Res. 1984;191:4–7.
Wang L, Bowen JR, Puniak MA, Guille JT, Glutting J. An evaluation of various methods of treatment for Legg-Calve-Perthes disease. Clin Orthop Relat Res. 1995;314:225–233.
Wiig O, Terjesen T, Svenningsen S. Prognostic factors and outcome of treatment in Perthes’ disease: a prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br. 2008;90:1364–1371.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (NS) has received research funding from DePuy Spine for work unrelated to this study. The institution of one or more of the authors (KM) has received funding from DePuy Spine for work unrelated to this study.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at BC Children’s Hospital, Vancouver, BC, Canada.
About this article
Cite this article
Saran, N., Varghese, R. & Mulpuri, K. Do Femoral or Salter Innominate Osteotomies Improve Femoral Head Sphericity in Legg-Calvé-Perthes Disease? A Meta-analysis. Clin Orthop Relat Res 470, 2383–2393 (2012). https://doi.org/10.1007/s11999-012-2326-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2326-3