Abstract
Background
Biomechanical studies suggest ulnohumeral chondral and ligamentous overload (UCLO) explains the development of posteromedial chondromalacia (PMC) in throwing athletes with ulnar collateral ligament (UCL) insufficiency. UCL reconstruction reportedly allows 90% of baseball players to return to prior or a higher level of play; however, players with concomitant posteromedial chondromalacia may experience lower rates of return to play.
Questions/purposes
The purpose of this investigation is to determine: (1) the rates of return to play of baseball players undergoing UCL reconstruction and posteromedial chondromalacia; and (2) the complications occurring after UCL reconstruction in the setting of posteromedial chondromalacia.
Methods
We retrospectively reviewed 29 of 161 (18%) baseball players who were treated for the combined posteromedial chondromalacia and UCL injury. UCL reconstruction was accomplished with the docking technique, and the PMC was addressed with nothing or débridement if Grade 2 or 3 and with débridement or microfracture if Grade 4. The mean age was 19.6 years (range, 16–23 years). Most players were college athletes (76%) and pitchers (93%). We used a modified four-level scale of Conway et al. to assess return to play with 1 being the highest level (return to preinjury level of competition or performance for at least one season after UCL reconstruction). The minimum followup was 24 months (mean, 37 months; range, 24–52 months).
Results
Return to play was Level 1 in 22 patients (76%), Level 2 in four patients (14%), Level 3 in two patients (7%), and Level 4 in one (3%) patient.
Conclusions
Our data suggest baseball players with concomitant PMC, may have lower rates of return to the same or a higher level of play compared with historical controls.
Level of Evidence
Level IV, case series. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the late cocking and early acceleration phases of the overhead throwing motion, the elbow is subjected to valgus moments associated with large forces to the medial structures of the elbow. Although several bony and soft tissue restraints normally maintain elbow stability, the anterior bundle of the ulnar collateral ligament (UCL) is the primary static restraint to valgus loads, which can reach up to 290 N resulting in angular velocity and may exceed 3000° per second [9, 10]. Repetitive overloading associated with the throwing motion can cause microscopic tears in the UCL with subsequent ligament attenuation and failure with the onset of degenerative changes, inability to throw, and chronic, disabling elbow pain in the overhead athlete [2, 5, 11, 24]. Cadaveric studies suggest valgus laxity may decrease contact area and increase peak contact stress in the elbow throughout the entire throwing motion, which may eventually lead to posteromedial impingement and subsequent chondromalacia [1, 15]. Osbahr and colleagues [15] recently introduced an expanded concept of medial elbow overload in overhead athletes termed ulnohumeral chondral and ligamentous overload (UCLO). This concept emphasizes how posteromedial elbow impingement in association with UCL insufficiency develops from abnormal contact pressures throughout the entire throwing motion and leads to chondromalacia.
Recent studies document that UCL reconstruction may reliably return athletes, including baseball players, to their previous level of play in approximately 80% to 90% of throwing athletes [5, 8, 12, 21, 23]. Despite these high rates of return to athletics, several studies suggest high school athletes, patients who have undergone prior elbow surgery, and patients with combined flexor-pronator injuries have lower rates of return to play (74%, 33%, and 12.5%, respectively) [7, 16, 18]. We have observed a cohort of baseball players who have a concomitant posteromedial chondromalacia, which may potentially affect outcomes after UCL reconstructive surgery. This posteromedial chondromalacia will typically involve the distal humerus within the posteromedial trochlea or olecranon fossa.
Therefore, we determined: (1) the rates of return to play of baseball players undergoing UCL reconstruction and posteromedial chondromalacia; and (2) the complications occurring after UCL reconstruction in the setting of posteromedial chondromalacia.
Patients and Methods
We identified all 161 baseball players who had UCL reconstructions performed by one surgeon (DWA) for UCL insufficiency. The indications for surgery were (1) a history of medial elbow pain that prevented throwing activities; (2) clinically apparent UCL insufficiency; (3) a preoperative MRI consistent with UCL injury; and (4) an overhead throwing athlete. From the total patient population of 161 patients undergoing UCL reconstruction for isolated UCL insufficiency, we identified 29 (18%) patients with concomitant posteromedial chondromalacia (UCL/PMC). The mean age of the baseball players was 19.6 years (range, 16–23 years). Most players were college athletes (76%) followed by high school (17%) and professional athletes (7%). In addition, most of the baseball players were pitchers (93%) with only one infielder and one catcher. Therefore, most of the UCL/PMC cases were college pitchers (72%). The minimum followup was 24 months (mean, 37 months; range, 24–52 months). No patients were lost to followup. No patients were recalled specifically for this study. All data were obtained from medical records and imaging, and return to play outcomes were confirmed with an Internet search of three professional baseball website databases (Major League Baseball, Minor League Baseball, and the Baseball Cube websites) as previously described [16, 20]. We obtained Institutional Review Board approval for this study.
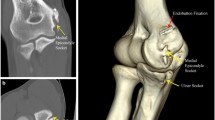
The diagnosis of UCL insufficiency and PMC was based on history, physical examination, and noncontrast MRI examination. In addition to the previously mentioned indication criteria, the presence of PMC was suggested by positive posteromedial impingement signs, which include posteromedial pain and/or crepitation when a valgus force is applied while the arm is in extension [13, 14, 24]. From the medical records, we extracted demographic information, including age, hand dominance, position, and preinjury level of play. In addition, we obtained findings from the clinical history (ability to play, presence and location of elbow pain, and symptom chronicity) and physical examination (ROM, valgus stress test, posteromedial impingement test, ulnar nerve symptoms) (Table 1). All baseball players underwent at least one preoperative MRI scan of the involved elbow, which was evaluated by one of several musculoskeletal radiologists and confirmed by one orthopaedic sports medicine surgeon. All structures of the elbow were evaluated on MRI with special attention dedicated to assessing ulnar collateral ligament status and the presence of PMC and osteophytes (Fig. 1). All clinical and MRI diagnoses were subsequently confirmed at the time of surgery during arthroscopic and open surgical reconstruction.
An arthroscopic examination was first performed in all patients followed by UCL reconstruction through a flexor-pronator muscle-splitting approach as previously described by Dodson and colleagues [8]. Surgical examination included an assessment of the arthroscopic valgus stress test, direct visualization of all chondral surfaces, documentation of the presence of osteophytes, status of the UCL, and type of graft in all patients. In particular, the UCL injury was assessed for injury, and chondromalacia was documented according to the modified Outerbridge classification (Grade 0, normal cartilage; Grade 1, cartilage softening and swelling; Grade 2, mild surface fibrillation and/or less than 50% loss of cartilage thickness; Grade 3, severe surface fibrillation and/or loss of more than 50% of cartilage thickness but without exposure of subchondral bone; Grade 4, complete loss of cartilage with subchondral bone exposure) [22].
Chondromalacia location was first recorded, and chondromalacia was subsequently addressed with no treatment in Grade 1, no treatment or débridement if Grade 2 or 3, and débridement or microfracture if Grade 4. The existence of osteophytes was then noted as present or absent. After all abnormalities were confirmed at the time of surgery, UCL reconstruction with or without PMC treatment was undertaken. Several operative variables were then evaluated, including type of UCL reconstructive autograft, the presence of chondromalacia and osteophytes, and performance of an ulnar nerve transposition (Table 2). If indicated by preoperative clinical symptoms, an ulnar nerve transposition was performed. Graft reconstruction was accomplished with 17 (59%) ipsilateral palmaris autografts, five (17%) contralateral palmaris, and seven (24%) contralateral hamstring autografts. Seventeen (59%) of the baseball players had Grade 2 chondral lesions followed by 10 (34%) patients with Grade 4 chondral lesions and two (7%) with Grade 3 chondral lesions. Of the 19 patients with Grade 2 or 3 chondromalacia, six (32%) were not treated and 13 (68%) were treated with isolated débridement (Fig. 2A–B). For the 10 patients with Grade 4 chondromalacia, two (20%) were treated with isolated débridement and eight (80%) were treated with microfracture (Fig. 3A–B). When osteophytes were present, isolated débridement/excision was performed in 20 (95%) patients (Fig. 4A–B). No osteophyte débridement/excision was performed in one (5%) patient. Three (10.3%) of the patients had an ulnar nerve transposition.
The postoperative protocol for all patients, as previously described, was the same regardless of the presence of posteromedial chondromalacia at the time of UCL reconstruction [8].
The arm was kept in a splint for 1 week in the immediate postoperative period. After 1 week, the sutures were removed and the elbow was managed in a hinged brace for approximately 3 additional weeks. The brace allowed motion from 45° of extension to 90° of flexion. Motion was then slowly advanced to full over the next 5 weeks. If the palmaris longus was used as the graft, wrist motion was encouraged. At approximately 6 weeks, supervised physical therapy was initiated at least three times per week and the brace was discontinued. Forearm and rotator cuff strengthening exercises were instituted to correct any loss of upper extremity motion. Flexor-pronator strengthening was performed in a conservative manner to strengthen but prevent subsequent overload and tendonitis. Patients typically started an interval throwing program for baseball players at the fourth postoperative month [19]. Players were not allowed to start pitching again competitively until at least 9 months after surgery.
Patients were scheduled for standard postoperative visits, including 2 weeks, 6 weeks, 4 months, and annual visits. Only clinical history and physical examinations were performed as part of the standard visit, and conventional radiographs were obtained on an annual basis. At each visit we assessed all patients using the scale by Conway et al. [5] as modified by Dines et al. [6] to account for return to play as based on one baseball season and not on an arbitrary 12-month time period. This scale subdivides outcomes based on level of return to play: Level 1—return to preinjury level of competition or performance for at least one season after UCL reconstruction; Level 2—return to play at a lower level of competition or performance for more than one season or able to throw daily batting practice; Level 3—able to play recreationally; and Level 4—unable to return to previous sport at any level. All operative and postoperative complications, including reoperations, were also recorded. Minor complications consisted of transient ulnar neuropathy and posteromedial impingement that resolved without a reoperation. Major complications consisted of permanent ulnar neuropathy and any reoperation.
Results
Twenty-two patients (76%) returned to play at Level 1, four (14%) at Level 2, two (7%) at Level 3, and one (3%) at Level 4 (Table 3). The patient who was unable to return to play was a 19-year-old college baseball player who developed calcification and proximal tearing of the UCL graft. He required revision reconstruction but decided against return to play. The two fair outcomes occurred in collegiate players who were able to return to throwing on only a recreational basis.
There were no operative complications. Postoperative complications were reported in four (14%) patients, including one minor and three major complications. The one minor complication included transient ulnar neuropathy, which resolved by 4 months postoperatively. The three (10%) major complications resulted in three reoperations, including two patients with postoperative posteromedial impingement and one patient with ulnar nerve symptoms. The two patients with posteromedial impingement had large osteophytes that were débrided during the initial surgery. They developed recurrent posteromedial impingement despite valgus stability with no pain related to the UCL.
Discussion
UCL insufficiency can be a potentially career-ending injury in baseball players. With modern surgical techniques, however, ligament reconstruction can reliably return athletes to their previous level of play 80% to 90% of the time [3–5, 8, 12, 21, 23]. Despite a high rate of return to play after UCL reconstruction, several studies have described subgroups of patients with lower rates of return to play using the scale of Conway et al. [5]: high school athletes (74% Level 1), revision patients undergoing UCL reconstruction (33% Level 1), and baseball players with concomitant flexor-pronator injuries (12.5% Level 1) [5, 7, 16, 18]. Because a thrower’s elbow is subjected to repetitive, valgus stresses in the setting of an incompetent UCL, abnormal contact pressures in the posteromedial elbow may also lead to chondromalacia from UCLO resulting in varying outcomes for return to play [15]. We have observed a cohort of baseball players who have a concomitant PMC, which may potentially affect outcomes after UCL reconstructive surgery. Therefore, we determined: (1) the rates of return to play of baseball players undergoing UCL reconstruction and posteromedial chondromalacia; and (2) the complications occurring after UCL reconstruction in the setting of posteromedial chondromalacia.
Several limitations should be considered when evaluating the results of this study. First, this study was retrospective, and we used no consistent treatment algorithm for specific chondral lesion grades. Because there are limited numbers of patients within each treatment group, we are not able to distinguish any differences in return to play as based on treatment. Considering the low incidence of these chondral lesions, it would be interesting but extremely difficult to perform a prospective and randomized study based on observation, débridement, and microfracture. Second, we did not identify Grade 1 chondromalacia because this was not specifically reported in the medical records. Despite this lack of information, Grade 1 chondromalacia has minimal to no chondral wear and we think unlikely to affect return to play alone. Because Grade 1 chondromalacia with chondral softening could be missed if not specifically probed during arthroscopy, the incidence and comparative outcomes of these lesions would also be ideal to understand if early identification of PMC in pathologic process is predictive of early disease and has any specific implications. Third, our study includes only short-term followup, and these chondral changes may have important long-term implications for return to play.
Return to play after UCL reconstruction has been evaluated in several studies using many techniques [3–5, 8, 12, 21, 23]. Overall, UCL reconstruction using the docking technique can reliably return athletes to their previous level of play approximately 90% of the time [8, 12, 17, 21, 23]; however, baseball players with concomitant PMC have not been historically evaluated as a subgroup. Our observations showed that only 76% of baseball players returned to the same or higher level of play after UCL reconstruction in the setting of PMC. The sentinel study by Conway and colleagues [5] and the largest UCL reconstruction series by Cain and colleagues [4] comment on the presence on osteophytes but not specifically chondromalacia. In addition, they do not discuss outcomes related to return to play when PMC is present within the elbow.
We found similar complications to those previously reported in the literature [3–5, 8, 12, 21, 23]. The recent study by Cain et al. [4] reports an overall 20% complication rate, including 16% minor and 4% major. All of the minor complications in the study by Cain et al. were related to transient ulnar neuropathy, which was higher than those reported in our study. As opposed to the docking technique, which includes optional ulnar nerve transposition, their technique is associated with an obligatory ulnar nerve transposition. These differences are likely not clinically important, because our study only had a limited number of patients. In fact, both of our studies reported only one case of ulnar neuropathy that required revision surgery.
After UCL reconstruction, baseball players with combined PMC and UCL injuries secondary to UCLO obtain slightly lower rates for return to play when compared with patients with isolated UCL tears that have been reported in the literature. Although prognosis may be minimally affected by PMC, intraoperative attention is necessary to assure proper recognition and treatment because there may be implications for long-term return to play.
References
Ahmad CS, Park MC, Elattrache NS. Elbow medial ulnar collateral ligament insufficiency alters posteromedial olecranon contact. Am J Sports Med. 2004;32:1607–1612.
Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16–23.
Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19(suppl):110–117.
Cain EL Jr, Andrews JR, Dugas JR, Wilk KE, McMichael CS, Walter JC 2nd, Riley RS, Arthur ST. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426–2434.
Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83.
Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044.
Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36:1061–1065.
Dodson CC, Thomas A, Dines JS, Nho SJ, Williams RJ 3rd, Altchek DW. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34:1926–1932.
Feltner ME. Three-dimensional interactions in a two-segment kinetic chain, part II: application to the throwing arm in baseball pitching. Int J Sport Biomech. 1989;5:420–450.
Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239.
Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158–1163.
Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22:1187–1191.
Miller CD, Savoie FH 3rd. Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg. 1994;2:261–269.
Moskal MJ. Arthroscopic treatment of posterior impingement of the elbow in athletes. Clin Sports Med. 2001;20:11–24.
Osbahr DC, Dines JS, Breazeale NM, Deng XH, Altchek DW. Ulnohumeral chondral and ligamentous overload: biomechanical correlation for posteromedial chondromalacia of the elbow in throwing athletes. Am J Sports Med. 2010;38:2535–2541.
Osbahr DC, Swaminathan SS, Allen AA, Dines JS, Coleman SH, Altchek DW. Combined flexor-pronator mass and ulnar collateral ligament injuries in the elbows of older baseball players. Am J Sports Med. 2010;38:733–739.
Paletta GA Jr, Wright RW. The modified docking procedure for elbow ulnar collateral ligament reconstruction: 2-year follow-up in elite throwers. Am J Sports Med. 2006;34:1594–1598.
Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32:1158–1164.
Reinold MM, Wilk KE, Reed J, Crenshaw K, Andrews JR. Interval sport programs: guidelines for baseball, tennis, and golf. J Orthop Sports Phys Ther. 2002;32:293–298.
Reynolds SB, Dugas JR, Cain EL, McMichael CS, Andrews JR. Débridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res. 2008;466:614–621.
Rohrbough JT, Altchek DW, Hyman J, Williams RJ 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–548.
Uhl M, Allmann KH, Tauer U, Laubenberger J, Adler CP, Ihling C, Langer M. Comparison of MR sequences in quantifying in vitro cartilage degeneration in osteoarthritis of the knee. Br J Radiol. 1998;71:291–296.
Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1193–1205.
Wilson FD, Andrews JR, Blackburn TA, McCluskey G. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83–88.
Acknowledgment
Joseph T. Nguyen was partially supported by the Clinical Translational Science Center (UL1-RR024996).
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
About this article
Cite this article
Osbahr, D.C., Dines, J.S., Rosenbaum, A.J. et al. Does Posteromedial Chondromalacia Reduce Rate of Return to Play After Ulnar Collateral Ligament Reconstruction?. Clin Orthop Relat Res 470, 1558–1564 (2012). https://doi.org/10.1007/s11999-011-2132-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2132-3