Abstract
Background
A concern regarding reverse shoulder arthroplasty (RSA) is the possibly higher complication rate compared with conventional unconstrained shoulder arthroplasty.
Questions/purposes
We determined (1) the rate of instability and infection; (2) whether diagnosis influenced instability and infection rates; and (3) whether these complications affect ASES, Constant, and WOOS scores after RSA.
Methods
A prospective database, clinical charts, and radiographs of 284 patients who had undergone primary (n = 212 patients) or revision (n = 72 patients) RSA were reviewed to identify patients whose postoperative course was complicated by instability or infection.
Results
The rate of instability was similar in patients with primary (eleven of 212 [5%)] and revision (six of 72 [8%]) reverse arthroplasty. The rate of infection was higher in the revision (five of 72 [7%]) than in the primary (three of 212 [1%]) group. Patients with an irreparable subscapularis tendon had a higher rate of instability (14 of 123 [12%]) compared with patients with a repairable subscapularis tendon (one of 161 [less than 1%]). The fracture sequelae group had the highest rate of instability (seven of 25 [28%]) among diagnoses within the primary group. The rates of infection were similar between the diagnoses within the primary group. The improvements in the ASES score, the Constant score, and the WOOS score from preoperatively to postoperatively were better in the no instability/infection group as compared with the instability/infection group.
Conclusions
This information confirms the available literature allowing surgeons to give patients realistic expectations regarding the infection and instability rates after RSA.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
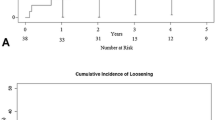
Reverse shoulder arthroplasty (RSA) was initially introduced in the 1970s to treat cuff tear arthropathy [1]. These initial RSA designs had a laterally offset center of glenohumeral rotation that led to a high rate (26%) of glenoid component loosening and failure [1]. In the early 1980s, Paul Grammont introduced a novel RSA designed with a “glenosphere” that medialized the center of rotation to within the bone of the glenoid and the era of modern RSA was born [8].
Since its approval in the United States in 2004, the use of RSA has become increasingly common in North America [5]. This increase in use has been accompanied by concern regarding the fact that the complication rate of RSA is higher than that of conventional unconstrained shoulder arthroplasty. Postoperative complications after RSA occur in up to 50% of patients in some series [18]. The two most common and major complications related to RSA are instability and infection [17]. Instability rates from 2% to 31% and infection rates from 1% to 15% have been reported [1, 2, 4, 6, 9, 10, 13–19]. One of the largest series in the literature to date contains 199 patients from two surgeons with an instability rate of 8% and an infection rate of 4% [17].
We evaluated our large prospective database to confirm the rates of instability and infection in RSA reported in other series. We determined (1) the rate of instability and infection; (2) whether diagnosis influenced instability and infection rates; and (3) whether these complications affect survey scores for self-perceived shoulder function after RSA.
Patients and Methods
We queried a prospective database and identified 284 patients who had undergone primary (n = 212 patients) or revision (n = 72 patients) RSA; all were included in this study. There were 108 males (38%) and 176 females (62%). RSA was performed on the dominant extremity in 168 patients (59%). The average age of the patients was 66.0 years (range, 35–93 years) at the time of surgery. After reviewing the database, the patients’ radiographs, and their clinical charts (surgical history, comorbidities, etc), these patients undergoing RSA were divided into a primary RSA group and a revision RSA group. The primary RSA group was further subdivided by etiology into 10 diagnostic categories. The diagnostic categories for primary RSA were primary cuff tear arthropathy (119), massive rotator cuff tears with pseudoparalysis (25), fracture sequelae (25), acute fractures (16), inflammatory arthropathies (ie, rheumatoid arthritis) (five), instability arthropathy (11), postinfectious arthropathy (six), tumor reconstructions (two), glenohumeral arthritis after radiation therapy (one), and primary glenohumeral arthritis (two). The revision RSA cases had all failed prior shoulder arthroplasty (total or hemiarthroplasty) and lacked a functioning rotator cuff. The minimum followup was 12 months postoperatively (average, 24 months; range, 12–48 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Our database of clinical and operative data for all patients undergoing arthroplasty was also queried, which was approved by the Institutional Review Board at our institution.
The sample size of 284 patients had 90% power with a Type I error rate ≤ 0.05 to find a difference in preoperative to postoperative change on the American Shoulder and Elbow Surgeons (ASES) score of 10 points or greater (ie, larger than the reported minimal clinically relevant difference of 9.7 points) on the ASES survey score using the reported population standard deviation for the ASES survey of 17 points. To maintain statistical power, the instability and infection groups were combined into an instability/infection (ie, complications) group to compare with the patients with no instability/infection (ie, no complications).
The Aequalis (Tornier, Edina, MN) RSA system was used in all patients. In all patients, the reverse prosthesis was implanted through the deltopectoral approach, except for two patients, who underwent a superior approach for concomitant repair of a deltoid detachment. The deltopectoral approach was used because of its familiarity, because it affords excellent exposure of the glenoid allowing inferior placement of the glenosphere and because it can be extended into an extensile exposure if required. The coracoacromial ligament and superior 1 cm of the pectoralis major were released and tenodesis or tenotomy of the long head of the biceps tendon was performed in all patients. The subscapularis tendon, if intact at the time of surgery, was transected using a transtendinous tenotomy and was circumferentially released to increase postoperative external rotation and facilitate repair. The status of the subscapularis tendon and whether it was repairable were assessed and recorded at the time of surgery. When repair was possible, a combined transosseous and transtendinous subscapularis repair was completed using a high-tensile strength nonabsorbable number 2 suture. Preparation of the glenoid included reaming an inferior tilt of 10° and a 36-mm glenosphere was used universally. The choice of a 36-mm glenosphere was based on the fact that this size glenosphere fits most patients. Although a 42-mm glenosphere is certainly more stable, its large size precludes its use in many patients. The humeral implant was cemented in 10° of retroversion in all patients. The “correct” version, however, is unknown because the RSA is a nonanatomic implant. Deltoid tension was assessed with the patient under complete neuromuscular paralysis. Humeral component length was increased using incrementally sized polyethylene spacers until axial motion between the glenosphere and the humeral component was less than 2 mm with longitudinal traction. A closed suction drain was placed at the time of wound closure and removed the day after surgery in all cases to minimize hematoma formation. All patients received antibiotic prophylaxis preoperatively and for 24 hours postoperatively.
After reverse shoulder arthroplasty, patients were seen at 1 week, 6 weeks, 3 months, 6 months, and 1 year. Radiographs were performed at every visit including AP in the plane of the scapula, scapular Y, and axillary views. Clinical parameters assessed were ROM, strength, and rotator cuff testing. All patients wore a neutral rotation brace for 3 to 4 weeks before beginning physical therapy. After this period, the patients participated in aquatic therapy rehabilitation whenever possible to improve shoulder ROM. Therapy was directed to improve elevation, extension, horizontal adduction, external rotation, and then internal rotation in succession. Patients who were unable to participate in aquatic therapy participated in a land-based regimen with the same objectives. After at least 6 weeks of aquatic or other therapy, if acceptable ROM was gained, patients graduated to a self-directed land-based program. Strengthening exercises were not prescribed for any patient.
Instability and infection rates were calculated using information from the database; these rates were substantiated by information in the patients’ radiographs and clinical charts. Functional survey scores, including the American Shoulder and Elbow Surgeons’ scores [12], Constant and adjusted Constant scores [3], Single Assessment Numerical Evaluation scores [20], and Western Ontario Osteoarthritis of the Shoulder (WOOS) scores [11] were also obtained from the database. One hundred forty-one of the 284 patients (50%) had complete preoperative and postoperative measures, 10 of whom were in the instability and infection group, at an average of 24 months postoperatively (range, 12–48 months). Although the patients are entered into the database prospectively, the completeness of their data relied on patient followup. It is for this reason that only half of the patients had complete data.
Frequencies and means were used to describe patient characteristics, and the characteristics were compared between groups using chi square analyses or t-tests as appropriate to the scale and distribution of the respective variables. Proportions were used to describe infection and instability rates. We evaluated the differences in infection and instability rates between the primary and revision groups using chi square analyses with exact probabilities. The differences in preoperative to postoperative survey scores were compared between patients with and without complications using two-way analysis of variance with repeated measures. There was no evidence of violations of the assumptions of these tests.
Results
The rate of instability was similar (p = 0.388) in patients with primary (11 of 212 [5%]) and revision (six of 72 [8%]) arthroplasty. The rate of infection was higher (p = 0.030) in the revision (five of 72 [7%]) than in the primary (three of 212 [1%]) group. The average age of patients in the instability/infection group was 62.8 ± 11.8 years, which was lower (p = 0.012) than the no instability/infection group (69.1 ± 10.7 years). Age was not related to the rates of either instability (p = 0.116) or infection (p = 0.703). Males compared with females had over twice the rate of instability (9% versus 4%) and infections (4% versus 2%). Surgery in the dominant extremity (n = 168 [59%]) was not a risk factor for instability or infection (p = 0.462). The proportion of patients with recorded medical comorbidities were similar in the instability/infection group and the no instability/infection group. Of the 20 patients in our series whose postoperative course was complicated by instability or infection, five (25%) patients’ postoperative courses were complicated by both. Of these five patients, three went on to resection arthroplasty, one has a dislocated and chronically infected RSA and is considering treatment options, and one has retained the prosthesis but is on chronic suppressive antibiotics (Tables 1, 2, 3, 4).
Patients with subscapularis tendon insufficiency at surgery (irreparable subscapularis tendon) had a higher (p < 0.001) rate of instability (14 of 123 [12%]) compared with patients with a repairable subscapularis tendon (one of 161 [less than 1%]). For the evaluation of the effect of diagnosis within the primary cases group, the following diagnostic groups were excluded because there were too few subjects in those groups (six or less) for meaningful statistical comparisons: inflammatory arthropathies (ie, rheumatoid arthritis), postinfectious arthropathy, tumor reconstructions, glenohumeral arthritis after radiation therapy, and primary glenohumeral arthritis. Only one case of instability occurred in all of these groups. These patients were included in all other aspects of the analysis. Thus, these analyses were conducted using the primary cuff tear arthropathy, massive rotator cuff tears with pseudoparalysis, fracture sequelae, acute fractures, and instability arthropathy diagnostic groups, representing 94% of all cases. The fracture sequelae group had a higher (p < 0.001) rate of instability (seven of 25 [28%]) than the other four groups combined (three of 171 [2%]). The instability arthropathy and massive rotator cuff tears with pseudoparalysis groups had higher (p = 0.015) rates of instability (three of 36 [8%]) relative to the acute fracture and cuff tear arthropathy groups, who had no instability (0%). The rates of infection were similar between the diagnoses within the primary group.
The improvements in the ASES score, the Constant score, and the WOOS score from preoperatively to postoperatively were better in the no instability/infection group as compared with the instability/infection group (Table 5). Age and time to followup (range, 1–5 years) were unrelated (p > 0.05) to any of the survey measures.
Discussion
Through the use of a large single-surgeon prospective database we confirmed (1) the rate of instability and infection; (2) whether diagnosis influenced instability and infection rates; and (3) whether these complications affect survey scores for self-perceived shoulder function after RSA.
This study has several limitations. First, although the overall number of patients undergoing RSA was substantial (n = 284), the number of patients affected by instability or infection was relatively low (n = 20), which limits statistical power. Nevertheless, we identified some factors that were related to the occurrence of these complications. Second, functional survey data were only available on 10 patients in the infection/instability group making it difficult to generalize to the RSA population in general, although we did observe large decrements in functional survey scores in that small group that may be indicative of the potential magnitude of effects resulting from complications after RSA.
With an overall infection rate of 3% and an instability rate of 6% we were able to confirm the reported infection and instability rates available in the literature [1, 2, 4, 6, 9, 10, 13–19]. The relevance of these data lies in the fact that this is the largest single-surgeon cohort in the literature to date with over 280 patients (Table 6).
The rate of instability was similar in the primary and revision groups but was affected by the preoperative diagnosis within the primary group. The effect of diagnosis may be partially attributable to the status of the subscapularis tendon at the time of surgery. Edwards et al. have previously reported the risk of dislocation after RSA was nearly twice as high in patients with an irreparable subscapularis tendon compared with those with a repaired subscapularis tendon [5]. As one would expect, because this report is an analysis of the same cohort, an irreparable subscapularis tendon at the time of surgery led to a significantly higher rate of instability in this series. In only one of the 17 cases of instability was the subscapularis tendon able to be repaired. The fracture sequelae diagnostic group had the highest rate of instability followed by the instability arthropathy and massive rotator cuff tear with pseudoparalysis diagnostic groups, whereas the acute fracture and cuff tear arthropathy diagnostic groups had no cases of instability. This is likely the result of the ability to better manage the subscapularis tendon in the patients with cuff tear arthropathy and acute fracture. The subscapularis tendon is usually difficult to manage in patients affected by fracture sequelae because their tuberosities are usually malunited, nonunited, or reabsorbed leading to mechanical impingement as well as subscapularis insufficiency. In addition, patients with fracture sequela have contractures and proximal humeral bone loss further exacerbating their instability. In patients with massive rotator cuff tears with pseudoparalysis and instability arthropathy, the subscapularis tendon is generally involved in the massive rotator cuff tears frequently associated with these conditions [7].
To the best of our knowledge there are no reports in the literature about how instability and infection affect survey scores for self-perceived shoulder function after RSA. It is intuitive, however, to believe patients affected by instability and infection after RSA would have worse survey scores than those without these postoperative complications. In the study group not affected by instability and infection the change in total Constant score from preoperative to postoperative (15 to 60) is similar to that reported in the literature (22 to 59) [17]. Likewise, the group without complications had favorable changes in their ASES scores (56 to 75) compared with the literature (34 to 68) [6]. In our study group affected by instability/infection, their change in total Constant scores (14 to 42) and ASES scores (55 to 61) from preoperative to postoperative were much less favorable when compared with the group without complications or the literature.
With the largest study to date on instability and infection after RSA, we have confirmed the infection and instability rates available in the literature, demonstrated how these complication rates can be affected by preoperative diagnosis, and shown the affects of these complications on survey scores for self-perceived shoulder function. This information allows surgeons to give patients realistic expectations regarding these complications and can be used during preoperative counseling to predict how likely they are to occur given the preoperative diagnosis. Additionally, these data can help manage expectations after these complications with respect to the ultimate outcome after RSA complicated by infection or instability.
References
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14(Suppl S):147S–161S.
Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2002;25:129–133.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164.
De Wilde L, Sys G, Julien Y, Van Ovost E, Poffyn B, Trouilloud P. The reversed Delta shoulder prosthesis in reconstruction of the proximal humerus after tumour resection. Acta Orthop Belg. 2003;69:495–500.
Edwards TB, Williams MD, Labriola JE, Elkousy HA, Gartsman GM, O’Connor DP. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:892–896.
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The Reverse Shoulder Prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697–1705.
Gartsman GM, Edwards TB. Shoulder Arthroplasty. 1st ed. Philadelphia: WB Saunders Elsevier; 2008.
Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68.
Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88:1742–1747.
Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89:292–300.
Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: The Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9:771–778.
Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594.
Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg. 2001;10:17–22.
Sirveaux F, Favard L, Oudet D, Huguet D, Lautman S. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive and nonrepairable cuff rupture. In: Walch G, Boileau P, Mole D, eds. Shoulder Prosthesis: Two to Ten Year Follow-up. Montpellier, France: Sauramps Medical; 2001:247–252.
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395.
Valenti PH, Boutens D, Nerot C. Delta 3 reversed prosthesis for osteoarthritis with massive rotator cuff tear: long-term results (> 5 years). In: Walch G, Boileau P, Mole D, eds. Shoulder Prosthesis: Two to Ten Year Follow-up. Montpellier, France: Sauramps Medical; 2001:253–259.
Wall B, Nove-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485.
Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486.
Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop Relat Res. 2009;467:225–234.
Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214–221.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (TBE) received in any 1 year outside funding or grants in excess of $10,000 from Tornier.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Trappey, G.J., O’Connor, D.P. & Edwards, T.B. What Are the Instability and Infection Rates After Reverse Shoulder Arthroplasty?. Clin Orthop Relat Res 469, 2505–2511 (2011). https://doi.org/10.1007/s11999-010-1686-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1686-9