Abstract
Background
High rates of heterotopic ossification have been associated with hip resurfacing as compared to THA. Bone debris from femoral head reamings is cited as one of the risk factors linked to increased rates of heterotopic ossification.
Questions/purposes
We therefore asked whether (1) the incidence of heterotopic ossification differed with and without the use of a plastic drape used to collect bone debris and (2) any of a number of variables (age, gender, diagnosis, previous hip surgery, operative time, and blood loss) related to the occurrence of HO.
Methods
We retrospectively reviewed 136 hip resurfacings performed using one of two techniques: Group 1 contained 64 hip resurfacings performed using a sterile drape around the femoral neck while reaming the femoral head to collect bone debris; Group 2 contained 72 hip resurfacings carried out with manually removing bone debris and utilizing a pulse lavage. Data were collected with respect to diagnosis, gender, previous surgery, postoperative complications, operative time, and blood loss to rule out confounding variables. The amount of heterotopic ossification was measured radiographically in hips after undergoing resurfacing arthroplasty. The minimum followup was 6 months (mean, 15 months; range, 6–27 months).
Results
No patient had heterotopic ossification of clinical importance and none had resection of the heterotopic ossification. Group 1 had a lower overall incidence of minor heterotopic ossification (32%) than Group 2 (58%). Risk factors linked to heterotopic ossification include male gender and operative time.
Conclusions
The use of a plastic drape to collect bone debris from femoral head reamings decreased the incidence of heterotopic ossification in resurfacing arthroplasty of the hip.
Level of Evidence:
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterotopic ossification (HO) is a common finding in radiographs of patients after THA and is an important complication that can compromise a patient’s function. The incidence of HO after THA in the literature ranges from 5% to 90%, but recent studies suggest an incidence of 32% to 67% [2, 8, 12, 22]. For some patients, HO is an incidental radiographic observation, but as many as 10% can experience functional impairments, such as pain and decreased ROM due to the inflammatory reaction produced by HO [22]. HO has also been associated with trauma, burns, genetic disorders, and soft tissue sarcomas [19, 26, 31]. The amount of HO differs greatly from small islands of bone within the soft tissues to bone spurs and ankylosis. Typically, the HO is asymptomatic, but a patient’s function can be influenced with higher degrees of ossification resulting in impairment of the hip arthroplasty due to impingement, instability, and decreased ROM [25, 34, 41]. HO occurs in the early postoperative course, becomes visible in 3 to 6 weeks, and matures in 3 months to 1 year [2, 33, 36]. In the first few months postoperatively, patients developing HO may suffer from symptoms of the inflammatory process, including local pain, mild edema, and erythema, which could be confused with infection [10, 16, 28]. Functional limitations are correlated to the severity of the heterotopic bone as described by Brooker et al. [12] with Grades III and IV deemed clinically important.
Hip resurfacing arthroplasty has undergone resurgence in recent years as a treatment for the young, active patient with osteoarthritis (OA) [5, 7, 14, 23, 47, 50]. The proposed advantages of hip resurfacing over THA include preservation of bone stock, restoration of hip biomechanics, lower dislocation rates, and more straightforward revisions [23, 49–51]. Complications associated with hip resurfacings include femoral neck fractures, avascular necrosis (AVN), increased metal ion levels, and increased incidence of HO [9, 23, 29, 42, 50]. Increased rates of HO have been linked to the extent of mechanical trauma at the time of surgery and have been positively correlated with the difficulty of the operation [3, 21]. Back et al. [8] prospectively reviewed 220 hip resurfacings with an overall HO rate of 58%. Two patients in the study underwent excision of HO for pain and stiffness, and one patient had resection for decreased ROM.
Surgeons cannot control patient-related risk factors for HO, including ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, male gender, previous hip surgery, and history of heterotopic bone, but surgical factors can be controlled [2, 3, 8, 18, 22, 25, 33, 35, 52–54, 58]. Surgical risk factors, including operative time, approach, difficulty of the procedure, soft tissue trauma, and bone debris, have been linked to increased rates of ectopic bone [2, 3, 8, 18, 20, 21, 25, 30, 33, 48, 53, 54]. Presuming bone debris is related to the frequency of HO, one of us (WGW) began using a sterile plastic drape to collect and contain bone debris during the preparation of the femoral head.
We therefore asked whether (1) the incidence of HO differed without and with the use of the plastic drape; and (2) any of a number of variables (age, gender, diagnosis, previous hip surgery, operative time, and blood loss) related to the occurrence of HO.
Patients and Methods
We identified and retrospectively reviewed all 149 hip resurfacing procedures performed by the two senior authors (WGW, RHJ) between June 2006 and May 2008. We excluded 13 patients revised to THA, five due to femoral neck fractures and two for acetabular loosening. No patients had a prior history of HO, and none received any form of HO prophylaxis. Six patients were lost to followup. This left 127 patients with 136 hip resurfacings. The patients were divided into two groups depending on whether a plastic drape had been used during the preparation of the femoral head: 60 patients (64 hips) with the drape and 67 patients (72 hips) without the drape. Before data collection, the adequate sample size was measured to be 130 (65 in each groups) based on the significance level of p < 0.05, power of 80%, and the targeted difference between the rate of HO in the two groups of 20%. This targeted difference of 20% was an arbitrarily chosen figure based on a reduction of rate of HO in patients with hip resurfacing from the previously published figure of 58% [8]. The actual power of the study after the data collection was analyzed for the main part of the study based on the difference in the rate of HO as a percentage of total resurfacings in each group, each sample size, and a confidence level of p < 0.05. The statistical power of the study was 0.86. The preoperative diagnosis included OA, AVN, posttraumatic arthritis, and arthritis secondary to dysplastic hip disease, with no cases of hypertrophic OA. The mean age at operation was 48 years (range, 19–66 years). There were 66 left and 70 right hips, 96 men and 31 women. Staged bilateral resurfacings included in the study were performed in nine patients. Prior surgeries, including core decompression, hip arthroscopy, intramedullary nailing, and open reduction internal fixation of acetabular and proximal femur fractures, had been performed on 12 patients receiving hip resurfacing on the ipsilateral side. None of these patients had HO resulting from their original surgery. The minimum followup was 6 months (mean, 15 months; range, 6–27 months). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
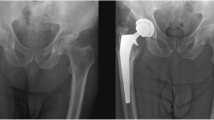
The procedures were carried out using a posterior approach with a 5–8 cm extended incision as compared to a standard THA approach. A capsulotomy was performed and the capsule completely released so that the femoral head could be displaced anteriorly and superiorly into a submuscular pocket to allow for acetabular exposure. The acetabulum was prepared with acetabular reamers and underreamed by 1 mm. Both surgeons implanted the acetabular components immediately after the acetabular preparation, and both surgeons prepared the femoral head similarly. A Steinmann pin was inserted with the help of the pin-centering guide or computer-assisted navigation. One surgeon (RHJ) usually prepared the femur first while the other (WGW) usually prepared the acetabulum first, unless the femoral head was excessively large, in which case he also prepared the femur first. Except for the following steps, the acetabular preparation and femoral head preparation were virtually identical. Both surgeons successively reamed and shaped the femoral head (Fig. 1), being careful to stop at the head-neck junction to avoid notching the superior aspect of the femoral neck. However, one surgeon (RHJ) manually removed bone debris using forceps and pulse lavage until the wound was clear of debris (Fig. 2) whereas the second surgeon (WGW) added an additional step before lavage in which he used a sterile plastic drape with a hole centered in the middle (3 M Health Care, St Paul, MN) to cover the entire wound, leaving the femoral head and neck exposed through the hole in the drape as described by Amstutz [4] (Fig. 3). The surgeon then proceeded to prepare the femoral head while the drape served to catch the majority of bone debris (Fig. 4). The drape containing the bone debris was then removed from the wound and placed onto the back table (Fig. 5) and any remaining bone debris was meticulously removed manually. Once components were placed, the hip was reduced and checked for stability and ROM, and the wound was copiously irrigated with normal saline using pulse lavage. Both surgeons manually débrided any devitalized or traumatized abductor muscle tissue (most commonly traumatized fibers of the gluteus minimus muscle) immediately before closure. The incisions were closed over a drain, and patients followed the same postoperative protocol. No specific postoperative regimen for prophylaxis against HO was administered in either group of patients.
The prosthesis used in all cases was the Birmingham Hip® Resurfacing prosthesis (Smith and Nephew, Memphis, TN). The components consist of a hydroxyapatite-backed acetabular component with a cemented femoral component. The cement used was Simplex® (Stryker Howmedica Osteonics, Kalamazoo, MI). The patients who underwent surgery by WGW and had a plastic drape for the collection of the bone debris during femoral head reaming were the treatment group (Group 1) (Fig. 4) and the group who had manual removal of bone debris operated on by RHJ were chosen as the control group (Group 2) (Fig. 2). Nursing, anesthesia records, and operative notes were reviewed to record blood loss and operative time.
Group 1 with the plastic drape technique consisted of 64 hips in 60 patients (Table 1). There were 47 men and 13 women; 45 hips had a diagnosis of OA and 15 hips a diagnosis of AVN. Two patients in this group had previous hip surgery, one with an intramedullary nail and the other status post open reduction internal fixation of a subtrochanteric femur fracture. The mean age at the time of surgery was 49 years (range, 23–65 years). Mean operative time was 153.7 minutes (range, 67–255 minutes), and mean blood loss was 354 mL (range, 100–1200 mL). Group 2 without the draping technique had 72 hip resurfacings in 67 patients (Table 1). There were 49 men and 18 women; 48 hips had a diagnosis of OA, 14 AVN, four posttraumatic arthritis, and one OA secondary to dysplastic hip disease. Ten patients in this group had previous hip surgery, including five patients with hip arthroscopy, three with status post open reduction internal fixation of acetabular fractures, one with intramedullary nail, and one with core decompression. The mean age at the time of surgery was 48 years (range, 20–67 years) with a mean operative time of 101.9 minutes (range, 55–170 minutes) and an average blood loss of 398 mL (range, 100–1900 mL).
Radiographs were taken with a standard magnification of 115%, digitized, and stored in a picture archiving and communication system. AP radiographs of the hip were taken preoperatively and at the immediate postoperative, 6-week, 6-month, and annual postoperative followups. Patients were seen in followup at 2 weeks for staple removal and then at 6 weeks, 3 months, 6 months, and 1 year for routine hip examination.
One of us (JSS) determined the presence of HO on the AP radiographs classified according to Brooker et al. [12]. The classification grades HO in four classes (Table 2). The reviewer was blinded to patient and surgeon and evaluated preoperative and immediate postoperative and followup radiographs. The films were evaluated to ensure patients with previous surgery did not have previous HO that would confound results and retained bone from the initial surgery seen in the immediate postoperative radiographs would not be considered HO. The Brooker classification system is a common rating scale for HO; however, Della Valle et al. [16] reported fair intraobserver reliability (κ = 0.74) and poor interobserver reliability (κ = 0.43).
The use of the plastic sterile drape as a specific risk factor for HO was evaluated. Rates of HO between Groups 1 and 2 were compared using z test with Yates correction applied to calculations. Multiple logistic regression analysis was performed to evaluate for statistically significant differences in other variables, including age, gender, diagnosis, operative time, blood loss, previous surgery, and postoperative infection. The data were compiled and tabulated using Microsoft® Excel® spreadsheets (Microsoft Corp, Redmond, WA). All statistical analyses were performed using SigmaStat® software (Systat Software Inc, San Jose, CA).
Results
The total rate of HO for all resurfacings was 46%, with 30% Brooker I, 9.6% Brooker II, and 8.8% Brooker III. Group 1 had a lower (p = 0.005) overall HO rate (32%), with 13 Brooker I, five Brooker II, and three Brooker III, than Group 2 (58%), with 25 Brooker I, eight Brooker II, and nine Brooker III (Table 2). There was no difference between the two groups when the HO was stratified by the level of severity using the Brooker classification.
We found no relationship of age, diagnosis, previous hip surgery, postoperative infection, and blood loss with surgical technique and HO. However, male gender (p = 0.004) and operative time (p = 0.046) were found to have a relationship with postoperative HO (Table 1).
Two patients in Group 1 had a postoperative course complicated by draining hematomas treated by irrigation and débridement along with intravenous antibiotics. None of the patients had revision or implant removal. One patient in Group 2 underwent irrigation and débridement of a superficial ulcer for a nonhealing wound postoperatively.
Discussion
With recent advances of metal-on-metal bearing surfaces, hip resurfacing has made a revival for the treatment of OA and AVN in the young, active population. THA is commonly associated with HO; however, hip resurfacings have been linked to increased rates of HO [3]. The exact pathogenesis of HO is unknown, but it is thought to result from the differentiation of mesenchymal cells into osteoprogenitor cells. To form heterotopic bone, there must be an inciting event such as surgery, a supply of mesenchymal cells such as bone debris, and a signal from the site of injury in an environment conducive to promoting the growth of heterotopic bone [2, 13, 26, 31]. HO can be experimentally induced by trauma to soft tissues, transplantation of living cells, or using extracts from bone such as BMP [1, 6, 19, 43, 55, 56]. Several authors have attributed bone dust as leading to the stimulation of HO [20, 25, 30, 33]. Ahrengart [2] and Sell et al. [48] proposed clearing the operative site of bone particles contributes to lower rates of HO. Our study proposed to evaluate whether a plastic drape used to limit the amount of bone debris deposited in the wound would decrease the rates of HO. Other risk factors for HO were also examined in this study, including age, gender, diagnosis, previous hip surgery, operative time, and blood loss.
Our study is subject to certain limitations. First, it is a retrospective review and the groups were not randomly selected. Second, this study is a review of two surgeons who might have had somewhat differing techniques. We believe the study would be ideally performed by a single surgeon in a random, prospective trial comparing plastic drape versus manual débridement alone. However, the two surgeons performed similar procedures with the exception of the use of the plastic sterile drape to collect bone debris. Each surgeon has HO rates in his THA population of 48%, the majority of which are Brooker I. As these two surgeons have similar rates of HO in their THA population, one can extrapolate similar techniques in the resurfacing approach should offer comparable rates of HO in their resurfacing population should the plastic drape not be used.
No patient had HO of any clinical importance and none had resection of the HO without or with the plastic drape. The majority of the HO seen in our population was Brooker I or II. Twelve patients did have Brooker III HO but had no functional limitations related to ROM, pain, or impingement. Brooker et al. [12] deemed Brooker III clinically important as increasing severity of ectopic bone has greater potential to cause such functional limitations and should raise clinical awareness when visualized on radiographs before examination, but we did not find these limitations in these 12 patients. The creation and removal of bone debris, considered a factor in development of HO, can be controlled by the surgeon. The ectopic bone is usually located lateral to the hip in the abductor musculature and about the tip of the greater trochanter, but it can be visualized medially, corresponding to the iliopsoas muscle and lesser trochanter [2, 15, 21, 44, 45]. This correlates to the location of HO we found. Rumi et al. [46] suggest osteoprogenitor cells responsible for HO originate from both the hip abductors and the femoral canal and the efficacy of local radiation indicates the osteogenic precursor cells are derived from local tissue rather than blood-borne cell lines. The femoral canal is not violated in hip resurfacings, but reaming and shaping the femoral head leave a substantial amount of bone debris that may supply the osteoprogenitor cells needed to stimulate bone growth within the soft tissues. The majority of these reamings are captured with the use of the plastic drape in an effort to limit the amount of bone debris deposited in the wound and decrease HO rates from 58% in Group 2 without the drape to 33% in Group 1.
Risk factors associated with HO in this study included operative time and male gender. Soballe et al. [53] and Hierton et al. [21] found increased duration of the operative procedure was linked to the formation of heterotopic bone. Toom et al. [54] quantified the operative time of 100 minutes as the critical time period above which there is a greater risk of HO. Hip resurfacing arthroplasty has been associated with increased rates of HO. Total rates of HO in our study were 46%, as compared to 33% in Group 1 and 58% in Group 2, with a rate of reported by Back et al. [8] of 58% (Table 3). Higher rates of HO in resurfacings are likely due to more surgical dissection, longer operative times, and increased difficulty as compared to THA [9, 23, 29, 50]. In our study, raw analysis of the data suggests otherwise. Group 1, using the draping technique to limit bone debris, had a higher mean operative time yet lower HO rates than Group 2 with shorter average operative times (52 minutes shorter) yet higher HO rates. This contradicts the literature, as we would expect higher rates of HO in Group 1 secondary to longer operative time, but Group 1 has lower rates of HO with the draping technique. Operative time independently predicted the formation of HO when both groups were pooled. This contradicts the literature and highlights the importance of the surgical technique, supporting our presumption that removal of bony debris during femoral preparation reduces the formation of HO. Male gender is also a risk factor for HO [2, 3, 18, 25, 39] and was a risk factor in our patient population. Numerous studies have looked at surgical approach in association with HO and reported trochanteric osteotomy is related to the highest incidence, while the posterior approach for THA is associated with the lowest incidence [18, 24, 25, 27, 33, 38]. Other reports by Duck and Mylod [17] and Morrey et al. [32] suggest no difference in HO formation and surgical approach used. HO prophylaxis is not without expense and complications, and surgical excision is an unwanted second procedure that has morbidity associated with it [11, 20, 27, 37, 39, 40, 57].
While patient risk factors cannot be controlled, our data suggest using a sterile plastic drape can decrease the incidence of HO by carefully collecting and limiting bone debris in the wound. We recommend using a plastic drape to capture femoral head reamings to limit the bone debris deposited in the wound and thus limit the formation of HO.
References
Aho HJ, Aro H, Juntunen S, Strengell L, Michelsson JE. Bone formation in experimental myositis ossificans: light and electron microscopy study. APMIS. 1988;96:933–940.
Ahrengart L. Periarticular heterotopic ossification after total hip arthroplasty: risk factors and consequences. Clin Orthop Relat Res. 1991;263:49–58.
Ahrengart L, Lindgren U. Heterotopic bone after hip arthroplasty: defining the patient at risk. Clin Orthop Relat Res. 1993;293:153–159.
Amstutz HC. Wright Conserve Plus Total Surface Arthroplasty Surgical Technique. Arlington, TN: Wright Medical Technology, Inc; 2003.
Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: surgical technique. J Bone Joint Surg Am. 2006;88:234–249.
Ashton BA, Allen TD, Howlett CR, Eaglesom CC, Hattori A, Owen M. Formation of bone and cartilage by marrow stromal cells in diffusion chambers in vivo. Clin Orthop Relat Res. 1980;151:294–307.
Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329.
Back DL, Smith JD, Dalziel RE, Young DA, Shimmin A. Incidence of heterotopic ossification after hip resurfacing. ANZ J Surg. 2007;77:642–647.
Back DL, Young DA, Shimmin AJ. How do serum cobalt and chromium levels change after metal-on-metal hip resurfacing? Clin Orthop Relat Res. 2005;438:177–181.
Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys. 2006;65:1289–1299.
Board TN, Karva A, Board RE, Gambhir AK, Porter ML. The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg Br. 2007;89:434–440.
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632.
Chalmers J, Gray DH, Rush J. Observations on the induction of bone in soft tissues. J Bone Joint Surg Br. 1975;57:36–45.
Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184.
DeLee J, Ferrari A, Charnley J. Ectopic bone formation following low friction arthroplasty of the hip. Clin Orthop Relat Res. 1976;121:53–59.
Della Valle AG, Ruzo PS, Pavone V, Tolo E, Mintz DN, Salvati EA. Heterotopic ossification after total hip arthroplasty: a critical analysis of the Brooker classification and proposal of a simplified rating system. J Arthroplasty. 2002;17:870–875.
Duck HJ, Mylod AG Jr. Heterotopic bone in hip arthroplasties: cemented versus noncemented. Clin Orthop Relat Res. 1992;282:145–153.
Eggli S, Woo A. Risk factors for heterotopic ossification in total hip arthroplasty. Arch Orthop Trauma Surg. 2001;121:531–535.
Ekelund A, Brosjo O, Nilsson OS. Experimental induction of heterotopic bone. Clin Orthop Relat Res. 1991;263:102–112.
Healy WL, Lo TC, DeSimone AA, Rask B, Pfeifer BA. Single-dose irradiation for the prevention of heterotopic ossification after total hip arthroplasty: a comparison of doses of five hundred and fifty and seven hundred centigray. J Bone Joint Surg Am. 1995;77:590–595.
Hierton C, Blomgren G, Lindgren U. Factors associated with heterotopic bone formation in cemented total hip prostheses. Acta Orthop Scand. 1983;54:698–702.
Higo T, Mawatari M, Shigematsu M, Hotokebuchi T. The incidence of heterotopic ossification after cementless total hip arthroplasty. J Arthroplasty. 2006;21:852–856.
Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years: an independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89:1431–1438.
Horwitz BR, Rockowitz NL, Goll SR, Booth RE Jr, Balderston RA, Rothman RH, Cohn JC. A prospective randomized comparison of two surgical approaches to total hip arthroplasty. Clin Orthop Relat Res. 1993;291:154–163.
Iorio R, Healy WL. Heterotopic ossification after hip and knee arthroplasty: risk factors, prevention, and treatment. J Am Acad Orthop Surg. 2002;10:409–416.
Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004;12:116–125.
Kjaersgaard-Andersen P, Ritter MA. Prevention of formation of heterotopic bone after total hip arthroplasty. J Bone Joint Surg Am. 1991;73:942–947.
Kjaersgaard-Andersen P, Schmidt SA, Pedersen NW, Kristensen SS, Pedersen P. Erythrocyte sedimentation rate and heterotopic bone formation after cemented total hip arthroplasty. Clin Orthop Relat Res. 1989;248:189–194.
Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:320–323.
Maloney WJ, Krushell RJ, Jasty M, Harris WH. Incidence of heterotopic ossification after total hip replacement: effect of the type of fixation of the femoral component. J Bone Joint Surg Am. 1991;73:191–193.
McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol. 2005;34:609–619.
Morrey BF, Adams RA, Cabanela ME. Comparison of heterotopic bone after anterolateral, transtrochanteric, and posterior approaches for total hip arthroplasty. Clin Orthop Relat Res. 1984;188:160–167.
Nayak KN, Mulliken B, Rorabeck CH, Bourne RB, Woolfrey MR. Prevalence of heterotopic ossification in cemented versus noncemented total hip joint replacement in patients with osteoarthrosis: a randomized clinical trial. Can J Surg. 1997;40:368–374.
Neal B. Effects of heterotopic bone formation on outcome after hip arthroplasty. ANZ J Surg. 2003;73:422–426.
Nilsson OS, Persson PE. Heterotopic bone formation after joint replacement. Curr Opin Rheumatol. 1999;11:127–131.
Nollen AJ, Slooff TJ. Para-articular ossifications after total hip replacement. Acta Orthop Scand. 1973;44:230–241.
Padgett DE, Holley KG, Cummings M, Rosenberg AG, Sumner DR, Conterato D, Galante JO. The efficacy of 500 centiGray radiation in the prevention of heterotopic ossification after total hip arthroplasty: a prospective, randomized, pilot study. J Arthroplasty. 2003;18:677–686.
Pai VS. Heterotopic ossification in total hip arthroplasty: the influence of the approach. J Arthroplasty. 1994;9:199–202.
Pakos EE, Ioannidis JP. Radiotherapy vs. nonsteroidal anti-inflammatory drugs for the prevention of heterotopic ossification after major hip procedures: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys. 2004;60:888–895.
Pellegrini VD Jr, Gregoritch SJ. Preoperative irradiation for prevention of heterotopic ossification following total hip arthroplasty. J Bone Joint Surg Am. 1996;78:870–881.
Pohl F, Seufert J, Tauscher A, Lehmann H, Springorum HW, Flentje M, Koelbl O. The influence of heterotopic ossification on functional status of hip joint following total hip arthroplasty. Strahlenther Onkol. 2005;181:529–533.
Rama KR, Vendittoli PA, Ganapathi M, Borgmann R, Roy A, Lavigne M. Heterotopic ossification after surface replacement arthroplasty and total hip arthroplasty: a randomized study. J Arthroplasty. 2009;24:256–262.
Reddi AH, Wientroub S, Muthukumaran N. Biologic principles of bone induction. Orthop Clin North Am. 1987;18:207–212.
Riegler HF, Harris CM. Heterotopic bone formation after total hip arthroplasty. Clin Orthop Relat Res. 1976;117:209–216.
Rosendahl S, Christoffersen JK, Norgaard M. Para-articular ossification following hip replacement: 70 arthroplasties ad modum Moore using McFarland’s approach. Acta Orthop Scand. 1977;48:400–404.
Rumi MN, Deol GS, Singapuri KP, Pellegrini VD Jr. The origin of osteoprogenitor cells responsible for heterotopic ossification following hip surgery: an animal model in the rabbit. J Orthop Res. 2005;23:34–40.
Schmalzried TP, Fowble VA, Ure KJ, Amstutz HC. Metal on metal surface replacement of the hip: technique, fixation, and early results. Clin Orthop Relat Res. 1996;329:S106–S114.
Sell S, Willms R, Jany R, Esenwein S, Gaissmaier C, Martini F, Bruhn G, Burkhardsmaier F, Bamberg M, Kusswetter W. The suppression of heterotopic ossifications: radiation versus NSAID therapy: a prospective study. J Arthroplasty. 1998;13:854–859.
Shimmin A, Beaule PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2008;90:637–654.
Shimmin AJ, Bare J, Back DL. Complications associated with hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:187–193, ix.
Silva M, Lee KH, Heisel C, Dela Rosa MA, Schmalzried TP. The biomechanical results of total hip resurfacing arthroplasty. J Bone Joint Surg Am. 2004;86:40–46.
Sneath RJ, Bindi FD, Davies J, Parnell EJ. The effect of pulsed irrigation on the incidence of heterotopic ossification after total hip arthroplasty. J Arthroplasty. 2001;16:547–551.
Soballe K, Christensen F, Kristensen SS. Ectopic bone formation after total hip arthroplasty. Clin Orthop Relat Res. 1988;228:57–62.
Toom A, Haviko T, Rips L. Heterotopic ossification after total hip arthroplasty. Int Orthop. 2001;24:323–326.
Urist MR. Bone: formation by autoinduction. Science. 1965;150:893–899.
Urist MR, Nakagawa M, Nakata N, Nogami H. Experimental myositis ossificans: cartilage and bone formation in muscle in response to a diffusible bone matrix-derived morphogen. Arch Pathol Lab Med. 1978;102:312–316.
Wick M, Muller EJ, Hahn MP, Muhr G. Surgical excision of heterotopic bone after hip surgery followed by oral indomethacin application: is there a clinical benefit for the patient? Arch Orthop Trauma Surg. 1999;119:151–155.
Wilkinson JM, Stockley I, Hamer AJ, Barrington NA, Eastell R. Biochemical markers of bone turnover and development of heterotopic ossification after total hip arthroplasty. J Orthop Res. 2003;21:529–534.
Acknowledgments
We thank Thorsten Seyler, MD, for assistance in statistical analysis and Cara Maguire, BA, for assistance in this investigation.
Author information
Authors and Affiliations
Corresponding author
Additional information
WGW is a consultant for Smith and Nephew (Memphis, TN) and Wright Medical Technology (Arlington, TN) with research support from Wright Medical Technology. RHJ is a consultant for Mako Surgical Corp (Ft Lauderdale, FL) and Wright Medical Technology, with research support from Wright Medical Technology. No monies from any of the companies were used in support of this study.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Shields, J.S., Mofidi, A., Ward, W.G. et al. Does a Plastic Drape Reduce Incidence of Heterotopic Ossification After Hip Resurfacing?. Clin Orthop Relat Res 469, 1606–1613 (2011). https://doi.org/10.1007/s11999-010-1606-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1606-z