Abstract
Background
Femoroacetabular impingement is recognized as a cause of hip pain in young adults and as a precursor to osteoarthritis although many questions persist regarding its management. One in particular is when to resect a pincer lesion and how much to resect. Instability can result from overresection and persistent impingement can result from underresection.
Questions/purposes
We therefore determined the correlation between the change in center-edge (CE) angle and the amount of acetabular rim resection.
Methods
We performed open acetabular rim trimming on 10 cadaveric hips. Radiographs were performed before and after rim resection every millimeter from 1 to 5 mm and we determined the CE angle. We performed linear regression to establish any correlation of the CE angle with the amount of resection.
Results
The CE angle could be predicted by −1.3X + 1.5 (R2 = 0.99), in which X = the amount of resection for 1 to 3 mm of resection. The average CE angle before resection was 35° ± 8.8° (range, 19°–58°).
Conclusions
The CE angle changes in a predictable way with acetabular rim trimming with larger amounts of resection resulting in greater changes in the CE angle.
Clinical Relevance
The ability to accurately plan the amount of acetabular rim resection in hip arthroscopy by knowing the exact change in CE angle with amount of rim removal may help prevent overresection or underresection in pincer trimming.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is recognized as a cause of hip pain in young adults and as a precursor to osteoarthritis [2, 14, 26]. Impingement is the result of abnormal contact between the proximal part of the femur and the acetabular rim during motion. Two mechanisms of FAI have been described, pincer and cam [2, 7, 18]. Impingement resulting from an aspherical femoral head is termed “cam impingement,” whereas impingement resulting from excess acetabular coverage is the result of “pincer impingement” [2].
Pincer deformity arises from general or local overcoverage of the femoral head by the acetabulum [18]. Local anterior overcoverage and/or posterior undercoverage of the femoral head can be secondary to a retroverted acetabulum [31]. Pain secondary to a retroverted acetabulum is often associated with repeated pinching as the femoral neck hits the retroverted acetabulum. These bony abnormalities may be treated with a periacetabular osteotomy with a improvement in ROM and Merle d’Aubigné score [32]. Global overcoverage can result from coxa profunda, which limits the ROM of the hip in all directions, causing a circumferential pattern of damage [20]. A persistent unfused os acetabuli can lead to FAI, but can also be seen as a consequence of FAI [2, 11, 15, 22]. Ossicles at the acetabular rim can be the result of a stress fracture from cam impingement and/or a congruent dysplastic hip [15, 22]. In a true os acetabuli, the orientation of the growth plate is parallel to the joint surface, whereas when the os is secondary to a stress fracture, the separation is perpendicular to the joint surface [22].
Surgical dislocation of the hip has been the main method of treatment of FAI with improved functional outcome, improved ROM, and decreased pain [1, 3, 5, 13, 25, 34]. As described originally by Ganz et al., the open method of treatment requires dislocation of the hip, preservation of the blood supply to the femoral head, and femoroacetabular osteoplasty [6]. The extent of the osteoplasty depends on the type of FAI: cam, pincer, or mixed-type. In cam and mixed-type, a femoral osteoplasty is performed to remove the prominent area of the femoral neck. In pincer and mixed-type, the acetabulum rim is trimmed to remove the pincer lesion. Recent advances have allowed for the treatment of cam and pincer deformities arthroscopically [29]. “Minimally invasive” trimming of the pincer lesion in patients with acetabular retroversion has been performed with improvement in functional outcome scores and with correction of the retroversion [16, 27].
During both methods of surgery, periodic dynamic assessment of the resection from both the femur and the acetabulum should be performed. Too much or too little bony resection can lead to problems. Underresection of either the cam or pincer lesion can lead to persistent impingement [8, 28]. Overresection is also undesirable. Greater than 30% resection of the femoral head-neck junction results in a decrease in the amount of energy necessary to produce a fracture [21]. Instability of the hip, resulting in subluxation or dislocation, can result from overresection [4, 23]. Some authors have recommended preoperative templating to ensure precise resection of the lesion [16, 24]. Acetabular rim resection resulting in a center-edge (CE) angle of greater than or equal to 25° is typically recommended [17]. In a previous study by Philippon et al., change in CE angle was = 1.2 + 0.72X mm of rim reduction, in which 1 mm of bony resection was equal to 1.92° [30]. These findings were seen in patients undergoing surgery for FAI.
We therefore asked whether the change in CE angle could be reliably predicted from the amount of acetabular rim resected.
Materials and Methods
We obtained 10 hips from five formalin-preserved complete human cadavers (three female and two male specimens) with a mean age of 83 years (range, 72–89 years) for this study. Specimens were positioned on an operating table in the supine position with neutral hip positioning. The hips were dissected free of overlying muscle and capsule. An AP radiograph of the hip was performed before any rim trimming. The labrum was elevated off of the rim of the acetabulum. The acetabular rim was removed in successive 1-mm increments measured with a ruler. The measurement was taken in three different areas. Using the zone method, this would correspond to Zones 1, 3, and 5 [10]. Clinically, the greatest depth of resection is taken at the apex of the pincer lesion and then tapered at the margins. However, an equal amount of resection was taken around the entire pincer lesion to maintain a standard amount of removed bone.
We took serial AP hip radiographs after 1, 2, 3, 4, and 5 mm of resection with the hip in neutral positioning. The radiographs were digitized and the CE angle was measured by three orthopaedists (AC, SK, JB) at various levels of training using Adobe Photoshop CS3 (San Jose, CA) [35]. The measurements were repeated on three separate occasions by each orthopaedist. Intraobserver correlation was computed using the intraclass correlation coefficient (ICC) two-way mixed model with measures of absolute agreement used to analyze the measurement reliability. Values of the ICC range from 0 to 1 with a higher value indicating better reliability. The coefficient of variance was used to find the deviation of mean values and assess the interobserver correlation. The interobserver correlation coefficient was 0.975 between observers and the ICC was 0.964, 0.953, and 0.919 for the three observers.
We used a general linear model regression to calculate the change in CE angle for each 1-mm acetabular rim reduction. The model is based on several assumptions. Linear regression assumes the data points are independent of each other. Despite hips being “in pairs,” the data collected from the hips were independent of their relationship to one another. We collected the change in CE angle degrees with each millimeter resected from the acetabulum; thus, each hip was essentially normalized and measurements of each hip were not dependent on the other hips or the cadavers. The assumption of homoscedasticity of the data in this model was validated by Bartlett’s test for homogeneity of variance [33]. The correlation of determination and the p value of the correlation were calculated. Statistical analysis was conducted using SPSS software for Windows, Version 17.0 (Chicago, IL).
Results
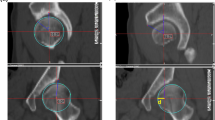
The change in CE angle for each millimeter removed can be predicted by the linear regression line −1.3X + 1.5 (Fig. 1). The correlation of the change in CE angle for each 1-mm acetabular rim reduction is significant (R2 = 0.99, p = 0.04). Bartlett’s test for homogeneity was also significant (p = 0.03). Reduction of the acetabular rim by 1 mm led to a change in CE angle of 0.12° ± 0.94°, 2 mm resulted in a decrease in CE angle of −1.1° ± 1.1°, and 3 mm decreased the CE angle by 2.6° ± 0.87°. With greater than 3 mm of resection of the acetabular rim, we began to observe subluxation of the hip. Three of 10 (30%) hips with 4 mm of acetabulum resection subluxated and seven of 10 (70%) hips with 5 mm of resection were subluxated. We attempted to correct for this when measuring the CE angle on the digitized radiographs by estimating the native center of the femoral head. However, when the CE angles from the subluxated hips were taken into account, the relationship between CE angle and amount resected was 0.22X − 1.2 (R2 = 0.07), producing an apparent paradoxical increase in CE angle of 0.4° for values greater than 3 mm of resection. Therefore, we only included the hips from 1 to 3 mm of resection for our calculation. The average CE angle before resection in the 10 hips was 35° (range, 19°–58°; SD = 8.8°).
Discussion
FAI can be the result of deformities on the femoral or acetabular side of the hip. Both open and arthroscopic techniques can be used to address the deformities. Overcoverage of the femoral head by the acetabulum, known as pincer impingement, may be addressed by trimming the pincer lesion. Care must be taken to prevent over- and underresection of the pincer lesion. Removal of too little bone can result in persistent impingement and pain [8, 28]. Removal of too much bone may lead to instability [4, 23]. Some authors have proposed templating the amount of resection of the pincer lesion for more accuracy [16, 24]. The purpose of our study was to determine if the correlation between the amount of rim resected and the CE angle could be reliably reproduced.
We acknowledge the limitations of our study. First, we were only able to quantify the lateral change of the pincer lesion with AP radiographs [24]. A false profile view would have allowed us to assess the change in anterior coverage through the anterior CA angle [19]. Accurate assessment of the anterior aspect of the pincer lesion intraoperatively can be accomplished by taking lateral views of the proximal femur [17]. However, this is difficult to reproduce during surgery and a method of templating the amount of anterior and superior resection on the fluoroscopic image of the hip intraoperatively has been proposed [24]. Second, three of 10 hips began to subluxate after we resected 4 mm of acetabular rim and seven of 10 began to subluxate when we resected 5 mm of acetabular rim. This is not surprising because removal of the soft tissues and labrum would remove several of the stabilizers of the hip. Although we attempted to correct for this when performing our measurements by adjusting for the native center of the femoral head, the resulting relationship was still aberrant. Thus, we calculated our formula only using the first 3 mm of resection to maintain accuracy. Third, the cadaveric hips in our study were grossly normal. However, because we were looking for a correlation of acetabulum rim removal with CE angle, hips with an actual pincer lesion may not have been necessary.
Using the CE angle, we found the amount of lateral acetabular rim removed during pincer trimming can be predicted by the formula −1.3X + 1.5. Our formula differs somewhat from a previously published formula in which change in CE angle was 1.2 + 0.72X mm of rim reduction [30]. This difference could be the result of differences in positioning of the hip for the radiograph and/or the number of hips studied.
The ability to accurately plan the amount of acetabular rim resection in surgery for FAI may help to prevent complications from hip arthroscopy. Indeed, revision hip arthroscopy is most commonly performed for pain resulting from persistent hip impingement, which may be the result of unaddressed or inadequate resection of the pincer lesion [8, 28]. Conversely, overresection of the acetabular rim can result in hip instability, including subluxation and dislocation [4, 9, 23]. Reduction of the CE angle to 20° or less results in acetabular dysplasia, which has been associated with arthritis [12]. Preoperative templating has been recommended and described by several authors [16, 24]. We recommend preoperatively deciding on the amount of rim resection by templating on radiographs by calculating the preoperative and then the desired CE angle. Using the formula, ∆CE angle = −1.3X + 1.5, in which X is the amount of millimeters resected, one can estimate the amount of millimeters of resection necessary for the desired CE angle.
References
Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779.
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73.
Benali Y, Katthagen B. Hip subluxation as a complication of arthroscopic débridement. Arthroscopy. 2009;25:405–407.
Espinosa N, Rothenfluh DA, Beck M, Ganz R. Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935.
Ganz R, Gill RJ, Gautlier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip. A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124.
Ganz R, Parvizi J, Beck M, Leunig M, Notzil H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295–1302.
Ilizaturri VM. Complications of arthroscopic femoraoacetabular impingement treatment. Clin Orthop Relat Res. 2009;467:760–768.
Ilizaturri VM, Byrd JW, Sampson TG, Guanche CA, Philippon MJ, Kelly BT, Dienst M, Mardones R, Shonnard P, Larson CM. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy. 2008;24:534–539.
Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176.
Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study. Acta Orthop. 2005;76:149–158.
Jager M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256–263.
Kassarjian A, Yoon LS, Beizile E, Connolly SA, Millis MB, Palmer WE. Triad of MR arthrographic findings in patients with cam-type femoroacetabular impingement. Radiology. 2005;236:588–592.
Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429.
Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–546.
Larson CM, Wulf CA. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular impingement in the supine position. Arthroscopy. 2009;25:1183–1192.
Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66.
Lequesne M, de Seze. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies [in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652.
Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253.
Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Femoroacetabular impingement: evaluation of the effect of the size of the resection. J Bone Joint Surg Am. 2005;87:273–279.
Martinez AE, Li SM, Ganz R, Beck M. Os acetabuli in femoro-acetabular impingement: stress fracture or unfused secondary ossification centre of the acetabular rim? Hip Int. 2006;16:281–286.
Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404.
Matsuda DK. Fluoroscopic templating technique for precision arthroscopic rim trimming. Arthroscopy. 2009;25:1175–1182.
Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Débridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181.
Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240:778–785.
Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23.
Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921.
Phillippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement. Am J Sports Med. 2007;35:1571–1580.
Philippon MJ, Wolff AB, Briggs KK, Kuppersmith DA, Zehms CT. Rim reduction for the treatment of pincer-type FAI correlates with pre and postoperative center edge angle (SS-32). Arthroscopy. 2009;25(Suppl 1):e18–e19.
Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288.
Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286.
Snedecor GW, Cochran WG. Statistical Methods. 8th ed. Ames, IA: Iowa State University Press; 1989.
Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Colvin, A.C., Koehler, S.M. & Bird, J. Can the Change in Center-edge Angle During Pincer Trimming Be Reliably Predicted?. Clin Orthop Relat Res 469, 1071–1074 (2011). https://doi.org/10.1007/s11999-010-1581-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1581-4