Abstract
Background
Numerous joint implant options of varying cost are available to the surgeon, but it is unclear whether more costly implants add value in terms of function or longevity.
Questions/purposes
We evaluated registry survival of higher-cost “premium” knee and hip components compared to lower-priced standard components.
Methods
Premium TKA components were defined as mobile-bearing designs, high-flexion designs, oxidized-zirconium designs, those including moderately crosslinked polyethylene inserts, or some combination. Premium THAs included ceramic-on-ceramic, metal-on-metal, and ceramic-on-highly crosslinked polyethylene designs. We compared 3462 standard TKAs to 2806 premium TKAs and 868 standard THAs to 1311 premium THAs using standard statistical methods.
Results
The cost of the premium implants was on average approximately $1000 higher than the standard implants. There was no difference in the cumulative revision rate at 7–8 years between premium and standard TKAs or THAs.
Conclusions
In this time frame, premium implants did not demonstrate better survival than standard implants. Revision indications for TKA did not differ, and infection and instability remained contributors. Longer followup is necessary to demonstrate whether premium implants add value in younger patient groups.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
TKA and THA have emerged as two of the twentieth century’s most common and reliable surgical procedures [5, 9, 16, 18, 27]. The aim of the surgery is to provide a pain-free, stable, mobile, and durable joint. Recent advances in joint arthroplasty technology have focused on improving motion and kinematics in TKA, improving arc of motion and stability in THA, and improving wear characteristics in both—all at increased cost over earlier designs.
Implant expense has traditionally been one of the costlier parts of the hospital bill for total joint arthroplasties (TJAs) [16, 19, 25]. Increasingly, efforts have been made to minimize costs associated with TJA surgery and hospitalization in an era of dwindling Medicare reimbursements and push for national healthcare reform [5, 17]. Surgeons might reasonably be expected to weigh these cost considerations against their desire to use new technology that may afford better function, fewer complications, and/or improved longevity of TJA for their patients. However, whether the new technology associated with so-called “premium” implants justifies the increased cost over standard implants that have performed well remains unknown and, in a more general sense, provides an important part of the rationale behind large joint registries.
We sought to determine whether higher-cost premium hip and knee implants were superior to standard knee and hip implants in terms of implant survival in our community total joint registry. Thus, the primary objective of this study was to assess the difference, if any, in the cumulative revision rate of premium and standard TKA and THA implants. Secondary aims were to analyze the effect of different variables such as age, gender, and diagnosis on the survival of the two implant categories. Finally, we examined any potential differences in patient length of stay and discharge disposition between the implant categories.
Patients and Methods
The HealthEast Joint Registry (HEJR) is a community-based total joint registry in the St Paul, MN, metropolitan area that provides information on more than 21,500 hip and knee arthroplasties performed since September 1, 1991. More than 40 community surgeons operating at five hospitals contribute complete registry data on all total joint operations performed. Details on the data collection methods and the application of statistical analyses for this registry have been previously reported [10].
For this study, we included primary TKAs that had a porous femur and cemented tibia, cemented femur and cemented tibia, or a cemented femur and cemented all-polyethylene tibia (n = 10,326). Cementless designs where both porous femoral and tibial components were utilized were excluded based on their small number. Premium TKA components were defined as mobile-bearing designs, high-flexion designs, those including oxidized-zirconium femoral components or newer moderately-crosslinked polyethylene inserts, or some combination of these designs (n = 2806). All TKAs from 1991 through 2000 were excluded, since the premium design inclusions above were not available before 2001 (n = 4043), and an additional 15 TKAs utilizing highly constrained or hinged designs were also excluded. This left a total of 6268 TKAs (3462 standard TKAs and 2806 premium TKAs) for analysis. All THAs that utilized cementless femoral and acetabular components with any bearing surface combination were considered for inclusion (n = 2973). Premium THAs included ceramic-on-ceramic, ceramic-on-polyethylene, or metal-on-metal designs (n = 1311). Again, all THAs from 1991 through 2001 were excluded since the premium design inclusions above were not available before 2002 (n = 792), and an additional two THAs that used non-highly-crosslinked liners were also excluded. This left a total of 2179 THAs (868 standard THAs and 1311 premium THAs) for analysis.
Of the 6268 TKAs, 64% were female, the average age was 66.4 years, and the minimum followup was 0 years (average, 3.4 years; range, 0.0–8.0 years). Of the 2179 THAs, 52% were female, the average age was 62.7 years, and the minimum followup was 0 years (average, 2.8 years; range, 0.0–7.0 years). We used revision of the index arthroplasty as the end point and defined revision as the removal, exchange, or addition of any prosthetic component. Other variables assessed were age, gender, year of index procedure, cost of primary implant, length of stay in hospital for index procedure (LOS), primary diagnosis, discharge disposition after index procedure, head size (for THAs only), and reason for revision.
Premium and standard implants were compared univariately using the Wilcoxon rank sum test for continuous variables (age, cost of primary implant, and LOS) and the Pearson’s chi-square test for categorical variables (gender, year of index procedure, primary diagnosis, discharge disposition, and reason for revision). We also performed subgroup analyses comparing premium TKAs with moderately-crosslinked polyethylene inserts, mobile-bearing/oxinium femoral component designs, and high-flexion designs to the standard TKAs separately. Cumulative revision rates (CRRs) were compared for the premium and standard implants using the Kaplan-Meier method to calculate the CRR and the log-rank test to compare those rates. Relative risk of revision was computed using Cox regression models and all variables of interest (except reason for revision) were considered for potential confounding. A confounder was defined as a variable that changed the main effect estimate by greater than 10%. Only age met those criteria for the TKA analysis, and age, cost of implant, and year of index procedure met those criteria for the THA analysis.
Results
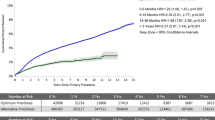
We found no difference in the CRR between premium and standard TKAs at 7 years (Fig. 1). When compared to standard TKAs, the premium TKAs were on average younger patients, had a higher implant cost, and were more often implanted from 2005 to 2008 (Table 1). There were no differences in gender or revision reason between the standard and premium TKAs. Finally, there was no difference in either the crude relative risk of revision (p = .94) or the age-adjusted relative rate of revision (p = .75) when comparing premium to standard TKAs.
In the subgroup analysis within the premium TKA group, we found no differences (p = 0.51–0.67) in CRRs between the premium subgroups and the standard TKAs. There were also no differences (p = 0.42–0.81) in the crude or adjusted relative risk of revision for any of the premium subgroups and the standard TKAs.
There was no difference in the CRR between premium and standard THAs at 6 years (Fig. 2). When compared to standard THAs, the premium THAs were on average younger patients, had a higher implant cost, and were more often implanted from 2005 to 2008. They also had a head size of greater than 32 mm more often (69% versus 36%) and were less often revised for dislocation (Table 2). There was no difference in gender between premium and standard THAs. Finally, there was no difference in either the crude (p = .24) or the age-adjusted relative risk of revision (p = .72) when comparing premium to standard THAs.
Discussion
The rising cost of health care in the United States and increasing constraints on economic resources have led to an increased emphasis on healthcare economic evaluation. Primary and revision TJA accounts for a higher percentage of Medicare spending than any other inpatient procedure [3]. With the number of such procedures expected to increase [16, 19], TJA continues to attract the attention of the Center for Medicare and Medicaid services. Since implant expense is a major portion of the total cost of the procedure [16–19, 25, 34] and increasing use of premium implants is one of the drivers [9], we sought to determine whether such implants could be demonstrated to have superior value in early- to midterm followup.
Our study has the obvious limitations inherent to the use of any joint registry. First, the use of survival analysis with an end point of revision surgery does not identify the proportion of the patients who might have had clinical failure or poor functional results, as is usually the case with cost-effectiveness studies [5]. Similarly, it cannot identify patients who may somehow benefit from superior functional results achieved with a premium implant. Second, there is a possibility that some patients might have had their revision surgery performed elsewhere, but we have previously reported a greater than 94% “capture rate” in our registry, and this limitation would presumably affect both premium and standard implant recipients in a similar distribution [10]. Third, the length of followup is short but was limited by the relatively recent introduction of some of the designs reviewed, and our registry will continue to capture these data prospectively over the longer term. The strength of the study lies in the community nature of the registry, with more than 40 surgeons participating, none of whom is an implant designer-developer or industry consultant. As a result, we would presume surgeon implant choices were unaffected by such direct relationships.
There is an essential conflict between surgeons and payors around the issue of implant choice, since a surgeon’s primary perspective is to select the “best” implant to achieve a superior outcome and meet the patient’s expectations, regardless of the cost of the implant [16, 17, 34]. Most surgeons would choose a more costly implant with “better” clinical results versus an inexpensive implant with “acceptable” results [34]. Patients overwhelmingly want their surgeon to choose their implant and want quality to be the overriding consideration in that choice [34]. Unfortunately, the lack of timely evidence that new innovations in TJA will result in superior outcomes and the certain knowledge that not all innovations improve outcome make such choices difficult [19].
Previously published reports demonstrate no obvious superiority of the premium implants over the standard lower-cost implants reviewed in this paper (Table 3). Reports of high-flexion knees [2, 23, 27], mobile-bearing knees [6, 24], oxidized-zirconium femoral components [22, 35], and moderately crosslinked polyethylene inserts [29, 31, 32] have not been consistently associated with either improved function or survival when compared to standard lower-cost designs. All-polyethylene tibial components have demonstrated similar or better mid- to long-term results than metal-backed tibial component designs at lower cost [1, 11, 12, 33]. Similarly, the results for the premium metal-on-metal and ceramic hip designs reviewed here have also been mixed, with improved wear characteristics balanced by concerns over metal ion concentrations, delayed hypersensitivity reactions, ceramic articulation squeaking, and fracture [7, 8, 13–15, 26, 28, 30, 36–38] (Table 4).
In a time frame of 6 to 7 years of survival data, premium TKA and THA implants in our registry did not demonstrate better survival than standard implants. The fact that patients receiving premium implants were more frequently discharged home and had shorter hospital LOS undoubtedly reflects their younger age and evolving rehabilitation and surgeon protocols during the same time frame. There were fewer THA patients revised for dislocation in the premium group, but this was not significant after adjusting for age grouping (< 60 years, 60–69 years, ≥ 70 years) and head size (< 32 mm versus ≥ 32 mm). Premium TKA implants as a percentage of total TKA implants in the HEJR rose to 62% during the years 2005 to 2008 and premium THA implants increased to 72% of the total during the same time period.
We believe surgeons should make implant choices with the patient’s best interest in mind. However, surgeons cannot watch from the sidelines during the intensifying debate over national healthcare reform. Evidence-based medicine on implant performance, including registry studies, randomized trials, and cost-effectiveness analysis, will permit us to make informed choices for our patients. Cost-awareness programs for surgeons are excellent first steps in managing implant costs [16, 34], and to date surgeons still play the primary role in determining the implant chosen. All innovation does not represent improvement, and higher cost does not necessarily equate to higher quality. Numerous studies point to the substantial percentage of early revision indications in TJA that are design-independent, such as infection and instability [4, 34]. Surgeons must continue to play a key role in deciding what represents rational cost-effective care or that role may be assumed by others.
References
Apel DM, Tozzi JM, Dorr LD. Clinical comparison of all-polyethylene and metal-backed tibial components in total knee arthroplasty. Clin Orthop Relat Res. 1991;273:243–252.
Bettinson KA, Pinder IM, Moran CG, Weir DJ, Lingard EA. All-polyethylene compared with metal-backed tibial components in total knee arthroplasty at ten years. A prospective, randomized controlled trial. J Bone Joint Surg Am. 2009;91:1587–1594.
Bozic KJ, Durbhakula S, Berry DJ, Naessens JM, Rappaport K, Cisternas M, Saleh KJ, Rubash HE. Differences in patient and procedure characteristics and hospital resource use in primary and revision total joint arthroplasty: a multicenter study. J Arthroplasty. 2005;20(Suppl 3):17–25.
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51.
Bozic KJ, Saleh KJ, Rosenberg AG, Rubash HE. Economic evaluation in total hip arthroplasty: analysis and review of the literature. J Arthroplasty. 2004;19:180–189.
Callaghan JJ. Mobile-bearing knee replacement: clinical results: a review of the literature. Clin Orthop Relat Res. 2001;392:221–225.
Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation: four to seven-year results. J Bone Joint Surg Am. 2000;82:789–798.
Dumbleton JH, Manley MT. Metal-on-metal total hip replacement: what does the literature say? J Arthroplasty. 2005;20:174–188.
Ezzet KA, Hermida JC, Colwell CW Jr, D’Lima DD. Oxidized zirconium femoral components reduce polyethylene wear in a knee wear simulator. Clin Orthop Relat Res. 2004;428:120–124.
Gioe TJ, Killeen KK, Mehle S, Grimm K. Implementation and application of a community total joint registry: a twelve-year history. J Bone Joint Surg Am. 2006;88:1399–1404.
Gioe TJ, Sinner P, Mehle S, Ma W, Killeen KK. Excellent survival of all-polyethylene tibial components in a community joint registry. Clin Orthop Relat Res. 2007;464:88–92.
Gioe TJ, Stroemer ES, Santos ER. All-polyethylene and metal-backed tibias have similar outcomes at 10 years: a randomized level I [corrected] evidence study. Clin Orthop Relat Res. 2007;455:212–218.
Grübl A, Marker M, Brodner W, Giurea A, Heinze G, Meisinger V, Zehetgruber H, Kotz R. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res. 2007;25:841–848.
Hamadouche M, Boutin P, Daussange J, Bolander ME, Sedel L. Alumina-on-alumina total hip arthroplasty: a minimum 18.5-year follow-up study. J Bone Joint Surg Am. 2002;84:69–77.
Hasegawa M, Ohashi T, Tani T. Poor outcome of 44 cemented total hip arthroplasties with alumina ceramic heads: clinical evaluation and retrieval analysis after 10-16 years. Acta Orthop Scand. 2001;72:449–456.
Healy WL, Iorio R. Implant selection and cost for total joint arthroplasty: conflict between surgeons and hospitals. Clin Orthop Relat Res. 2007;457:57–63.
Healy WL, Iorio R, Lemos MJ, Patch DA, Pfeifer BA, Smiley PM, Wilk RM. Single price/case price purchasing in orthopaedic surgery: experience at the Lahey Clinic. J Bone Joint Surg Am. 2000;82:607–612.
Healy WL, Iorio R, Richards JA. Opportunities for control of hospital cost for total knee arthroplasty. Clin Orthop Relat Res. 1997;345:140-147.
Healy WL, Iorio R, Richards JA, Lucchesi C. Opportunities for control of hospital costs for total joint arthroplasty after initial cost containment. J Arthroplasty. 1998;13:504–507.
Hooper G, Rothwell A, Frampton C. The low contact stress mobile-bearing total knee replacement: a prospective study with a minimum follow-up of ten years. J Bone Joint Surg Br. 2009;91:58–63.
Huang CH, Ma HM, Lee YM, Ho FY. Long-term results of low contact stress mobile-bearing total knee replacements. Clin Orthop Relat Res. 2003;416:265–270.
Kim YH, Kim JS, Huh W, Lee KH. Weight of polyethylene wear particles is similar in TKAs with oxidized zirconium and cobalt-chrome prostheses. Clin Orthop Relat Res. 2010;468:1296–1304.
Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475.
Kim YH, Yoon SH, Kim JS. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg Br. 2007;89:1317–1323.
Levine DB, Cole BJ, Rodeo SA. Cost awareness and cost containment at the Hospital for Special Surgery: strategies and total hip replacement cost centers. Clin Orthop Relat Res. 1995;311:117–124.
Lusty PJ, Tai CC, Sew-Hoy RP, Walter WL, Walter WK, Zicat BA. Third-generation alumina-on-alumina ceramic bearings in cementless total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2676–2683.
McCalden RW, MacDonald SJ, Bourne RB, Marr JT. A randomized controlled trial comparing “high-flex” vs “standard” posterior cruciate substituting polyethylene tibial inserts in total knee arthroplasty. J Arthroplasty. 2009;24(Suppl):33–38.
Migaud H, Jobin A, Chantelot C, Giraud F, Laffargue P, Duquennoy A. Cementless metal-on-metal hip arthroplasty in patients less than 50 years of age: comparison with a matched control group using ceramic-on-polyethylene after a minimum 5-year follow-up. J Arthroplasty. 2004;19(Suppl 3):23–28.
Minoda Y, Aihara M, Sakawa A, Fukuoka S, Hayakawa K, Tomita M, Umeda N, Ohzono K. Comparison between highly cross-linked and conventional polyethylene in total knee arthroplasty. Knee. 2009;16:348–351.
Murphy SB, Ecker TM, Tannast M. Two- to 9-year clinical results of alumina ceramic-on-ceramic THA. Clin Orthop Relat Res. 2006;453:97–102.
Ries MD. Highly cross-linked polyethylene: the debate is over—in opposition. J Arthroplasty. 2005;20(Suppl 2):59–62.
Rodriguez JA. Cross-linked polyethylene in total knee arthroplasty: in opposition. J Arthroplasty. 2008;23(Suppl):31–34.
Rodriguez JA, Baez N, Rasquinha V, Ranawat CS. Metal-backed and all-polyethylene tibial components in total knee replacement. Clin Orthop Relat Res. 2001;392:174–183.
Sharkey PF, Sethuraman V, Hozack WJ, Rothman RH, Stiehl JB. Factors influencing choice of implants in total hip arthroplasty and total knee arthroplasty: perspectives of surgeons and patients. J Arthroplasty. 1999;14:281–287.
Spector BM, Ries MD, Bourne RB, Sauer WS, Long M, Hunter G. Wear performance of ultra-high molecular weight polyethylene on oxidized zirconium total knee femoral components. J Bone Joint Surg Am. 2001;83(Suppl 2):80–86.
Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, Miller RK. Ceramic-on-polyethylene bearing surfaces in total hip arthroplasty: seventeen to twenty-one-year results. J Bone Joint Surg Am. 2001;83:1688–1694.
Yoo JJ, Kim YM, Yoon KS, Koo KH, Song WS, Kim HJ. Alumina-on-alumina total hip arthroplasty: a five-year minimum follow-up study. J Bone Joint Surg Am. 2005;87:530–535.
Zijlstra WP, Cheung J, Sietsma MS, van Raay JJ, Deutman R. No superiority of cemented metal-on-metal vs metal-on-polyethylene THA at 5-year follow-up. Orthopedics. 2009;32:479–485.
Acknowledgments
We thank Kathy Killeen, MOT for her ongoing work with the HEJR and the surgeons of HealthEast who continue to contribute their patients to this important effort.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the HeathEast Joint Registry, HealthEast Hospitals, St. Paul, MN.
About this article
Cite this article
Gioe, T.J., Sharma, A., Tatman, P. et al. Do “Premium” Joint Implants Add Value?: Analysis of High Cost Joint Implants in a Community Registry. Clin Orthop Relat Res 469, 48–54 (2011). https://doi.org/10.1007/s11999-010-1436-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1436-z