Abstract
Background
Various landmarks can guide tibial component rotational alignment in routine TKA, but with the deeper tibial resection levels common in complex primary and revision TKAs, it is unknown whether these landmarks remain reliable.
Questions/purposes
We asked whether three techniques for determining tibial component rotation based on local anatomic landmarks are reliable deeper tibial resection levels.
Patients and Methods
The femoral transepicondylar axis was identified by three independent reviewers on MR images of knees from 24 men and 24 women and transposed at a traditional tibial resection level and at the level of the proximal, middle, and distal parts of the proximal tibiofibular joint. Three axes were drawn on axial slices at these levels: the geometric center of the tibial plateau to the medial 1/3 of the tubercle, the posterior condylar line of the tibia, and the largest mediolateral dimension of the tibia. These lines were compared with the transposed femoral epicondylar axis line.
Results
The posterior condylar line of the tibia is the least variable local landmark for tibial component positioning at deep resection levels.
Conclusions
Assuming the normal posterior condylar line of the tibia is visible at revision, setting the tibial component at 10° external rotation with respect to the posterior condylar axis of the tibia gets the tibial component within 10° of proper rotation in 86% to 98% of patients, even to the distal part of the proximal tibiofibular joint. The experienced surgeon then can adjust this position based on cues from an assortment of other axes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Proper positioning of TKA components is important for the functional outcome and longevity of the procedure [8, 9, 11]. Although the desired positions and guiding landmarks for placement of femoral and tibial components in the coronal and sagittal planes have been well described, rotational positioning (in the transverse plane) of the components can be problematic [13]. Patellofemoral kinematics is altered with femoral and tibial component rotational malpositioning greater than 5°. Larger amounts of combined internal rotation (7°–17°) may lead to patellar dislocation or loosening [3]. Isolated tibial component rotational malpositioning of 15° has been noted in cadavers to alter patella kinematics and/or polyethylene loading with some prosthetic designs, including mobile bearings [5, 10]. One would expect the success of revision TKA might be similarly affected by tibial component malrotation.
Various anatomic landmarks have been described to serve as rotational reference points for primary TKA. On the femoral side, the posterior condyles of the femur, Whiteside’s line [15], and the transepicondylar axis (TEA) can be used to determine appropriate component rotation [3, 4]. Tibial references are less well defined, with the tibial tubercle, PCL insertion, posterior condylar line of the tibia, widest dimension of the tibial surface, ankle malleolar axis, and anterior contour of the tibia as examples of described landmarks [1–3, 6, 7, 13]. Although these references have been supported for use at a standard resection level for primary TKA, it is not known whether such rotational alignment strategies are applicable when the tibia is resected more distally, as is common in complex primary and revision TKAs. Clearly, landmarks well away from the cut tibial surface will not be affected by resection level. Other landmarks, such as the insertion of the PCL, disappear as the resection level moves distally. As the numbers of revision TKAs performed in the US are expected to increase substantially in the coming years, it is important to establish reliable techniques to achieve proper rotational positioning of TKA tibial components at distal resection levels.
We asked (1) which of three previously described techniques using local anatomy to establish tibial component rotation is most accurate, on average, for determining tibial component rotation at distal resection levels, (2) which of these three techniques is the most precise (least variable) across different knee specimens, and (3) which of these three techniques has the least interobserver and intraobserver variability.
Patients and Methods
Three different orthopaedic surgeons (an experienced total joint arthroplasty surgeon and two total joint arthroplasty fellows) independently evaluated the same 48 MR images of the knee (24 men and 24 women) in this study. These axial scans were obtained from patients who were being evaluated for internal derangement of the knee at our institution from 2006 to 2008. The average age of the patients was 53 years (range, 25–74 years). All of the patients had no more than mild knee osteoarthritis, no history of fracture about the knee, no complete ligamentous injury, and no inflammatory arthropathy. Patients with mild osteoarthritis and meniscal tears were included in the study. Power analysis, based on a pilot sampling of 10 patients, revealed 48 patients would be needed at 0.80 power to detect a difference of 10° between axes with alpha = 0.05. Institutional Review Board approval was obtained.
Images were acquired on a 1.5-T scanner (GE Medical Systems, Milwaukee, WI). Fast spin echo images (repetition time [TR] = 2500; echo time [TE] = 16.5) were obtained from above the patella to below the tibial tubercle. The MRI scans were obtained using a standard clinical protocol with the knees in full extension and axial sections constructed in a plane parallel to the tibial articular surface. The field of view was 16 cm and the slice thickness was 3.5 mm with a 0.5-mm interslice gap. Anatomic landmarks and rotational axes were constructed using a computer workstation (Stentor iSite™ Version 3.3.3, 2005; Phillips, Amsterdam, The Netherlands).
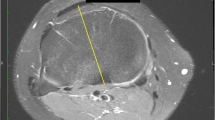
Each person reviewing the MRI scans first identified the femoral TEA using the image that he thought best depicted the medial and lateral femoral epicondyles. The medial epicondyle was defined as the center of the medial sulcus if one was present, or was defined as the peak of the medial epicondyle if a sulcus was not present. The axis was established by drawing a line through the centers of the epicondyles. The TEA then was projected distally onto the tibial images that were to be evaluated. The femoral TEA served as a reference axis for the tibial axes measured in this study.
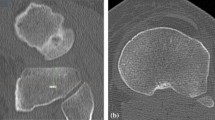
On the tibial side, each evaluator created three axes: the axis across the greatest medial to lateral width of the tibial plateau (ML), the posterior tibial condylar axis (PC), and the axis perpendicular to the line connecting the midpoint of the greatest mediolateral dimension of the tibial slice being evaluated to the medial 1/3 of the tibial tubercle (TUB) (Figs. 1, 2). Because the tibial tubercle was not always visible on the MR slices evaluated, the patellar tendon was used as a surrogate for the tibial tubercle in these slices. The PCL insertion was not used as the posterior point on this line as the PCL insertion disappears at the more distal resection levels.
A box and whiskers plot incorporating the measurements of all three observers is shown. The vertical axis represents the difference in degrees between the position of the measured axis and the reference femoral epicondylar axis. The line in the box denotes the median value, the upper and lower ends of the box span the central half of all the values, and the whiskers indicate the range of values. The TUB axis was the most accurate across all resection levels, but the ranges, as spanned by the error bars, were smallest with the PC axis. ML is the axis defined by the greatest mediolateral dimension of the tibial surface. PC is the posterior tibial condylar axis. TUB is the axis connecting the geometric center of the tibial plateau with the medial 1/3 of the tibial tubercle. Resection levels are 6–8 mm below the tibial surface, and the proximal (P), middle (M), and distal (D) levels of the proximal tibiofibular joint.
A graph shows the mean positions of the three axes in relation to the reference femoral epicondylar axis. The mean ML and PC axes moved toward internal rotation with deeper resection levels. In contrast, the mean TUB axis moved toward external rotation, and was the most accurate (closest to zero) across all resection levels.
Each of these three axes was identified at four different levels on the proximal tibia, as referenced by the coronal scout images on the computer workstation. The proposed resection levels were between 6 and 8 mm below the joint, the proximal tibiofibular joint, the middle aspect of the tibiofibular joint, and the distal aspect of the proximal tibiofibular joint. The first resection level is a standard amount in a primary TKA, and the latter resection levels are more distal resection levels frequently required in complex primary or revision TKA. We chose to reference the more distal resection levels to the tibiofibular joint rather than measuring standard distances below the native joint line because the original level of the joint line is not commonly known in the revision setting, and because standard distances would be proportionally larger or smaller resections based on the patient’s bone size. The proximal tibiofibular joint usually is preserved in the revision setting and provides a reasonable landmark for depth of tibial resection.
The ML dimension of the tibia was characterized as the widest point across the tibial plateau at each resection level. The PC axis was a line formed connecting the posterior margins of the medial and lateral tibial condyles. The axis relative to the patellar ligament insertion was created by first identifying the center point of the ML axis on the tibial plateau and then creating a line to the medial 1/3 mark of the tibial tubercle, or the patellar tendon when the tubercle was not visible on the slice. The TUB axis was the perpendicular to this line. For each observer, 12 data points were collected on each MR image of the knee (three axes at each of four different resection levels), with negative numbers correlating to internal rotation relative to the reference femoral TEA and positive numbers correlating to external rotation.
For each axis at each resection level, we calculated average difference from the reference TEA, the range of axis positions, and standard deviation. The difference between the average value and zero degrees was used to determine accuracy. The precision of each proposed reference axis was assessed using an equality of variance F test, which was applied separately for each of the three observers at each dissection level. We sought to compare each axis with the others to determine which axis had the least amount of variability (alpha = 0.05; S-Plus® Statistical Program; TIBCO, Palo Alto, CA). Because the equality of variance test was applied separately to the three observers, we could determine whether particular axes had better precision across all raters, or if the variability was more rater-dependent. We calculated intraclass correlation coefficients to quantify interobserver agreement of the three axis measurements. Finally, to evaluate test-retest intraobserver reliability, 10 of the subjects were reevaluated by one of the observers 2 months after initially measuring all of the axes. Pearson correlation coefficients then were calculated to evaluate test-retest intraobserver reliability for each axis.
Results
The data, as averaged for the three observers, were summarized in a box and whiskers plot (Fig. 1). For each rater, at all resection levels, the average ML and PC axes were internally rotated relative to the TEA, and the TUB axis was neutral or externally rotated. As the resection level moved distally, each of these axes, on average, deviated farther from the reference TEA axis (Fig. 2). The TUB axis, on average, was nearest to the TEA at all resection levels. Even at the aspect of the distal tibiofibular joint, the mean TUB axis was externally rotated only 5° from the reference TEA. Thus across all raters, and at all resection levels, the TUB axis was, on average, the most accurate indicator of the location of the transposed femoral epicondylar axis.
The most precise axis, however, was the PC axis. Across all raters and all resection levels distal to the standard level, the standard deviation of the measured axis position was lowest for the PC axis. Equality of variance testing confirmed that the PC axis had less variance than the ML and TUB axes, particularly as resection levels moved distally (Table 1). In addition, the range of axis alignment with the PC axis was the smallest of the three axes tested across all resection levels.
The PC also had the best interobserver agreement at all resection levels as reflected by higher intraclass correlation coefficients at every resection level (Table 2). Test-retest intraobserver reliability of the three axes revealed Pearson correlation coefficients of 0.75 for the ML axis, 0.92 for the PC axis, and 0.89 for the TUB axis.
Discussion
Prior studies have evaluated the morphologic features of the proximal tibia and have proposed various anatomic landmarks for rotational positioning of the tibial component at standard resection levels for primary TKA [1–3, 6, 7, 13]. More distal resection levels, however, are needed for complex primary and revision TKAs, but there is no information available regarding whether these more proximal anatomic landmarks remain valid at distal resection levels. Knowing the cross-sectional anatomy of the tibia changes with the depth of tibial resection, we sought to determine what local anatomic features of the proximal tibia are least dependent on the depth of resection and can be used at deeper resection levels to set the rotational orientation of the tibial component.
One must recognize limitations of this study. First, owing to osteophytes, osteolysis, fracture, or other factors that may alter the morphologic features of the proximal tibia, the natural contour of the resected tibial surface in an actual revision setting no longer may be visible or it may be distorted at the time of revision TKA. The conclusions of this study are valid only if the natural contours of the tibia are identifiable. Second, the normal tibia rotates with respect to the femur as one goes into full extension (the so-called screw-home mechanism). There is thus no single axis that defines the relationship of femoral rotation to tibial rotation. We studied knees imaged at or near full extension with MRI. The conclusions for this study are thus most applicable to the knee at this position. This is close to the position of peak knee loading during gait and thus probably is the most important position to consider. Third, our conclusions also are applicable for surgeons who reference component rotation off of the epicondylar axis of the femur. If one were to use the gap balancing technique for determining femoral component rotation, the femur would not necessarily be aligned with the transepicondylar axis and thus one would not have the goal of aligning the tibial component to the femoral transepicondylar axis either. Finally, all of the axes determined in this study were manually identified without computer assistance. Whether computerized techniques to determine axes would change the results of this study is yet to be determined.
We found, at a standard resection level for primary TKA, use of any of the proposed axes would provide, on average, rotational positioning of the tibial component within 6° of the reference femoral TEA. With deeper resection levels, however, each of the axes deviated farther from the reference axis, with the TUB axis deviating toward external rotation and the ML and PC deviating into more internal rotation. On average, the TUB axis was the most accurate, as it remained closest to the reference femoral TEA across all resection levels.
However, the most precise (least variable) axis was the PC axis. Although on average it deviated into more internal rotation than the TUB axis, the PC axis had the smallest standard deviation of all the axes tested throughout all resection levels deeper than the standard resection level, with the differences in standard deviation becoming more pronounced and statistically significant as the resection level moved distally. This precision also is reflected by the range, which was lowest for the PC axis at all resection levels.
The PC axis also had the greatest interobserver agreement with intraclass correlation coefficients greater than the ML and TUB axes at all resection levels. The PC axis also had the greatest intraobserver agreement, closely followed by the TUB axis. The ML axis had the poorest intraobserver agreement. Variability across observers and across subjects is a source of outliers for rotational alignment, and the superior consistency of the PC line of the tibia in terms of precision and interobserver and intraobserver agreement makes this line an attractive reference axis for rotational placement of the tibial component. Because the average posterior condylar orientation ranges from 6° to 11° internal rotation with respect to the femoral TEA, one can set the tibial component in approximately 10° external rotation with respect to the PC axis of the tibia at all resection levels. Given the variance and the range of the data obtained in this study, and assuming that one could find a consistent way of achieving this 10° correction from the posterior condylar line, if one were to define an outlier as being greater than 10° from the reference axis, such an alignment strategy would result in approximately 2% to 14% of tibial components being outliers depending on the resection level and the observer.
As has been noted with other studies evaluating tibial landmarks at a standard resection level for primary TKA, high variability of proximal tibial landmarks remains a problem [2, 13, 14]. We also found a wide range of axis orientations across subjects (25° to 35° for the various axes at the standard resection level, which increased to 35° to 51° at more distal resections). Thus, although we found the PC axis to be the least variable axis to reference the tibial component rotation, as rotational errors of 5° to 15° can lead to maltracking problems of the patella [3, 5, 10], the PC axis was still variable enough to fail in some patients. Given the fallibility of any single rotational alignment technique for the tibia, our general approach is to combine information from multiple references when setting tibial component rotation during revision TKA. A combination of techniques reportedly provides improved alignment on the femoral side of the articulation [12] and should be applicable on the tibial side as well. With this study, we have learned the ML and PC axes trend toward increased internal rotation whereas the TUB axis trends toward increased external rotation with deeper tibial resection levels. The least variable axis across subjects and across tibial resection levels is the PC axis. Setting the tibial component at 10° external rotation with respect to the PC axis of the tibia will get the tibial component within 10° of proper rotation in 86% to 98% of patients, depending on the resection level and the observer. This provides a good starting point for setting tibial component rotation in complex primary or revision TKA. The experienced surgeon then can adjust this position based on cues from an assortment of other axes.
References
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res. 2005;436:172–176.
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res. 2004;420:213–219.
Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153.
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–47.
Chowdhury EA, Porter ML. A study of the effect of tibial tray rotation on a specific mobile bearing total knee arthroplasty. J Arthroplasty. 2005;20:793–797.
Dalury DF. Observations of the proximal tibia in total knee arthroplasty. Clin Orthop Relat Res. 2001;389:150–155.
Incavo SJ, Coughlin KM, Pappas C, Beynnon BD. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty. 2003;18:643–648.
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007; 458:131–136.
Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49–64.
Nagamine R, Whiteside LA, White SE, McCarthy DS. Patellar tracking after total knee arthroplasty: the effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res. 1994;304:262–271.
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper: Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13.
Siston RA, Cromie MJ, Gold GE, Goodman SB, Delp SL, Maloney WJ, Giori NJ. Averaging different alignment axes improves femoral rotational alignment in computer-navigated total knee arthroplasty. J Bone Joint Surg Am. 2008;90:2098–2104.
Siston RA, Goodman SB, Patel JJ, Delp SL, Giori NJ. The high variability of tibial rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:65–69.
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y. Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2002;402:196–201.
Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995;321:168–172.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the VA Palo Alto Healthcare System.
About this article
Cite this article
Graw, B.P., Harris, A.H., Tripuraneni, K.R. et al. Rotational References for Total Knee Arthroplasty Tibial Components Change with Level of Resection. Clin Orthop Relat Res 468, 2734–2738 (2010). https://doi.org/10.1007/s11999-010-1330-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-010-1330-8