Abstract
Background
Multiple studies suggest tranexamic acid reduces blood loss and red cell transfusions in patients undergoing THA or TKA. However, many of the dosing schedules in these studies are not ideally suited for routine application.
Questions/purposes
We asked whether one 20-mg per kg intraoperative dose of tranexamic acid in patients having primary THA or TKA would (1) decrease perioperative blood loss and red cell transfusion rates and (2) be a cost-effective protocol.
Patients and Methods
We retrospectively reviewed the records of 234 patients operated on from April 1 to June 30, 2007 (before our study protocol) and 259 patients from April 1 to June 30, 2008 with the single-dose protocol. We then compared change in hemoglobin, transfusion rates, hemoglobin at discharge, hospital length of stay, and complications between the two groups. No other routine patient care practices or blood conservation program strategies were altered during this time.
Results
We found a reduction in the decrease in hemoglobin in 2007 compared with 2008 for THA and TKA (46 to 39 g/L and 45 to 36 g/L, respectively), which led to a reduction in transfusion rates (13.5% to 3.6% and 13.1% to 2.0%, respectively) and higher hemoglobin levels at discharge. There were no recorded major adverse events associated with the introduction of this protocol.
Conclusions
One 20-mg per kg intraoperative dose of tranexamic acid reduced the perioperative decrease in hemoglobin and red blood cell transfusion rates in patients having TKA and THA compared with those of a similar cohort of patients in whom the protocol was not used. This weight increment dosing facilitated pharmacy drug preparation, led to minimal dose variability and wastage, and resulted in a substantial estimated cost savings.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tranexamic acid (TEA), a synthetic analog of the amino acid lysine, acts by competitively blocking the lysine binding site of plasminogen, which leads to inhibition of fibrinolysis [2]. As TEA enters the extravascular space and accumulates in tissues for up to 17 hours, the basis for its mechanism of action is thought to be inhibition of tissue fibrinolysis and consequent stabilization of clots [14]. Multiple studies show TEA can reduce blood loss and red blood cell transfusion in patients undergoing primary arthroplasty [1, 3–5, 8–10, 12, 13, 15, 17–19, 22]. However, the dosing schedules of either an initial bolus of TEA followed by a 6- to 12-hour infusion or multiple intravenous bolus doses are cumbersome and labor-intensive, making them difficult to introduce in a busy operating room schedule and arthroplasty service.
In a meta-analysis, Cid and Lozano [4] reported the reduction in risk of receiving a blood transfusion was independent of the total dose of TEA given. In another review of the use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopaedic surgery, Kagoma et al. [12] considered 21 studies in which the dose of TEA ranged from 10- to 20-mg initial bolus followed either by an infusion of 1 to 10 mg per kg per hour for 4 to 30 hours or repeated doses of the initial dose of TEA every 3 hours for one to four doses. As the most commonly prescribed dose of TEA was a 10-mg per kg initial bolus dose followed by a second similar dose at 3 hours, we decided to adopt one dose of 20 mg per kg to be given before the onset of fibrinolysis. We presumed a second dose would not be required owing to its prolonged extravascular effectiveness.
For a 3-month period before introduction of the routine use of TEA in our patients having primary arthroplasty, this same single-dosing schedule had been administered to all patients undergoing arthroplasty of one of the authors (JH) who had had previous experience with the use of TEA. Reduced transfusion rates between the patient of this surgeon and the rest of the patients of the arthroplasty group with no apparent increase in postoperative thromboembolic events encouraged introduction of the routine use of TEA in our entire population of patients undergoing arthroplasty.
Therefore, we asked whether this dosing protocol could complement our existing blood conservation program (1) by reducing perioperative blood loss and red cell transfusion rates and (2) by reducing costs.
Patients and Methods
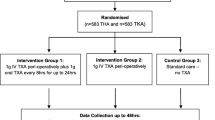
To answer the above questions, we designed a retrospective comparative study. For a 3-month period beginning April 1, 2008, to June 30, 2008, we prospectively studied all 259 patients (109 patients having THA and 150 having TKA) having primary, elective arthroplasties who had been administered TEA using our dosing protocol. Our protocol was to exclude patients with a documented history of a venous thromboembolic event being treated with lifelong anticoagulation, patients with a known congenital thrombophilia, or patients who had had a venous thromboembolic event within the 12 months preceding surgery. No patients actually were excluded from the study group based on these criteria in this study. As a control group, we obtained data for 234 patients (89 who had THA and 145 who had TKA) prospectively followed for total joint arthroplasty and who were operated on from April 1 to June 30, 2007, when this protocol was not in place. The use of these data derived from the perioperative blood conservation database met the requirements of our institutional ethics review board. No other routine patient care or surgical practices were altered during this time; specifically no other blood conservation program strategies were changed. All patients in both groups received 5000 IU of dalteparin for venous thromboembolism prophylaxis given subcutaneously for 10 days beginning on Postoperative Day 1. High-risk patients were administered dalteparin for 28 days postoperatively.
For the study group (new protocol), all scheduled patients were seen in the preoperative clinic 3 to 4 weeks before their surgery, where intraoperative and perioperative blood conservation strategies routinely are discussed and ordered. At that preoperative assessment visit, we ordered one intraoperative dose of 20 mg TEA per kg to be given either immediately before skin incision for THA or approximately 10 minutes before tourniquet release (at patellar clamping) for TKA. We chose a specific end point for each procedure to administer the drug as there are slight variations in surgical techniques among surgeons. We believed consistent specific timing of the administration of the TEA dose allowed for its maximum antifibrinolytic effect. To further simplify the introduction of this protocol, the hospital pharmacy supplied the TEA rounded off to the nearest 5 kg patient weight per 100 mg TEA in a 50-mL minibag (Table 1), which was attached to the patient’s chart on the day of surgery in the surgical preparation unit. In our institution, preoperative antibiotics are placed on the patient’s chart in a similar manner to be administered in the operating room by the anesthesiologists, so this was not a new situation for them.
Before implementation, all arthroplasty surgeons and hospital pharmacists had endorsed this protocol. One week before implementation, a memorandum explaining the new TEA protocol had been circulated to all anesthesiologists and nursing staff working in the perioperative areas.
All data were collected as part of a provincial blood conservation program (Ontario transfusion coordinators [ONTraC]) and maintained by two nurse coordinators [7]. Data collected included preoperative and postoperative hemoglobin and hematocrit levels, hemoglobin at discharge, change in hemoglobin (mean reduction in hemoglobin), allogeneic blood transfusions, length of hospital stay, and complications. Preoperative hemoglobin levels were drawn before surgery as part of our preadmission process. Postoperative hemoglobin levels were drawn routinely as part of a complete blood cell count on Postoperative Days 1 and 3. The mean reduction in hemoglobin was calculated by subtracting the lowest mean postoperative hemoglobin level from the mean preoperative hemoglobin level. Complications, namely thromboembolic events, were identified by cross-referencing all study patients with our joint arthroplasty database for any adverse events and by manual chart review.
TEA costs were obtained through our hospital pharmacist and were based on 2008 contract costing using a Sandoz (Princeton, NJ) generic brand. Costs for one unit of concentrated red blood cells were obtained through our hospital blood bank and also were based on 2008 costing. Costs were estimated using an average dose of TEA for a patient weighing 80 kg, or approximately $19.36 (Canadian dollars). A per patient cost of transfusion was calculated by multiplying the number of patients who had transfusions by the number of units of packed cells received by the cost per unit of packed cells divided by the number of patients operated on during the 3-month period. For 2008, we included the additional cost of the TEA bolus. A cost comparison was performed based on the reduction in transfusion rates for THAs and TKAs using TEA between 2007 and 2008. We made an assumption that on average any patient receiving an allogeneic red blood cell transfusion in our institution received two units of packed red blood cells, which was our normal transfusion protocol at that time. The approximate cost for one unit of concentrated red blood cells in Canada is $400.00 (Canadian dollars). Hidden costs such as pharmacist’s hours, portering costs, and blood bank salaries were not included.
We used an independent-samples t test (normal distribution) to compare change in hemoglobin or transfusion rates, for hip and knee separately between the two groups. Before the comparisons, a one-sample Kolmogorov-Smirnov test was performed on all data sets to confirm normal data distributions (SPSS 17, SPSS Inc., Chicago, IL).
Results
The decrease in hemoglobin was less in 2007 than in 2008 for patients who had THAs and TKAs (46 to 39 g/L [p < 0.001] and 45 to 36 g/L [p < 0.001], respectively) (Table 2). There was a reduction in transfusion rates in 2008 compared with 2007 for patients who had THAs and TKAs (13.5% to 3.6% [p < 0.001] and 13.1% to 2.0% [p < 0.001], respectively). Greater hemoglobin levels at discharge were observed in patients in 2008 than in 2007, more so for patients who had TKAs (p < 0.001) than for patients who had THAs (p = 0.143). The mean length of stay in hospital was shorter in 2008 than in 2007 for patients who had THAs (4.7 days from 5.4 days) and TKAs (4.5 days from 4.8 days). Five of the 493 patients (1%) had a deep vein thrombosis (DVT) identified on clinical examination and confirmed with an ultrasound of the affected extremity; three of these were patients who had received TEA in 2008. Three DVTs were in patients who had THAs, and two were in patients who had TKAs. These five patients were treated with therapeutic dalteparin or warfarin by the hematology service without additional complications.
All patients received the TEA as ordered. We identified approximate 10% (range, 13.5%−3.6%) and 11% (range, 13.1%−2.0%) reductions in transfusion rates using TEA for patients having THAs and TKAs, respectively. In 2007, we can calculate an approximate per patient cost of transfusion of $105.98 (Canadian dollars) ([31 patients transfused × two units of packed red blood cells × $400.00 (Canadian dollars) per unit of red blood cells]/234 patients), assuming on average any patient receiving an allogeneic red blood cell transfusion in our institution received two units of red blood cells. For 2008, including the additional cost of the TEA bolus, the calculated per patient cost of transfusion was reduced to $40.98 (Canadian dollars) (TEA cost [$19.36] (Canadian dollars) + per patient cost of transfusion of $21.62 (Canadian dollars), ie, [seven patients transfused × two units of packed red blood cells × $400.00 (Canadian dollars) per unit of red blood cells]/259 patients). In our institution, we perform approximately 1000 primary arthroplasties a year, which would amount to a yearly savings of approximately $65,000.00 (Canadian dollars).
Discussion
Despite aggressive attempts to reduce perioperative transfusion rates through our blood conservation program, we believed we had reached a plateau in our endeavors and looked for alternative strategies. We reviewed the literature regarding the use of antifibrinolytics, specifically TEA, and were impressed that multiple studies showed the ability of TEA to reduce blood loss and red blood cell transfusion in patients undergoing primary arthroplasties [1, 3–6, 8–10, 12, 13, 15, 17–19, 22] (Table 3). We concluded the most commonly used protocol of TEA reported in the literature was that of two doses of 10 mg per kg given 3 hours apart. We believed this would be a difficult protocol to institute as the second dose would be due at the time the patient was being discharged from the postoperative recovery room back to the floor and therefore either would be forgotten or delayed. We therefore asked whether one 20-mg per kg intraoperative dose of TEA in patients having primary THA or TKA would (1) decrease perioperative blood loss and red cell transfusion rates and (2) decrease cost.
We acknowledge several limitations. First, we used a database for all information, and such databases have inherent limitations to the quality of data collected. However, all data were collected prospectively as part of a provincial blood conservation program (ONTraC) and maintained by two full-time nurse coordinators [7]. Our hospital transfusion database was created in January 2004 as part of a provincial blood conservation initiative and contains documented hemoglobin levels and transfusion rates for all patients having arthroplasty. Second, we used the mean reduction in hemoglobin as a surrogate marker for blood loss and other factors may have led to a reduction in the mean hemoglobin, such as hemodilution from perioperative fluid resuscitation and the type of anesthetic used. Third, neuraxial anesthesia has been associated with less perioperative blood loss in patients having THA and TKA, compared with general anesthesia [11, 20]. The majority of patients at our institution receive spinal anesthesia for primary joint arthroplasty, however, and this has not changed appreciably between 2007 and 2008. Moreover, Zufferey et al. [22] did not find the type of anesthesia modified the results in their meta-analysis on the use of TEA. Fourth, our study was restricted to quantifying blood loss through the mean reduction in hemoglobin and blood transfusion requirements. We considered other potential sources of blood loss, such as wound drainage and wound hematomas, as beyond the scope of this study. Additional studies are needed to better address these issues. An analysis of major complications with our joint arthroplasty database and manual chart review failed to identify any infections or reoperations in the two groups. Finally, the calculation of transfusion cost savings is approximate and for Canada only and may not be the same for other countries.
One advantage of our study is that it compares a prospective cohort of patients operated on by the same surgeon group. This study also includes THA and TKA but with a different administration protocol for each procedure. In their meta-analysis of randomized controlled trials comparing the risk of receiving transfusion of allogeneic red blood cell units after TKA between patients who received TEA or not, Cid and Lozano [4] showed the ability of TEA to reduce transfusions in this population was independent of dose. They reported similar reductions in transfusion rates whether a low-dose (15–35 mg/kg) or a high-dose (135–150 mg/kg) protocol was used [4]. Other publications regarding the use of TEA in orthopaedic surgery also have shown the ability of TEA to reduce blood loss and red blood cell transfusion in patients undergoing primary arthroplasties [1, 3–5, 8–10, 12, 13, 15, 17–19, 22] (Table 3).
There is a paucity of literature discussing the cost-effectiveness of different TEA protocols. In their study of 39 cemented THAs using a dose of 10 mg/kg, followed by two interval doses 8 hours apart, Niskanen and Korkala [17] described TEA as an effective and economic drug for reduction of blood. Johansson et al. [10] calculated the use of TEA would save 47 euros per patient when considering the cost of blood and TEA only. Considering the same costs in our study, we estimate a reduction of approximately $65.00 (Canadian dollars) per patient cost of transfusion using TEA.
One could argue any increased complications, such as symptomatic DVTs, might erase any cost savings. One of our major concerns with the initiation of this protocol was that the antifibrinolytic effect of this medication might lead to an increase in venous thromboembolic events. However, two recent publications suggest TEA does not result in an increase in thromboembolic events [1, 12]. Lozano et al. [13] also reported the use of TEA was not associated with an increase in thrombotic complications either clinically or as documented by contrast venography. In addition, because inflammation and coagulation are directly associated, any change in one may indirectly affect the other. Nilsson et al. [16] found allogeneic transfusion was independently associated with a 1.5-fold increase in the risk of development of thromboembolism postoperatively.
We found one 20-mg per kg intraoperative dose of TEA in our patients having primary, elective THA and TKA reduced the perioperative decrease in hemoglobin compared with a similar cohort of patients for whom the protocol was not used. More importantly, this protocol led to a reduction in red blood cell transfusions, which can have associated severe immunomodulatory consequences [21]. We have found this protocol has been well received and accepted by the nurses, anesthesiologists, and arthroplasty surgeons: it has been used for patients of all six arthroplasty surgeons by all 30 anesthesiologists. We have observed that premixing the drug by the pharmacy to the nearest 5 g per 100 mg has facilitated pharmacy drug preparation, minimized dose variability and wastage, and increased ease of availability. This protocol also appears to be cost-effective in the Canadian marketplace. We have since adopted this protocol as part of the routine care of our patients having primary and revision arthroplasties. We continue to screen all patients for any history of a thromboembolic event. Patients with a positive history are reviewed by the medical director of the perioperative blood conservation program on an individual basis to discuss the appropriate risks and benefits. We continue to withhold TEA in the majority of these cases unless there is an overwhelming reason to try to minimize transfusion risk and with patient’s consent, such as with a patient who is a Jehovah’s Witness or a patient with antibodies to red blood cells.
References
Alvarez JC, Santiveri FX, Ramos I, Vela E, Puig L, Escolano F. Tranexamic acid reduces blood transfusion in total knee arthroplasty even when a blood conservation program is applied. Transfusion. 2008;48:519–525.
Astedt B. Clinical pharmacology of tranexamic acid. Scand J Gastroenterol Suppl. 1987;137;22–25.
Camarasa MA, Ollé G, Serra-Prat M, Martín A, Sánchez M, Ricós P, Pérez A, Opisso L. Efficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement: a randomized clinical trial. Br J Anaesth. 2006;96:576–582.
Cid J, Lozano M. Tranexamic acid reduces allogeneic red cell transfusions in patients undergoing total knee arthroplasty: results of a meta-analysis of randomized controlled trials. Transfusion. 2005;45:1302–1307.
Claeys MA, Vermeersch N, Haentjens P. Reduction of blood loss with tranexamic acid in primary total hip replacement surgery. Acta Chir Belg. 2007;107:397–401.
Fergusson DA, Hebert PC, Mazer CD, Fremes S, MacAdams C, Murkin JM, Teoh K, Duke PC, Arellano R, Blajchman MA, Bussieres JS, Cote D, Karski J, Martineau R, Robblee JA, Rodger M, Wells G, Clinch J, Pretorius R; BART Investigators. A comparison of aprotinin and lysine analogues in high-risk cardiac surgery. N Engl J Med. 2008;358:2319–2331.
Freedman J, Luke K, Monga N, Lincoln S, Koen R, Escobar M, Chiavetta J. A provincial program of blood conservation: The Ontario Transfusion Coordinators (ONTraC). Transfus Apher Sci. 2005;33:343–349.
Gill JB, Rosenstein A. The use of antifibrinolytic agents in total hip arthroplasty: a meta-analysis. J Arthroplasty. 2006;21:869–873.
Ho KM, Ismail H. Use of intravenous tranexamic acid to reduce allogeneic blood transfusion in total hip and knee arthroplasty: a meta-analysis. Anaesth Intensive Care. 2003;31:529–537.
Johansson T, Pettersson LG, Lisander B. Tranexamic acid in total hip arthroplasty saves blood and money: a randomized, double-blind study in 100 patients. Acta Orthop. 2005;76:314–319.
Juelsgaard P, Larsen UT, Sorensen JV, Madsen F, Soballe K. Hypotensive epidural anesthesia in total knee replacement without tourniquet: reduced blood loss and transfusion. Reg Anesth Pain Med. 2001;26:105–110.
Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W. Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res. 2009;123:687–696.
Lozano M, Basora M, Peidro L, Merino I, Segur JM, Pereira A, Salazar F, Cid J, Lozano L, Mazzara R, Macule F. Effectiveness and safety of tranexamic acid administration during total knee arthroplasty. Vox Sang. 2008;95:39–44.
Mannucci PM. Hemostatic drugs. N Engl J Med. 1998;339:245–253.
Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland DE. Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: a prospective, randomised controlled trial. J Bone Joint Surg Br. 2007;89:306–309.
Nilsson KR, Berenholtz SM, Garrett-Mayer E, Dorman T, Klag MJ, Pronovost PJ. Association between venous thromboembolism and perioperative allogeneic transfusion. Arch Surg. 2007;142:126–132; discussion 133.
Niskanen RO, Korkala OL. Tranexamic acid reduces blood loss in cemented hip arthroplasty: a randomized, double-blind study of 39 patients with osteoarthritis. Acta Orthop. 2005;76:829–832.
Orpen NM, Little C, Walker G, Crawfurd EJ. Tranexamic acid reduces early post-operative blood loss after total knee arthroplasty: a prospective randomised controlled trial of 29 patients. Knee. 2006;13:106–110.
Rajesparan K, Biant LC, Ahmad M, Field RE. The effect of an intravenous bolus of tranexamic acid on blood loss in total hip replacement. J Bone Joint Surg Br. 2009;91:776–783.
Sharrock NE, Mineo R, Urquhart B, Salvati EA. The effect of two levels of hypotension on intraoperative blood loss during total hip arthroplasty performed under lumbar epidural anesthesia. Anesth Analg. 1993;76:580–584.
Stainsby D, Jones H, Asher D, Atterbury C, Boncinelli A, Brant L, Chapman CE, Davison K, Gerrard R, Gray A, Knowles S, Love EM, Milkins C, McClelland DB, Norfolk DR, Soldan K, Taylor C, Revill J, Williamson LM, Cohen H; SHOT Steering Group. Serious hazards of transfusion: a decade of hemovigilance in the UK. Transfus Med Rev. 2006;20:273–282.
Zufferey P, Merquiol F, Laporte S, Decousus H, Mismetti P, Auboyer C, Samama CM, Molliex S. Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology. 2006;105:1034–1046.
Acknowledgments
We acknowledge Drs. Steven MacDonald, James McAuley, Richard McCalden, and Robert Bourne for contribution of their patients to this study and Jeff Guerin for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (JH, DN) has received funding from Smith and Nephew (Memphis, TN), DePuy (Warsaw, IN), and Stryker (Mahwah, NJ).
Each author certifies that his or her institution approved the protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at London Health Sciences Center.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-010-1270-3
About this article
Cite this article
Ralley, F.E., Berta, D., Binns, V. et al. One Intraoperative Dose of Tranexamic Acid for Patients Having Primary Hip or Knee Arthroplasty. Clin Orthop Relat Res 468, 1905–1911 (2010). https://doi.org/10.1007/s11999-009-1217-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-1217-8