Abstract
Current-generation metal-on-metal hip resurfacing implants (SRAs) have been in widespread global use since the 1990s, and in the United States, specific implants have recently been approved for clinical use. Many recent publications describe short-term survivorship achieved by either implant-designing surgeons or high-volume centers. National joint replacement registries (NJRRs) on the other hand report survivorship achieved from the orthopaedic community at large. We therefore reviewed SRA survivorship from national registry data and compared with that reported from individual centers. Additionally, we compared SRA survivorship reported by registries and compared prognosticators for failure with those of conventional total hip arthroplasty (THA). Although resurfacing was associated with an overall increased failure rate in comparison to THA (Australian registry 5-year cumulative revision rate [CRR], 3.7% and 2.7%, respectively), there were exceptions to this. Male patients younger than 65 years with primary osteoarthritis had equivalent results with SRA and THA (Australian registry 5-year CRR, 2.5% and 2.8%, respectively). Head size over 50 mm in diameter was a predictor of surface replacement arthroplasty survivorship and only females with a head diameter of 50 mm or greater (14% of females) had a comparable survivorship to males. Diagnoses other than primary osteoarthritis bear a higher risk of early revision of SRA as compared with THA. Revision of SRA does not lead to reproducible results with rerevision rates of 11% at 5 years. Given these predictors of failure, our review of data from the NJRR suggests stringent patient selection criteria might enhance the survival rates of SRA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical techniques for contemporary primary THA are well established. Several National Joint Replacement Registries (NJRRs) have reported the intermediate- to long-term survivorship of THA [5, 13, 18, 21, 22, 38, 39]. The data collected in the NJRR have some important weaknesses, but also represent the survivorship of thousands of implants [35]. This allows for identifying various prognosticators for implant failure such as male gender, age younger than 60 years, dysplasia of the hip (DDH) or avascular necrosis (AVN) as the primary diagnosis, and certain bearing surfaces [5, 18, 38]. The longevity of the implant in young patients remains the most problematic concern [2, 20]. Unfortunately, the introduction of cementless designs has not led to a uniformly major improvement in survivorship [5, 7, 24]. Although these components often have reproducible bone ingrowth rates, the bearing has often been the weak link in the system with issues of polyethylene wear and osteolysis.
Surface replacement arthroplasty (SRA) proponents cite many proposed advantages for use in the young and active patient such as preservation of proximal femoral bone stock, improved patient function, and lower wear rates secondary to the use of metal-on-metal bearings [1, 8, 12, 31, 40]. The first generations of SRA had been abandoned with high midterm failure rates, ranging from 12% to 60% resulting from the femoral component design and the polyethylene bearing surface [3, 16, 30]. The contemporary generation hip resurfacings have recently been introduced and can be considered a relatively “new” procedure. They combine a cementless, porous-coated, monoblock acetabular component with a stemmed femoral component implanted with bone cement and a metal-on-metal bearing articulation. Short-term clinical followup reports of 4 to 7 years suggest survival rates varying between 94% and 100% (Table 1). Femoral neck fractures and aseptic loosening [1] are reportedly the most frequent causes of failure (Table 1). These early results have been published mainly from the designer centers. The experiences of these high-volume arthroplasty surgeons have led to adaptations in the surgical techniques and, consequently, the results are still “evolving” [4, 8, 26, 31, 34]. Moreover, studies of risk factors highlight the importance of surgical expertise, patient selection criteria, and good bone quality for implant survival [4, 8, 26, 31, 34]. Although resurfacing might be an alternative to conventional THA, these criteria specifically apply to SRA and could make these procedures more complex and potentially less reproducible than conventional THA. The survivorship of various SRA designs has now been published from several NJRRs [5, 28, 39] and can be compared with those of conventional THA.
We therefore reviewed reports from these NJRR’s to (1) determine whether the results of SRA are indeed less reproducible than those of THA; (2) identify the failure modes; (3) determine whether we could identify prognosticators for early failure that might enhance survival of SRA by better patient selection; (4) determine whether the prognosticators were similar for SRA and THA; and (5) determine the survival of revisions of SRA.
Materials and Methods
We obtained data on THA and SRA from the Annual Reports of the 2008 Australian [5], the English (and Welsh) [28] Joint Replacement Registry (published in 2008), and the 2006 and 2007 Annual Swedish reports [38, 39]. We used the key words “hip replacement” and “joint replacement registries” to identify articles in PubMed that reported data from the NJRR and that had been published in the English literature between 2000 and 2009. The most recent data from the Finnish, Norwegian, and Danish NJRR on THA were derived from four published reports [13, 18, 21, 22].
We then first compared the survival and revision rates of SRA with those of aged-matched THA results. Second, we compared the different failure modes of SRA and THA. The failure modes within the first 3 to 5 years could be compared in the Swedish NJRR but were not adjusted for age [38, 39]. Third, we identified the prognosticators for failure of THA reported in the NJRR. These were (1) gender; (2) age; (3) indication for surgery; (4) fixation mode; and (5) bearing surface. Three prognosticators were considered applicable for the survival of SRA: (1) gender; (2) age; and (3) indication for surgery. We then compared the influence of these three prognosticators on failure of SRA and THA. Finally, we searched the registries for the survivorship of the revisions of SRA.
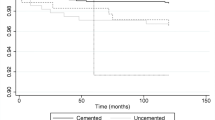
Revision rates were estimated in the registries using the Kaplan-Meier survival analysis method [5, 28, 38, 39]. Cumulative percent revision was used in the Australian registry [5]. This term refers to the complement (in probability) of the Kaplan-Meier survivorship function at a certain time multiplied by 100 [5]. Hazard ratios were used to evaluate the relative risks related to each risk factor with adjustment for the other factors. The log-rank tests and hazard ratios reported with each curve were used for analytical comparisons of prostheses survival in the Australian Registry [5]. Multivariable Cox regression was used to estimate hazard ratios for prosthesis type, age group, gender, and indication for surgery as risk factors for revision. In all models, age was included as a categorical variable [28]. Cox regression analysis to adjust for interference between different variables and the followup period and outcome was used in the Swedish registry [39].
Results
The procedure type (SRA versus THA) was the most important predictor for implant survival of hip arthroplasty in England and Wales [28]. After adjusting for age, gender, and physical status, SRA had a fivefold increased risk for revision and a considerably higher first-year revision rate of 1.6% in comparison to cemented THA (0.3%) [28]. The relative risk for revision after SRA was more than threefold after adjustment for age, gender, diagnosis, and approach in Sweden [39]. In Australia, SRA had a higher (p < 0.001) revision rate than THA after adjustment for gender and age. The 5-year cumulative percentage revision rate (CRR) of SRA was 3.7% as opposed to 2.7% for THA (Table 2) [5]. The Birmingham Hip Resurfacing (BHR) (Smith & Nephew, Memphis, TN) was the most commonly used device with the longest followup [5, 28, 39]. The 3-year revision rate was 1.8% in England and Wales [28]. The revision burden was 3.4% for SRA in Sweden [39]. The 7-year CRR was 4.6% as opposed to 3.4% for THA in Australia [5]. The number of revisions per 100 observed component years for the BHR was 0.8 as opposed to 2.6 and 2.3 for the ASR (DePuy, Warsaw, IN) and Durom (Zimmer, Warsaw, IN), respectively [5].
Aseptic loosening (31%) and fracture (31%) accounted for 66% of revisions of SRA [28, 39] (Table 3). In THA, aseptic loosening (46%) and dislocation (19%) represented 66% of the indications for revision [38]. Fifty-five percent of SRA revisions were directed toward the femoral components as opposed to only 12% of THA revisions. Cup only (14%) or both component revisions (31%) accounted for 45% of SRA revisions, whereas these revisions were performed in 86% of the THA cases in patients younger than 50 years of age [38, 39].
We identified three prognostic factors that differed with SRA and THA: gender, age, and surgical indication. Male patients had a lower risk of revision of SRA than females irrespective of age [5, 39]. The 5-year CRR for females was 2.5 times higher than that of males. This difference in failure rates disappeared after adjustment for femoral component sizes 50 mm or greater, which were used in 14% of the female and in 84% of the male patients. In addition, within gender, head sizes 50 mm or greater were associated with a lower (p < 0.001) risk of revision at 5 years, which was comparable to the CRR of THA (Table 2) [5]. The 1-year failure rates of SRA in females (2.1%) were considerably higher than those for THA (0.3%) in Sweden [39]. The 5-year CRR of SRA in females was more than twofold higher than that of THA (Table 2) [5]. Younger females did better with THA and THA in females with an older age at the time of surgery did best [5, 28]. In males, the 1-year revision rates of SRA were 1% higher than those of THA (0.6%) [28].
At 5 years, however, the CRR of SRA (2.6%) was equal to THA (2.8%) [5]. Males younger than 64 years of age did best with SRA [5, 28]. Finally, the differences in revision rates between SRA and THA were larger in females than in males (Table 2) [5]. Patients younger than 55 years of age at the time of SRA had the lowest CRR at 1 and 5 years [5, 28]. The 5-year CRR in males younger than 65 years of age remained comparable to those younger than 55 years of age. In females, however, a dramatic increase in revision rates was seen in those between 55 and 64 years of age (Table 2) [5]. Age had an opposite effect on the 5-year CRR of SRA as compared with THA; the younger the patients undergoing SRA, the lower their 5-year CRR was as opposed to a lower CRR in older patients with THA (Table 2) [5]. The indications for SRA did not considerably vary between different NJRRs with primary osteoarthritis (OA) accounting for 94% of the indications followed by DDH (3%) and AVN (2%), which were associated with a high 5-year CRR of 12% and 6%, respectively [5, 39]. The 5-year CRR of SRA for OA was 1% higher than that of THA, whereas the 5-year CRR of SRA for DDH was four times higher than that of THA (3%) [5].
Eleven percent of the revised SRAs were rerevised within 5 years in the Australian NJRR. The rerevision rate of SRA was 2.8 per 100 observed component years. The 1-, 3-, and 5-year CRRs were 2.9%, 8.4%, and 11.1%, respectively. These results were similar to the rerevision rate of conventional THA (8.2% at 3 years) and were higher than the 1-, 3-, and 5-year CRRs of primary THA (1.2%, 2%, and 2.7%, respectively) [5].
Discussion
The results of new technologies such as the current-generation SRA devices reported from highly specialized centers are often the best possible results and do not necessarily reflect what is achieved with general use. Registries not only capture the survival rates of SRA performed nationwide, but also capture those of conventional THA. It was our aim to evaluate and compare the midterm survivorship and the prognosticators for failure of SRA with those of THA. Specifically, we reviewed reports from these NJRRs to (1) determine whether the results of SRA are indeed less reproducible than those of THA; (2) identify the failure modes; (3) determine whether we could identify prognosticators for early failure that might enhance survival of SRA by better patient selection; (4) determine whether the prognosticators were similar for SRA and THA; and (5) determine the survival of revisions of SRA.
Registries have a number of limitations. First, the weakest potential link remains the quality of data collection. This possible hazard is efficiently bypassed in the registries with the longest track records [5, 13, 18, 21, 22, 38, 39] with capture rates exceeding 95% of cases performed. Unfortunately, the data from only a few registries are directly accessible and the data of some registries are only early followup data [5, 28, 38, 39]. Second, failure of hip arthroplasties is often multifactorial [33]. Registry data lack specific parameters important for the survival of the implant such as patient-related data (eg, body weight, femoral head cysts [1]), surgical experience [4, 19, 25, 26, 34], and surgical technique (eg, computer-assisted navigation [10, 32]). Third, most often only revision is considered a failure. Everything comes down to the definition of “failure,” which in survival analysis is interpreted as an event instead of a process such as loosening of a component [11, 22]. Radiographic features such as stem shaft angle and abduction of the socket are important for failures in SRA [1, 8, 27], but their influence as a predictor for failure will not be noticed if they are not captured in the database. Postoperative complications (eg, nerve palsy [6, 26]) can be considered as important modes of failure. The overall complication rate varied from 0% to 18% in a meta-analysis of 13 trials with 3594 SRAs. The mean revision rate, however, was 3.7% (Table 1). The overall success rate would thus be an overestimation if only revision is considered as the end point. Functional parameters are especially important with regard to “failure” of SRA in the young, active patient. Some questionnaires (EQ-5D index) are now implemented in the Swedish Hip Registry, but no data on SRA are currently available. It will take approximately another 3 to 5 years before sufficient prospective data will be available [22]. Therefore, taking all of these considerations together, the current “failure” rates of SRA and conventional THA, solely based on registry data with revision as the end point, may actually be an underestimation. Fourth, poorly performing implant designs become obvious from the registry data after 5 to 7 years [13, 22], if not sooner. This was reproduced with specific SRA implants [5, 39]. The differences between well-performing implants are much harder to distinguish. Nevertheless, this would be desirable because the performance of most implants is continuously improving and we strive to identify the best implants. Confounding factors other than age, gender, and diagnosis are often not considered and therefore small differences between well-performing implants must be interpreted with caution. Additionally, lower rates of revision surgery have been observed in countries with longstanding registries [9]. Registry results provide a feedback loop to the surgeons and have an impact on indications, procedures, and implants used [5, 22]. For example, since 2003, there has been little change in the proportion of females having primary THA in the Australian NJRR. However, there has been a 5% decline in females undergoing SRA over a time period of 4 years, probably indicating the early higher revision rates in females with SRA had an impact on the indications for the procedure [5]. In other words, there is some form of positive bias in general practice introduced by the use of NJRR. Finally, it is important to understand that registries may be capturing implants in different phases of their implementation. In other words, an implant that has been on the market for 10 years when a registry begins will not have any learning curve captured in the registry data compared with an implant that is released after the registry has begun. In the early years of a registry, therefore, there is a bias introduced against new implants and technologies associated with a learning curve. Some may argue that is valid and all new implants should be assessed and compared with current well-performing implants. Others may argue that this is an unfair bias potentially restricting the ability to evaluate any proposed long-term benefits of an implant by only focusing on the very short-term results. Obviously, once a registry is well-established and has been in place for many years, this becomes less of a concern as each implant’s early-year results can be evaluated and compared.
Despite these limitations, registries provide an enormous amount of data with relevant information regarding survival rates that can be correlated to prognosticators such as primary diagnosis, age, and gender. The early failure rates of SRA as captured in the NJRR were somewhat higher but comparable to those reported in the literature (Table 1). However, they were substantially higher than those of THA after adjustment for age and gender.
Important information can be derived from carefully evaluating the revision data in terms of which component failed and the mode of failure. Aseptic loosening was a problem equivalent to periprosthetic fracture as an indication for revision of SRA in 31% of the cases [39], which was similar to the incidence reported in the literature [1, 6, 8, 12, 14, 15, 17, 23, 26, 29, 36, 37, 40] and 15% less than the incidence in revision of THA [38]. In SRA, 55% of the time a stem-only revision was performed. In THA, 55% of the time a cup only revision was performed. In other words, the resurfacing shells and the THA stems underwent the fewest revisions. Would the combination of both lead to fewer revisions in the younger patient population? Unfortunately, no data on large-diameter metal-on-metal THA are available yet.
The effects of gender and age on survivorship are interrelated. There was an opposite effect of gender as a prognosticator for failure of SRA in comparison to THA, which could not be detected from the published studies on SRA survival (Table 1). Females with a SRA have a higher risk for failure than age-matched males and females with a THA. In contrast, males younger than 65 years of age at the time of surgery had comparable, and even slightly improved, 5-year survival rates with SRA than with THA. In addition, it would appear that one of the most important predictors for 5-year survival of SRA was the use of component sizes 50 mm or greater in diameter. The survival rates of both females and males with these component sizes were equal to each other.
Patients with OA as the primary diagnosis for hip arthroplasty had the best survival rates and the use of SRA for DDH and AVN should be cautioned.
The premise that a revision of SRA leads to equal results of a primary THA should be cautiously reevaluated because the 5-year rerevision rates of SRA (11%) were higher than those of primary THA at 5 (2.7%) and even 7 (3.4%) years. These rerevision rates were actually equal to the rerevision rates of an all-component THA revision.
In summary, the knowledge of SRA is evolving and the techniques are changing. Despite their limitations, registries should be considered as a sensitive detection tool that can provide early data on component outcomes, often sooner than randomized, controlled trials, depending on the outcome measure being evaluated. Current registry data on SRA demonstrate an overall increased failure rate compared with THA in all patients with primary OA, with the exception of the younger male patient and patients who can accommodate components with head sizes over 50 mm in diameter. However, males younger than 65 years of age and women with larger component sizes receiving SRA have equivalent short-term survivorship as patients receiving THA when stringent SRA criteria are adhered to. It must also be emphasized that the survivorship of a revision of a failed SRA should not be considered as equivalent to a primary THA because the rerevision rate is much higher and instead is equivalent to the rerevision rate of a failed THA.
References
Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39.
Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA, Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients < 40 years old. J Arthroplasty. 2001;16(Suppl 1):140–144.
Amstutz HC, Dorey E, O’Carroll PF. THARIES resurfacing arthroplasty. Evolution and long-term results. Clin Orthop Relat Res. 1986;213:92–114.
Amstutz HC, Le Duff MJ, Campbell PA, Dorey FJ. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing. Results of 600 Conserve Plus with a 3- to 9-year follow-up. J Arthroplasty. 2007;22:481–489.
Australian Orthopaedic Association Web site. National Joint Replacement Registry Annual Report 2008. Available at: www.dmac.adelaide.edu.au/aoanjrr/. Accessed January 6, 2009.
Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings. J Bone Joint Surg Br. 2005;87:324–329.
Beaulé PE, Dorey FJ. Survivorship analysis of cementless total hip arthroplasty in younger patients [Letter]. J Bone Joint Surg Am. 2001;83:1590–1591.
Beaulé PE, Dorey FJ, LeDuff MJ, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93.
Bourne RB, Maloney WJ, Wright GJG. An AOA critical issue the outcome of the outcomes movement. J Bone Joint Surg Am. 2004;86:633–640.
Cobb JP, Kannan V, Dandachli W, Iranpour F, Brust KU, Hart AJ. Learning how to resurface cam-type femoral heads with acceptable accuracy and precision: the role of computed tomography-based navigation. J Bone Joint Surg Am. 2008;90:57–64.
Collis DK, Mohler CG. Comparison of clinical outcomes in total hip arthroplasty using rough and polished cemented stems with essentially the same geometry. J Bone Joint Surg Am. 2002;84:586–592.
Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184.
Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, Havelin LI. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br. 2007;89:1574–1580.
Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Am. 2008;90:1137–1142.
Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years: an independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89:1431–1438.
Howie DW, Campbell D, McGee M, Cornish BL. Wagner resurfacing arthroplasty: the results of one hundred consecutive arthroplasties after eight to ten years. J Bone Joint Surg Am. 1990;72:708–714.
Jacobs MA, Goytia RN, Bhargava T. Hip resurfacing through an anterolateral approach. J Bone Joint Surg Am. 2008;90:38–44.
Johnsen SP, Sørensen HT, Lucht U, Søballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. J Bone Joint Surg Br. 2006;88:1303–1308.
Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001;83:1622–1629.
Kim WC, Grogan T, Amstutz HC, Dorey FJ. Survivorship comparison of THARIES and conventional hip arthroplasty in patients younger than 40 years old. Clin Orthop Relat Res. 1987;214:269–277.
Mâkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170.
Malchau H, Garellick G, Eisler T, Kärrholm J, Herberts P. The Swedish hip registry. Clin Orthop Relat Res. 2005;441:19–21.
McBryde CW, Shears E, O’Hara JN, Pynsent PB. Metal-on-metal hip resurfacing in developmental dysplasia. J Bone Joint Surg Br. 2008;90:708–714.
McLaughlin JR, Lee KR. Total hip arthroplasty in young patients. Clin Orthop Relat Res. 2000;373:153–163.
Mont MA, Ragland PS, Etienne G, Seyler TM, Schmalzried TP. Hip resurfacing arthroplasty. J Am Acad Orthop Surg. 2006;14:454–463.
Mont MA, Seyler TM, Ulrich SD, Beaulé PE, Boyd HS, Grecula MJ, Goldberg VM, Kennedy WR, Marker DR, Schmalzried TP, Sparling EA, Parker Vail T, Amstutz HC. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70.
Morlock MM, Bishop N, Zustin J, Hahn M, Rüther W, Amling M. Modes of implant failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg Am. 2008;90:89–95.
National Joint Registry for England and Wales. Fourth Annual Report. Available at: www.njrcentre.org.uk. Accessed January 6, 2009.
Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600.
Schmalzried TP, Buttman D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677–688.
Schmalzried TP, Silva M, de la Rosa MA, Choi E-S, Fowble VA. Optimizing patient selection and outcomes with total hip resurfacing. Clin Orthop Relat Res. 2005;441:200–204.
Seyler TM, Lai LP, Sprinkle DI, Ward WG, Jinnah RH. Does computer-assisted surgery improve accuracy and decrease the learning curve in hip resurfacing? A radiographic analysis. J Bone Joint Surg Am. 2008;90:71–80.
Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing. J Bone Joint Surg Br. 2005;87:463–464.
Siebel T, Maubach S, Morlock MM. Lessons learned from early clinical experience and results of 300 ASR hip resurfacing implantations. Proc Inst Mech Eng. 2006;220:345–353.
Söderman P, Malchau H, Herberts P, Zügner R, Regnér H, Garellick G. Outcome after total hip arthroplasty. Part II: disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop Scand. 2001;72:113–119.
Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five year results of the Birmingham hip resurfacing arthroplasty. J Bone Joint Surg Br. 2008;90:436–441.
Stulberg BN, Trier KK, Naughton M, Zadzilka JD. Results and lessons learned from a United States hip resurfacing investigational device exemption trial. J Bone Joint Surg Am. 2008;90:21–26.
Swedish Hip Arthroplasty Register Annual Report 2006. Available at: www.jru.orthop.gu.se. Accessed January 6, 2009.
Swedish Hip Arthroplasty Register Annual Report 2007. Available at: www.jru.orthop.gu.se. Accessed January 6, 2009.
Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170.
Author information
Authors and Affiliations
Corresponding author
Additional information
One the authors (SJM) is a consultant with DePuy. The other author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
About this article
Cite this article
Corten, K., MacDonald, S.J. Hip Resurfacing Data from National Joint Registries: What Do They Tell Us? What Do They Not Tell Us?. Clin Orthop Relat Res 468, 351–357 (2010). https://doi.org/10.1007/s11999-009-1157-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-1157-3