Abstract
Skeletal reconstruction of large tumor resection defects is challenging. Free vascularized fibular transfer offers the potential for rapid autograft incorporation in limbs compromised by adjuvant chemotherapy or radiation. We retrospectively reviewed 30 patients treated with free vascularized fibular graft reconstruction of large skeletal defects after tumor resections (mean defect length, 14.8 cm). The minimum followup was 2 years (mean, 4.9 years; range, 2–15 years). One patient died with liver and lung metastases at 3 years postoperatively. Loss of limb occurred in one patient. Five patients either had metastatic disease (one patient) or had metastatic disease (four patients) develop after treatment, with a mean time to metastasis of 18 months. The overall complication rate was 16 of 30 (53%), with a reoperation rate of 12 of 30 (40%). Union was attained in all 30 grafts. Primary union was attained in 23 (77%) at a mean of 6 months. Secondary union was achieved in seven (23%) after revision fixation and bone grafting; the mean subsequent time to union was 9.2 months, with an index of 1.33 additional operations per patient. Graft fracture (20%) and infection (10%) were other common complications. Despite a high complication rate, free vascularized fibular graft reconstruction offers a reliable treatment of large skeletal defects after tumor resection without increased risk of limb loss, local recurrence, or tumor metastasis.
Level of Evidence: Level IV, case series. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Limb salvage surgery has largely replaced amputation for operative treatment of multiple types of neoplasms in the upper and lower extremities [2, 25, 28, 32]. However, skeletal reconstruction after bone loss remains challenging with regard to limb length preservation, cosmesis, and function. Patients requiring resection of sarcomas, in particular, are often young and thus subject their reconstructed limbs to high functional demands and cosmetic scrutiny.
Multiple reconstructive options for skeletal defects exist, including allografts [4, 8, 12, 15, 21, 25, 26, 29], autografts [1–7, 9, 11, 13–20, 33], and endoprostheses [10, 22, 24, 25, 31]. Given the relatively young age of most patients with a primary bone sarcoma [11, 22], there is a premium on durability of reconstruction. As biologically favorable alternatives to allograft reconstruction have evolved, reconstruction techniques using free vascularized bone have become well-described and well-established [9, 10]. Of the multiple osseous donor sites, the free vascularized fibular graft (FVFG) has become the most commonly transferred vascular autograft for reconstructing segmental bone defects after trauma, nonunion, pseudarthrosis, osteonecrosis, and tumor resection [9, 10, 22, 24]. The process of microvascular free fibular transfer was first reported in 1975 by Taylor et al. [30] who described two patients with limb-threatening lower extremity trauma. In 1977, Weiland et al. [32] reported the first reconstruction of long bones with vascularized fibula after tumor resection. Since these early reconstructions, complication rates reported after FVFG reconstruction remain high (37%–80%), although the frequency of the different complications varies widely [1, 3, 5, 6, 9, 15].
Unlike cortical allograft and nonvascularized autograft, vascularized bone grafts do not depend on gradual revascularization [5, 9, 10]. Revascularization of nonvascularized autograft and allograft is slow and usually restricted to the peripheral third of the graft [2, 5, 12]. Thus allograft and nonvascularized autograft heal by creeping substitution, the slow process of simultaneous osteoclastic and osteogenic activity, which weakens these grafts and renders them susceptible to nonunion, delayed union, and fracture [15, 17, 23]. Consequently, their use is limited to defects smaller than 5 to 8 cm in length. Vascularized autografts, in contrast, retain their biologic and mechanical properties, heal by primary union, and can hypertrophy in response to load [13] (Fig. 1). The FVFG offers broader structural application and lower donor site morbidity than vascularized rib or iliac crest grafts [19]. The FVFG can provide a cortical strut for reconstructions up to 26 cm in length [3, 24]. Additionally, the robust dual blood supply of the fibula with its arborescent nutrient endosteal vessels and six to nine periosteal vessels renders it amenable to transverse and longitudinal splitting. Reconstructions using FVFG have the potential for rapid union and are more resistant to infection in hostile environments than allografts [6]. This offers the potential to minimize complications in patients whose underlying physiologic milieu may be compromised owing to chemotherapy, immunosuppression, or radiation therapy. Numerous authors have described FVFG for reconstruction after resections for tumors, yet their reports contain little data regarding patient survival, local recurrence, or tumor metastasis and variable data regarding specific complications [1, 3, 5, 6, 9, 15, 33].
(A) A radiograph shows an AP projection of the humerus of a patient (aged 15 years) taken 9 years after FVFG reconstruction of the proximal diaphysis after resection of an osteosarcoma. (B) A lateral view of the same humerus is shown. The fibula has hypertrophied to the approximate size of unresected portions of the distal diaphysis.
Based on our clinical experience with 30 free vascularized fibular transfers for reconstruction of skeletal defects after oncologic resection, we investigated six variables (three oncologic parameters and three common complications): (1) limb survival, (2) local recurrence, (3) tumor metastasis, (4) graft nonunion, (5) graft fracture, and (6) infection.
Patients and Methods
We retrospectively reviewed our records for all 30 FVFG reconstructions of skeletal defects after tumor resection performed between 1980 and 2006. Patients were identified from oncology and reconstructive surgery databases and medical records were reviewed to supplement information from the database. We recorded patient demographics, primary diagnosis, prior surgical procedures, location of malignancy, presence of metastatic disease, survivorship, adjuvant therapy, medical history, presence of local recurrence, complications (including infection rates), and operative details. Fifteen male and 15 female patients were identified, with a mean age of 29.3 years (range, 7–75 years) (Table 1). There were 27 primary bone tumors and three soft tissue sarcomas invading underlying bone. Sites of resection and reconstruction included the femur (n = 9), tibia (n = 8), radius (n = 7), humerus (n = 5), and ulna (n = 1). Primary osseous tissue diagnoses included osteosarcoma (n = 14), giant cell tumor (n = 4), chondrosarcoma (n = 2), adamantinoma (n = 2), Ewing’s sarcoma (n = 1), fibrosarcoma (n = 1), malignant fibrous histiocytoma (n = 1), aneurysmal bone cyst (n = 1), and intraosseous hemangioma (n = 1). Diagnoses for soft tissue sarcomas invading bone included malignant fibrous histiocytoma (n = 1), synovial sarcoma (n = 1), and liposarcoma (n = 1). The minimum followup was 2 years (mean, 4.9 years; range, 2–15 years). No patients were recalled specifically for this chart review study. No patients were lost to followup. We had prior Institutional Review Board approval with a waiver of written consent from patients.
Twenty-four resections were for malignant bone or soft tissue tumors and six resections were for aggressive benign tumors of bone. Wide resection of the primary tumor was attempted in all patients. Twenty-four FVFG reconstructions were performed at the time of tumor resection and six were performed in delayed fashion. There were six osteocutaneous and 24 osseous grafts. Resections were performed by one of three orthopaedic surgeons (BEB, LSL, JH). Harvest and inset of FVFG were performed by one of four orthopaedic or plastic surgeons. Fibulas were harvested through a standard technique [20]. Arterial anastomosis was generally end-to-end using various donor vessels. Venous anastomosis was generally end-to-end using either one or two associated venae comitantes [20]. When an osteocutaneous flap was not used, Cook implantable Doppler probes (Cook Vascular Inc, Vandergrift, PA) were placed into recipient vessels. The mean length of the skeletal defect after resection was 14.8 cm. The mean length of the inset fibula was 17.5 cm. Osteosynthesis was adapted for individual reconstructions by one of the three surgeons but typically involved plate and screws (n = 17), intramedullary nail (n = 9), external fixation (n = 3), or screws alone (n = 1). Twenty-one reconstructions were intercalary and seven were for arthrodesis (four wrist, two ankle, one knee); there were two epiphyseal transfers.
We instituted continuous elevation of the limb for the first 14 postoperative days in patients with upper extremity grafts and lower extremity grafts below the knee. When necessary (eg, for patient transfer), a dependent position was permitted for less than 30 seconds at a time during this period. Patients with femoral grafts received 3 days of bed rest. For all patients, supervised passive ROM was initiated in the hospital beginning on the second postoperative day under the guidance of an inpatient physical therapist (lower extremity grafts) or an occupational therapist (upper extremity grafts). For patients with lower extremity grafts, supervised instruction was given for transfer to a wheelchair with elevated leg rests by a physical therapist. Active ROM and dependent limb position were permitted in the third postoperative week. Use of crutches or a walker for mobility without weightbearing on the operative leg was guided by a physical therapist for patients with lower extremity grafts. All patients were restricted from weightbearing in the operated extremity until the following criteria were met: absence of pain and periosteal new bone formation bridging the osteosynthesis site on two orthogonal radiographic projections as determined by one of three treating surgeons (BEB, LSL, JH).
Clinic followup occurred 2 weeks postoperatively for suture/staple removal and wound inspection, 6 weeks postoperatively, and then every 4 to 8 weeks until osseous union was deemed adequate by one of three treating surgeons (BEB, LSL, JH). Radiographs were obtained at every postoperative visit during this time. For the purpose of radiographic evaluation, all postoperative radiographs were evaluated independently by one, blinded musculoskeletal radiologist (CH) for evidence of union, hypertrophy, resorption, fracture, or hardware migration. Osseous union was defined as described by Gebert et al. [9] and included attenuation or absence of osteotomy line, presence of external bridging callus, or bony trabeculae spanning the osteosynthesis site.
Results
Twenty-nine of 30 patients (97%) retained a functionally salvaged limb during the followup; we converted one reconstruction to an amputation. At the end of the study period, one patient had died (Table 1) of metastatic disease.
Two patients had local recurrences (Table 2). One had a hemicortical resection of the femur for treatment of synovial sarcoma of the thigh that invaded bone. This was reconstructed with a FVFG and intramedullary nail. Local recurrence and lung metastases were diagnosed simultaneously 2.5 years postoperatively. The other patient had a giant cell tumor of the distal tibia and has had three total episodes of local recurrence despite repeat resection.
Five patients (17%) had metastatic disease (Table 2). One patient had lung metastasis at presentation (osteosarcoma). Three patients had lung metastasis develop (two with osteosarcoma, one with synovial sarcoma). One patient with malignant fibrous histiocytoma had liver and lung metastasis and did not survive. The mean time to metastasis was 18 months (range, 4–30 months).
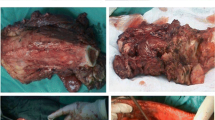
There was an overall complication rate of 53% (16 of 30). The reoperation rate was 40% (12 of 30) (Table 3). Nonunion was the most common complication (23%). Union ultimately was attained in all 30 grafts (Fig. 2). Twenty-three patients (77%) achieved successful union without additional interventions. Seven patients (23%) had nonunions develop. Nonunions were seen at the proximal osteosynthesis site in four patients, at the distal osteosynthesis site in two patients, and proximally and distally in one patient. Each ultimately progressed to union after reoperation (consisting of revision fixation and bone grafting) with an average of 1.33 subsequent operations performed.
Five patients experienced nonunion at six different sites (one patient experienced nonunion of the proximal and distal osteosynthesis sites). These radiographs show the forearm of a 17-year-old girl who underwent resection of a giant cell tumor of the distal radius with FVFG reconstruction. (A) Nonunion of the proximal osteosynthesis site 6 months postoperatively is shown. The patient underwent bone grafting and revision internal fixation. (B) Subsequent union was achieved by 13 months postoperatively. All five patients with nonunions subsequently achieved union at a mean of 9.2 months, with an average of 1.33 additional procedures performed.
Graft fracture was the second most common complication (20%) (Fig. 3). There were six fractures. Fractures occurred in two of five humeral grafts, two of nine femoral grafts, and two of eight tibial grafts. No fractures occurred in the radius or ulna. Four of six fractures were in fibulas fixed with plate osteosynthesis, one in a fibula secured by an external fixator (tibial reconstruction), and one in a fibula secured via intramedullary nail (femoral reconstruction). Three of the six fractures occurred after trauma (humerus twice, femur once). The other three fractures were stress fractures (tibia twice, femur once). One of the stress fractures occurred 10 years after reconstruction.
Fractures of the fibular graft occurred in six patients (20%). Three fractures occurred after trauma. Four of the six fractures were in patients with plate osteosynthesis of the graft. These radiographs show the arm of a 10-year-old boy who underwent FVFG reconstruction of a proximal humeral defect after resection of an osteosarcoma. (A) The incorporated graft is seen 6 months postoperatively. (B) Lateral and (C) AP views show a fracture through the grafted fibula at the most proximal screw 10 months postoperatively after a same-level fall. (D) AP and (E) lateral views show a healed fracture after 6 months of nonoperative management. (F) A radiograph shows the appearance of the humerus 3 years after the index procedure and almost 2 years after the fracture occurred.
Infection was the third most common complication (10%) (Table 3). One patient had a superficial wound infection that healed after débridement and local wound care. One patient had osteomyelitis of the proximal tibia develop 4 years after the index procedure and was treated successfully with débridement and intravenous antibiotics. One patient had osteomyelitis of the reconstructed distal femur develop 10 years after the index procedure and had conversion surgery to an above-knee amputation. One patient with osteomyelitis of the distal femur after a previous allograft reconstruction was treated with resection of the infected allograft and FVFG reconstruction and sustained union without subsequent infection.
Discussion
Skeletal reconstruction of large oncologic resection defects is challenging. Free vascularized fibular transfer offers the potential for rapid autograft incorporation in limbs compromised by adjuvant chemotherapy or radiation. There are few series describing this specific application of FVFG [6, 9, 27, 33]. Furthermore, these series report sparse data regarding local recurrence or tumor metastasis and describe variable rates of the different postoperative complications [6, 9, 27, 33]. The clinical series of patients who underwent FVFG reconstruction of oncologic skeletal defects at our institution offers the benefits of a large sample size, a large defect size, and long-term followup relative to the existing literature. Our primary goal was to describe the rates and features of six specific clinical occurrences: (1) limb survival, (2) local recurrence, (3) tumor metastasis, (4) graft nonunion, (5) graft fracture, and (6) infection. A secondary goal of this study, and the focus of this discussion, was to synthesize our outcomes in these six areas with those reported in similar series (Table 4).
Several shortcomings must be acknowledged. First, although we had a relatively large number of patients, our analysis is limited by the accrual of subjects over an extended period. Operative techniques, especially regarding osteosynthesis and periarticular reconstruction, have advanced during this time. Second, some means of functional assessment we use presently (eg, the Musculoskeletal Tumor Society 1993 rating scale) did not exist when the data for first patients were entered in the database. The resultant disparity in documentation of limb function from one decade to the next prevents functional outcome measures from being a part of this study. Third, although FVFG hypertrophy was observed in all patients in this study, changes in radiographic technique and equipment during the study period make quantitative measures of graft hypertrophy [9] unreliable. Despite these shortcomings, the study does elucidate the anticipated complications and results when FVFG is used in the treatment of large oncologic skeletal defects.
Previous series analyzing FVFG reconstruction of tumor resection defects have reported 100% rates of limb salvage (Table 4) and our data confirm those rates (97%) [6, 9, 27, 33]. Of these five series, ours had the longest mean defect length, the greatest mean patient age, and the second-longest followup. The one loss of limb in our series occurred 10 years after the index reconstruction owing to infection; perhaps with similarly long followup, other investigations would find failures of limb salvage. By comparison, the largest series of allograft reconstruction of oncologic skeletal defects (718 reconstructions followed for at least 2 years) had a 78% rate of limb salvage [21]. In the series of Rodl et al. [26] with 17 allograft reconstructions after resection of high-grade malignant bone tumors, only seven grafts survived 5 years, leading to the characterization of allograft reconstruction as “at best a temporary solution” in this scenario. Whereas the only limb loss among the 131 FVFG reconstructions (Table 4) occurred after 10 years, most limb loss after allograft reconstruction occurs within the first 3 years postoperatively [4, 21, 26].
We investigated the rate of local recurrence because it is an important component of the overall success of the primary operative procedure. However, we would not expect the type of reconstruction after any limb-sparing resection to directly influence the rate of local recurrence. Given an inverse relationship between wound infection and local recurrence after resection/reconstruction, some have speculated, because of the reported lower rates of infection with FVFG reconstruction compared with allograft reconstruction, there might be an indirect influence on local recurrence [6, 10]. We found no evidence to support this in our series or on review of the literature. Previous series have had reported local recurrence rates between 0% and 8%, which are similar to our rate (Table 4) [6, 9, 27, 33]. Similarly, Mankin et al. [21] reported a 10% local recurrence rate in 285 patients receiving allograft reconstruction after limb-sparing resection of high-grade malignancies. The rate of local recurrence in patients with nonhigh-grade malignancies in that series was not reported [21].
Although limb salvage has replaced amputation as the preferred treatment for malignant neoplasms of the extremities, the preponderance of evidence that this may be done safely without an increased risk of metastatic disease comes from series describing allograft and endoprosthetic reconstruction of resultant skeletal defects [8, 10, 11, 22, 25, 27]. Although we would expect the risk of metastatic disease to be related to the resection technique and adjuvant therapy, we believed it was important to investigate the rate of metastatic disease in our series because little attention has been given to this issue in other series investigating FVFG reconstruction. Our overall metastatic rate of 17% included one patient with osteosarcoma who had known metastasis at the time of primary tumor resection; he was disease-free 5 years postoperatively. Chen et al. [6] reported development of distant metastasis in six of 25 patients (24%). Rose et al. [27], Zaretski et al. [33], and Gebert et al. [9] did not report rates of metastatic disease, although Zaretski et al. [33] and Gebert et al. [9] mentioned this development in at least four of their combined 51 patients. The large series of allograft reconstructions of oncologic skeletal defects of Mankin et al. [21] had a 38% rate of metastatic disease. However, the poorer oncologic outcomes in their series likely have more to do with poorer adjuvant therapy options for the earlier patients rather than the choice of reconstructive technique.
Like other reconstructive options for large skeletal defects, FVFG reconstruction is associated with a high rate of complications (Table 4). We found an overall complication rate of 53%. Forty percent of patients required at least one additional operation. The lowest complication rate in a similarly sized study was 37% [33], but that study had a shorter followup. We found complications accrued with time, with some complications occurring at greater than 10 years’ followup. The highest complication rate in a similar study was 80% [27], and this series was the only one with a mean followup (5.6 years) longer than ours (4.9 years). Our most common complication was nonunion (23%), which is unique in comparison to similar studies (Table 4). Fracture was the most common complication in two series [9, 27], both of which were limited to FVFG reconstruction of the upper extremity. Infection was the most common complication in a third series [33]. Chen et al. [6] reported infection and nonunion together at the top of the list of complications in 25 patients at 12% each. Despite nonunion being common in our series, the ultimate rate of union was 100%, which is higher than in similar studies. Our high rate of union compares favorably with other large series of skeletal reconstructions using FVFG [6, 7, 19, 20, 23]. Although time to union is a difficult parameter to measure in any rigorous way, Minami et al. [23] reported a time to union (4 months) in a series of reconstructions performed for various indications. Higher rate of union and more rapid time to union are benefits of FVFG reconstruction over allograft reconstruction. Although structural allograft may be strong initially when compared with prehypertrophic FVFG, the avascular nature of allograft does not favor the biology of healing and renders these grafts ultimately more susceptible to nonunion [2, 4, 8, 12, 21, 25, 26]. Similar oncologic reconstructive studies using allograft have had reported final rates of nonunion of 34% and 17%, respectively [4, 21].
Graft fracture was only slightly less common (20%) in our series than nonunion. This complication is important because it greatly alters rehabilitation and theoretically is preventable by limiting weightbearing activity until graft hypertrophy has occurred. Diagnosis may be difficult; unlike native stress fractures, some graft fractures are identified incidentally without antecedent complaints of pain [23], as was the case in three of our patients. In similar studies, rates of fracture have been highly variable, with one series of 30 patients having no fractures [33] and another series having fractures at a rate of 40% [27]. In our series, there were traumatic fractures in two of five humeri and no fractures in the radius or ulna. This is consistent with the observations of Gebert et al. [9] who reported fractures in five of 11 humeri and no fractures of the radius or ulna. Conversely, the relatively low rate of lower extremity fracture (one of eight tibias, two of nine femurs) in our patients was different from the experience of others. Arai et al. [1], de Boer et al. [7], and Minami et al. [23] reported rates of lower extremity graft fracture between 25% and 45%. Although allograft fractures occur at a similar rate [4, 21], they have a greater association with failure of limb salvage when they do occur; in the series of Mankin et al. [21], 49% of allograft reconstructions complicated by fracture ended in failure. In another series of allografts, the rate of fracture was 27%, but 75% of limbs with a fractured allograft required either amputation or revision reconstruction using another technique [4]. In contradistinction, all six graft fractures in our series healed. This represents another potential advantage of FVFG over allograft.
Our rate of infection (10%) was comparable to those of similar series (4.8%–33%) and was favorable when compared with infection rates reported with allograft use (16%–30%) [4, 8, 15, 21]. The one failure of limb salvage in our study was attributable to graft infection. Of the 91 patients in the four studies similar to ours, there were no failures of limb salvage attributable to graft infection [6, 9, 27, 33]. This is distinctly different from allografts, which have failure rates in excess of 80% after infection [2, 4, 8, 21, 26, 29].
Although a high complication rate may be anticipated, the free vascularized fibula may be used to reconstruct large oncologic skeletal defects with a high rate of successful limb salvage and without increased rates of local recurrence or distant metastasis. Complications from nonunion, fracture, and infection presented challenges but rarely prevented limb preservation in our patients with long-term followup. Future prospective investigations should attempt to identify risk factors for complications to optimize this biologic reconstructive technique.
References
Arai K, Toh S, Tsubo K, Nishikawa S, Narita S, Miura H. Complications of vascularized fibula graft for reconstruction of long bones. Plast Reconstr Surg. 2002;109:2301–2306.
Bae DS, Waters PM, Gebhardt MC. Results of free vascularized fibula grafting for allograft nonunion after limb salvage surgery for malignant bone tumors. J Pediatr Orthop. 2006;26:809–814.
Belt PJ, Dickinson IC, Theile DR. Vascularised free fibular flap in bone resection and reconstruction. Br J Plast Surg. 2005;58:425–430.
Brigman BE, Hornicek FJ, Gebhardt MC, Mankin HJ. Allografts about the knee in young patients with high-grade sarcoma. Clin Orthop Relat Res. 2004;421:232–239.
Brown KL. Limb reconstruction with vascularized fibular grafts after bone tumor resection. Clin Orthop Relat Res. 1991;262:64–73.
Chen CM, Disa JJ, Lee HY, Mehrara BJ, Hu QY, Nathan S, Boland P, Healey J, Cordeiro PG. Reconstruction of extremity long bone defects after sarcoma resection with vascularized fibula flaps: a 10-year review. Plast Reconstr Surg. 2007;119:915–924; discussion 925–926.
de Boer HH, Wood MB, Hermans J. Reconstruction of large skeletal defects by vascularized fibular transfer: factors that influenced the outcome of union in 62 cases. Int Orthop. 1990;14:121–128.
Dick HM, Malinin TI, Mnaymneh WA. Massive allograft implantation following radical resection of high-grade tumors requiring adjuvant chemotherapy treatment. Clin Orthop Relat Res. 1985;197:88–95.
Gebert C, Hillman A, Schwappach A, Hoffmann CH, Hardes J, Kleinheinz J, Gosheger G. Free vascularized fibular grafting for reconstruction after tumor resection in the upper extremity. J Surg Oncol. 2006;94:114–127.
Gherlinzoni F, Picci P, Bacci G, Campanacci D. Limb sparing versus amputation in osteosarcoma: correlation between local control, surgical margins and tumor necrosis: Istituto Rizzoli experience. Ann Oncol. 1992;3(suppl 2):S23–S27.
Ghert M, Colterjohn N, Manfrini M. The use of free vascularized fibular grafts in skeletal reconstruction for bone tumors in children. J Am Acad Orthop Surg. 2007;15:577–587.
Griffiths HJ, Anderson JR, Thompson RC, Amundson P, Detlie T. Radiographic evaluation of the complications of long bone allografts. Skeletal Radiol. 1995;24:283–286.
Heitmann C, Erdmann D, Levin LS. Treatment of segmental defects of the humerus with an osteoseptocutaneous fibular transplant. J Bone Joint Surg Am. 2002;84:2216–2223.
Hriscu M, Mojallal A, Breton P, Bouletreau P, Carret JP. Limb salvage in proximal humerus malignant tumors: the place of free vascularized fibular graft. J Reconstr Microsurg. 2006;22:415–421.
Hsu FY, Tsai SW, Lan CW, Wang YJ. An in vivo study of a bone grafting material consisting of hydroxyapatite and reconstituted collagen. J Mater Sci Mater Med. 2005;16:341–345.
Jobe MT. Free vascularized bone transplant. In: Canale TS, ed. Campbell’s Operative Orthopaedics. St Louis, MO: CV Mosby; 1998:3226–3236.
Lee KS, Han SB, Baek JR. Free vascularized osteocutaneous fibular graft to the tibia in 51 consecutive cases. J Reconstr Microsurg. 2004;20:277–284.
Lin CH, Wei FC, Chen HC, Chuang DC. Outcome comparison in traumatic lower extremity reconstruction by using various composite vascularized bone transplantation. Plast Reconstr Surg. 1999;104:984–992.
Malizos KN, Nunley JA, Goldner RD, Urbaniak JR, Harrelson JM. Free vascularized fibula in traumatic long bone defects and in limb salvaging following tumor resection: comparative study. Microsurgery. 1993;14:368–374.
Malizos KN, Zalavras CG, Soucacos PN, Beris AE, Urbaniak JR. Free vascularized fibular grafts for reconstruction of skeletal defects. J Am Acad Orthop Surg. 2004;12:360–369.
Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res. 1996;324:86–97.
Mercuri M, Capanna R, Manfrini M, Bacci G, Picci P, Ruggieri P, Ferruzzi A, Ferraro A, Donati D, Biagini R, et al. The management of malignant bone tumors in children and adolescents. Clin Orthop Relat Res. 1991;264:156–168.
Minami A, Kasashima T, Iwasaki N, Kato H, Kaneda K. Vascularised fibular grafts: an experience of 102 patients. J Bone Joint Surg Br. 2000;82:1022–1025.
Phemister DB. Bone growth and repair. Ann Surg. 1935;102:261–285.
Quill G, Gitelis S, Morton T, Piasecki P. Complications associated with limb salvage for extremity sarcomas and their management. Clin Orthop Relat Res. 1990;260:242–250.
Rodl RW, Ozaki T, Hoffmann C, Bottner F, Lindner N, Winkelmann W. Osteoarticular allograft in surgery for high-grade malignant tumours of bone. J Bone Joint Surg Br. 2000;82:1006–1010.
Rose PS, Shin AY, Bishop AT, Moran SL, Sim FH. Vascularized free fibula transfer for oncologic reconstruction of the humerus. Clin Orthop Relat Res. 2005;438:80–84.
Simon MA, Aschliman MA, Thomas N, Mankin HJ. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1986;68:1331–1337.
Sorger JI, Hornicek FJ, Zavatta M, Menzner JP, Gebhardt MC, Tomford WW, Mankin HJ. Allograft fractures revisited. Clin Orthop Relat Res. 2001;382:66–74.
Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft: a clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55:533–544.
Upton J, Kocher MS, Wolfort FG. Reconstruction following resection of malignancies of the upper extremity. Surg Oncol Clin N Am. 1996;5:847–892.
Weiland AJ, Daniel RK, Riley LH Jr. Application of the free vascularized bone graft in the treatment of malignant or aggressive bone tumors. Johns Hopkins Med J. 1977;140:85–96.
Zaretski A, Amir A, Meller I, Leshem D, Kollender Y, Barnea Y, Bickels J, Shpitzer T, Ad-El D, Gur E. Free fibula long bone reconstruction in orthopedic oncology: a surgical algorithm for reconstructive options. Plast Reconstr Surg. 2004;113:1989–2000.
Acknowledgments
We thank Dr. John Harrelson for clinical assistance, Dr. Clyde Helms of the Duke Musculoskeletal Radiology team for radiographic analysis, and Sherry Malthouse-Dufore for assistance with data and image collection and analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and waived informed consent for participation in the study and all investigations were conducted in conformity with ethical principles of research.
This work was performed at Duke University Medical Center.
About this article
Cite this article
Eward, W.C., Kontogeorgakos, V., Levin, L.S. et al. Free Vascularized Fibular Graft Reconstruction of Large Skeletal Defects after Tumor Resection. Clin Orthop Relat Res 468, 590–598 (2010). https://doi.org/10.1007/s11999-009-1053-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-1053-x