Abstract
The accuracy and precision of any computer-aided surgical device is critical to its utility. We asked the following question: how accurate and precise are the values measured by an imageless computer navigation system as compared with those measured using postoperative CT scans? Twenty-five patients (26 hips) underwent primary THA using an imageless computer navigation system for placement of the acetabular component. Inclination and anteversion were measured in the operative coordinate system as defined by Murray. Accuracy, precision, and bias were computed, and Bland-Altman analysis was used to assess levels of agreement. The accuracy (mean ± standard deviation of the absolute difference between computer-assisted navigation and CT) was 1.8° ± 1.2° for inclination and 2.0° ± 2.0° for anteversion. Precision was 3.4° for inclination and 5.5° for anteversion. Bias was 0.52° for inclination and 0.35° for anteversion. Limits of agreement were 4.26° for inclination and 5.58° for anteversion. An imageless computer navigation system can precisely determine acetabular cup position.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Optimal acetabular cup position is an important determinant of early and long-term success of a THA. Poor cup position has been associated with impingement [7], dislocation [2, 9, 17, 22, 27, 28, 34], accelerated polyethylene wear [5, 22], pelvic osteolysis [25, 41], component loosening [13], and component migration [22]. Methods to determine acetabular component position intraoperatively historically have consisted of freehand techniques and the use of mechanical guides. In the past decade, the accuracy of these methods has come into question. Freehand [23, 36] and mechanically guided [6, 12, 16, 31] techniques have resulted in inaccurate cup inclination and anteversion, with numerous cups placed outside the predefined safe zone as described by Lewinnek et al. [24]. Cup position using these techniques, even in the hands of experienced surgeons, may result in considerable positional outliers.
The inability to obtain and maintain a stable pelvic position, especially in the lateral decubitus position, has been reported by numerous authors [2, 8, 12, 30]. This may precipitate misjudgment in estimation of pelvic orientation relative to mechanical guides and surgical instruments. In addition, anatomic landmarks can be difficult to observe in cases of posttraumatic deformity or in severe dysplasia, more so now in an age of decreasing incision length [1]. Finally, cup position can change on insertion of the final component into the pelvis secondary to pelvic motion and even secondary to impaction of the cup into the acetabulum.
Computer-assisted navigation systems (CASs) with real-time adjustments for pelvic positional changes have emerged in an effort to more accurately position the acetabular component. Imageless CASs use digitally registered pelvic landmarks referenced to an optical array fixed to the pelvis to establish the anatomic anterior pelvic plane. The registered points include both anterior superior iliac spines (ASISs) and either the bilateral pubic tubercles or the pubic symphysis. With these points defined, real-time component inclination and anteversion can be determined by tracking the array with an optical camera or electromagnetic tracking system. Studies have suggested this technique may be highly efficacious in obtaining optimal acetabular cup position and reducing positional outliers [19–21, 31], although pelvic landmarks can become obscured by overlying soft tissue, which makes direct referencing, even with a pointed probe, difficult [37, 41]. A considerable quantity of tissue overlying the ASISs and/or pubic tubercles in an obese patient may introduce measurement error. Given this potential error, can the surgeon trust the values acquired by the CAS and, if so, to what degree? For the surgeon to be confident in the values of inclination and anteversion acquired by the CAS, the accuracy and precision of these values should be evaluated.
We therefore asked the following question: how accurate and precise are the values of acetabular cup inclination and anteversion measured by an imageless CAS as compared with those measured using postoperative CT scans?
Materials and Methods
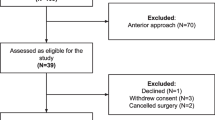
We prospectively followed 25 patients who underwent primary THA between February 2006 and December 2006 using an imageless CAS (Ci™ System; Orthopaedics, Inc, Warsaw, IN, and BrainLAB AG, Feldkirchen, Germany) to place the acetabular component. Sixty-five patients underwent primary THA during the study period. Use of the CAS was not offered to everyone during the study period. Reasons for exclusion included severe osteoporosis, computer unavailability, and patient choice. Ten patients (16%) were excluded owing to the obesity pattern. Patients were not excluded on the basis of body mass index (BMI), but they were excluded if the surgeon thought the pattern of obesity might make placement of the navigation arrays and palpation of the ASISs or pubic tubercles difficult. CAS was used in 36 of the 65 patients. We also excluded the first five patients who had CAS surgery to avoid possible errors resulting from a learning curve. This decision was made a priori after all the surgeries were performed but before the CT scans were obtained. The remaining 31 patients were contacted by telephone and asked to participate. Twenty-five patients agreed to enroll in the study and had a pelvic CT scan. One patient had bilateral arthroplasties, so 15 right hips and 11 left hips were included in the analysis. The sample consisted of 10 men and 15 women with a mean age of 67 years (range, 37–78 years). The mean BMI was 26 kg/m2 (range, 19–34 kg/m2). Twenty-three patients had a diagnosis of primary osteoarthritis, the one patient with bilateral THAs had a diagnosis of osteonecrosis in both hips, and one patient had prior hip resurfacing hemiarthroplasty. Five of the 25 patients were classified as obese as measured by a BMI greater than 30 kg/m2 (range, 31.3–34.4 kg/m2). Ten were classified as overweight (BMI, 25–30 kg/m2), and 10 had a BMI less than 25 kg/m2. We had prior Institutional Review Board approval. All patients gave informed consent to the use of CAS and acquisition of the postoperative CT scan.
The senior author (WLB) performed all surgeries. With the patient in the supine position, using sterile technique two Steinmann pins were placed into the iliac crest approximately two fingerbreadths proximal to the ASIS on the operative side (Fig. 1). Points corresponding to the bilateral ASISs and bilateral pubic tubercles were referenced superficially to the pelvic pins using a blunt probe equipped with optical sensing spheres. Care was taken to palpate the midpoints of the bony landmarks. Any panniculus was elevated above the ASISs. The prepubic fat pad was elevated from below using one finger to palpate the symphysis pubis. The pubic tubercles were registered on either side of the finger. The patient then was moved to the lateral decubitus position, with care taken to preserve sterility of the pins fixed to the pelvis, followed by standard hip and leg preparation and draping. A posterolateral approach was used in all cases. Incision length averaged 11 cm, with a range of 10 cm to 14 cm. After preparation of the acetabulum, the acetabular implant (Pinnacle®, DePuy Orthopaedics, Inc, Warsaw, IN) was inserted with an offset inserter equipped with an optical array (Fig. 2). It is the senior author’s practice to use an initial target position of the acetabular component of 40° inclination and 30° anteversion as measured in the operative coordinate system as defined by Murray [30]. This corresponds to 44° radiographic inclination and 22.5° radiographic anteversion in the radiographic coordinate system [30] (Table 1).
With the patient in the supine position, two Steinmann pins are placed using a sterile technique into the iliac crest approximately two fingerbreadths proximal to the ASIS on the operative side. This photograph shows placement of the first pin. Points corresponding to bilateral ASISs and bilateral pubic tubercles are referenced superficially to the pelvic pins using a blunt probe equipped with optical sensing spheres. Great care is taken to palpate the midpoints of the bony landmarks.
Final inclination and anteversion of the implant were recorded by the CAS after final impaction and positioning of the acetabular shell. The femur then was prepared and trial femoral components inserted. The hip was taken through a range of motion and stability of the hip throughout the range of motion was tested. It is the senior author’s practice to use the coplanar test as described by Ranawat and Maynard [35] to determine appropriate acetabular implant position [25]. In brief, the senior author’s interpretation of Ranawat’s sign is performed as follows: the hip is extended to neutral and adducted to the midline. The hip then is rotated internally 45° with the knee flexed 90° and used as a protractor to judge the degree of rotation. The plane of the face of the cup is compared with the plane of the equator of the head. In this study, if the plane of the equator was not parallel to the face of the liner, then the acetabular cup was repositioned appropriately and new values of inclination and anteversion were recorded by the CAS if repositioning occurred. The hip capsule then was repaired, followed by layered closure of the soft tissues and skin. No pin tract infections or dislocations occurred.
Inclination and anteversion are relative terms that must be defined precisely with respect to the planes from which they are referenced. Murray [30] described the three coordinate systems used to define these terms: operative, anatomic, and radiographic. The imageless CAS used in this study determines values of inclination and anteversion in the operative coordinate system. To maintain consistency, therefore, the CT scans also were analyzed using the operative coordinate system. The terms “operative inclination” and “operative anteversion” used in this study refer to these values as measured in the operative coordinate system.
All patients were scanned feet first in the supine position with the feet taped together to prevent motion. A small pad was used under the knees for patients who were unable to tolerate a completely supine position owing to lower back discomfort or inability to completely straighten one or both legs. Patients were positioned on the table with the patient’s long axis parallel and centered to the long axis of the CT table. Emphasis also was placed on a level pelvis (based on palpation of the ASIS). Patients were instructed to lie perfectly still with shallow breathing for the duration of the scan (5–10 minutes on the scan table).
All scans were obtained at a minimum of 6 weeks after the index surgery (mean, 24 weeks; range, 6–43 weeks). All patients were scanned on the same General Electric LightSpeed® 16-detector scanner (GE Medical Systems, Milwaukee, WI) with the following technical parameters: 1-second tube rotation time, 2.5-mm slice thickness, 2.5-mm interslice interval, 9.38-mm table increment per second, scanner pitch 0.938:1, no gantry tilt, 140-kVp tube potential, 150-mA tube current 150, and large-scan field of view (FOV). Display FOV varied with patient size in an effort to use the smallest display FOV to include the patient’s entire bony pelvic anatomy. Using these parameters, the resulting images, two-dimensional and three-dimensional (3D) reconstructions, were judged subjectively to be free of interfering artifacts. Patients were scanned from approximately 2 cm superior to the ASIS points to approximately 3 cm inferior to the inferior margin of the pubis symphysis.
All CT scan raw data in DICOM (Digital Imaging and Communications in Medicine) format were entered into a commercially available 3D rendering software package (Mimics®; Materialise, Ann Arbor, MI). Independent segmentation was performed on the pelvic bone and on the metal acetabular components. The acetabular component operative inclination (Fig. 1) and operative anteversion (Fig. 2) were determined by an observer (AAJ) blinded to the preoperative plan and intraoperative data.
A result is valid if it is accurate and precise. Accuracy (agreement between the two methods) was defined as the absolute difference between the surgeon’s CT reading and the CAS reading. Precision (repeatability) was defined as the 95% limit on the difference between the CAS and CT values. Bias was computed as the difference between the means of inclination and anteversion values obtained by CAS and CT.
Scatterplots and Pearson’s correlation coefficients were used to evaluate the association of the absolute difference between CAS and CT values with BMI.
Because a high correlation does not necessarily imply there is good agreement between two methods that each have some error in their measure, we also used Bland-Altman 2-standard deviation (SD) limit of agreement analysis [3] to compare the values obtained by CAS and CT. A Bland-Altman limit of agreement analysis visually displays the discrepancy between two measurements across the means. Limits of agreement, defined as 2 standard deviations around the mean difference, were computed [3]. We plotted the mean of the individual CT scan values (assumed as the gold standard) [8, 14, 15, 19, 26, 38, 40] and CAS values (new device) against their difference. The mean difference and 1-SD and 2-SD limit lines were constructed around the difference. The percentage of pairs that fell within these values was computed [4].
Results
The accuracy (mean of the absolute difference between CAS and CT) was 1.8° ± 1.2° for inclination and 2.0° ± 2.0° for anteversion. Precision was 3.4° for inclination and 5.5° for anteversion. Bias was 0.52° for inclination and 0.35° for anteversion. Limits of agreement were 4.26° for inclination and 5.58° for anteversion [3] (Table 2). Mean CT values for inclination and anteversion were 38.8° ± 3.5° and 32.2° ± 6.8°, respectively. Mean CAS values were 39.4° ± 4.0° for inclination and 32.6° ± 7.0° for anteversion. Correlations between CAS and CT values were r = 0.850 for inclination and r = 0.919 for anteversion (Fig. 3). The Bland-Altman plots (Fig. 4) show 96% of inclination values and 92% of anteversion values were within 2 SDs of the mean. We observed no correlation between the absolute mean difference of the CAS and CT values and BMI for inclination (p = 0.30) or anteversion (p = 0.98) (Fig. 5).
Discussion
Trust in the accuracy and precision of any tool used in surgery is critical to its clinical utility. This is perhaps even more the case for costly computer-aided devices such as imageless CASs where the surgeon is relying on the data provided by the system to achieve his/her goal of component orientation. We asked the following question: how accurate and precise are the values for acetabular cup inclination and anteversion measured by an imageless CAS as compared with those measured using postoperative CT scans?
We first emphasize the data reported here are only directly applicable to the specific imageless CAS used and for the specific technique used in palpating and registering the bony landmarks in a select patient population without substantial truncal obesity. Second, this study is not a comparison of manual and CAS techniques. There are other published studies addressing the issue of safe zones and outliers [10, 15, 18–20, 24, 32, 39]. Instead, regardless of the target orientation chosen, we focused on the accuracy and precision of the values obtained. Third, we did not address the more difficult question of what the specific target orientation of the acetabular component should be. There is substantial variation in patients’ pelvic orientation during activities of daily living [7]. Determining the optimal individual target position for each patient may not be feasible, but future research should consider this problem. Finally, there is also concern that there is no absolute gold standard against which we can compare the values obtained by the CAS. We chose postoperative CT scans for comparison, but there may be errors in obtaining the values of inclination and anteversion from these scans. CT scan measurement as a method of determining postoperative cup position represents the most contemporary measurement technique. With the ability to precisely reference anatomic landmarks, CT scanning has emerged as the gold standard in determination of postoperative acetabular cup position [8, 14, 15, 19, 26, 38, 40]. CT protocols, using artifact suppression software, effectively reduce image distortion and acquire precise data points. We created 3D models of the pelvis and points of registration precisely defined. The position of the acetabular cup was referenced to the same planes, which were generated by the same points used during the operative procedure with the CAS. Thus, a true comparison of the inclination and anteversion given by the CAS and a CT scan could be made.
Accurate determination of the computer-generated planes is dependent on accurate points of registration. Wolf et al. [41], using a computerized kinematic model, reported substantial error in estimation of inclination and anteversion if points of reference to define the anterior pelvic plan were not accurate. Given this association, registration of the ASISs and pubic tubercles must be as accurate as possible. Spencer et al. [37], in a cadaver model, reported interobserver measurement variability for inclination and anteversion using an imageless CAS dependent on superficial landmark registration. The authors of that study imply overlying soft tissue obscures accurate registration of bony landmarks when obtained superficially. They speculate, in an obese patient with a large quantity of soft tissue, registration of landmarks may be even more inaccurate. Parratte and Argenson [32] reported an increase in acetabular cup position measurement error with an imageless CAS when the patients had a BMI greater than 27 kg/m2 compared with patients with a BMI less than 27 kg/m2. We found no correlation between BMI and accuracy in this study; however, the mean BMI in our patients was less than 27 kg/m2 (26.2 kg/m2). Less than 20% of our study cohort was obese, but the mean BMI of 26 kg/m2 is in line with BMI reported in hip arthroplasty studies. In a study of 800 primary THAs on 759 patients, the mean BMI preoperatively was 27.8 kg/m2 [29]. Patel and Albrizio reported a mean BMI of 28.3 kg/m2 in 550 patients undergoing primary THA [33].
Our data compare favorably with results of others investigating the accuracy of CASs for acetabular cup placement (Table 3). Ybinger et al., in a recently published study using CT validation and involving four centers, reported an average difference of 3.5° ± 4.4° for inclination and 6.5° ± 7.3° for anteversion [42]. They also reported inclination differences correlated with the thickness of the soft tissue overlying the ASISs, whereas the differences in anteversion showed a correlation with the thickness of the soft tissue overlying the pubic tubercles. These soft tissue thicknesses were measured on axial CT images. Dorr et al., in another recent study [8], reported a mean inclination difference of 4.4° and a mean anteversion difference of 4.1°. The mean BMI in their patients was 26.8 kg/m2 compared with the mean BMI of 26.2 kg/m2 in our patients. We found a smaller difference between CAS values and those measured on a postoperative CT scan for inclination and anteversion. This may be attributable in part to our practice of excluding patients with truncal obesity patterns from our study. Dorr et al. [8] used a method for registration of bony landmarks that punctured the skin for direct palpation of the bone with the probe. Despite this more direct method of registration, the precision and bias were less accurate than the values we obtained. The reason for our better accuracy most likely is the result of one or more of the following: differences in surgical technique, use of a different CAS, and/or use of a different method for CT analysis.
We believe an imageless CAS can provide accurate and precise real-time determination of the acetabular cup position in a patient population that does not have severe osteoporosis or substantial truncal obesity. The accuracy and precision values we obtained are among the highest reported to date for acetabular component position using an imageless CAS. Speculation remains regarding whether this level of accuracy can be achieved in patients in whom bony anatomic landmarks are difficult to palpate and identify. In such cases, the method of puncturing the skin for direct palpation, as reported by Dorr et al. [8], may provide sufficient accuracy.
References
Argenson JN, Ryembault E, Flecher X, Brassart N, Parratte S, Aubaniac JM. Three-dimensional anatomy of the hip in osteoarthritis after developmental dysplasia. J Bone Joint Surg Br. 2005;87:1192–1196.
Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001;50:265–274.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310.
Dallal GE. Comparing two measurement devices. 2007. Available at: http://www.tufts.edu/~gdallal/compare.htm. Accessed May 11, 2009.
Del Schutte H Jr, Lipman AJ, Bannar SM, Livermore JT, Ilstrup D, Morrey BF. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13:621–626.
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364.
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321.
Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99.
Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop Relat Res. 1980;151:169–178.
Fukunishi S, Fukui T, Imamura F, Nishio S. Assessment of accuracy of acetabular cup orientation in CT-free navigated total hip arthroplasty. Orthopedics. 2008;31:pii: orthosupersite.com/view.asp?rID = 31515.
Grutzner PA, Zheng G, Langlotz U, von Recum J, Nolte LP, Wentzensen A, Widmer KH, Wendl K. C-arm based navigation in total hip arthroplasty: background and clinical experience. Injury. 2004;35(suppl 1):S-A90–A95.
Hassan DM, Johnston GH, Dust WN, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. J Arthroplasty. 1998;13:80–84.
Hedlundh U, Ahnfelt L, Hybbinette CH, Weckstrom J, Fredin H. Surgical experience related to dislocations after total hip arthroplasty. J Bone Joint Surg Br. 1996;78:206–209.
Herrlin K, Pettersson H, Selvik G. Comparison of two- and three-dimensional methods for assessment of orientation of the total hip prosthesis. Acta Radiol. 1988;29:357–361.
Jenny JY, Boeri C, Dosch JC, Uscatu M, Ciobanu E. Navigated non-image-based positioning of the acetabulum during total hip replacement. Int Orthop. 2009;33:83–87.
Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179.
Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–208.
Kalteis T, Beckmann J, Herold T, Zysk S, Bathis H, Perlick L, Grifka J. [Accuracy of an image-free cup navigation system: an anatomical study] [in German]. Biomed Tech (Berl). 2004;49:257–262.
Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88:163–167.
Kalteis T, Handel M, Herold T, Perlick L, Baethis H, Grifka J. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29:272–276.
Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300.
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534.
Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg. 2002;7:99–106.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220.
Lucas DH, Scott RD. The Ranawat sign: a specific maneuver to assess component positioning in total hip arthroplasty. J Orthop Tech. 1994;2:59–62.
Marx A, Pfortner J, von Knoch M, Wiese M, Loer F, Saxler G. [Influence of the x-ray technique on evaluation of cup anteversion after total hip arthroplasty][in German]. Z Orthop Ihre Grenzgeb. 2006;144:394–399.
McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res. 1990;261:159–170.
Minoda Y, Kadowaki T, Kim M. Acetabular component orientation in 834 total hip arthroplasties using a manual technique. Clin Orthop Relat Res. 2006;445:186–191.
Moran M, Walmsley P, Gray A, Brenkel IJ. Does body mass index affect the early outcome of primary total hip arthroplasty? J Arthroplasty. 2005;20:866–869.
Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232.
Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163.
Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty: a prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499.
Patel AD, Albrizio M. Relationship of body mass index to early complications in hip replacement surgery: study performed at Hinchingbrooke Hospital, Orthopaedic Directorate, Huntingdon, Cambridgeshire. Int Orthop. 2007;31:439–443.
Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210.
Ranawat C, Maynard M. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25.
Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grutzner PA, Steffen R, von Knoch M, Holland-Letz T, Bernsmann K. The accuracy of free-hand cup positioning: a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop. 2004;28:198–201.
Spencer JM, Day RE, Sloan KE, Beaver RJ. Computer navigation of the acetabular component: a cadaver reliability study. J Bone Joint Surg Br. 2006;88:972–975.
Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res. 2005;436:144–150.
Widmer KH, Grutzner PA. Joint replacement-total hip replacement with CT-based navigation. Injury. 2004;35(suppl 1):S-A84–A89.
Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701.
Wolf A, Digioia AM 3rd, Mor AB, Jaramaz B. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res. 2005;437:132–137.
Ybinger T, Kumpan W, Hoffart HE, Muschalik B, Bullmann W, Zweymuller K. Accuracy of navigation-assisted acetabular component positioning studied by computed tomography measurements: methods and results. J Arthroplasty. 2007;22:812–817.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (WLB) have received funding from DePuy Orthopaedics, Inc, Warsaw, IN.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Sutter General Hospital.
About this article
Cite this article
Ryan, J.A., Jamali, A.A. & Bargar, W.L. Accuracy of Computer Navigation for Acetabular Component Placement in THA. Clin Orthop Relat Res 468, 169–177 (2010). https://doi.org/10.1007/s11999-009-1003-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-1003-7