Abstract
The functional outcomes of periacetabular osteotomy (PAO) and factors predicting outcome in the older patient with acetabular dysplasia are not well understood. We therefore retrospectively determined the functional outcome of 70 patients (87 hips) over age 40 treated with PAO in three institutions; we also determined whether preoperative factors, particularly the presence of osteoarthritis, influenced the survival of the hip or time to total hip arthroplasty after PAO. The average age at surgery was 43.6 years. The minimum followup was 2 years (mean, 4.9 years; range, 2–13 years). Twenty-one hips (24%) had undergone total hip arthroplasty (THA), at a mean of 5.2 years after PAO (range, 1.9–7.6 years). Surviving hips had a mean improvement in Harris hip score from 60.7 to 90.3 and in total WOMAC pain score from 8.7 to 3. We observed no differences in preoperative or postoperative radiographic measurements or preoperative clinical function scores (HHS, WOMAC) in hips surviving and hips having THA. The risk of THA at 5 years after PAO was 12% in hips with preoperative Tönnis Grade 0 or 1 and 27% for Tönnis Grade 2. Our preliminary study suggests that PAO will give satisfactory functional and pain scores in patients over age 40 having dysplastic hips with mild or no arthrosis.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Bernese periacetabular osteotomy (PAO) is an effective joint-preserving procedure for symptomatic congruous acetabular dysplasia. Multiple studies report on the functional outcomes, predictors of outcomes, and survival rates for PAO and other acetabular reorientation osteotomies performed for symptomatic acetabular dysplasia [2, 5, 10, 13, 16, 19, 22, 23]. The Bernese periacetabular osteotomy has reportedly led to good to excellent results for approximately 75% to 93% of patients [15, 16, 19, 23]. The majority of procedures are performed in adolescents and young adults, and the average age at surgery in these studies ranges from 21 to 32 years, with followup times from 2 to 11 years [17]. The study with the longest followup, by the originators of the procedure, reported 60% of hips survived with an average followup of 20.4 years [20]. The average age at surgery was 29 years [20]. These authors identified several parameters associated with poor outcomes [20], which included older age at surgery and higher preoperative osteoarthritis grade. Other studies also identified older age and higher grade of preoperative arthritis as predictors of PAO failure [9, 22]. Yasunaga et al. reported the results of 24 patients with acetabular dysplasia over the age of 46 treated with rotational acetabular osteotomy (RAO), noting 70% survivorship of hips at 10 years. They suggested RAO minimized the progression of osteoarthritis in this patient population [26].
Only one study in the literature has evaluated patients over the age of 40 treated with PAO [4]. This study compared a group of 28 patients to a similarly aged group of patients treated with total hip arthroplasty (THA). Although the quality-of-life outcomes were higher in the THA group the authors reported a substantial number of patients with PAO had good and very good outcomes [4]. Another study, using a constructed model based on the current literature, evaluated cost-effectiveness of PAO versus THA for this patient population, concluding that PAO was preferable for Tönnis grade 0, 1 and 2 patients but not Grade 3 [17].
With only these two limited studies in the literature, we chose to evaluate our patients older than 40 years of age with symptomatic acetabular dysplasia treated with PAO. We asked the following questions: (1) what is the rate of THA and expected survivorship of PAO in this patient population? (2) What is the radiological and functional improvement seen in this group of patients? (3) How do those patients whose hips survived differ from those patients whose hips went on to THA in terms of radiographic parameters and preoperative outcome scores? and (4) How does the amount of preoperative osteoarthritis influence the survivorship of PAO in this patient population?
Methods and Materials
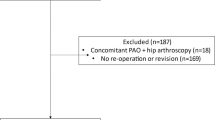
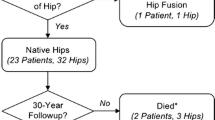
In a collaborative effort, the Academic Network for Conservational Hip Outcomes Research (ANCHOR) group, consisting of three departments of orthopaedic surgery with large PAO experience (Children’s Hospital Boston, Mayo Clinic, and Washington University-St. Louis), sought to define the outcomes of PAO in a homogeneous group of patients, all with symptomatic developmental acetabular dysplasia over the age of 40 years at time of surgery. Each center performs a high volume of PAOs. WUSTL performed 166 and Mayo performed 263 from 1996 to 2005, while CHB performed 742 from 1991 to 2006. The cases included in this study consisted of 6% of WUSTL patients, 12% Mayo patients, and 7% of CHB patients. Patients were excluded for acetabular dysplasia secondary to Down’s syndrome, inflammatory arthritis, Legg-Calve-Perthes disease, neuromuscular diagnoses such Charcot-Marie-Tooth or cerebral palsy, or isolated acetabular retroversion. With these exclusions we had 73 patients (90 affected hips). Of the 73 patients, 17 patients had bilateral PAOs and were over the age of 40 for both procedures. One of the bilateral patients had her first PAO at age 39 years 9 months and this hip was excluded from the analysis. Two patients died more than 2 years after surgery because of events unrelated to the surgery (one motor vehicle fatality; one myocardial infarction), leaving 70 patients (87 hips) for evaluation. The average age of the patients at the time of surgery was 43.6 years (range, 40–51 years). Minimum followup was 2 years (mean, 4.9 years; range, 2–13 years). We obtained IRB approval from each of the three participating institutions.
The abductor-sparing direct anterior approach was used by all three centers [11, 12]. All three institutions used intraoperative fluoroscopy. At CHB, a more oblique or bikini-line skin incision was routine. At the other two institutions, a longitudinal Smith-Petersen incision was routine.
Each institution evaluated their own patients and evaluated their own radiographs. Two institutions (Mayo and WUSTL) evaluated patients with the Harris hip score (HHS), and one (CHB) used the WOMAC scoring system to evaluate patients’ functional outcome. Both of these are validated outcomes scores to assess function. Each score has been used in prior studies to assess the functional outcome of patients treated with a PAO for dysplasia [1, 7, 15, 23, 24]. Forty-seven hips were evaluated with the WOMAC and 42 were evaluated with the HHS. Patients were evaluated preoperatively as well as on subsequent followup visits. The most recent postoperative score for the respective outcome score was used for analysis. CHB began using the WOMAC in 2000, and not all patients had preoperative WOMAC scores recorded. Therefore, 22 hips of the 45 hips from CHB were excluded from preoperative WOMAC score analysis. HHS preoperative and postoperative scores were available for all 40 hips evaluated at the other two institutions. Information was obtained either in the office or over the phone through the help of a nonclinical research assistant.
Radiographic analysis was performed on anteroposterior (AP) pelvis and faux profil view preoperatively and postoperatively [8], evaluating measures of severity of dysplasia radiographic signs of osteoarthritis. Each institution had one individual who was not the operating surgeon and was blinded to the patient outcomes read the radiographs. Preoperative analysis was performed to define the group as being dysplastic and postoperative radiographs were used to evaluate correction and signs of osteoarthritis. Analysis of the AP pelvis radiograph consisted of determining the Tönnis grade (TG) [21] to evaluate osteoarthrosis; and measuring both the lateral center edge (LCEA) of Wiberg [25] (normal, > 25°; possible dysplasia, 20°–25°; definite dysplasia, < 20°) and the Tönnis roof angle (TA) (normal, 0–10°; dysplasia, > 10°) to determine the severity of dysplasia. The faux profil view was used to evaluate anterior acetabular coverage by measuring the anterior center-edge angle (ACEA) (normal, > 20°). The Tönnis grade (TG) was used to evaluate radiographically the degree of osteoarthritis present preoperatively. Five categories are used to define the degree of osteoarthritis. Grade 0 is a normal hip with no signs of osteoarthritis. Grade 1 is defined as subchondral sclerosis with minimal joint space and minimal osteophyte formation. Grade 2 is defined as subchondral cyst formation and moderate joint space narrowing. Grade 3 has severe but localized joint space narrowing, and Grade 4 is defined as a hip with total joint involvement and severe cartilage loss.
Clinical and radiological assessments (except Tönnis grade) were summarized using means and standard deviations. Although some variables were slightly skewed, conclusions based on means and medians (and on parametric and nonparametric tests) were comparable. Therefore, in this text, we will present only results based on means for simplicity. The preoperative and postoperative functional scores from CHB (WOMAC) were summarized separately from the scores measured by WUSTL and Mayo (HHS). Comparisons between preoperative and postoperative scores WOMAC and HHS were performed through paired t-tests. Comparisons of preoperative WOMAC, HHS, and preoperative radiological variables were assessed through unpaired t-tests. Comparison of the proportion of hips in the three alternative preoperative Tönnis grade categories between surviving and THA hips was performed using Pearson chi square tests. Time to THA was estimated using Kaplan-Meier methods. Since preoperative Tönnis grade is often cited as a predictor of outcome for periacetabular osteotomy, a comparison of time to THA across Tönnis grade groups was performed through a log-rank test. Increase in the risk of THA with Tönnis grade was based on a hazard ratio and 95% confidence interval obtained in a Cox proportional hazards analysis. All analyses were performed in S-plus 8.0 (Insightful Corporation, Seattle, WA).
Results
Of the 87 hips, 66 (76%) were preserved at last followup. The other 21 hips (24%) subsequently had a THA with the average time from PAO to THA 5.2 years (range, 1.9–7.6 years). The mean time to THA for these 87 patients was 8.4 years (95% CI = 7.4–9.4) (Fig. 1). Thirty-one of the surviving hips were followed for at least 5 years and of those, four were followed for at least 10 years.
The patients followed with the HHS (n = 42) had an average preoperative score of 60.2 ± 11.4, which improved to 85.4 ± 17.1 at last followup. For the hips followed with the WOMAC, the average preoperative pain score (n = 23) was 8.9 ± 4.9 and the average postoperative WOMAC score for pain improved to 3.9 ± 4.9. All treated hips were dysplastic preoperatively (Table 1) and radiographic measures were corrected to normal ranges by PAO.
The mean age at the time of surgery was similar (p = 0.486) in the group with a surviving hip and the group converted to THA (44.2 years ± 3.1 for surviving group; 43.8 ± 2.6 for THA group). Preoperative scores of the surviving hips were slightly better than those of the THA hips scored with the HHS (60.7 ± 11.6 versus 57.6 ± 10.7) but were slightly worse for the hips scored with WOMAC (8.7 ± 5.6 versus 8.2 ± 2.6) (Table 2). For the surviving hips, clinical scores were considerably improved postoperatively; HHS improved from 60.7 ± 11.6 to 90.3 ± 12.2 and WOMAC improved from 8.7 ± 5.6 to 3.0 ± 4.4. We found no difference between the surviving and the THA hips in any of the following radiographic measures: average LCEA, TA, and ACEA, either preoperatively or postoperatively (Table 3).
The average preoperative Tönnis grade was similar (p = 0.10) for the surviving hips and those converted to THA. Of the Tönnis Grade 2 hips (n = 16) 50% went on to THR, which represented 39% of the hips that went on to THA. In the surviving hips only 14% had a preoperative Tönnis Grade 2. As the radiographic severity of osteoarthritis increased preoperatively the time to failure tended to decrease (p = 0.07) (Fig. 2).
Three graphs represent the distribution of patients by preoperative Tönnis grade. (A) The grade for all patients is shown. (B) The grade for each survival group is illustrated. (C) The grade for the THA group is shown. The number of patients for each group is also represented as percentage for each distribution.
The percentage of hips going on to THA increased as the amount of preoperative osteoarthrosis increased; 10% with Tönnis Grade 0, 25% with Tönnis Grade 1, 50% with Tönnis Grade 2. Based on the Kaplan-Meier estimates and how preoperative osteoarthritis affected survivorship, the risk of THA by 5 years post-PAO was 13.1% for preoperative Tönnis Grade 0, 10.9% for Tönnis Grade 1, and 27.3% for Tönnis Grade 2. Patients with preoperative Tönnis Grade of 2 had a risk of THA 2.2 times higher than patients with preoperative Tönnis Grade of 0 or 1 (hazard ratio = 2.19; 95% CI = 1.01, 4.77) (Fig. 3).
There were few complications. One patient had global nonunion associated with GI sepsis 1 month after surgery, salvaged successfully with bone grafting. There was one sciatic sensory neuropraxia, which partially resolved. Neither of these patients had THA. No other complications were noted.
Discussion
The outcomes of PAO in patients over the age of 40 years have not been looked at extensively. We wished to define the outcome for this patient group in order to compare it to the outcomes in the literature for patients of all ages treated with PAO. Additionally, we wanted to examine the differences between the survival group and the THA group and then assess preoperative arthritis as a predictor of survival in this patient population.
This multicenter study of 87 hips treated after the age of 40 with PAO for symptomatic dysplasia has several limitations. First, we had no control group, though some comparison can be made to prior studies. Secondly, the CHB group lacked preoperative scores for the 22 hips treated prior to 2000, though the other preoperative and postoperative demographics and postoperative results were no different from the hips treated at CHB treated after 2000. Since the primary goal of the study was to look at outcomes, we believe inclusion of these 22 hips is reasonable as similar improvement was seen in the patients with HHS. Second, we lacked direct imaging of articular cartilage. The prospective preoperative use of the dGEMRIC technique may allow improved patient selection though more precise evaluation of the health of the articular cartilage [3, 6]. Third, we used only the most recent clinical outcome score to assess the patients’ clinical function. Without the interval clinical data and only evaluating the current functional score, it is unclear how well patients responded initially to surgery. Fourth, the lack of interval radiographic data prevented the evaluation of how well the joint space was maintained over time. However, this radiographic information would not have influenced our conclusion regarding the factors associated with clinical outcome. Fifth, rapidity of recovery from surgery is another important factor to consider for patients deciding between a PAO and THA. We did not evaluate the average recovery time for this group, nor did we have a control group of THA to compare. That said, it is our impression that this patient group has a more prolonged recovery than younger PAO patients and those treated with THA. Finally, we did not critically assess retroversion as a preoperative or postoperative factor. We recognize postoperative retroversion may have contributed to the failure of some hips. Because both sitting and supine films were used for the AP pelvis radiograph and an ovary shield was often used preventing some films from being assessed for pelvic tilt and rotation, not every film could be evaluated reliably for acetabular version.
Periacetabular osteotomy has been effective in treating younger patients with mild or no arthrosis [20, 22], and RAO has been similarly effective in both younger and older patients with no, mild, or even moderate arthrosis [26]. In this study of patients over 40 treated with PAO there was a mean followup time of approximately 5 years and 76% of hips were still preserved with PAO at latest followup. The mean survivorship for all 87 hips was 8.4 years, with 66 patients overall maintaining their native hip joint with an average followup of 5 years. Compared to younger patients, this group did have higher rate of THA and confirms the findings of Steppacher, that relatively advanced age is a risk factor for conversion to THA after PAO [20]. In a meta-regression analysis of 23 studies by Sambandam, the average age of patients was 30 years (range, 22.7–37.6 years) and the rate of THA ranged from 0% to 17%, with followup times ranging from 2 years to 12 years [17]. In our study, with 24% of patients going on to THA at approximately 5.2 years, the rate of THA is higher than what is reported for younger patients. Despite a somewhat higher rate of conversion to THA in our study compared to younger patients, those who survived had good to excellent functional scores.
The improvement in outcomes scores in the surviving hips in the present study is a similar improvement in function as reported by other studies [4, 10, 22, 24]. The only difference observed between the survival group and the THA group was the large number of patients in the THA with a higher Tönnis grade preoperatively.
Although our study confirms relative advanced age as a risk factor for failure of PAO, it also suggests the presence of preoperative osteoarthritis contributes to early failure. Although we cannot definitively conclude that preoperative arthritis is more important than age, this is our impression. Many studies have indicated the presence of preoperative osteoarthritis is a risk factor for failure of PAO, and our findings also support this fact [20]. In treating the symptomatic patient with dysplastic hip over the age of 40, deciding between THA and a joint-preserving PAO can be difficult. While this patient population can be very active, PAO provides substantial improvement in symptoms globally and with activities [24]. We found the presence of Tönnis Grade 2 changes preoperatively increased the risk of conversion to THA by twofold compared to Grade 0 or 1. In the study of Sharifi et al., the authors determined that in Tönnis Grade 0, Grade 1, and Grade 2 OA, PAO was more cost-effective than THA [18]. Garbuz et al. compared PAO and THA in patients over 40 years old in a cross-sectional cohort comparison study [4]. They considered only patients treated with PAO with preoperative OA Grade 0 or 1. With mean followup of about 4 years, they noted good/very good functional and pain results in 85% of patients with THA, compared to 53% of the patients with PAO having good/very good functional scores and 62% of PAO patients with good/very good pain scores. They noted most PAO patients did have good/very good outcomes, but concluded PAO should be performed after age 40 only in “highly selected cases.” This selection process should carefully consider the amount of preoperative osteoarthritis, and a more accurate assessment of the articular cartilage, such as with dGEMRIC, may better identify candidates for PAO, particularly for this patient population. Because preliminary data suggest that PAO does not compromise the result of subsequent THA, and the results of revision THA after previous THA do not routinely compare to primary THA [14], periacetabular osteotomy is an important option for patients over 40 with dysplasia, who are not willing to undergo a THA.
The outcomes of PAO in most patients in our study has encouraged us to begin a prospective study with more extensive outcome measures, and with both radiographic and MR imaging. While PAO is a technically challenging procedure, the results in our three experienced centers suggest it has a role in treating selected patients over 40 with symptomatic acetabular dysplasia.
References
Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop. 2008;32:611–617. Epub 2007 Jun 20.
Crockarell J Jr, Trousdale RT, Cabanela ME, Berry DJ. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Relat Res. 1999;363:45–53.
Cunningham T, Jessel R, Zurakowski D, Millis MB, Kim YJ. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg Am. 2006;88:1540–1548.
Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty. 2008;23:960–963. Epub 2008 Mar 14.
Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724.
Kim YJ, Jaramillo D, Millis MB, Gray ML, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am. 2003;85:1987–1992.
Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7-15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840.
Lequesne M, deSeze S. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies [in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652.
Matheney TH, Kim Y-J, Zurakowski D, Matero C, Millis MB. Mid to long-term results of Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009, in press.
Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32.
Millis MB, Murphy SB. The Boston concept. peri-acetabular osteotomy with simultaneous arthrotomy via direct anterior approach [in German]. Orthopade. 1998;27:751–758.
Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98.
Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005;433:129–135.
Parvizi J, Burmeister H, Ganz R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin Orthop Relat Res. 2004;423:118–122.
Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926.
Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop. 2005;76:67–74.
Sambandam SN, Hull J, Jiranek WA. Factors predicting the failure of Bernese periacetabular osteotomy: a meta-regression analysis. Int Orthop. 2008 Aug 22. [Epub ahead of print].
Sharifi E, Sharifi H, Morshed S, Bozic K, Diab M. Cost-effectiveness analysis of periacetabular osteotomy. J Bone Joint Surg Am. 2008;90:1447–1456.
Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644.
Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. New York, NY: Springer; 1987.
Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85.
Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res. 1999;363:54–63.
van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002;84:339–343.
Wilberg G. Studies of dysplastic acetabula and congenital subluxation of the hip joint with special reference to the comlixation of osteoarthritis. Act Chir Scand (Suppl 58). 1939:7–38.
Yasunaga Y, Takahashi K, Ochi M, Ikuta Y, Hisatome T, Nakashiro J, Yamamoto S. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85:266–272.
Acknowledgments
We thank Clarissa Valim, MD, ScD, for her assistance with the statistical analysis and Catherine Matero for her assistance with organizing the data collection. We also thank Professor Reinhold Ganz for invaluable mentoring.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Children’s Hospital Boston, Boston, MA, Washington University School of Medicine, St. Louis, MO, and the Mayo Clinic, Rochester, MN.
About this article
Cite this article
Millis, M.B., Kain, M., Sierra, R. et al. Periacetabular Osteotomy for Acetabular Dysplasia in Patients Older than 40 Years: A Preliminary Study. Clin Orthop Relat Res 467, 2228–2234 (2009). https://doi.org/10.1007/s11999-009-0824-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0824-8