Abstract
The use of hexapod circular external fixators has simplified the ability to correct complex limb deformities without cumbersome frame reconfigurations. These frames are applied primarily using half pin mountings and may be difficult to utilize given the constraints of traditional half pin constructs. We compared the biomechanical performance of simplified divergent half pin frames to mountings currently being utilized for application of hexapod frames. Three 6-mm half pins per limb segment were placed into sawbones at 60° divergent angles in both the sagittal and coronal planes in a 2-cm diaphyseal fracture gap model. Pin mountings were attached to a standardized four-ring construct. This was compared to similar four-ring frames with two differing pin/wire configurations: (1) two tensioned wires per ring placed at 90° angles, a total eight wires; and (2) two 5-mm half pins per ring placed at 90° angles, a total eight half pins. The divergent 6-mm half pin frames demonstrated similar performance compared the standardized tensioned wire and 5-mm half pin frames in terms of axial micromotion and angular deflection. Based on the mechanical performance of these divergent half pin frames we believe they can be used clinically without detrimental consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the development of more sophisticated and complex external fixation devices [23, 24, 29] for the correction of complex malunions, nonunions, and deformities, there has been increased interest in simplifying the surgical techniques of frame application [13, 14, 19, 23], especially when utilizing devices that can be applied in multiple configurations [15, 23, 24, 26]. These complex devices have included monolateral external fixators configured in uniplanar and biplanar applications [3, 7, 10]; ring fixators [8, 18] with combinations of smooth and olive transfixion wires ring fixators with half pin mountings [13, 14] alone; and hybrid fixators [11, 21, 22, 23] with multiple pin and wire mountings in combination with ring and monolateral configurations [24, 27, 29]. All have sought to produce the ideal combination of stability and simplicity of application while allowing for appropriate micromotion at the site of pathology aiding in the production of fracture callus, distraction regenerate, or fracture remodeling. Additionally, the type of fixator must be versatile and adaptable to the character of the condition being treated, as well as optimized for cost in the current economic climate.
Simple monolateral fixators are advantageous for their ease of application, access to soft tissues, and ability to modify or perform frame “build down” over time [3–7]. The use of half pins has been adapted to circular fixation and many studies document the biomechanical properties of these half pin circular constructs [8, 20, 21]. Multiple pins are necessary to achieve performance comparable to traditional wire frames, and with the development of hexapod frames, the application of multiple pins and/or wires becomes problematic when selecting suitable mounting positions for fixation points. The fixation points have to respect anatomic constraints but must also respect the multiple support struts in order to avoid strut impingement. Many pin mounting configurations have been evaluated, as well as changes in the bar/ring geometry and pin/wire diameter [2–4, 6, 7].
Several studies have evaluated the effect of pin divergence (angle from the perpendicular) in terms of overall frame stability [19, 23, 25]. These studies suggest with increasing pin obliquity the stability of the pin-bone interface increases correspondingly. Rigidity against torsional strain is optimized at 60° divergence from the perpendicular as well [23, 25]. It is believed increasing pin diameter along with a corresponding increase in pin divergence angles will allow a simplified frame construct with no degradation in the mechanical performance of a circular frame [23–26]. Multiple divergent pins in both the coronal and sagittal planes, in theory, would stabilize a frame’s performance in all vectors.
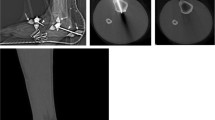
We have demonstrated high rates of union when treating periarticular fractures, complex deformity correction of nonunions and malunions, and limb lengthening and bone transport using multiple divergent pin circular frames [26–29] (Fig. 1). However, the exact orientation of pin placement and optimum number of pins is not known at this time.
(A) A divergent half pin frame using three 6-mm half pins above and below the nonunion is shown. Note each pin is divergent in both the coronal and sagittal planes allowing for simplified frame application. (B) This frame avoids the potential for pin/strut impingement as a minimum of fixation points are mounted to the frame and thus allows maximum excursion of the adjustment struts.
In this pilot study, we evaluated the biomechanical consequences of applying half pins at 60° divergent angles in external fixator frames stabilizing simulated diaphyseal defects. We then compared the stability of these divergent pin frames to standard ring fixator constructs currently in use clinically.
Materials and Methods
We simulated standardized transverse diaphyseal fractures of the tibia in Sawbones® (#3302; Pacific Regional Laboratories, Vashon WA, 405 mm) stabilized with one of three circular fixator mountings. Three separate frame configurations were tested: (1) a standard Ilizarov wire frame (90°-W) (n = 5); (2) a 5-mm half pin frame (90°-P) (n = 5); and (3) a 6-mm divergent frame (60°-D) (n = 5). A 2-cm fracture gap was standardized. The constructs were cycled under load on an MTS machine (MTS Systems, Eden Prairie, MN) and biplanar video analysis evaluated for displacement calculations. A power study was performed and determined five frames per configuration be tested for a total of 15 frames evaluated. We based our power study on the assumption that any decrease in frame stability in the divergent pin study group would be detrimental (ie, frame is less stable than is currently being provided by contemporary frame constructs). Thus any decrease in testing stability would be noted as potentially harmful and small differences would be considered unacceptable (significant).
The Sawbones tibiae were mounted proximally by placing a steel pot over the plateau with sagittal and coronal planes stabilized using bolts advanced into the pot until firm contact was achieved with the cortex. Distally, a steel pot with composite metal molded around the plafond was used for fixation. The pots were parallel to each other and perpendicular to the mechanical axis of the tibia. Mounting consistency was achieved by using a jig in which the tibiae were placed in the same position in the steel pot distally while the metal cooled and solidified around the plafond. This allowed mechanical loading parallel to the mechanical axis.
The external frames were then applied to the tibial construct. A mounting plate was used to position the tibia centrally in the frame for the traditional Ilizarov tensioned wire and 90° half pin model mountings. The central location was chosen for the control models as this is the most stable configuration for both the tensioned wire and half pin mountings combined. This position was chosen in an effort to achieve the most stable construct and to avoid the mechanical changes that occur when the bone is eccentrically located in the frame (Fig. 2A–B). For the divergent pin frames, the tibiae were mounted as they would be clinically located, eccentric in the frame with the rings positioned 3 cm from the anteromedial surface of the tibia. Eccentric location for the divergent configuration mimics the clinical situation and thus was tested in this fashion. This eccentric position also compensates for the extended pin length required to attach a pin to the frame and the tibia with extreme oblique pin insertion angles.
(A) This standard four-ring Ilizarov frame with two wires mounted on each ring with two rings above and below a fracture is similar to the construct tested. (B) The 90° orientation of two wires on each ring is shown with the bone located in the center of the ring. This wire positioning limits frame translation in both AP and mediolateral directions and is the most stable wire orientation.
Axial loads were applied using an MTS 858 test frame (MTS Systems). The models were cycled with 500 N at a frequency of 1 Hz for 3660 cycles. Most patients with frames do not fully weight bear initially following application of their frames. Because this is a defect model, we chose less than full weight bearing to simulate the known clinical situation. This simulates partial weight bearing for a limited testing period. Fatigue testing or testing to construct failure was not performed.
We constructed a standard four-ring Ilizarov frame (90º-W) using 180-mm carbon fiber rings (Fig. 2A). Each ring was mounted to the tibia with two smooth 1.8-mm transfixation stainless steel wires positioned 90° to each other (Fig. 2B). Two rings per each limb segment were applied on either side of proposed fracture with the inner rings positioned 1 cm from the osteotomy site and the proximal/distal rings 4 cm from the articular joint line to facilitate specimen potting and MTS mounting. All rings were connected via four threaded rods equidistant to each other. All wires were tensioned to 130 Kg using an Ilizarov wire tensioner. The osteotomy was completed using a reciprocating saw and a jig locked to the bone to ensue reproducibility (eight wires total).
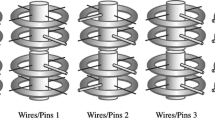
The same carbon-fiber four-ring frame (90º-P) was constructed analogous to the frame used for the Ilizarov wire model. Each ring was mounted to the tibia using two 5-mm stainless steel half pins at 90° to each other (coronal plane deviation only). Pins were inserted perpendicular to the rings and attached directly to the ring using appropriate pin-holding clamps. The juxtaosteotomy pins were placed 1 cm adjacent to the osteotomy site and the juxtaarticular pins were placed 1 cm from the mounting pots. The pins were placed perpendicular to the cortex at 90° to each other. Pin couples for each ring were oriented perpendicular to the frontal plane and parallel to the coronal plane for a 90° pin spread (eight pins total) (Fig. 3A–B).
(A) A 90° 5-mm half pin frame is mounted using two pins per ring placed perpendicular to each other for a total of eight half pins. Frames were preconstucted prior to mounting and subsequent osteotomy. (B) An axial view demonstrates the 90º pin orientation to each other. These pins do not diverge in the sagittal plane.
The 60° frame (60º-D) was constructed with the same four composite ring frame. Three 6-mm stainless steel pins were placed in the proximal limb segment and three 6-mm pins placed in the distal limb segment. Pins were placed 60° off the perpendicular in both the sagittal and coronal planes. The pin locations were similar in that the intercalary pins entered the bone approx 1 cm from the fracture gap on both sides of the fracture. And at either end of the model, the pins entered the bone 1 cm from the potting. For each limb segment, pin divergence in the coronal plane around the frame was set at 100° with the third pin bisecting the first two. This was selected as the maximum divergence allowable in the clinical situation that would avoid impingement of soft tissues of the anterior or posterior compartments. Each pin diverged 60° from the perpendicular in the sagittal axis for each model (Fig. 4A–B). All frames were preconstructed with pin-holding clamps mounted in predetermined locations to ensure standardization of divergent frame mountings (six pins total).
Under cyclic loading conditions, measurements of fracture displacement in the axial, coronal, and sagittal planes were calculated using digital video running at 30 frames per second. Two cameras were mounted at 90° to each other with one focused on the sagittal plane of the fracture and the other on the coronal plane. The duration of the testing was recorded for each model (Fig. 5). This digital data allowed frame-by-frame analysis using Macintosh iMovie (Apple, Cupertino, CA, USA). Still images were taken at the peak and trough of fracture gap movements. Measurements were made using still frames and the public domain NIH Image program (developed at the U.S. National Institutes of Health and available on the Internet at http://rsb.info.nih.gov/nih-image/). Measurements were made at the initial minute, 10, 20, 30, 40, 50, and 60 minutes. During this time frame, measurements were made every 10 cycles and entered into an Excel spreadsheet (Microsoft Corp., Redmond, WA). The initial position was used to calibrate to NIH Image measurements according to the measured fracture gap.
From these data, we analyzed direction and magnitude of all displacements to determine the total displacement as well as net strain. The axial, coronal, and sagittal displacements were analyzed during the testing duration and compared between frame groups. We did this to determine any temporal degradation during the testing.
Strain was described using measures of central tendency (mean and median) and variability (standard deviation and range). Each individual model’s degree of 3-D strain was evaluated (Tables 1, 2). Displacements in the axial, sagittal and coronal plane for each model and each frame construct were evaluated and compared. Net strain was calculated and compared between all frame configurations (The lower the median strain, the more rigid the frame).
Results
The transfixation wire model was less rigid (p = 0.02) than the 90° half pin model (median strain of 0.36 and 0.26, respectively). The transfixation wire model was also less rigid (p = 0.03) than the 60° oblique model (median strains of 0.36 and 0.26, respectively). The 60° and 90° half pin frames had similar (p = 1.00) median strains and were similar in their frame rigidity (0.26 in both cases) (Table 3).
Discussion
This pilot study was developed to determine the mechanical properties of an external fixator pin mounting that has been in use by the senior author (JTW) with excellent clinical results. We presumed the total strain associated with the divergent pin frame would be no different than the mechanical characteristics of other commonly used half pin and transfixation frames.
A major limitation of this study is that it only addresses mid-diaphyseal mounting configurations. For periarticular fractures or nonunions, the 60° divergent ring block would need to be combined with metaphyseal transfixation wires in order to evaluate this configuration for metaphyseal mountings. It is well known that large half pins should be avoided for metaphyseal fixation and thus this model does not address this clinical situation [23, 26]. We attempted to mount the frames respecting the anatomic constraints of the tibia. However the acute insertion angle of 60° may be difficult to perform clinically. This angle was chosen as it is the only alternative to perpendicular pins that has been mechanically evaluated in the literature [25]. The mountings described should not be translated exactly to the clinical situation, as these are idealized mountings and readers are cautioned against placing these pins without a thorough knowledge of the 3-D anatomy. This study suffers from the common limitation of sample size. If more frames in each configuration were available for testing, further parametric comparisons could be obtained. Additionally the overall effect of simply increasing the pin diameter from 5 mm to 6 mm in the 90°-P control frame is unknown.
Motion, specifically axial micromotion, increases the rate of fracture healing. However, at some threshold axial micromotion becomes excessive and will prevent healing [9, 15, 16]. Kenwright and Goodship [16] and others [17] induced axial compression in a clinical experiment showing a shorter time to weight bearing and an earlier radiographic appearance of healing. However, shear and torsional movements are undesirable for healing compared to axial loading [1]. The absolute magnitude of the strain applied at a fracture gap rather than the vector of strain determines its ability to form a stable osseous union [1, 2, 16–18]. This balance of rigidity and micromotion has yet to be adequately defined for an ideal stiffness of a fixator construct.
The traditional Ilizarov transfixation wire frame is more complex and requires additional training for safe application. As with all fixation methods, accuracy of reduction, preloading, and cortical contact are the primary determinants of stiffness [8, 17, 18]. However, for pure transfixation wire frames, multiple authors have demonstrated factors which can change the stiffness of these constructs [8, 12, 18, 20, 23]. Moving the rings closer together, increasing the number of wires, the use of olive wires, decreasing the ring diameter, increasing wire tension, and changing the ring material can all increase frame stiffness. Lastly, perpendicular crossing angles (90°) between the wires and central position of the bone in the frame maximize frame stiffness [18–20].
In order to simplify these complex circular frame mountings, investigators devised the concept of hybrid fixation—the use of transfixation wires in combination with monolateral half pin/bar constructs [10]. Numerous investigators demonstrated detrimental cantilever loading occurred with this construct despite ease of frame application [19–23]. Adjuvant anterior half pins as well as the use of full circular rings was necessary to achieve comparable stability [19–23]. Although perceived as simplistic to apply, these mechanically inferior hybrid frames have largely been abandoned.
Green et al. [13, 14] were the first to demonstrate reliable circular frame constructs utilizing large pin fixation techniques. A system of half pin connections facilitated the use of half pins in conjunction with a circular frame. The Rancho technique readily demonstrated the use of half pins to greatly simplify frame application. Multiple pin mountings using 5-mm half pin constructs [12, 13] with pins oriented perpendicular to the bone are described in this elegant simplified technique.
Our clinical experience with the 6-mm divergent half pin frames was driven by the desire to further simplify Greens’ frame application technique and yet avoid strut impingement of pins onto hexapod struts, when carrying out complex deformity corrections using the Taylor spatial frame (Smith & Nephew Inc, Memphis, TN). We believe decreasing the number of half pins and increasing the remaining half pin diameter with divergent pin orientations would help to avoid this troublesome complication without sacrificing frame stability. The use of this construct has been applied at our institution for deformity correction, malunion correction, nonunion, and definitive acute fracture management without clinical consequence [26–29]. The mechanical results demonstrate equivalent frame characteristics when a divergent frame is compared to constructs currently in clinical use.
For treating complex problems using external fixation, the surgeon must have a thorough understanding of the mechanical principals for the chosen technique. Additionally, the treatment method should optimize patient care and comfort, and minimize possible complications. In the current medical climate which values cost containment of resources, the judicious use of hardware, and the optimal functional outcome of treatment methods, this technique and frame construct is well-suited to these goals. However, this construct may not be well-suited to periarticular pathology where tensioned wires may be necessary to obtain a stable pin-bone interface rather than half pins in this location. The concept of three divergent 6-mm half pins per limb segment, however, is a valuable concept to use for all frame configurations treating mid diaphyseal pathology. While this frame allows for ease and economy of frame application, it can be used without sacrificing frame stability. This is in deference to previous frame constructs which promoted frame simplicity at the cost of frame stability.
References
Augat P, Burger J, Schorlemmer S, Henke T, Peraus M, Claes L. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res. 2003;21:1011–1017.
Augat P, Claes L, Hanselmann KF, Suger G, Fleischmann W. Increase of stability in external fracture fixation by hydroxyapatite-coated bone screws. J Appl Biomater. 1995;6:99–104.
Behrens F. A primer of fixator devices and configurations. Clin Orthop Relat Res. 1989;241:5–14.
Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989;241:15–23.
Behrens F, Comfort TH, Searls K, Denis F, Young TJ. Unilateral external fixation for severe open tibial fractures: a preliminary report of prospective evaluation. Clin Orthop Relat Res. 1983;178:111–120.
Behrens F, Johnson WD. Unilateral external fixation: methods to increase and reduce frame stiffness. Clin Orthop Relat Res. 1989;241:48–56.
Behrens F, Johnson WD, Koch TW, Kovacveic N. Bending stiffness of unilateral and bilateral fixator frames. Clin Orthop Relat Res. 1983;178:103–110.
Calhoun JH, Li F, Ledbetter BR, Gill CA. Biomechanics of the Ilizarov fixator for fracture fixation. Clin Orthop Relat Res. 1992;280:15–22.
Chao EYS, Aro HT, Lewallen DG, Kelly PJ. The effect of rigidity on fracture healing in external fixzation. Clin Orthop Relat Res. 1989;241:24–35.
Fischer DA. Skeletal stabilization with a multiplane external fixation device: design rationale and preliminary clinical experience. Clin Orthop Relat Res. 1983;180:50–62.
Fitzpatrick DC, Sommers MB, Kam BC, Marsh JL, Bottlang M. Knee stability after articulated external fixation. Am J Sports Med. 2005;33:1735–1741.
Gasser B, Boman B, Wyder D, Schneider E. Stiffness characteristics of the circular Ilizarov device as opposed to conventional external fixators. J Biomech Eng. 1990;112:15–21.
Green SA. The Ilizarov method: Rancho technique. Orthop Clin North Am. 1991;22:677–688.
Green SA, Harris L, Wall DM, Ishkanian J, Marinow H. The Rancho mounting technique for the Ilizarov method. A preliminary report. Clin Orthop Relat Res. 1992;280:104–116.
Kabata T, Tsuchiya H, Sakurakichi K, Yamashiro T, Watanabe K, Tomita K. Reconstruction with distraction osteogenesis for juxta-articular nonunions with bone loss. J Trauma. 2005;58:1213–1222.
Kenwright J, Goodship AE. Controlled mechanical stimulation in the treatment of tibial fractures. Clin Orthop Relat Res. 1989;241:36–47.
Kershaw CJ, Cunningham JL, Kenwright J. Tibial external fixation, weight bearing, and fracture movement. Clin Orthop Relat Res. 1993;293:28–36.
Kummer FJ. Biomechanics of the Ilizarov external fixator. Clin Orthop Relat Res. 1992;280:11–14.
Metcalfe AJ, Saleh M, Yang L. Techniques for improving stability in oblique fractures treated by circular fixation with particular reference to the sagittal plane. J Bone Joint Surg Br. 2005;87:868–872.
Podolsky A, Chao EY. Mechanical performance of Ilizarov circular external fixators in comparison with other external fixators. Clin Orthop Relat Res. 1993;293:61–70.
Pugh KJ, Wolinsky PR, Dawson JM, Stahlman GC. The biomechanics of hybrid external fixation. J Orthop Trauma. 1999;13:20–26.
Pugh KJ, Wolinsky PR, Pienkowski D, Banit D, Dawson JM. Comparative biomechanics of hybrid external fixation. J Orthop Trauma. 1999;13:418–425.
Roberts CS, Dodds JC, Perry K, Beck D, Seligson D, Voor MJ. Hybrid external fixation of the proximal tibia: strategies to improve frame stability. J Orthop Trauma. 2003;17:415–420.
Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of the Ilizarov-Taylor spatial frame. J Bone Joint Surg Am. 2006;88 Suppl 4:156–174.
Shearer J, Egan J. Computerized analysis of pin geometry. In: Coombs R, Green SA, Sarmeinto A, eds. External Fixation and Functional Bracing. London, UK: Orthotext; 1989:129–135.
Watson JT. Principles of External Fixation and Bone Transport. In: Rockwood CA, Green DP, Bucholz RW, eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006:258–296.
Watson JT. Distraction osteogenesis. J Am Acad Orthop Surg. 2006;14:S168–S174.
Watson JT, Anglen J. Infected fractures In: Stannard JP, Schmidt AH, Kregor PJ, eds. Surgical Treatment of Orthopaedic Trauma. New York, NY: Thieme; 2006:20–24.
Watson JT, Kuldjanov D. Bone defects. In: Rozbruch SR, Ilizarov S, eds. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare; 2006:185–201.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (JTW) has received funding from Smith & Nephew.
About this article
Cite this article
Lenarz, C., Bledsoe, G. & Watson, J.T. Circular External Fixation Frames with Divergent Half Pins: A Pilot Biomechanical Study. Clin Orthop Relat Res 466, 2933–2939 (2008). https://doi.org/10.1007/s11999-008-0492-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0492-0