Abstract
Patients with osteoarthritis secondary to developmental dysplasia of the hip (DDH) typically are young and active, which might affect functional ratings or failure rates after resurfacing arthroplasty. We therefore evaluated 24 patients (32 hips; mean age, 44.2 years) after hip resurfacing performed for osteoarthritis secondary to DDH. We used the Harris hip score (HHS), the University of California, Los Angeles (UCLA) activity scale, and a sports and activity questionnaire. A radiographic analysis also was performed. We followed patients a minimum of 28 months (mean, 43 months; range 28–60 months). The HHS improved from a mean of 54.7 to 97.3 and UCLA activity levels increased from a mean of 5.3 to 8.6. All patients returned to sports activity at a mean of 11 weeks after surface replacement. There were no major differences in preoperative and postoperative participation in the most common sports and activities. Two of the 32 replacements (6%) failed. We detected femoral radiolucencies in 10 of the remaining 30 hips. Despite satisfactory outcomes in clinical scores, return to sports, and hip biomechanics, the failure rate of 6% was disappointing. Additional followup is important to assess if failure rates increase in these young, active patients.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of modern metal-on-metal hip resurfacing arthroplasty has led to reports of encouraging short- to midterm results [2, 10, 17] and currently, there is a renaissance in use of these devices The fundamental concepts of hip resurfacing are to spare bone at the femoral side in young, active, and high-demand patients with osteoarthritis of the hip and to achieve greater stability with the large head. Back et al. reported improved HHS (from 63 to 98) and a 99% survivorship of Birmingham hip resurfacing 3 years after surgery in patients with a mean age of 52 years [5]. In a young group of patients (48 years), Daniel et al. reported only one failure in 440 hips a mean of 3.3 years after Birmingham hip resurfacing [10]. Amstutz et al. reported a revision rate of 3%, HHS of 94, and UCLA activity level of approximately 8 in patients 48 years old 3.5 years after surgery [2].
The group in whom hip resurfacing might be considered includes relatively young patients with osteoarthritis secondary to DDH. However, Amstutz et al. recently reported disappointing results of resurfacing for Crowe Types I and II DDH with respect to the durability of the femoral component [1]. Knecht et al. reported good functional results of resurfacing, but the short followup of only 1.5 years precludes drawing meaningful conclusions [14].
When performing arthroplasty in dysplastic hips, the anatomic abnormalities offer reconstructive challenges [4]. Moreover, increasing degrees of dysplasia, increased femoral antetorsion, abductor muscle insufficiency, adductor muscle contractures, and limb-length discrepancies contribute to an often observed abnormal gait pattern in these patients [18]. Because of these differences one might anticipate differing outcomes in patients with DDH.
We addressed the following questions: (1) Can hip resurfacing arthroplasty in patients with DDH provide improved clinical scores, increased range of motion (ROM), restoration of limb-length discrepancies, and a low failure rate?; (2) What are the radiographic results of component position, hip biomechanics, heterotopic ossifications, and radiolucencies?; and (3) Can the patients return to work and sports activity?
Materials and Methods
We retrospectively reviewed 24 selected patients (32 hips) who underwent hip resurfacing arthroplasty for osteoarthritis secondary to DDH between April 2002 and January 2005. During the same period 96 patients (mean age, 54.2 years) with DDH underwent stem-type THA. Indications for resurfacing included young age (ie, younger than 60 years), active lifestyle (ie, participation in sports), an explicit request by the patient to undergo resurfacing arthroplasty, and the absence of severe deformities of the proximal femur on plain radiographs such as excessive antetorsion, severe valgus or varus alignment, and severe head deformities. There were 18 women and six men; eight resurfacings were bilateral. Mean age at the time of surgery was 44.2 years (range, 30–57 years). All patients participated in sports before surgery. The preoperative body mass index (BMI) was 23.8 kg/m2 (range, 16.4–32.46 kg/m2). Classification of DDH was Crowe Type I in 27 hips and Type II in five hips; no hip was classified as Type III [9]. The mean preoperative center-edge (CE) angle according to Wiberg [20] was 15.3° (range, 5°–18°), and the mean preoperative acetabular roof (AC) angle was 18.6° (range, 11°–25°). Using the Kellgren and Lawrence classification, seven hips had Grade 2, 16 had Grade 3, and nine had Grade 4 osteoarthritis [13]. The minimum followup was 28 months (mean, 43.0 months; range, 28–60 months). No patients were lost to followup. The study was approved by the local ethical committee and all patients provided written informed consent.
Surgery was performed by two senior surgeons (OH, UM) using a posterior approach in all cases. The approach involved posterior release from the piriformis tendon to the gluteus maximus tendon. In all hips, we performed a partial incision of the gluteus maximus tendon to decrease muscle and soft tissue tension and to obtain better exposure. After a posterior incision of the capsule, the hip was dislocated and a partial capsulectomy anteriorly and superiorly was performed. Release of the inferior capsule completed the mobilization of the proximal femur. In 10 hips, the Durom prosthesis (Zimmer, Winterthur, Switzerland) was implanted, and in 22 hips, the Birmingham Hip Resurfacing prosthesis (BHR; Smith & Nephew, Solothurn, Switzerland) was used, depending on the surgeon’s preference. In two hips in the BHR group, we used the dysplasia cup with additional screw fixation. The gluteus maximus tendon was carefully repaired during wound closure and the posterior structures were reattached. Perioperative antibiotic prophylaxis was prescribed for all patients using a second-generation cephalosporin. Daily low-molecular-weight heparin was administered for 4 weeks postoperatively for prevention of thromboembolism. No radiation or indomethacin prevention for heterotopic ossification was used; however, most patients were given a nonsteroidal antiinflammatory drug (diclofenac) for approximately 1 week for pain. All patients started walking on the first postoperative day; weightbearing was allowed as tolerated. Crutches were used for 4 to 6 weeks after surgery.
Two of the authors (FDN, MS) clinically reevaluated all patients independently of our routine followups between February and June 2007. Neither author was involved in surgery. Harris hip scores and UCLA activity scale were assessed. The ROM was assessed clinically with a goniometer. Limb-length discrepancies were determined by measuring the length from the superior-anterior spine to the medial malleolus with the patient in the supine position. Using a self-designed sports and activity questionnaire [16], we assessed preoperative and postoperative sports activity. Preoperative and postoperative working status was recorded. Failures were defined as conversion or pending conversion to conventional THA for any reason. Complications included reoperations for any reason (except failures), dislocations, infections, nerve injuries, major hematomas, and iliopsoas irritations.
The radiographic analysis was performed by one of the authors (ML) who was blinded to the clinical results and not involved in surgery. The femoral component and cup position were assessed using standardized anteroposterior and (90°) cross-table radiographs. Anteversion or retroversion of the femoral component was assessed by measuring the stem axis in relation to the femoral neck axis on the 90°-cross–table radiographs. To assess biomechanical restoration of the hip, we calculated the hip lever arm ratio (abductor moment arm divided by body moment arm) and measured femoral offset (distance between the femoral shaft axis and the femoral head center). Heterotopic ossifications were determined according to the classification of Brooker et al. [7]. Radiolucent lines greater than 1 mm in thickness around the acetabular cup were recorded in the three zones described by DeLee and Charnley [11]. For femoral radiolucencies, we used the rating system developed by Amstutz et al. in which a score of 0 to 9 points was assigned based on lucencies in three zones around the femoral stem [2].
All data were tested for normal distribution using the Shapiro-Wilk W test. Differences between preoperative and postoperative scores (HHS, UCLA), ROM, neck-shaft angle, and stem shaft angle, and hip biomechanics were analyzed using two-tailed paired t-tests. The Wilcoxon signed ranks test was used to compare preoperative and postoperative frequency and duration of sports engagement. Analysis was performed using the software package SPSS (Version 14; SPSS Inc, Chicago, IL).
Results
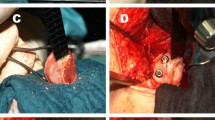
The HHS improved (p = 1.93E−14) from 54.7 (range, 36–83) to 97.3 (range, 72–100). UCLA activity levels increased (p = 2.46E−07) from 5.3 (range, 2–10) to 8.6 (range, 5–10). Thirteen of the patients had postoperative activity scores of 9 or 10, indicating participation in impact sports. Flexion improved (p = 0.0004) from 95.7° (range, 45°–120°) preoperatively to 106.7° (range, 90°–130°) after surgery. The internal/external rotation arc improved (p = 1.45E−05) from 33.8° (range, 0°–80°) to 53.8° (range, 25°–75°). Abduction increased (p = 0.0002) from 32.0° (range, 10°–50°) to 39.2° (range, 30°–50°). Preoperatively, eight patients had limb-length discrepancies of 1 cm or less, three had 1- to 2-cm discrepancies, and two had discrepancies greater than 2 cm. Residual discrepancies of 1 cm or less were detected in three patients postoperatively; limb-length discrepancies of 1.5 cm were observed in two patients. Two of the 32 hip resurfacings failed (6.3%). The first hip failed in a male patient as a result of a femoral neck fracture that occurred 6 weeks after resurfacing arthroplasty (Fig. 1A). The preoperative NSA was 118° after a previous femoral varisation osteotomy (Fig. 1B). Reevaluating the postoperative radiographs, we observed a 15° valgus position of the femoral component and notching at the head-neck junction (Fig. 1C). This hip was revised to a conventional stem with a modular large metal head; the socket was left in situ (Fig. 1D). The second hip was revised 6 months after resurfacing arthroplasty as a result of persistent hip pain in a female patient which we attributed to inferior component impingement as a result of component malpositioning (cup inclination 70°) (Fig. 2A). This hip was revised to a conventional stem-type design (both components replaced)(Fig. 2B). Both hips were classified as having Crowe Type I dysplasia. There was one hematoma, which resolved without additional surgery. No infections, dislocations, nerve palsy, or iliopsoas irritation occurred.
(A) A femoral neck fracture 6 weeks after resurfacing arthroplasty was the reason this hip resurfacing failed. (B) The preoperative radiograph of the patient’s hip showed a preoperative neck-shaft angle of 118° after a previous varisation osteotomy. (C) Reevaluating the postoperative radiographs, we observed a 15° valgus position of the femoral component and notching at the head-neck junction. (D) The hip was revised to a conventional stem with a modular large metal head; the socket was left in situ. The patient did well after the revision surgery.
(A) The second hip in our series was revised 6 months after resurfacing arthroplasty because the patient had persistent pain which we believed was related to an inferior component impingement after malpositioning of the socket. (B) The hip was revised to a conventional stem-type design (both components replaced). The patient did well after the revision surgery.
The postoperative radiographs revealed the femoral components were implanted in a mean of 2.5° relative valgus (p = 0.026) (Table 1). Based on cross-table radiographs, the femoral component was retroverted in 20 hips (Table 1). Femoral offset and the hip lever arm ratio increased (p = 5.15E−05 and p = 1.28E−06, respectively) after surgery (Table 1). Brooker Grade I heterotopic ossifications were seen in two hips (6.3%); there were no Grade II, III, or IV ossifications. No radiolucencies were observed on the acetabular side. Femoral radiolucencies around the metaphyseal stem were detected in 10 of the nonrevised hips (33.3%). Six of these hips with a score of 1 had radiolucencies only around the tip. Three hips with a score of 4 had lucencies in two zones and one hip had a score of 7 with incomplete lucencies in all three zones. All patients with metaphyseal stem lucencies were free of symptoms at the time of followup.
At a mean of 11.2 weeks (range, 6–28 weeks) after surface replacement, all patients returned to sports activity. They were engaged in 6.6 (range, 2–11) different recreational and sports activities before surgery and in 6.0 (range, 1–15) after resurfacing (p = 0.229). There were no major changes concerning preoperative and postoperative participation in the most frequent activities (Table 2). Sports that were completely stopped after surgery were single tennis (four patients), snowboarding (two), soccer (two), ice hockey, basketball, volleyball, and martial arts (one each). After surgery, one patient began playing competitive field hockey and one patient started high-intensity rock climbing. All patients were engaged in activities a mean of 3.3 times (range, 1–5) and 5.4 hours (range, 0.5–27.5 hours) per week preoperatively. After surgery, these values decreased to 2.8 times (range, 1–5; p = 0.015) and 4.1 hours (range, 1.5–20 hours; p = 0.012) per week, respectively. Surgery could maintain the patients’ ability to work; all 21 patients who were employed before surgery returned to work.
Discussion
The introduction of modern metal-on-metal hip resurfacing arthroplasty has led to reports of encouraging short- to midterm results [2, 10, 17]. The device is commonly used to treat young and active patients, and one group in whom this might be considered includes relatively young patients with osteoarthritis secondary to DDH. The anatomic abnormalities in DDH offer surgical challenges [4], particularly in resurfacing, and therefore one might anticipate differing complication rates or outcomes in patients with DDH. Our study addressed the following questions: (1) Can hip resurfacing arthroplasty in patients with DDH provide improved clinical scores, increased ROM, restoration of limb-length discrepancies, and a low failure rate?; (2) What are the radiographic results for component position, hip biomechanics, heterotopic ossifications, and radiolucencies?; and (3) Can patients return to work and sports activity?
Our study has numerous limitations. The results are short-term of a relatively small number of patients. More valid conclusions particularly regarding the clinical importance of femoral stem radiolucencies might have been drawn after longer observation, but we believe the high revision rate in this young and physically active group of patients warrants this report. The inclusion of two different implants might have been a confounding factor; however we did not find differences between the implants concerning clinical scores, radiographic parameters, and sports activity (data not shown). Finally, the lack of a control group (ie, patients with DDH who underwent stem-type THA) is an additional weakness.
With respect to the HHS, UCLA scale, and ROM, our clinical results were satisfactory and consistent with those reported for patients treated with surface arthroplasty for reasons other than dysplasia [2]. Our results also are comparable to those reported by Amstutz et al. for patients with Crowe Types I and II DDH [1]. One obvious limitation of resurfacing in patients with DDH is that limb-length discrepancies cannot be adequately corrected. Approximately two-thirds of the patients with limb-length discrepancies before surgery had residual discrepancies after hip resurfacing. Amstutz et al. reported residual limb-length discrepancies in approximately 30% of their patients with DDH who had discrepancies before resurfacing [1]. Failures at the femoral side are the main limitation of surface replacement survival [3, 8]. Accordingly, one patient in our series had a femoral neck fracture 6 weeks after surface replacement. We attribute this failure to improper patient selection and surgical errors. The hip had a preoperative NSA of only 118° after previous femoral varisation osteotomy, a large femoral head cyst, and the postoperative radiographs revealed notching at the head-neck junction. All of these features are well-known risk factors for femoral failure [3, 8]. The second failure was related to persistent hip pain we believed was related to component malposition (cup inclination of 70°); revision was performed 6 months after the index surgery. Although the failure rate of 6% was high, both failures could be partially ascribed to poor patient selection and improper component positioning. Our revision rate is between those reported by Amstutz et al. for hip resurfacing in patients independent of the etiology (3% at 3.5 years) and for surface replacement in patients with DDH (10% at 6 years) [1, 2].
Radiographically, we observed a postoperative stem-shaft angle of approximately 139° and cup inclination of 47°, therefore, the achieved component positions are similar to those reported after surface replacement in nondysplastic hips [2, 5]. We found the femoral offset and hip lever arm ratio, improved in these patients. This observation contrasts those of previous reports showing that femoral offset and hip lever arm ratio decreased after surface arthroplasty, but in nondysplastic hips [12, 15]. We attribute this difference to the restoration of a normal center of rotation in the resurfaced dysplastic hip. Compared with previous reports [5, 19], we observed a low incidence of heterotopic ossifications (6.3% Grade I ossifications), although no indomethacin or radiation was administered to prevent heterotopic ossifications. The low incidence of heterotopic ossifications in our patients might be a result of the combination of the surgical approach (posterior with a routine partial release of the gluteus maximus tendon to reduce soft tissue and muscle tension), careful coverage of the soft tissues with a cloth during all reaming steps (to avoid dissemination of bony particles), and use of nonsteroidal antiinflammatory drugs for pain in most patients. An incidence of femoral stem radiolucencies of approximately 30% or greater also was reported [2, 17]. Most of the lucencies detected in our patients were localized sclerotic lines at the tip of the metaphyseal stem. All patients with radiolucencies were completely free of symptoms, however, longer-term followup is needed to determine the clinical importance and potential progression of these lucencies. Surgically, anterior wall deficiency was addressed successfully with approximately 25°-cup anteversion. Despite not having objective measurements of anterior coverage such as CT scans, at followup, none of the patients had clinical signs of a psoas affection, which would suggest insufficient seating of the cup under the anterior wall. Another challenge was restoration of limb length, which similarly is limited with resurfacing as the correction of excessive femoral antetorsion, which we suggest as an exclusion criterion for surface replacement.
All employed patients resumed work after surgery and all returned to sports activities. In general, our patients participate in sports or activities of their choice after surgery as long as they have no symptoms or pain. However, we do not recommend high-impact activities with running and jumping sequences. Each patient is educated individually concerning her or his expectations and apprised that we recommend low- and middle-impact activities such as cycling, swimming, hiking, fitness-/weight-training, golf, cross-country- and downhill skiing (except short-turns and moguls) postoperatively. Despite several high impact activities being stopped (as we recommended), greater than 40% of patients engaged in impact sports after surgery. The patients participated in a mean of six different sports and activities three times and 4 hours per week. These values are in line with those reported for patients who underwent surface arthroplasty for reasons other than dysplasia [16]. Nevertheless, the high activity levels should be considered with respect to the increased risk of implant failure, particularly for female patients with DDH [6].
Our data suggest the clinical outcome of hip resurfacing arthroplasty in patients with DDH is satisfactory at short-term followup with respect to clinical scores, restoration of hip biomechanics, and return to sports activity. However, limb-length discrepancies were not adequately corrected and the 6% failure rate 3.6 years after surgery was higher than anticipated. Longer followup is important to assess if failure rates increase in this young, active group of patients.
References
Amstutz HC, Antoniades JT, Le Duff MJ. Results of metal-on-metal hybrid hip resurfacing for Crowe type-I and II developmental dysplasia. J Bone Joint Surg Am. 2007;89:339–346.
Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39.
Amstutz HC, Campbell PA, Le Duff MJ. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg Am. 2004;86:1874–1877.
Argenson JN, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–45.
Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329.
Beaule PE, Dorey FJ, LeDuff M, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93.
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632.
Campbell P, Beaule PE, Ebramzadeh E, LeDuff M, De Smet K, Lu Z, Amstutz HC. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46.
Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23.
Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32.
Girard J, Lavigne M, Vendittoli PA, Roy AG. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88:721–726.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Knecht A, Witzleb WC, Beichler T, Gunther KP. [Functional results after surface replacement of the hip: comparison between dysplasia and idiopathic osteoarthritis][in German]. Z Orthop Ihre Grenzgeb. 2004;142:279–285.
Loughead JM, Chesney D, Holland JP, McCaskie AW. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg Br. 2005;87:163–166.
Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–711.
Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip: a five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600.
Romano CL, Frigo C, Randelli G, Pedotti A. Analysis of the gait of adults who had residua of congenital dysplasia of the hip. J Bone Joint Surg Am. 1996;78:1468–1479.
Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939;58:5–135.
Acknowledgments
We thank Nicola A. Maffiuletti, Katharina Widler, Marguerite Staub, and Seraina Rizzi for help with the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Naal, F.D., Schmied, M., Munzinger, U. et al. Outcome of Hip Resurfacing Arthroplasty in Patients with Developmental Hip Dysplasia. Clin Orthop Relat Res 467, 1516–1521 (2009). https://doi.org/10.1007/s11999-008-0456-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0456-4