Abstract
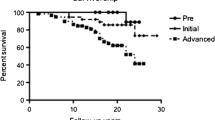
Long-term results of periacetabular osteotomy for advanced-stage osteoarthritis secondary to developmental dysplasia of the hip are reportedly unsatisfactory compared with results for early-stage osteoarthritis. Other preoperative information that can be used to determine indications for periacetabular osteotomy is therefore important to avoid performing osteotomy in young patients with advanced-stage osteoarthritis who would not likely achieve substantial benefit. We retrospectively reviewed 47 patients (49 hips) with advanced-stage osteoarthritis who underwent rotational acetabular osteotomy (RAO) using preoperative congruency in abduction. The minimum postoperative followup was 8 years (mean, 12.3 years; range, 8–20 years) and mean age at surgery was 43.1 years (range, 30–59 years). At followup, osteoarthritic stage was improved in 12 hips, unchanged in 24 hips, and had progressed in 13 hips. Preoperative joint congruency in abduction was good in 13 hips, poor in 32 hips, and narrowed in four hips. Patients with better congruency in abduction had better results. We believe osteoarthritis with good congruency in abduction preoperatively remains a good indication for RAO even in advanced stages of disease.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is one of the most common causes of secondary osteoarthritis in young adults (average, 29.9 years; range, 13–61 years) [4]. Periacetabular osteotomy, such as Steel’s triple osteotomy [23], Eppright’s dial osteotomy [2], the RAO developed by Ninomiya and Tagawa [14], and Ganz periacetabular osteotomy [3], allow the femoral head to be covered with articular cartilage. There have been some reports of periacetabular osteotomy on patients with DDH and advanced-stage osteoarthritis [8, 16, 24, 31], and the few published long-term results suggest variable results (23%–50% progression of osteoarthritis stage at 8.5–13 years followup) [16, 24, 31].
Numerous factors influence the long-term results of periacetabular osteotomy, including age at operation [32], operative technique [10], and osteoarthritis stage [13]. In a study of the long-term results of RAO for advanced osteoarthritis of the hip [16], we identified contraindications to RAO in patients who have a deformity of the femoral head that is associated with advanced osteoarthritis; however, at followup we could not predict the patients with excellent results using preoperative roundness of the femoral head. Based on putative predictive factors, numerous studies report the use of preoperative functional radiographs to identify candidates for periacetabular osteotomy [1, 11, 26, 30] but these studies did not consider congruency in abduction.
Therefore, we asked: (1) would patients with good preoperative joint congruency have better results than those without; and (2) would differences in preoperative severity of dysplasia and femoral head coverage after surgery influence the likelihood of having excellent, good, and poor results at followup?
Materials and Methods
We retrospectively reviewed 56 patients (58 hips) in whom RAO was performed for advanced stage osteoarthritis secondary to DDH between 1985 and 1998. Indications for RAO were a CE angle [29] less than 20° on radiographs, progressive pain that interfered with daily activities, and age younger than 60 years. Nine patients were lost to followup after more than 8 years. Forty-seven patients (49 hips) had more than 8 years followup consisting of clinical and radiographic assessments (recall rate of 84%). Forty-four of these 49 hips were described previously in an analysis of the long-term results of RAO for advanced osteoarthritis of the hip [16]. There were 44 women and three men with a mean age at surgery of 43.1 years (range, 30–59 years). The minimum followup for all 47 patients was 8 years (mean, 12.3 years; range, 8–20 years).
Acetabular osteotomy was performed according to the technique of Ninomiya and Tagawa [14]. The patient was placed in the lateral decubitus position. We used a combination of anterior iliofemoral and posterior approaches through one, anteriorly convex skin incision. After circumferential exposure, an osteotomy was performed using a special curved osteotome, starting just outside the capsule. The acetabular fragment was rotated anterolaterally and transfixed to the pelvis with two Kirschner wires. Nonweightbearing mobilization was allowed after surgery. One-third partial weightbearing with crutches was allowed in the sixth postoperative week, two-thirds partial weightbearing at 3 months, and full weightbearing at 4 months.
One of the authors (KO) evaluated preoperative and postoperative function using the scoring system of Merle d’Aubigné and Postel [12], that assigns a maximum of 6 points in each of three categories (pain, mobility, ability to walk). The preoperative scores were recorded routinely on the patients’ charts by an independent assessor. All scores at followup were recorded by one of the authors (KO).
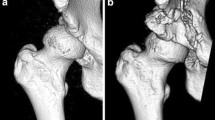
Anteroposterior radiographs were taken preoperatively, 3 months postoperatively, and at the final followup. All radiographs were taken with the patients in the supine position. Anteroposterior radiographs were taken with a source-to-film distance of 110 cm. The patient’s feet were internally rotated with the toes at 15° ± 5° to ensure the xray beam was centered on the superior aspect of the pubic symphysis. For each patient, two conventional pelvic radiographs were taken preoperatively. We obtained the first film in the neutral position and the second film in abduction [27]. One of the authors (KO) classified osteoarthritis before surgery and at followup into four stages according to the modified radiographic staging system of the Japanese Orthopaedic Association [13]: Stage 1 (prearthritis stage) is characterized by no osteoarthritic change; Stage 2 (early stage) has slight narrowing of the joint space (2 mm or greater joint space remaining); Stage 3 (advanced stage) has narrowing of the joint space (less than 2 mm joint space remaining); and Stage 4 (end stage) has complete loss of the joint space. The inclusion criterion for this study was Stage 3 (advanced stage) osteoarthritis. To evaluate joint congruency, we used the modified classification according to Yasunaga et al. [30]. Preoperative joint congruency in abduction and postoperative congruency in neutral position were classified into three grades. The preoperative joint congruency was graded as good if the joint space width at the narrowest point was 50% or greater of the widest point, poor if the joint space width at the narrowest point was less than 50% of that at the widest point, and narrowed if no more than 2 mm joint space remained in any area of the hip (Fig. 1).
To test the reproducibility of the radiographic measurements, three of the authors (KO, HE, MO) measured the narrowest and widest points of the joint space width, CE angle, AHI, and acetabular angle in five randomly selected hips. Each observer measured each hip three times with a 1-week interval between measurements. We analyzed the data for intraobserver and interobserver variances. The interclass correlation coefficients of joint space width, CE angle [29], AHI [6], and acetabular angle [20] were 0.96, 0.97, 0.99, and 0.99, respectively, for intraobserver variances and 0.95, 0.95, 0.97, and 0.98, respectively, for interobserver variances. Two authors (KO, HE) examined interobserver reproducibility of osteoarthritis stage at followup and preoperative congruency in abduction using 20 randomly selected hips. Interobserver variability (kappa statistics) was 0.93 and 0.92, respectively.
To evaluate the results of RAO, we classified the patients into three groups according to radiographic and clinical results at followup. Excellent was defined as osteoarthritis Stage 1 or 2 at followup (improved from preoperative stage) and pain and mobility scores greater than 5 points (maximum 6 points); good was defined as osteoarthritis Stage 3 at followup (same as preoperative stage); and poor was defined as osteoarthritis Stage 4 at followup (progressed from preoperative stage).
Based on the above classification, 12 hips had excellent results, 24 had good results, and 13 had poor results at followup. We compared these three groups for age at operation, duration of followup, CE angle, AHI, acetabular angle, and Merle d’Aubigné and Postel score. Four hips that progressed to end stage underwent THA during the followup period. These four hips were classified in the poor group.
We used the Mann–Whitney U test to compare preoperative congruency and followup results, and Wilcoxon rank tests to compare preoperative and postoperative CE angles, AHI, and acetabular angle. Kruskal–Wallis tests were used to compare age at operation, duration of followup, CE angle, AHI, acetabular angle, and Merle d’Aubigné and Postel clinical score among three groups (excellent, good, poor results at followup).
Results
Patients with better preoperative joint congruency in abduction had better results (p = 0.001). Preoperative joint congruency in abduction was good in 13 hips (27%), poor in 32 (65%), and narrowed in four (8%). The 13 hips with good congruency preoperatively resulted in nine hips in the excellent group, three in the good group, and one in the poor group at followup. The 36 hips with poor and narrowed congruency resulted in three hips in the excellent group, 21 in the good group, and 12 in the poor group at followup. Postoperative joint congruency in neutral position was good in 14 hips (29%), poor in 32 (65%), and narrowed in three (6%). Good preoperative congruency in abduction (p = 0.001) and postoperative congruency in neutral position (p < 0.001) were observed more often in patients with excellent results at followup than in patients who had preoperative poor or narrowed congruency (Table 1).
Center-edge angle, AHI, and acetabular angle were improved (p < 0.001) after surgery, with no preoperative, postoperative, and followup differences in these parameters among the groups. The Merle d’Aubigné-Postel scores were improved only in the excellent (p = 0.011) and good (p < 0.001) groups (Table 2).
No intraoperative or early postoperative complications, such as perforation of the joint using a chisel, deep infection, postoperative movement of the rotated acetabulum, or delayed union of the osteotomy site, were observed in any patient.
Discussion
Preoperative information predicting poor outcomes of periacetabular osteotomy is important to avoid performing osteotomy in young patients with advanced-stage osteoarthritis who would not likely achieve substantial benefit. We therefore asked whether: (1) patients with good preoperative joint congruency had better results than those without good congruency; and (2) do differences in preoperative severity of dysplasia and femoral head coverage after surgery predict patients with excellent, good, and poor results at followup?
Our study has several limitations. First, although we compared our results with those of previously published studies, this retrospective study lacked a control group from the same interval and followup. We cannot be certain whether the differences are important because of heterogeneity in patient selection, surgery, and outcome evaluation. This limitation could be applicable to any study using historical controls. Second, we did not use independent observers for the clinical assessments. Third, we used categorical ratings for the outcomes. Our particular rating is somewhat arbitrary, and we cannot ensure the likelihood of having a good given predictive variable would not change if we used differing definitions for the categories. Despite these limitations, however, we believe our data allow us to address our questions.
Preoperative osteoarthritis stage reportedly influences the results of periacetabular osteotomy [9, 13, 18, 22, 28]. For early-stage osteoarthritis secondary to DDH, satisfactory long-term results of periacetabular osteotomy have been reported [13, 15, 25]; however, for advanced-stage disease, the few published middle or long-term results suggest that 23% to 50% of patients progressed to end stage or that THA was performed as an additional operation after 8.5 to 13 years followup [16, 24, 31]. Some authors described the relationship between postoperative data and final results of osteotomy [5, 15, 17, 19, 31] (Table 3); however, postoperative data, unlike preoperative data, are not useful in planning the surgery. Several authors have suggested periacetabular repeat osteotomy could be considered in patients who showed improvement in joint congruency with the hip in abduction [1, 11, 26, 30]. Postoperative joint congruency is reportedly a useful predictor of postoperative outcomes [31]. Nine of our 13 hips with good congruency in abduction had excellent results at followups greater than 8 years. Even in patients with advanced-stage osteoarthritis, indications for RAO were noted in hips with good preoperative congruency in abduction (Figs. 2, 3). Theoretically, if a nondegenerative portion of the hip remained in a nonweightbearing area, periacetabular osteotomy might shift an area of the acetabulum that was not already altered by the degenerative process to the weightbearing area. Good joint congruency in abduction preoperatively therefore might predict whether the nondegenerative area could be shifted to the weightbearing area postoperatively. Some cartilaginous remodeling after RAO was reported in an animal model [21]. Good congruency after RAO may reduce the instability between the femoral head and rotated acetabulum and disperse weightbearing, which because of hip dysplasia had been concentrated on a small area of the acetabulum preoperatively, to a wider area of the acetabulum postoperatively. These conditions may stimulate cartilage remodeling even in advanced stages of osteoarthritis.
(A) Preoperative radiographs of a 35-year-old woman show advanced-stage osteoarthritis, and (B) good congruency in abduction. Her hip score was 11 points. Radiographs obtained (C) 3 months postoperatively and (D) 13 years postoperatively show early-stage osteoarthritis associated with increased joint space width. The hip score was 18 points.
Preoperative radiographs of the hip of a 42-year-old woman show (A) advanced-stage osteoarthritis, and (B) good congruency in abduction.. Her hip score was 11 points. Radiographs obtained (C) 3 months postoperatively, and (D) 10 years postoperatively show early-stage osteoarthritis associated with increased joint space width. The hip score was 17 points.
There have been some reports describing the relationship between postoperative coverage of the femoral head and long-term results of periacetabular osteotomy (Table 3). Some authors reported no relationship between preoperative and postoperative CE angles, AHI, acetabular roof obliquity [15, 31], and followup results, whereas others reported that postoperative CE angle [4] and AHI [7, 19] in patients with good results were larger than in patients with poor results. To obtain better femoral head coverage, the surgical approach [7] or line of osteotomy [5] has been modified. We observed no differences in femoral head coverage radiographically among our patients with excellent, good, or poor results at followup. According to our results, even if sufficient coverage of the acetabulum is obtained by a superior surgical technique during RAO, patients without good congruency in abduction preoperatively may have poor results more than 8 years later.
We consider osteoarthritis associated with good congruency in abduction preoperatively a good indication for RAO, even in patients with advanced stages of disease. In contrast, patients without good congruency in abduction and advanced osteoarthritis may experience progression to end-stage disease with this procedure.
References
Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417–1423.
Eppright RH. Dial osteotomy of the acetabulum in the treatment of dysplasia of the hip. J Bone Joint Surg Am. 1975;57:1172.
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36.
Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T. The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg. 1992;111:187–191.
Hasegawa Y, Masui T, Yamaguchi J, Kawabe K, Suzuki S. Factors leading to osteoarthritis after eccentric rotational acetabular osteotomy. Clin Orthop Relat Res. 2007;459:207–215.
Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–768.
Ito H, Matsuno T, Minami A. Rotational acetabular osteotomy through an Ollier lateral u approach. Clin Orthop Relat Res. 2007;459:200–206.
Kanai H, Takatori Y, Umeyama T, Nakamura S, Morimoto S, Ninomiya S. Rotational acetabular osteotomy for the treatment of dysplastic hips with end-stage osteoarthrosis: a biological alternative to total hip arthroplasty? Arch Orthop Trauma Surg. 1999;119:376–379.
Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840.
Matsui M, Masuhara K, Nakata K, Nishii T, Sugano N, Ochi T. Early deterioration after modified rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Br. 1997;79:220–224.
Mayo KA, Trumble SJ, Mast JW. Results of periacetabular osteotomy in patients with previous surgery for hip dysplasia. Clin Orthop Relat Res. 1999;363:73–80.
Merle d’Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475.
Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69:259–265.
Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430–436.
Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia: a follow-up for more than ten years. J Bone Joint Surg Br. 2002;84:59–65.
Okano K, Enomoto H, Osaki M, Shindo H. Rotational acetabular osteotomy for advanced osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg Br. 2008;90:23–26.
Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926.
Schramm M, Hohmann D, Radespiel-Troger M, Pitto RP. Treatment of the dysplastic acetabulum with Wagner spherical osteotomy: a study of patients followed for a minimum of twenty years. J Bone Joint Surg Am. 2003;85:808–814.
Schramm M, Pitto RP, Bar K, Meyer M, Rohm E, Hohmann D. Prophylaxis of secondary osteoarthrosis with spherical osteotomy in residual acetabular dysplasia: analysis of predictive factors of success. Arch Orthop Trauma Surg. 1999;119:418–422.
Sharp IK. Acetabular dysplasia: the acetabular angle. J Bone Joint Surg Br. 1961;43:268–272.
Shimogaki K, Yasunaga Y, Ochi M. A histological study of articular cartilage after rotational acetabular osteotomy for hip dysplasia. J Bone Joint Surg Br. 2005;87:1019–1023.
Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20.
Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973;55:343–350.
Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I. Long-term results of rotational acetabular osteotomy in young patients with advanced osteoarthrosis of the hip. J Orthop Sci. 2000;5:336–341.
Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I, Mabuchi A. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci. 2001;6:137–140.
Trousdale RT, Cabanela ME. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand. 2003;74:119–126.
von Rosen S. Diagnosis and treatment of congenital dislocation of the hip joint in the new-born. J Bone Joint Surg Br. 1962;44:284–291.
Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;58:28–38.
Yasunaga Y, Ikuta Y, Kanazawa T, Takahashi K, Hisatome T. The state of the articular cartilage at the time of surgery as an indication for rotational acetabular osteotomy. J Bone Joint Surg Br. 2001;83:1001–1004.
Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am. 2006;88:1915–1919.
Yasunaga Y, Takahashi K, Ochi M, Ikuta Y, Hisatome T, Nakashiro J, Yamamoto S. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85:266–272.
Acknowledgments
We thank Dr. Katsuro Iwasaki, Dr. Kenji Yamada, and Dr. Katsuro Takahashi for assistance and advice concerning RAO.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Okano, K., Enomoto, H., Osaki, M. et al. Joint Congruency as an Indication for Rotational Acetabular Osteotomy. Clin Orthop Relat Res 467, 894–900 (2009). https://doi.org/10.1007/s11999-008-0443-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0443-9