Abstract
We asked whether radiographic angles and signs of hip osteoarthrosis differ between radiographs of the pelvis taken in standing and supine positions. We retrospectively reviewed the radiographs of 61 patients (72 hips) with developmental dislocation of the hip. The minimum followup after closed reduction was 15 years (mean, 44 years; range, 15–64 years). We used pelvic radiographs in supine and standing positions taken at the same time and determined the following parameters: minimal joint space width, acetabular roof obliquity (AC angle), depth of the acetabulum (ACM angle), and center-edge angle. Osteoarthrosis was assessed according to Kellgren and Lawrence. Two independent observers measured all radiographs manually with a goniometer. AC angle, center-edge angle, and minimum joint space width differed between the radiographs taken in supine and standing positions at followup, whereas osteoarthrosis grading and the ACM angle did not. The AC angle depended on patient position and predicted development of osteoarthrosis. The minimum joint space width was influenced by the radiographic position with greater values in the supine position. ACM angle and the osteoarthrosis grade according to Kellgren and Lawrence were unaffected by the patient’s position.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical decisions are often based on radiographic parameters. Symptoms may or may not predate radiographic changes [14]. Radiographs of the pelvis are routinely used to diagnose, observe, or predict the natural course of developmental hip dislocation (DDH). Several features on planar radiographs of the hip (acetabular roof obliquity, depth of the acetabulum, center-edge angle) and radiographic signs (Kellgren and Lawrence [5]) of osteoarthrosis (OA) are particularly used. However, in addition to the problems of inter- and intraobserver reliability, the position of the patient can influence the information obtained from these radiographs. In most hospitals, the radiographs are routinely taken in the supine position. Radiographs taken in the standing position are likely to differ from those taken in the supine position, although this issue has been rarely addressed [10–12].
We asked whether the above radiographic angles and signs of hip OA differ between standing and supine positions in a long-term followup of patients after closed reduction of developmental hip dislocation and whether the angles correlated with the development of OA.
Materials and Methods
We retrospectively reviewed the radiographs of 61 patients (71 hips) with DDH. All patients had been treated by closed reduction alone [6]. In 10 patients, both hips had been treated. All patients were treated at the University of Iowa Hospitals and Clinics. Fifty-one patients were female and 10 patients were male. The average age at the time of closed reduction was 17.9 months (standard deviation [SD], 14.3; range, 1–96 months). The average age at the time of evaluation was 45.9 years (SD, 8.7; range, 23–66 years). The minimum followup after closed reduction was 15 years (mean, 44 years; range, 15–64.3 years) at last evaluation.
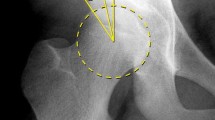
We used pelvic radiographs in the supine and standing positions to determine the following parameters: minimal joint space width of the hips, Kellgren and Lawrence classification for OA [5] (Table 1), acetabular roof obliquity (AC angle [1]) (Fig. 1), depth of the acetabulum (ACM angle [4]) (Fig. 2), and the center-edge angle (CE angle as described by Wiberg [15]) (Fig. 3). All radiographs were taken sequentially at the same followup examination.
This radiograph demonstrates the correct measurement of the CE angle of Wiberg [15].
Two independent observers (SF, CP) measured all radiographs twice manually with a goniometer; neither observer was the treating physician. One investigator was an experienced orthopaedic surgeon (SF), whereas the other was a last-year medical student (CP). Interobserver and intraobserver reliability (test-retest) was calculated for all parameters. Pearson’s correlation coefficients between the two measurements from the same individual were always higher (p < 0.001) than r = 0.9 for Examiner 1 (SF) and higher (p < 0.001) than r = 0.86 for Examiner 2 (CP) in all parameters. Thus, we decided to use the average from both measurements of one examiner for further analysis. Pearson’s correlation coefficients between the two examiners were always higher (p < 0.001) than r = 0.78 in all parameters. Thus, we used the average from both examiners for further analysis. The correlation coefficients of the overall average of each parameter with each single measurement were always higher (p < 0.001) than r = 0.9.
We used Student’s t-test for paired samples to compare the three angles and Kellgren-Lawrence grade [5] in the same patient at different times and Student’s t-test for unpaired samples to compare the parameters between groups of patients at the same time. We checked the normality assumption by Kolmogorov-Smirnov testing. Pearson’s coefficient was calculated for determination of correlations. To determine any possible relationship of late OA to the measured angles, we divided the hips into two subgroups based on normal values by Tönnis [10] for the measured AC angle at last followup, one group with an angle less than 15° (n = 32) and the other with an angle greater than 15° (n = 27). We similarly compared the incidence of OA in hips that at followup had an ACM angle of less than 50° (n = 23) versus an ACM angle of greater than 50° (n = 36) and a CE angle of less than 30° (n = 44) compared with those greater than 30° (n = 15). Analysis was performed using the Statistical Package for Social Sciences for Windows, release 11.0 (SPSS GmbH, Munich, Germany).
Results
The AC angle, CE angle, and minimum joint space width differed between the radiographs taken in supine and standing positions at followup, whereas the OA grading according to Kellgren and Lawrence [5] and the ACM angle did not (Table 2). AC angles were greater (p < 0.001), CE angles smaller (p < 0.001), and minimum joint space width was less (p < 0.001) in standing radiographs (Table 2).
We found no correlations between the AC, ACM, and CE angles and the radiographic signs of OA. Hips with an AC angle of less than 15° had greater (p ≤ 0.01) Kellgren and Lawrence scores [5] in supine and standing radiographs compared with those with an AC angle of greater than 15° (Table 3). Neither the initial ACM angle nor CE angle predicted OA.
Discussion
Because radiographic angles to monitor patients with DDH for development of OA are based on plane films of the pelvis and because the findings are prone to intra- and interobserver variability and patient positioning (supine versus standing), we asked whether those radiographic angles and signs of OA differed between standing and supine positions, and whether the angles correlated with the development of OA.
We acknowledge several limitations. The angles were determined manually on radiograph hard copies by ruler and goniometer. On some radiographs, it was difficult to determine the superior point of the tear drop figure as reference marker for the measurement of the AC angle. There is also a potential risk of measurement error determining the center of the femoral head to estimate the CE angle. Computer-aided measurement aids in calculation but still depends upon manual location of anatomic landmarks. Furthermore, pelvic inclination and its direct influence on the measured angles is difficult to control on a standard radiograph of the pelvis [8]. However, our intra- and interobserver calculation demonstrated reliability measurements.
We found the AC angle, CE angle, and minimum joint space width differed between the radiographs taken in the supine and standing positions at followup, whereas the OA grading according to Kellgren and Lawrence [5] and the ACM angle did not. We observed no correlation of the three angles and radiographic signs of OA. Tönnis [11] proposed normal values for the AC, ACM, and CE angles. In our study, patients who had an AC angle of less than 15° had a lower OA grading than patients with an AC angle of more than 15°. Distinguishing ACM and CE angles as normal or abnormal did not predict radiographic OA.
Thus, the AC angle depends on the position of the patient yet predicts development of hip OA. Other than the reports of Tönnis [10–12], these correlations have not yet been confirmed in a long-term radiographic study. Tönnis suggested an influence of the lumbar lordosis on the AC angle and Ball and Kommenda [2] introduced an index for determination of pelvic tilt. They concluded the most favorable position is full extension of the hip and neutral rotation of the legs with the knees slightly flexed in a supine position. This position compensates for the lumbar lordosis, but there are no normal values available for this technique. The Kellgren and Lawrence classification [5] is unaffected by the patient’s position on the radiograph. This can be explained by the fact that the score mainly aims at osteophytes that do not differ between standing and supine positions and is less influenced by the joint space width. A higher incidence of radiographic OA in patients with DDH has been previously demonstrated [13]. However, radiographs taken in the supine position cannot be used to evaluate joint space width. An important finding of our study was the AC angle depends on the position of the patient. As expected, the minimum joint space width is influenced by the position, leading to greater values in the supine position. ACM angle and the OA grade according to Kellgren and Lawrence [5] were unaffected by the patient’s position.
It is well known many if not most cases of hip OA are secondary to a developmental deformity [3, 7, 9]. New observations on more or less subtle deformities have resulted in an expanding field of hip preservation surgery in the mature patient [7,9]. The clinician must be aware of the changes in various parameters dependent on whether the radiographs are taken in the supine or weightbearing position. We believe this information of particular importance when planning reorientation procedures of the dysplastic acetabulum.
References
Classic. Translation: Hilgenreiner on congenital hip dislocation. J Pediatr Orthop. 1986;6:202–214.
Ball F, Kommenda K. Sources of error in the roentgen evaluation of the hip in infancy. Ann Radiol. 1968;11:298–303.
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement. A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
Idelberger K, Frank A. A new method for determination of the angle of the pelvic acetabulum in child and in adult [in German]. Z Orthop Ihre Grenzgeb. 1952;82:571–577.
Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16:494–501.
Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792.
Millis M, Kim Y. Rationale of osteotomy and related procedures for hip preservation: a review. Clin Orthop Relat Res. 2002;405:108–121.
Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248.
Siebenrock KA, Schoeninger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286.
Tönnis D. Über Änderungen des Pfannendachwinkels der Hüftgelenke bei Dreh- und Kippstellung des kindlichen Beckens. Z Orthop. 1962;96:462–478.
Tönnis D. Congenital Dysplasia, Dislocation of the Hip in Children and Adults. New York, NY: Springer; 1987.
Tönnis D, Brunken D. Eine Abgrenzung normaler und pathologischer Hüftpfannendachwinkel zur Diagnose der angeborenen Hüft- dysplasie. Arch Orthop Trauma Surg. 1968;64:197–228.
Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–338.
Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76.
Wiberg G. Studies on dysplastic acetebula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;58:83.
Acknowledgments
We thank all patients taking part in this study. Moreover, we thank the staff of the Department of Radiology, University of Iowa, Hospital and Clinics, in particular the xray technicians, for contributing to our study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
About this article
Cite this article
Fuchs-Winkelmann, S., Peterlein, CD., Tibesku, C.O. et al. Comparison of Pelvic Radiographs in Weightbearing and Supine Positions. Clin Orthop Relat Res 466, 809–812 (2008). https://doi.org/10.1007/s11999-008-0124-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0124-8