Abstract
The incidence of obesity and the number of hip arthroplasties being performed in Australia each year are increasing. Although uncommon, periprosthetic infection after surgery can have a devastating effect on patient outcomes. We therefore asked whether obesity correlated with periprosthetic infection after primary hip arthroplasty. We further asked whether variables such as patient comorbidities, operative time, blood transfusions, use of drains, and cementation practices correlated with periprosthetic infection. We hypothesized obesity was an independent risk factor for the development of acute periprosthetic infection after primary hip arthroplasty. We reviewed 1207 consecutive primary hip arthroplasties separating patients into four weight groups, normal, overweight, obese, and morbidly obese, and compared for incidence of periprosthetic infection between the groups. We observed a considerably higher infection rate in obese patients; the correlation was independent of patient comorbidities such as diabetes and cardiovascular disease. We also observed a correlation between infection rates and using a posterior approach in obese patients. The incidence of periprosthetic infection was not influenced by operative time, transfusion requirements, use of drains, and cementation practices. In this series, obesity was an independent risk factor for acute periprosthetic infection after primary hip arthroplasty.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of obesity in Australia is reportedly on the increase, with Australia being ranked high among those with the fattest people. It has been estimated more than 2/3 of the male population (67%) are overweight and 19% are obese, whereas 1/2 of the female population (52%) are overweight and 22% are obese [1]. Obesity has been cited as a risk factor for having osteoarthritis of the hip develop and various studies have shown overweight people are strongly overrepresented among patients undergoing orthopaedic surgery [6, 10, 20, 22, 27].
Independent of the incidence of obesity, the number of THAs being performed in Australia each year also is increasing [2]. Although much has been reported on the improvement in function and quality of life for patients after joint arthroplasty, considerable risks of postoperative complications for patients who are obese also have been reported [8, 17, 19, 23, 24, 26, 36]. However, few studies report the incidence of deep infection in patients who are obese after primary hip arthroplasty. Some studies do suggest a relationship, yet there is also the argument that factors such as coexisting comorbidities are responsible for high incidences of deep infection rather than obesity and studies that have controlled for comorbidities have found no direct correlation between obesity and periprosthetic infection [28–30].
We therefore asked whether there was a correlation between obesity and the incidence of periprosthetic infection. We further asked whether variables such as patient comorbidities, surgical approach, operative time, blood transfusions, use of drains, and cementation practices correlated with periprosthetic infection. We hypothesized obesity was an independent risk factor for the development of acute periprosthetic infection after primary hip arthroplasty.
Materials and Methods
We retrospectively analyzed prospectively collected data for all 1207 patients who underwent primary elective hip arthroplasty from January 1998 to December 2005. Prosthetic joint infections were defined as those with two or more positive deep sample cultures for bacteria or one positive culture with purulence surrounding the joint at operation. All patients who incurred an acute deep infection up to 1 year after hip arthroplasty at our institution were included in the analysis. The median age was 69 years (range, 18–97 years); 673 patients were female and 534 were male. There were 552 left hips and 655 right hips replaced. The median body mass index (BMI) of the group was 28.1 kg/m2 (range, 15.4–52.7 kg/m2). The main reasons for patients undergoing hip arthroplasty were osteoarthritis (n = 999), osteonecrosis (n = 84), rheumatoid arthritis (n = 43), developmental dislocation of the hip (n = 37), and other (n = 44). The major comorbidities were cardiac (n = 736), gastrointestinal (n = 277), respiratory (n = 175), and endocrine (n = 172). Sixty-two percent of patients had multiple comorbidities (two or more). No patients were lost to followup during the first 12 months after their procedure, but there were 13 deaths (0.11%) during the first 12 months after the primary surgery.
Body mass index data were classified according to the US Centers for Disease Control and Prevention (CDC) guidelines [7, 15]. A BMI less than 25 kg/m2 was classified as normal, 25 to 29 kg/m2 as overweight, 30 to 39 kg/m2 as obese, and 40 kg/m2 or greater as morbidly obese. Of the 1207 patients who underwent THA, only 25% (n = 301) were within the normal weight range. Thirty-seven percent (n = 445) of patients were overweight, 34% (n = 417) of patients were obese, and 4% (n = 44) of patients were morbidly obese. Although slightly more men were either overweight or obese than women, the prevalence of morbid obesity was greater for women (5%) than men (2%). Of the 999 patients with osteoarthritis, the median age at the time of surgery (62 years) was younger (p = 0.001) for the morbidly obese group than for all others (obese, 69 years; overweight and normal weight, 71 years). A greater number of patients who were obese and morbidly obese undergoing THA had multiple comorbidities. Fifty-three percent (n = 160) of patients in the normal weight range had two or more comorbidities, 60% (n = 267) in the overweight group, 69% (n = 288) in the obese group, and 70% (n = 31) in the morbidly obese group.
Hip arthroplasty was conducted in a positive-pressure operating room. Patients received perioperative prophylactic antibiotics, which consisted of 1 g intravenous cefazolin on induction and continued for 24 hours postprocedure. Where a preexisting allergy to cephalosporins was identified, prophylaxis was substituted with 1 g vancomycin twice daily for 24 hours with the first dose administered on induction. The dosage and timing of antibiotic prophylaxis were administered as per protocol in all 22 patients diagnosed with deep infection, with one patient of the 22 receiving vancomycin because of an allergy to cephalosporins. All patients had a urinary catheter inserted in the operating room just before surgery, which remained in situ for 48 hours. Gentamicin was given just before insertion and removal of the urinary catheter. Regional anesthesia was used in 1102 cases and general anesthesia in 105 cases. A totally cemented prosthesis was used in 397 patients, cemented stem only (hybrid) in 602 patients, and a totally uncemented prosthesis in 208 patients. Antibiotic-impregnated cement was introduced at our institution in March 2002 and was used in 553 cases. An anterolateral (Hardinge) approach was used in 854 cases, whereas a posterior approach was used in 353 cases. Operative approach was surgeon specific, with each surgeon consistently using the same approach for all primary hip arthroplasties performed during the study period.
Postoperative care for all patients was standardized through the use of our clinical pathway for THA introduced at our institution in 1995. Low-pressure suction drains were used in 1060 patients and remained in situ for 24 to 48 hours. The median postoperative hemoglobin level was 99 g/dL (range, 54–153 g/dL) and 429 patients received an allogenic blood transfusion postoperatively. Autologous blood transfusions were not used during the study time frame.
We reviewed the medical records for all study patients, including inpatient data, discharge summaries, and outpatient followup notes. Data collected included patient demographics, comorbidities, operative time, length of stay, discharge destination, complications, and readmissions that occurred within the first 12 months of the index surgery. Once data collection was complete, patients were separated into one of four groups according to their preoperative BMI classification as described previously.
The differences in infection rates between categorical groups were determined using the chi square test and nonparametric continuous data were analyzed using the Mann-Whitney and the Kruskal-Wallis one-way analysis of variance on ranks. We determined whether diabetes and cardiac disease, two comorbidities commonly linked with obesity, were associated with an increased risk of periprosthetic infection. We then determined whether the operative approach influenced infection for the four weight groups. Data were maintained and analyzed using Microsoft® Excel® (Microsoft Corp, Redmond, WA) and SigmaStat® for Windows Version 3.0.1 (SPSS Inc, Chicago, IL).
Results
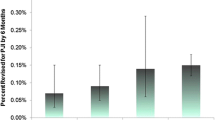
We observed a periprosthetic infection rate of 1.8%. When separated by BMI, the infection rate was higher (p = 0.002) in obese patients: 1.0% (n = 3) of patients within the normal weight range and 0.9% (n = 4) of overweight patients had an acute prosthetic infection develop after primary hip arthroplasty, compared with 2.6% (n = 11) of obese patients and 9.1% (n = 4) of morbidly obese patients.
No particular comorbidity correlated with an increased incidence of periprosthetic infection (Table 1). The incidence of infection tended to be higher (p = 0.15) for patients with diabetes (3.9%) than for patients without diabetes (1.6%). In contrast, the periprosthetic infection rate was higher (p = 0.002) in obese groups when patients without diabetes were separated by BMI (Table 2): the infection rates in patients without diabetes were 1.1% (n = 3) and 0.5% (n = 2) in normal and overweight patients, compared with 2.6% (n = 9) and 8.6% (n = 3) in obese and morbidly obese patients. Patients without cardiac disease also had a higher (p = 0.024) incidence of periprosthetic infection among obese groups than among nonobese groups (Table 3): the infection rates for this subgroup occurred in 1.0% (n = 2) and 0.0% (n = 0) of normal and overweight patients, compared with 3.6% (n = 4) and 8.3% (n = 1) in obese and morbidly obese patients.
The incidence of periprosthetic infection was greater (p = 0.001) in obese groups than in nonobese groups when a posterior approach was used; however, this difference was not evident when an anterolateral (Hardinge) approach was used (Tables 4, 5). The rate of infection for patients when a posterior approach was used was 0% (n = 0) and 0.8% (n = 1) for normal and overweight patients, compared with 2.5% (n = 3) and 18.8%% (n = 3) in obese and morbidly obese patients.
Median operative time (skin to skin) was longer (p = 0.013) for patients who were morbidly obese than for patients in the other three groups: median operative time was 100 minutes (range, 45–195 minutes) for patients in the normal weight range, 105 minutes (range, 40–290 minutes) for patients who were overweight and obese, and 120 minutes (range, 55–180 minutes) for patients who were morbidly obese. However, there was no difference (p = 0.23) in operative time for patients without and with periprosthetic infection (Table 1): the median procedure time was 112 minutes (range, 50–190 minutes) for the 22 patients who had infection develop and 105 minutes (range, 50–295 minutes) for patients who did not have infection develop.
We observed a similar (p = 0.93) infection rate between patients with and without the use of a postoperative drain (Table 1): the infection rate in patients with a drain was 1.9% (n = 20), compared with 1.4% (n = 2) without a drain. The periprosthetic infection rate was similar (p = 0.23) for patients who had a postoperative blood transfusion (2.6%; n = 11) and patients who did not (1.4%; n = 11) (Table 1).
The incidence of periprosthetic infection was not different for cemented and uncemented prostheses (Table 1). The infection rate for a totally cemented prosthesis or hybrid was 2.0% (n = 20), compared with 1.0% (n = 2) for a totally uncemented prosthesis (p = 0.46). The rate of infection in those cases in which antibiotic-impregnated cement was used was 1.6% (n = 9), compared with 2.5% (n = 11) of cases in which cement was not impregnated with antibiotics (p = 0.48).
Discussion
Substantial improvements in function and quality of life for patients after joint arthroplasty have been reported but considerable risk for complications for patients who are obese also has been reported [8, 17, 19, 23, 24, 26, 36]. Few studies report specifically on the incidence of acute periprosthetic infection for obese patients after primary hip arthroplasty and even fewer have controlled for comorbidities [28–30]. The aim of this study was to determine if obesity was an independent risk factor for periprosthetic infection and to analyze the patient and surgical variables that have been reported to correlate with infection.
Our study has several limitations. This was a retrospective analysis of prospectively collected data. Although postoperative care of patients was standardized through clinical pathway protocols, some differences in surgical technique were identified; namely, preference for surgical approach and use of drains differed among surgeons. However, each surgeon’s practice was consistent throughout the study period and not influenced by individual patient characteristics. We analyzed these variables and found no relationship with infection rates and therefore believe these variables did not detract from our finding that obesity as an independent risk factor for acute periprosthetic infection after primary hip arthroplasty.
Our major finding was a considerably higher incidence of acute periprosthetic infection after primary hip arthroplasty in obese and morbidly obese patients compared with nonobese patients. Of the few existing reports in the current literature, there is argument for and against a correlation between obesity and the incidence of infection [16, 28, 29, 33]. In a recent study of considerable size, an initial association between BMI and infection after THA was reported. However, by using regression analysis and separating out coexisting conditions such as diabetes mellitus, obesity was no longer an independent predictor of infection after hip arthroplasty [29]. Only nine of 800 patients in that study were morbidly obese and the power of the study may be too low to give a precise estimate of the effect of BMI on the risk of rare complications. In contrast, a study of similar size reported a higher infection rate after hip arthroplasty in patients who were “highly obese” (BMI ≥ 35 kg/m2) than in patients who were “non-highly obese” (BMI < 35 kg/m2), with an odds ratio of 4.2 [30]. Although a higher incidence of diabetes mellitus in patients who were highly obese also was reported in the same study, only one of the five patients with infection had diabetes and this patient was in the nonhighly obese group. Our study concurs with these findings. When we compared periprosthetic infection rates in patients without diabetes mellitus or cardiovascular disease, we still observed a higher infection rate in obese patient groups than in nonobese groups. We also were able to report on a much larger cohort of morbidly obese patients.
We also observed the periprosthetic rate was considerably higher in patients who were obese and morbidly obese than in patients who were nonobese when surgery was performed through a posterior approach. This difference was not evident when a Hardinge approach was used. Reports of infectious complications related to the surgical approach are limited. A recent Cochrane review of complications related to surgical approach could identify only four prospective cohort studies related to this relationship [21]. These, however, have not indicated a predisposition to infection when either the posterior or Hardinge approach was used [3, 4, 11, 38].
Operative time took considerably longer for the morbidly obese group than for all other weight groups. According to the CDC guidelines for the prevention of surgical site infection, an operative time greater than 2 hours is considered a risk factor for surgical site infection in hip arthroplasty [25]. Prolonged procedure time has been reported as an independent risk factor for surgical site infection [13, 14, 20, 31, 34]. However, we found no difference in the median operative times for patients who had a deep infection develop and for those who did not.
We observed no difference in the periprosthetic infection rates for patients who received an allogenic blood transfusion after surgery and for patients who did not receive a transfusion. It has been reported the transfusion of allogenic blood in patients undergoing joint arthroplasty increases the risk of complications, including infection [5, 32]. In a recent paper, it was reported transfusion of allogenic blood increased the risk of a deep-seated infection by a factor of 12 for patients undergoing primary hip or knee arthroplasty [35]. However, this paper cites a review by Innerhofer et al. [18] who compared the postoperative risk of infection after primary arthroplasty for patients who had allogenic and autologous blood transfusions. Closer inspection reveals, while there was a 12-fold increased risk of infection in patients who had allogenic blood transfusions after joint arthroplasty, these infections included wound, urinary tract, and chest infections. No reference was made to deep-seated infections.
We found no difference in the periprosthetic infection rate of patients with or without the use of a postoperative drain. Although the use of a surgical drain was governed by surgeon preference in our study, the protocol for the removal of drain tubes was consistent. A large randomized controlled trial of the use of drains in THA also concluded there was no difference in deep infection rates with or without the use of drains [37].
The use of cemented prostheses has been associated with an increased incidence of deep infection in primary hip arthroplasty compared with totally uncemented prostheses when using revision as the end point; however, the difference is not evident when antibiotic-impregnated cement is used [12]. Although we are reporing on only the first 12 months after index surgery, when we compared the incidence of acute periprosthetic infection in uncemented hip arthroplasties with hybrid and fully cemented arthroplasties, we found no difference in the infection rates between the groups. Nor did we observe a difference in the infection rate for a cemented prosthesis regardless whether the cement was impregnated with antibiotics.
Deep infection after hip arthroplasty remains one of the most challenging and difficult orthopaedic complications in terms of prevention and treatment. Although successful eradication or suppression of infection has been achieved in a majority of cases at our institution [9], treatment is not without substantial cost to patients, caregivers, and the healthcare system. As such, establishing risk factors for periprosthetic infection is of paramount importance. Our study shows obesity is a risk factor for acute periprosthetic infection after primary hip arthroplasty. We further establish the risk was independent of patient comorbidities such as diabetes and cardiovascular disease. Higher infection rates were seen for patients who underwent surgery using a posterior approach in particular. The incidence of periprosthetic infection was not influenced by operative time, transfusion requirements, use of drains, and cementation practices.
References
Australian Bureau of Statistics. National Health Survey 2004–05; Summary of results. Available at: http://www.health.gov.au/internet/wcms/publishing.nsf/content/health-pubhlth-strateg-hlthwt-obesity.htm, 2006. Accessed on 15 December 2005.
Australian Orthopaedic Association. National Joint Replacement Registry Annual Report. Hip and knee replacement from September 1999 to December 2003. Adelaide: AOA. Available at: http://www.dmac.adelaide.edu.au/aoanjrr/publications.jsp. Accessed on 21 August 2006.
Baker AS, Bitounis VC. Abductor function after total hip replacement: an electromyographic and clinical review. J Bone Joint Surg Br. 1989;71:47–50.
Barber TC, Roger DJ, Goodman SB, Schurman DJ. Early outcome of total hip arthroplasty using the direct lateral vs the posterior surgical approach. Orthopedics. 1996;19:873–875.
Borghi B, Casati A. Incidence and risk factors for allogenic blood transfusion during major joint replacement using an integrated autotransfusion regimen. The Rizzoli Study Group on Orthopaedic Anaesthesia. Eur J Anaesthesiol. 2000;17:411–417.
Böstman OM. Prevalence of obesity among patients admitted for elective orthopaedic surgery. Int J Obes Relat Metab Disord. 1994;18:709–713.
Centers for Disease Control and Prevention. National Center for Health Statistics; BMI—Body Mass Index for Adults. Available at: http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-adult.htm. Accessed on 14 December 2005.
Chan CL, Villar RN. Obesity and quality of life after primary hip arthroplasty. J Bone Joint Surg Br. 1996;78:78–81.
Choong PF, Dowsey MM, Carr D, Daffy J, Stanley P. Risk factors associated with acute hip prosthetic joint infections and outcome of treatment with rifampin-based regimen. Acta Orthop, in press.
Cooper C, Inskip H, Croft P, Campbell L, Smith G, McLaren M, Coggon D. Individual risk factors for hip osteoarthritis: obesity, hip injury, and physical activity. Am J Epidemiol. 1998;147:516–522.
Downing ND, Clark DI, Hutchinson JW, Colclough K, Howard PW. Hip abductor strength following total hip arthroplasty: a prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand. 2001;72:215–220.
Engesaeter LB, Espehaug B, Lie SA, Furnes O, Havelin LI. Does cement increase the risk of infection in primary total hip arthroplasty? Revision rates in 56,275 cemented and uncemented primary THAs followed for 0–16 years in the Norwegian Arthroplasty Register. Acta Orthop. 2006;77:351–358.
Fitzgerald RH Jr, Nolan DR, Ilstrup DM, Van Scoy RE, Washington JA 2nd, Coventry MB. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977;59:847–855.
Garibaldi RA, Cushing D, Lerer T. Risk factors for postoperative infection. Am J Med. 1991;91:158S–163S.
Garrow JS, Webster J. Quetelet’s index (W/H2) as a measure of fatness. Int J Obes. 1985;9:147–153.
Horan F. Obesity and joint replacement. J Bone Joint Surg Br. 2006;88:1269–1271.
Ilstrup DM, Nolan DR, Beckenbaugh RD, Coventry MB. Factors influencing the results in 2,012 total hip arthroplasties. Clin Orthop Relat Res. 1973;95:250–262.
Innerhofer P, Klingler A, Klimmer C, Fries D, Nussbaumer W. Risk for postoperative infection after transfusion of white blood cell-filtered allogeneic or autologous blood components in orthopedic patients undergoing primary arthroplasty. Transfusion. 2005;45:103–110.
Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005;435:232–238.
Jain SA, Roach RT, Travlos J. Changes in body mass index following primary elective total hip arthroplasty: correlation with outcome at 2 years. Acta Orthop Belg. 2003;69:421–425.
Jolles BM, Bogoch ER. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev. 2006;3:CD003828.
Karlson EW, Mandl LA, Aweh GN, Sangha O, Liang MH, Grodstein F. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am J Med. 2003;114:93–98.
Knutsson S, Engberg IB. An evaluation of patients’ quality of life before, 6 weeks and 6 months after total hip replacement surgery. J Adv Nurs. 1999;30:1349–1359.
Lehman DE, Capello WN, Feinberg JR. Total hip arthroplasty without cement in obese patients: a minimum two-year clinical and radiographic follow-up study. J Bone Joint Surg Am. 1994;76:854–862.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278; quiz 279–280.
Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552–560; discussion 555A.
Marks R, Allegrante JP. Body mass indices in patients with disabling hip osteoarthritis. Arthritis Res. 2002;4:112–116.
McLaughlin JR, Lee KR. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg Br. 2006;88:1286–1292.
Moran M, Walmsley P, Gray A, Brenkel IJ. Does body mass index affect the early outcome of primary total hip arthroplasty? J Arthroplasty. 2005;20:866–869.
Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty. 2005;20(7 suppl 3):46–50.
Proietto J, Baur LA. 10: Management of obesity. Med J Aust. 2004;180:474–480.
Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43:459–469.
Sadr Azodi O, Bellocco R, Eriksson K, Adami J. The impact of tobacco use and body mass index on the length of stay in hospital and the risk of post-operative complications among patients undergoing total hip replacement. J Bone Joint Surg Br. 2006;88:1316–1320.
Saleh K, Olson M, Resig S, Bershadsky B, Kuskowski M, Gioe T, Robinson H, Schmidt R, McElfresh E. Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res. 2002;20:506–515.
Sitges-Serra A, Insenser JJ, Membrilla E. Blood transfusions and postoperative infections in patients undergoing elective surgery. Surg Infect (Larchmt). 2006;7(suppl 2):S33–S35.
Stickles B, Phillips L, Brox WT, Owens B, Lanzer WL. Defining the relationship between obesity and total joint arthroplasty. Obes Res. 2001;9:219–223.
Walmsley PJ, Kelly MB, Hill RM, Brenkel I. A prospective, randomised, controlled trial of the use of drains in total hip arthroplasty. J Bone Joint Surg Br. 2005;87:1397–1401.
Weale AE, Newman P, Ferguson IT, Bannister GC. Nerve injury after posterior and direct lateral approaches for hip replacement: a clinical and electrophysiological study. J Bone Joint Surg Br. 1996;78:899–902.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
About this article
Cite this article
Dowsey, M.M., Choong, P.F.M. Obesity is a Major Risk Factor for Prosthetic Infection after Primary Hip Arthroplasty. Clin Orthop Relat Res 466, 153–158 (2008). https://doi.org/10.1007/s11999-007-0016-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-007-0016-3