Abstract
Research is an integral part of evidence-based practice in the emergency department and critical care unit that improves patient management. It is important to understand the need and major obstacles for conducting research in emergency settings. Herein, we review the literature for the obligations, ethics and major implications of emergency research and the associated limiting factors influencing research activities in critical care and emergency settings. We reviewed research engines such as PubMed, MEDLINE, and EMBASE for the last two decades using the key words “emergency department”, “critical care”, “research”, “consent”, and “ethics” as the search terms. Research within emergency settings is slow or non-existent due to time and financial constraints as well as the lack of a research tradition. There are several barriers to conducting research studies in emergency situations such as who, what, when, and how to obtain patient consent. The emergency environment is highly pressurized, emotional, and overburdened. The time taken for research is a particular risk that could delay the desired immediate interventions. Ethical issues abound, particularly relating to informed consent. Research in emergency settings is still in its infancy. Thus, there is a strong need for extensive research in the emergency setting through community awareness, resource management, ethics, collaborations, capacity building, and the development of a research interest for the improvement of patient care and outcomes. We need to establish a well-structured plan to assess and track the decision-making capacity, consider a multistep enrolment and consent strategy, and develop an integrated approach for recruitment into studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the years, emergency services have been improved to deliver a better quality of care for critically ill patients through evidence-based medicine (Bion and Heffner 2004; Wright et al. 2005). Research activities in emergency settings have demonstrated substantial benefits for improving patient care and management. However, there are several obstacles to conducting proper research in emergency settings (Good and Driscoll 2002). For instance, despite the huge burden of traumatic injuries, community-based research in trauma and critical care is disproportionately low (Roberts et al. 2005). For sustainable injury prevention, trauma research should be supplemented with an efficient trauma audit process and an appropriate trauma quality management system (Eid et al. 2008). Data analysis with real-time documentation is extremely important for improving the clinical database system in emergency settings (Rhodes and Pollock 2006). Implementation of research strategies in emergency and trauma settings is the key to inform injury prevention strategy. Therefore, advanced research studies focusing on the patient flow, resources, capability, and capacity of the emergency department (ED) are needed. Research analyses focusing on EDs would help in the advanced life-saving technologies and procedures and assist in the preparation for large-scale disaster management. Medical research in emergency medicine is widely recognized for identifying potential risk factors and it additionally helps in maintaining appropriate clinical care (Madden and Cole 1995). Introducing newer drugs into clinical practice needs thorough assessment of safety and efficacy using research methodologies. However, conducting this kind of research is still under ethical regulation and hospital resources. Herein, we reviewed the literature for the obligations, ethics and major implications of emergency research and the associated limiting factors influencing research activities in critical care and emergency settings. We sought to investigate whether there is a need for research in an emergency setting, what the areas that require particular focus are and what else could be done to overcome research dilemmas under critical situations.
Methods and Results
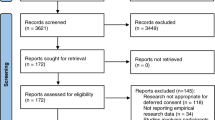
A traditional narrative review was undertaken utilizing research engines such as PubMed, MEDLINE, and EMBASE over the last two decades (January 1991 to December 2014) using the key word search terms “emergency”, “critical care”, “research”, “consent”, and “ethics”. Medical Subject Headings (MeSH) terms used were critical care” [MeSH Terms] OR (“critical” [All Fields] AND “care” [All Fields]) OR “critical care” [All Fields]) AND (“research” [MeSH Terms] OR “research” [All Fields])) AND (“ethics” [Subheading] OR “ethics” [All Fields] OR “ethics” [MeSH Terms].
The initial search yielded 1613 articles which were reviewed independently. All abstracts were reviewed to select articles related to emergency research including ED, and ICU settings, critical care, implications of consent in emergency situation and human subject’s ethics. Articles written in English which are available in electronic databases and specific institutional sites were included. After thorough screening, a total of 59 relevant articles were included and reviewed. However, non-emergency research articles, studies that are not relevant to the main topic, abstracts, unpublished data and non-English articles were excluded. Emergency research is defined as “planned research involving human subjects who have a life-threatening medical condition that necessitates urgent intervention (for which available treatments are unproven or unsatisfactory), and who, because of their condition (such as traumatic brain injury) cannot provide informed consent” (Mayo Clinic 2015). The targeted field of this kind of research includes prehospital, ED, and ICU settings. The non-urgent emergency condition typically deals with the situation in which a delay of an initial 24 h would not increase the likelihood of an adverse outcome (Uscher-Pines et al. 2013). Emergency situation is defined as an acute situation that may pose the risk of permanent injury, loss of function, or death.
Discussion
Research in emergency settings is usually slow or non-existent due to time and financial constraints as well as to the lack of a research tradition (Good and Driscoll 2002). Does research in the emergency setting need specific or special procedures? For instance, should physicians attending unconscious patients in the emergency room or injured patients in the trauma room follow specific standard operating procedures (SOPs)? There is a potential to develop tailored individualized SOPs in different EDs which particularly focus on different patient populations (Kortgen et al. 2006; Sathyanarayana Rao et al. 2011). SOPs also reduce the time delay between the results dissemination of clinical trials and the inclusion of significant trial findings into routine clinical practice. Generally, SOPs affirm that all research conducted within the study site abide the federal regulations, ICH GCP and institutional policies to protect the rights and welfare of the participants. Moreover, SOPs provide autonomy, improve the quality of collected data and science of the study, and serve as a reference and guideline on how research will be conducted. All ongoing SOPs should be reviewed at regular intervals to reassess the applicability of the policy (Association of clinical research professionals 2015; Standard Operating Procedures 2014).
Barriers to Conducting Research in Emergency Settings
There are several barriers for conducting research studies in emergency situations. One of the major limiting factors is the surrounding conditions which are highly pressured, the need for immediate action, the family emotional situation, and so the physicians involved are often over-burdened for research (Good and Driscoll 2002). The availability of limited resources, lack of institutional support, and ethical barriers are major challenges for conducting research in these settings (Runyon et al. 2013). For instance; obtaining an informed consent (ethical obligation) from an acute myocardial infarction (AMI) patient in the emergency and ICU remains a primary concern in developing research-based diagnostics and risk stratification. A lack of competency (due to severe pain, opiates, anxiety with fear of death, and circulatory hypoperfusion), together with the failure of the process of disclosure (poor communication by physicians and an educational mismatch between the patients and information provider) remain the primary factors limiting the consent process for research in AMI patients (Williams et al. 2003). Yuval et al. (2000) assessed the prospects of a subgroup of AMI patients who signed an informed consent form in the ISIS-4 trial. The comprehension of the trial was reported as full (31 %), partial (50 %), and no understanding (19 %) of the consent content (Yuval et al. 2000). Comprehensions were related to the time spent for explanation rather than the personnel or type of consent. Consent was given by 55 % of the patients in the hopes of receiving better treatment and follow-up, whereas 14 % gave no clear reason, and 8 % were afraid to refuse to participate in the study.
The lack of research experience by emergency physicians limits their competencies in addressing critical issues. In addition, researchers involved in emergency medicine reported a lack of resources, infrastructure support, and collaboration as the other significant constraints on research (Canadian Association of Emergency Physicians 2002). Further, challenges in emergency care research that need more attention include the management of hospital resources (i.e., beds and staff) and accurate diagnosis for effective and timely intervention (Canadian Association of Emergency Physicians 2002). Researchers have identified the overutilization of EDs, particularly for non-emergency cases that results from frequent ED visits (Richardson and Hwang 2001). Overcrowding in an ED leads to worse medical outcomes (increased post-admission mortality) and sub-optimal patient care (higher complication rates, e.g. infections) (Pines et al. 2006; Sprivulis et al. 2006).
Ethical Issues in Conducting Emergency Research
Barriers to informed consent for research purposes in emergency settings are unique when the time frame for research and the vulnerability of the patients are considered (Schmidt et al. 2004). The comprehension and satisfaction with the informed-consent process are markedly lower among patients with lower educational levels (Breese et al. 2007). According to the HERO-2 study which evaluated the readability of patient information sheets, educational status of subjects, perception of the consent process, and level of comprehension of information to give consent. The authors observed that the patients have less suitability to provide consent based on level of comprehension. Of the 22 % (75/345) educated subjects, only 63 read the information sheet prior to their decision to provide or refuse consent (Williams et al. 2003). This finding demonstrates an important obstacle to deliver the appropriate consent information. In another study, the important factors found to affect patient understanding of consent details included pain, level of education, and gender (Hilden and Gammelgaard 2002). Recently, Kulkarni et al. (2014) addressed the role of audio–video recordings while conducting the informed consent process. The authors believed that this process would reassure authorities and the community about the standards maintained by the industry in obtaining proper consent and increase society’s faith in clinical research. However, the privacy and costs of this tool are of great concern.
Patients in the ED are usually admitted in an unconscious state and require urgent medical intervention to survive. For recruiting such patients in a research study, informed consent is the primary requirement, and it demands the delivery of succinct and sufficient information about potential risks and benefits of participation. However, most of the time in emergency settings, it is not feasible to obtain informed consent from the patients or legally authorized representatives for enrolment in a study.
Emergency research is applicable to subjects who have acute, serious, and life-threatening conditions needing urgent medical intervention within a stipulated time frame. There may be an unacceptable risk of fatality associated with delayed intervention for seeking the patient’s consent. Thus, patient condition and the effect of the time required obtaining consent from the patient or family members are the basic principles to guide the conduct of research in emergency settings. Moreover, it has been regarded as necessary to analyse the situations in which emergency research would be acceptable, and this needs to be prioritized (Adams and Wegener 1999). Hirshon et al. (2013) reviewed the implications of ethical conduct and associated complexities in acute care research in global settings. The authors identified a global need for ethical conduct of research involving human subjects. Nevertheless, there is a specific need for developing regional knowledge and competence to ensure the ethical conduct of acute care research according to the specific socio-cultural norms. Although emergency research is privileged, with special provisions of exemption for informed consent, the research protocol and ways in which waivers of consent are reported must be assessed by an independent regulatory body (Adams and Wegener 1999). Furthermore, ED patients represent a vulnerable population that needs special efforts for enrolment to ensure their autonomy and understanding of the purposes and risks of participation (Halila 2007). A misunderstanding of the randomization process in a trial, believing that the physician can place them in the most beneficial study arm, is a common phenomenon among ICU patients (Donatelli et al. 2006). This is often referred to as therapeutic misconception.
With the increased involvement of the public in health care decisions, there is a strong debate on the issue of a waiver of informed consent for research in emergency settings. A lack of consent clearly signifies unethical practices and the loss of individual autonomy in research (Kaufman 1997). The major concern for waiving informed consent is that it compromises the willingness of individuals to participate in a study. However, if a patient is unable to consent, the ethical implications of conducting research with the highest ethical standards could be attained by communicating with the community, family members, and relatives of the patient about the potential risks and benefits of the study if and only if they are available at the scene at the time (Quest and Marco 2003).
The proposed draft of the Declaration of Helsinki permits (Article 24) the introduction of a waiver of informed consent for critically ill patients “when the research involves only slight risk or when the procedures to be used are customarily used in the practice of medicine without documentation of consent” which provoked controversy (Medical Ethics Committee of the World Medical Association 1999). In the US, emergency research regulations were approved by the Department of Health and Human Services (DHHS) to allow research in emergency settings with a waiver of informed consent (Food and Drug Administration 2013). These are the guidelines for conducting emergency research under a waiver of informed consent to safeguard against unethical research conduct. Currently, in various countries such as the US, EU member states, Canada, and Australia, there are provisions for the research without informed consent in emergency situations (Lecouturier et al. 2008). In addition, European nations such as Austria, Belgium, France, Netherlands, Germany, and Spain have their own national legislation for emergency research (Lemaire et al. 2005). In the UK, an amendment has been made to the European Union Clinical Trials Directive (2006) to allow research without consent in emergency situations through approval from ethics committees (Department of Health, United Kingdom 2006). In the US, post-implementation of the regulations for exception from informed consent (EFIC) using community consultation demonstrated high levels of satisfaction and trust in physician-investigators as indicated by surveys (Govindarajan et al. 2013).
Could the research in emergency settings be excused from obtaining informed consent due to a restricted therapeutic time frame and need for urgent intervention? The answer remains debatable. Almost half of the European Union member states accept the deferred consent (patient and/or proxy) for conducting clinical research in the acute emergency settings (Kompanje et al.2014).
Liddell et al. (2006) highlighted the European medico-legal aspects of the Clinical Trials Directive (Directive 2001/20/EC) implemented for protection of incapacitated individuals. They observed a serious problem with Article 5(a) that necessitates written consent to be taken from a legal representative on every occasion before interacting with incapacitated adults for a research purpose. According to Gamble et al. (2013) the European Clinical Trials Directive (2001/20/EC) provided no directions for obtaining consent in emergency settings, compelling member states to either work in deviation from the directive or to accept restraints on emergency care research. Recently, the European Parliament proposed a regulation that will replace Directive 2001/20/EC which incorporates a provision for deferred consent that permits the delivery of information and obtaining informed consent, even after the initiation of the trial, providing the minimal risk and minimal burden criterion should be fulfilled. However, two of these criteria are conflicting. First, owing to the urgency of the situation (sudden life-threatening conditions), it is impossible to supply information and obtain informed consent prior to inclusion in the study. Second is the non-availability of a legal representative (Gamble et al. 2013). Moreover, the new EU Clinical Trial Regulation adopted on the 16th April 2014 (Regulation (EU) No 536/2014) will come into effect no sooner than 28th May 2016 (Petrini 2014).
Exceptions to the Informed Consent Requirement
Studies in emergency research usually involve the most vulnerable population, who are unable to provide informed consent. Such emergency conditions require prompt action and generally provide insufficient time and opportunity to locate and obtain consent from the subject’s legally authorized representative. Therefore, an exemption to informed consent is needed under these conditions. The impracticality and emergency setting of the research are the two usual exceptions to the requirement of informed consent.
The impracticality permits conducting research with an exception for informed consent under criteria that allow for only minimal risk, the waiver of consent not adversely affecting the rights and welfare of the study subjects, the research not being able to be practically performed without a waiver, and the subjects being provided with additional information afterwards (Daugherty and White 2010). Figure 1 summarizes the exception from informed consent requirements for emergency care research (Halperin et al. 2007). Similarly, to perform emergency research using a waiver of consent, several conditions should be fulfilled (Tables 1, 2) (Daugherty and White 2010; Jacobs et al. 2011; Jansen et al. 2007; Ogilvie et al. 2011).
Although, it was the first randomized placebo-controlled trial of adrenaline in cardiac arrest versus placebo in humans, waiver of consent was given as shown in the Jacobs et al. study (2011). Similarly, Ogilvie et al. (2011) performed the first and largest trial to investigate the reliability of bispectral index (BIS) versus clinical judgment for estimating sedation level in mechanically ventilated trauma patients using a waiver of informed consent. Annane et al. (2004) highlighted the impact of introducing waiver consent for sepsis patients. The authors reported the enrollment rate of 4 subjects per month with informed consent which escalates to 10 patients per month after approval for waiver consent. In addition, only few subjects (3 %) were able to provide informed consent, 23 % of the subjects included using informed consent obtained from the patient’s next of kin whereas, a majority (74 %) of the subjects were enrolled using deferred consent.
Deferred Consent
Deferred consent is defined as randomization at the investigator’s discretion according to criteria that have been clearly explained during an ethical review of the protocol, followed by a request for the patient’s (deferred subject) or representative’s (deferred proxy) informed consent during a later phase (Jansen et al. 2007).
There are various emergency clinical trials that have utilized deferred consent. Table 2 represents various studies utilizing deferred and waiver of informed consent in emergency settings (Jacobs et al. 2011; Ogilvie et al. 2011; Annane et al. 2004; Jansen et al. 2007; Annane et al. 2000; Harvey et al. 2006; Marshall et al. 1998; Harvey et al. 2005; Maitland et al. 2011; Young et al. 1996). Few investigators advocated the use of data in the case of patient death without signing the deferred consent; provided that all possible efforts have been attempted in a timely manner within an explicit predetermined period in the submitted study protocol to obtain permission from patient’s next of kin (time limit of 72 h or use an independent physician) (Jansen et al. 2009). However, serious concerns have been raised by the regulatory authorities regarding the ethical conduct of a trial in which the unproven “standard of care” has been investigated by some trial. Rivers et al. (2001) collected data for 111 patients with severe sepsis or shock; of these, deferred consent was obtained in 92 patients, whereas 13 died before consent was asked for, 3 refused consent, and in 3 cases, the relatives were not available. The ethics committee did not allow the use of the already obtained data from the patients who died before consent could be sought. In a second scenario, Harvey et al. (2005) used deferred consent from patients who regained consciousness, regardless of whether assent from a relative was obtained earlier. Another study reported the inclusion of patient data in the trial investigation, even though the patient died without recovering consciousness (Jansen et al. 2007). Data were not used for patients who died either with assent obtained from a relative or who had neither a relative’s assent nor a subject-deferred consent. In a fourth scenario, the majority of patients were included using deferred consent (Annane et al. 2004) and consent was sought as early as possible. This study was mainly performed among the survivors, but reported the use of data even if the patients died before regaining mental capacity. Moreover, attributing it to higher 1-month deaths, a considerable amount of information was evaluated without consent. Young et al. (1996) demonstrated persistent efforts to contact the patients’ relatives and reported the consultation of an independent physician prior to declaring the need for a waiver of consent. In this case, relatives could not be contacted by any means or the patient died before contacting the relatives. Under such circumstances, the institutional review board (IRB) was informed, and the data were used for the analysis.
Jansen et al. (2009) described the real ethical arguments pertinent in real emergency research. The authors advocated the use of deferred proxy consent in place of informed patient consent under emergency situations. However, they described two obstacles i.e. validity and practical feasibility of deferred proxy consent. The first concern was the validity of judgment for providing deferred consent or refusal under such situations and the other issue was the feasibility to use already obtained data before approaching proxies for deferred consent in the case of death of the patient. The authors suggested approaching the patient’s relatives to obtain consent after explaining the study provided, if it is ethically valid to do so. In another study, Jansen et al. (2010) focused on the validity of clinical trial findings under circumstances where deferred consent was not possible due to early mortality. The authors identified a lower statistical power; selection bias, asymmetric randomization, and reduced external validity of the trial findings after excluding patients without having obtained deferred consent. They concluded that it is unethical not to use data from subjects with completed study procedures or in which deferred consent was not obtained.
Kompanje et al. (2007) discussed the effect of prior written proxy consent on delayed therapeutic time-frames in acute severe traumatic brain injury patients. The authors recommended the use of deferred consent which significantly reduced the initial time for the study of drug administration and considered it ethically justifiable in an emergency situation.
In a recent multicentre study, Offerman et al. (2013) recruited patients at the ED, and none of them were informed about the study during their recruitment. The investigators contacted the patients or their legally designated surrogates through the telephone 2 weeks post-discharge to obtain consent for their study participation after providing all the components of informed consent. The authors concluded that a deferred telephone contact for obtaining consent is a competent process with effective perception by both the subjects and surrogates. They also advocated taking permission for deferred telephone consent from IRBs in minimal-risk studies that need a telephone follow-up. Woolfall et al. (2014) found that most of the subjects who represented patients were unfamiliar with deferred consent, but responded positively to a general description of the method. Trust in practitioners for their capability in making research-related decisions is an important factor associated with positive responses.
Maitland et al. (2011) discussed the approach and suitability for obtaining research consent involving severely sick children who remained under-represented in research as the present regulations are challenging for acute care researchers. The authors utilized a modified form of deferred consent which was based on verbal assent from guardians during initial recruitment followed by obtaining complete written consent post-stabilization of the child’s condition. There is a need to evaluate the perception of key stakeholders of the acceptability and appropriateness of deferred consent.
Figure 2 shows the ethical principles for conducting medical research and the role of consent. Table 3 summarizes the conditions for using deferred consent and the exception for informed consent from different continents (Africa, Europe, and USA) (Andra le Roux-Kemp 2014).
Deferred Consent from the Bereaved Relatives of Deceased Patients
The availability of consent should be respected as thoroughly as possible, but certain points should also be considered, as proposed by Jansen and colleagues (Table 1) (Jansen et al. 2007).
In their study, Maitland et al. (2011) decided not to approach parents for retrospective consent in the case of early death before obtaining full informed consent. The reasons for that were mainly supported by 3 explanations: (a) assent has already been obtained from the parents and so further trial information could be provided to them if they are keen to know and discuss after the death of the recruited child; (b) undergoing the complete process of consent might impose guilt on parents for providing acceptance to participate in research and it is challenging to convince them about expected fatal outcome of severe illness retrospectively: (c) it is the obligation of trial team and ethics review committees to ensure the prospect of maximum benefit and minimal risk for such a trial through appropriate selection of potential subjects not with parents.
Multi-step Enrolment and Consent Strategy
Richmond and Ulrich (2007) suggested four recommendations to facilitate the enrolment of patients into critical care studies:
-
1.
Establish a structured plan to assess and track decision-making capacity.
-
2.
Develop a consent process that is commensurate with the study risk.
-
3.
Consider a multistep enrolment and consent strategy.
-
4.
Develop an integrated approach to recruit subjects into the studies.
Moreover, Richmond used a 3-step process to obtain consent in one of his injury studies
-
1.
Verbal consent to obtain simple baseline data while the patients were in the ED and permission to release the patient’s name to the research team.
-
2.
A random selection of subjects from the entire pool of potential candidates who had been identified by the enrollers (a written informed or a verbal consent depending on the patient disposition).
-
3.
An in-person meeting, where written consent was obtained.
FDA Regulations (21 CFR 50.24) for a Waiver of Informed Consent in Emergency Care Research
For the improvement of outcomes in patients with life-threatening medical conditions, the Federal Food, Drug, and Cosmetic Act permits a waiver of consent to provide potential treatments or an improvement in treatment in cases where the current treatment is unproven or unsatisfactory. Under these circumstances, the responsibilities of the sponsors, clinical investigators, and IRBs involve (a) a consultation with community representatives where the research will be undertaken; (b) information to be disclosed at a public platform prior to the initiation and completion of the study; (c) the thoroughness of the investigator to contact the legally authorized representatives; and (d) study oversight by an independent data monitoring committee (Food and Drug Administration 2013).
According to 21 CFR 50.24(a)(4), any study that cannot be conducted without a waiver of informed consent is permitted under two circumstances. First, the results obtained from consenting subjects could not be generalized to subjects who are unable to provide consent (i.e., in coma). It is noteworthy that patients capable of providing consent might have a greater chance of full recovery in comparison to subjects incapable of providing consent, or they may be less susceptible to the risks of the treatment (Schrems 2014).
Second, if the research would not be excessively held up by limiting it to consenting subjects, the FDA would assume that the research is to be performed on consenting subjects. For instance, it may be possible to obtain consent in advance from a patient who does not have the condition that will be treated, but who suffers from a particular disease or condition that places the subject at an extremely high risk for the event to be treated (i.e. cardiac patients at a high risk for cardiac arrest). However, even if the at-risk population can be identified, it may be infeasible to get consent from all patients, as the frequency of the specific life-threatening condition is infrequent. Therefore, subject enrolment would take too long to conduct the study in a reasonable amount of time (Food and Drug Administration 2013).
Eligibility for a Study to be Conducted Under 21 CFR 50.24
Studies considered for 21 CFR 50.24 must fulfil all of the following criteria: (i) the human subjects should be in a life-threatening condition that requires urgent intervention; (ii) current treatments are unproven or unsatisfactory; (iii) the acquisition of accurate scientific evidence is important to establish the safety and effectiveness of the intervention; (iv) the medical condition of the subject makes it impractical to obtain informed consent; (v) the investigative intervention must be performed before consent can be obtained from the subject’s legally authorized representative; (vi) there is no acceptable way to prospectively select individuals that are likely to become suitable for participation; (vii) participation in the research carries a high possibility of direct benefit to the study subjects; and (viii) it is not feasible to perform the clinical investigation without the waiver (Food and Drug Administration 2013; Halperin et al. 2007).
Regulation 21 CFR 50.24(a)(1) has directed IRBs to record whether the available treatments are unproven or unsatisfactory. The meaning of “unproven therapy” is comprised of treatment that is acceptable as the “standard of care”, but lacks rigorous scientific validations or submission to the FDA for approval; treatment that lacks sufficient clinical or pre-clinical information to justify the safety or efficacy of the product; treatment for which current information is insufficient to advocate approval, although the data have been submitted to the FDA; a product that is not approved or labelled for the specific indication under study; or an available product or therapy not indicated for use in a particular patient group such as a childhood population.
“Unsatisfactory” treatment might be “available” and “approved”, but it remains unsatisfactory. Despite the effectiveness of an available product or therapy, its use is associated with certain drawbacks such as safety and efficacy issues; the effective treatment time is too long (e.g. time to the cessation of symptoms); the treatment has constraints related to the setting in which it is required, e.g. the treatment should be administered in the field, but needs optimal cooling or might be challenging to use (requires surgical intervention for vascular access) (Food and Drug Administration 2013). Similarly, despite adrenaline being considered as standard of care during CPR, its use in treating out-of-hospital cardiac arrest patients versus placebo has been criticized (Jacobs et al. 2011) (Table 2).
A research study can be classified as of minimal, low, intermediate, or high incremental risk, depending upon the FDA labelling status of the treatment (Food and Drug Administration 2013). Under certain circumstances, it is acceptable to perform a study with minimal risk criteria without the requirement of documented consent (Hirshon et al. 2013; Food and Drug Administration 2013) (e.g. an approved mechanical cardiopulmonary resuscitation device versus standard CPR; amiodarone versus lidocaine). For a diagnostic study, minimal risk should include being non-invasive and not being used for real-time clinical decisions (e.g. non-invasive monitor, low-volume blood drawing). Minimal risk is also very unlikely to have community sensitivity (Halperin et al. 2007).
Limitations
The present report did not focus on prehospital research which remains a limitation of the current review. From the patient’s perspective, the prehospital research and informed consent is probably as important as in the ED and ICU settings. Therefore, we believe that out of hospital critical care research requires an extensive debate and further review of literature. Moreover, this report did not focus on data from one particular continent but we have addressed different opinions to make it broad and open for further discussion, and feasible for consideration under the diversity of culture and traditions worldwide.
Recommendations and Conclusions
For conducting successful research in emergency settings, feasible and cost-effective strategies should be implemented together with institutional support and sufficient funding. Collaboration provides an important means of promoting and supporting research in emergency settings and also facilitates the dissemination of the findings of evidence-based practice. Education and training through continuing medical education programs could be effective for increasing research capabilities and exposure. Furthermore, the involvement of non-medically qualified research associates is a reasonable option for enhancing research activities in the ED.
On the other hand, emergency medicine research abiding by ethical principles presents unique challenges to the informed consent process. This includes the time frame in which the research is performed and the vulnerability of the patients in the ED. Nonetheless, in many circumstances, informed consent is possible if the researcher is diligent and takes the time to adequately explain the study to the potential subject. Every researcher should have a personal obligation to ensure that he or she respects the rights of the subjects. If the subject is capable of providing consent, precautions should be taken to ensure that they have a decision-making capacity and are offered sufficient time to have their questions answered to their satisfaction. However, if consent is impractical, special attention should be given to protect the interests of the subjects.
Moreover, we should not exclude vulnerable cases from research projects, as this will affect their needs and violate the ethical principles of justice and beneficence. If we consider vulnerability as a context-related and situational concept with the existing approaches to informed consent, the ethical principles can be balanced and preserved during the entire research process, as has been recently reported by Schrems (2014).
Although emergency care research is privileged with special provisions of exemption for informed consent, the research protocol and way in which waiver consent is reported must be assessed by an independent regulatory body. In addition, the researchers involved in such studies have an obligation to consider the patients’ prospects and ethical conduct of research for the pre-hospital and ED settings. Research in emergency settings is still at an early stage, so there is a strong need for extensive research through community awareness, resource management, ethics, collaborations, capacity building, and the development of a research interest for the improvement of patient care and outcomes.
References
Adams, J. G., & Wegener, J. (1999). Acting without asking: An ethical analysis of the Food and Drug Administration waiver of informed consent for emergency research. Annals of Emergency Medicine, 33(2), 218–223.
Andra le Roux-Kemp. (2014). Deferred consent in emergency care research: A comparative perspective of south african regulations. Journal of Philosophy, Science and Law (Special Issue), 14, 47–62. http://jpsl.org/archives/deferred-consent/. Accessed March 15, 2015.
Annane, D., Outin, H., Fisch, C., & Bellissant, E. (2004). The effect of waiving consent on enrollment in a sepsis trial. Intensive Care Medicine, 30(2), 321–324.
Annane, D., Sebille, V., Charpentier, C., Bollaert, P. E., Francois, B., Korach, J. M., et al. (2000). Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. Journal of the American Medical Association, 288(7), 862–871.
Association of clinical research professionals (ACRP). (2015). Standard operating procedures for the conduct of clinical research. http://www.acrpnet.org/MainMenuCategory/Resources/SOPs/Standard-Operating-Procedures-for-the-Conduct-of-Clinical-Research.aspx. Accessed October 25, 2015.
Bion, J. F., & Heffner, J. E. (2004). Challenges in the care of the acutely ill. Lancet, 363, 970–977.
Breese, P. E., Burman, W. J., Goldberg, S., & Weis, S. E. (2007). Education level, primary language, and comprehension of the informed consent process. Journal of Empirical Research on Human Research Ethics, 2(4), 69–79.
Canadian Association of Emergency Physicians (CAEP). (2002). The future of emergency medicine in Canada: Submission from CAEP to the Romanow Commission. Part 2. CJEM, 4(6), 431–438.
Daugherty, E. L., & White, D. B. (2010). Conducting clinical research during disasters. AMA Journal of Ethics, 12, 701–705. http://virtualmentor.ama-assn.org/2010/09/pdf/ccas1-1009.pdf. Accessed December 27, 2014.
Department of Health, United Kingdom. (2006). Medicines for human use (clinical trials) amendment (No. 2) regulations 2006. Statutory Instrument 2006 No 2984. Retrieved from http://www.opsi.gov.uk/si/si2006/20062984.htm. Accessed August 03, 2014.
Donatelli, L. A., Geocadin, R. G., & Williams, M. A. (2006). Ethical issues in critical care and cardiac arrest: Clinical research, brain death, and organ donation. Seminars in Neurology, 26(4), 452–459.
Eid, H. O., Lunsjo, K., Torab, F. C., & Abu-Zidan, F. M. (2008). Trauma research in the United Arab Emirates: Reality and vision. Singapore Medical Journal, 49(10), 827–830.
Food and Drug Administration. (2013). U.S. Department of Health and Human Services. Title 21 (food and drugs) code of federal regulation, part 50.24: Exception from informed consent requirements for emergency research. Retrieved from http://www.fda.gov/downloads/RegulatoryInformation/Guidances/UCM249673.pdf. Accessed December 25, 2014.
Gamble, C., Woolfall, K., Williamson, P., Appleton, R., & Young, B. (2013). New European Union regulation of clinical trials is conflicting on deferred consent in emergency situations. British Medical Journal, 346, f667. doi:10.1136/bmj.f667.
Good, A. M. T., & Driscoll, P. (2002). Clinical research in emergency medicine: Putting it together. Emergency Medicine Journal, 19(3), 242–246.
Govindarajan, P., Dickert, N. W., Meeker, M., De Souza, N., Harney, D., Hemphill, C. J., et al. (2013). Emergency research: Using exception from informed consent, evaluation of community consultations. Academic Emergency Medicine, 20(1), 98–103.
Halila, R. (2007). Assessing the ethics of medical research in emergency settings: How do international regulations work in practice? Science and Engineering Ethics, 13(3), 305–313.
Halperin, H., Paradis, N., Mosesso, V, Jr, Nichol, G., Sayre, M., Ornato, J. P., et al. (2007). Recommendations for implementation of community consultation and public disclosure under the Food and Drug Administration’s “Exception from informed consent requirements for emergency research”: A special report from the American Heart Association Emergency Cardiovascular Care Committee and Council on Cardiopulmonary, Perioperative and Critical Care: Endorsed by the American College of Emergency Physicians and the Society for Academic Emergency Medicine. Circulation, 116(16), 1855–1863.
Harvey, S. E., Elbourne, D., Ashcroft, J., Jones, C. M., & Rowan, K. (2006). Informed consent in clinical trials in critical care: Experience from the PAC-Man Study. Intensive Care Medicine, 32(12), 2020–2025.
Harvey, S., Harrison, D. A., Singer, M., Ashcroft, J., Jones, C. M., Elbourne, D., et al. (2005). Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): A randomised controlled trial. Lancet, 366(9484), 472–477.
Hilden, J., & Gammelgaard, A. (2002). Premature stopping and informed consent in AMI trials. Journal of Medical Ethics, 28(3), 188–189.
Hirshon, J. M., Hansoti, B., Hauswald, M., Sethuraman, K., Kerr, N. L., Scordino, D., et al. (2013). Ethics in acute care research: A global perspective and research agenda. Academic Emergency Medicine, 20(12), 1251–1258.
Jacobs, I. G., Finn, J. C., Jelinek, G. A., Oxer, H. F., & Thompson, P. L. (2011). Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation, 82(9), 1138–1143.
Jansen, T. C., Bakker, J., & Kompanje, E. J. (2010). Inability to obtain deferred consent due to early death in emergency research: Effect on validity of clinical trial results. Intensive Care Medicine, 36(11), 1962–1965.
Jansen, T. C., Kompanje, E. J., & Bakker, J. (2009). Deferred proxy consent in emergency critical care research: Ethically valid and practically feasible. Critical Care Medicine, 37(1 Suppl), S65–S68.
Jansen, T. C., Kompanje, E. J., Druml, C., Menon, D. K., Wiedermann, C. J., Bakker, J., et al. (2007). Deferred consent in emergency intensive care research: What if the patients dies early? Use of the data or not? Intensive Care Medicine, 33(5), 894–900.
Kaufman, S. R. (1997). The World War II plutonium experiments: Contested stories and their lessons for medical research and informed consent. Culture, Medicine and Psychiatry, 21(2), 161–197.
Kompanje, E. J., Maas, A. I., Menon, D. K., & Kesecioglu, J. (2014). Medical research in emergency research in the European Union member states: Tensions between theory and practice. Intensive Care Medicine, 40(4), 496–503.
Kompanje, E. J., Maas, A. I., Slieker, F. J., & Stocchetti, N. (2007). Ethical implications of time frames in a randomized controlled trial in acute severe traumatic brain injury. Progress in Brain Research, 161, 243–250.
Kortgen, A., Niederprum, P., & Bauer, M. (2006). Implementation of an evidence-based “standard operating procedure” and outcome in septic shock. Critical Care Medicine, 34(4), 943–949.
Kulkarni, N. G., Dalal, J. J., & Kulkarni, T. N. (2014). Audio–video recording of informed consent process: Boon or bane. Perspectives in Clinical Research, 5(1), 6–10.
Lecouturier, J., Rodgers, H., Ford, G. A., Rapley, T., Stobbart, L., Louw, S. J., et al. (2008). Clinical research without consent in adults in the emergency setting: A review of patient and public views. BMC Medical Ethics, 9, 9. doi:10.1186/1472-6939-9-9.
Lemaire, F., Bion, J., Blanco, J., Damas, P., Druml, C., Falke, K., et al. (2005). The European Union Directive on Clinical Research: Present status of implementation in EU member states’ legislations with regard to the incompetent patients. Intensive Care Medicine, 31(3), 476–479.
Liddell, K., Bion, J., Chamberlain, D., Druml, C., Kompanje, E., Lemaire, F., et al. (2006). Medical research involving incapacitated adults: Implications of the EU Clinical Trials Directive 2001/20/EC. Medical Law Review, 14(3), 367–417.
Madden, C., & Cole, T. B. (1995). Emergency intervention to break the cycle of drunken driving and recurrent injury. Annals of Emergency Medicine, 26(2), 177–179.
Maitland, K., Molyneux, S., Boga, M., Kiguli, S., & Lang, T. (2011). Use of deferred consent for severely ill children in a multi-centre phase III trial. Trials, 12, 90. doi:10.1186/1745-6215-12-90.
Marshall, L. F., Maas, A. I., Marshall, S. B., Bricolo, A., Fearnside, M., Iannotti, F., et al. (1998). A multicenter trial on the efficacy of using tirilazad mesylate in cases of head injury. Journal of Neurosurgery, 89(4), 519–525.
Mayo Clinic. (2015). Institutional review board (IRB): Definition of terms. http://www.mayo.edu/research/institutional-review-board/definition-terms. Accessed June 6, 2015.
Medical Ethics Committee of the World Medical Association (1999). Proposed revision of the World Medical Association declaration of Helsinki. Ferney-Voltaire, France: World Medical Association (WMA document 17.C/Rev1/99).
Offerman, S. R., Nishijima, D. K., Ballard, D. W., Chetipally, U. K., Vinson, D. R., & Holmes, J. F. (2013). The use of delayed telephone informed consent for observational emergency medicine research is ethical and effective. Academic Emergency Medicine, 20(4), 403–407.
Ogilvie, M. P., Pereira, B. M., Ryan, M. L., Gomez-Rodriguez, J. C., Pierre, E. J., Livingstone, A. S., et al. (2011). Bispectral index to monitor propofol sedation in trauma patients. Journal of Trauma, 71(5), 1415–1421.
Petrini, C. (2014). Regulation (EU) No 536/2014 on clinical trials on medicinal products for human use: An overview. Annali dell Istituto Superiore di Sanita, 50(4), 317–321.
Pines, J. M., Hollander, J. E., Localio, A. R., & Metlay, J. P. (2006). The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Academic Emergency Medicine, 13(8), 873–878.
Quest, T., & Marco, C. A. (2003). Ethics seminars: Vulnerable populations in emergency medicine research. Academic Emergency Medicine, 10(11), 1294–1298.
Rhodes, K. V., & Pollock, D. A. (2006). The future of emergency medicine public health research. Emergency Medicine Clinics of North America, 24(4), 1053–1073.
Richardson, L. D., & Hwang, U. (2001). Access to care: A review of the emergency medicine literature. Academic Emergency Medicine, 8(11), 1030–1036.
Richmond, T. S., & Ulrich, C. (2007). Ethical issues of recruitment and enrollment of critically ill and injured patients for research. AACN Advanced Critical Care, 18(4), 352–355.
Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., et al. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345, 1368–1377. doi:10.1056/NEJMoa010307.
Roberts, I., Shakur, H., Yates, D., & Sandercock, P. (2005). Trauma care research and the war on uncertainty. British Medical Journal, 331(7525), 1094–1096.
Runyon, M. S., Sawe, H. R., Levine, A. C., Pousson, A., House, D. R., Agrawal, P., et al. (2013). Clinical and translational research in global health and emergency care: A research agenda. Academic Emergency Medicine, 20(12), 1272–1277.
Sathyanarayana Rao, T. S., Radhakrishnan, R., & Andrade, C. (2011). Standard operating procedures for clinical practice. Indian Journal of Psychiatry, 53(1), 1–3.
Schmidt, T. A., Salo, D., Hughes, J. A., Abbott, J. T., Geiderman, J. M., Johnson, C. X., et al. (2004). Confronting the ethical challenges to informed consent in emergency medicine research. Academic Emergency Medicine, 11(10), 1082–1089.
Schrems, B. M. (2014). Informed consent, vulnerability and the risks of group-specific attribution. Nursing Ethics, 21(7), 829–843.
Sprivulis, P. C., Da Silva, J. A., Jacobs, I. G., Frazer, A. R., & Jelinek, G. A. (2006). The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Medical Journal of Australia, 184(5), 208–212.
Standard Operating Procedures for Good Clinical Practice by Sponsors of Clinical Trials CenterWatch. (2014). http://store.centerwatch.com/p-438-standard-operating-procedures-for-good-clinical-practice-by-sponsors-of-clinical-trials.aspx. Accessed October 24, 2015.
Uscher-Pines, L., Pines, J., Kellermann, A., Gillen, E., & Mehrotra, A. (2013). Emergency department visits for nonurgent conditions: Systematic literature review. The American Journal of Managed Care, 19(1), 47–59.
Williams, B. F., French, J. K., White, H. D., & HERO-2 consent substudy investigators. (2003). Informed consent during the clinical emergency of acute myocardial infarction (HERO-2 consent substudy): A prospective observational study. Lancet, 361(9361), 918–922.
Woolfall, K., Young, B., Frith, L., Appleton, R., Iyer, A., Messahel, S., et al. (2014). Doing challenging research studies in a patient-centred way: A qualitative study to inform a randomised controlled trial in the paediatric emergency care setting. BMJ Open, 2014(4), e005045. doi:10.1136/bmjopen-2014-005045.
Wright, D., Crouch, R., & Clancy, M. (2005). Role of networks in supporting emergency medicine research: Findings from the Wessex emergency care research network (WECReN). Emergency Medicine Journal, 22(2), 80–83.
Young, B., Runge, J. W., Waxman, K. S., Harrington, T., Wilberger, J., Muizelaar, J. P., et al. (1996). Effects of pegorgotein on neurologic outcome of patients with severe head injury. A multicenter, randomized controlled trial. Journal of the American Medical Association, 276(7), 538–543.
Yuval, R., Halon, D. A., Merdler, A., Khader, N., Karkabi, B., Uziel, K., et al. (2000). Patient comprehension and reaction to participating in a double-blind randomized clinical trial (ISIS-4) in acute myocardial infarction. Archives of Internal Medicine, 160(8), 1142–1146.
Acknowledgments
All authors read and approved the manuscript with no conflict of interest and no financial issue to disclose. All Authors have contributed in the design, data interpretation, manuscript drafting and approval. This Work received no specific grant from any funding agency in the public, commercial or not-for-profit sectors’.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Menyar, A., Asim, M., Latifi, R. et al. Research in Emergency and Critical Care Settings: Debates, Obstacles and Solutions. Sci Eng Ethics 22, 1605–1626 (2016). https://doi.org/10.1007/s11948-015-9730-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11948-015-9730-5