Opinion statement
Standard treatment of anaplastic astrocytoma (AA) in good performance patients consists of maximal safe surgical resection followed by focal, fractionated, external beam radiotherapy (RT) alone or in combination with concurrent and adjuvant temozolomide (TMZ). Since prospective data regarding the use of chemoradiotherapy for AA is lacking, the practice is based on the extrapolation of results from a randomized study in glioblastoma (GB). Whether the data from the GB study can and should be extrapolated is controversial, although a large multicenter, randomized, phase III study is underway to define optimal initial AA treatment. Patients should be tapered off corticosteroids completely or to the lowest dose necessary to treat neurologic dysfunction. Anti-epileptic drugs (AED) are not indicated unless there is a history of seizure; levetiracetam is the preferred AED in malignant glioma (MG). Unless there is evidence of intracranial hemorrhage, venous thromboembolism (VTE) should be treated with low-molecular-weight heparin (LMWH) therapy. At recurrence, patients with good performance status are usually treated with cytotoxic chemotherapy following, or in lieu of, repeat surgery. TMZ is the preferred chemotherapeutic agent in patients without prior exposure; lomustine is recommended for tumors resistant to TMZ. In patients with neurologic dysfunction secondary to tumor edema and mass effect who are not amenable to surgery, the use of bevacizumab is associated with improved neurologic function and better quality of life. Given the limited treatment options at tumor recurrence, consideration for enrollment on a clinical trial is encouraged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
AA is a malignant glioma (MG) with mean age of onset of 41 years [1]. In population-based registries, it constitutes 4 % of all malignant nervous system tumors [1] and 10 % of all gliomas [2]. The prognosis for patients with AA can be variable although it is generally poor. Despite treatment, median survival and the 5-year survival rate are 3 years and 28 %, respectively [3, 4]. Although AA may arise as a new primary “de novo” tumor, 75 % result from dedifferentiation of a lower-grade astrocytoma [5]. Exposure to ionizing radiation and rare genetic syndromes such as neurofibromatosis types 1 and 2, tuberous sclerosis, and Li-Fraumeni are the only established causes of AA. Various occupational and environmental exposures have been suggested by some investigators, although evidence is lacking [6–9].
AA presents with localized or generalized neurological signs and symptoms, which are determined by the neuro-anatomical location of the tumor. Generalized signs and symptoms consist of headache, seizures, and personality change. Compared with low grade glioma, seizures are less common; seizures were the presenting symptom in 46 % of AA in 1 study [10]. Localized signs and symptoms include focal weakness, sensory symptoms, gait ataxia, visual symptoms, and language dysfunction.
Magnetic resonance imaging (MRI) with administration of gadolinium contrast is the optimal non-invasive technique for the diagnosis and management of AA [11, 12]. MRI is useful to establish a differential diagnosis, guide tumor biopsy or resection, plan radiotherapy, and monitor response to treatment and diagnose disease progression [13]. Head computerized tomography (CT) scan and non-contrast MRI are not adequate for thorough evaluation, but CT must suffice for those unable to undergo an MRI.
On MRI, AA presents as an ill-defined T1-weighted hypointense and T2-weighted hyperintense mass with associated vasogenic edema. Typically, nodular areas of gadolinium enhancement are present, although up to one third of tumors may show no contrast enhancement [5, 14]. The presence of abnormal enhancement in a tumor implies the presence of a high-grade tumor even if a biopsy shows a low-grade tumor as sampling error may occur. Additional advanced imaging techniques such as Diffusion-Weighted Imaging, proton MR spectroscopy, and MR perfusion may aid in the diagnosis and management of AA [5, 14, 15].
AA often displays heterogeneous histology, consisting of distinct areas of low and high grade tumor, which is thought to indicate biologic progression from a lower grade precursor. Since the diagnosis is sometimes determined from small biopsy tissue specimens, sampling error may occur [16]. The World Health Organization (WHO) classification scheme is the most widely used system of grading glial tumors. AA, defined as a grade III glioma, is characterized by increased mitotic activity, marked cellularity, and nuclear atypia, whereas necrosis or extensive microvascularization are absent [12, 17]. The MIB-1 labeling index is usually 5 % to 10 %, but may overlap with low grade astrocytoma or GB, and show considerable variation within a given tumor [18–21].
There is no single molecular marker that defines AA, although mutations in TP53 are frequent, and differentiate AA from oligodendroglial tumors. The Cancer Genome Atlas GB project has resulted in a tremendous influx of new data concerning the genomic alterations in gliomas [22, 23, 24•]. The data relates primarily to primary (de novo) GB, although a small number of secondary tumors were included. AA is thought to share a common lineage and thus molecular pathology with secondary GB [25, 26]. Utilizing gene expression profiling, Phillips et al. identified novel subgroups of high grade glioma (Proneural, Proliferative, and Mesenchymal) defined by distinct clinical and molecular characteristics [27]. Nearly all AA tumor specimens and good prognosis GB were classified as Proneural. The Proneural subtype had the best prognosis and expresses genes associated with normal brain processes and neurogenesis rather than gene expression indicative of cell proliferation and angiogenesis that are found in the other 2 subtypes. The relevance of these subtypes to treatment is yet to be determined.
Epigenetic silencing of the O6 –methyl-guanyl-methyl-transferase (MGMT) DNA repair gene by promoter methylation has been associated with longer survival for GB patients, particularly those treated with alkylating agents such as TMZ [28–30]. Much less is known about the prognostic value of MGMT methylation in AA. A retrospective study demonstrated MGMT promoter methylation in 54.7 % (35 of 64 patients) of AA [31]. The median survival of WHO grade III gliomas with a methylated MGMT promoter showed a trend in longer survival, although it was not statistically significant (9.7 vs 6.1 years, P = 0.33). The authors concluded that MGMT failed to demonstrate a prognostic or predictive role although the study was confounded by the fact that only one third of patients were treated with TMZ after malignant progression and another quarter did not receive any adjuvant chemotherapy.
Wick et al. analyzed the MGMT promoter methylation status in 202 evaluable WHO grade III gliomas treated on a randomized phase III trial.[32] MGMT promoter methylation was detected in 50 % (48 of 96) of AA. MGMT promoter methylation was associated with better progression free survival (PFS) regardless of whether patients were treated with alkylating chemotherapy agents or RT alone. The authors concluded that MGMT promoter hypermethylation in anaplastic gliomas may be regarded as a prognostic marker for good outcome in patients treated with radiotherapy or predictive for response to radiotherapy itself. They speculated that MGMT hyper-methylated anaplastic gliomas may carry a general defect in regulation of DNA methylation leading to epigenetic inactivation of multiple genes, including genes linked to radio-resistance.
Somatic mutations of the isocitrate dehydrogenase enzymes (IDH1 and IDH2) appear to play a critical role in the pathogenesis of most AA and secondary GB [23, 24•, 33•, 34]. The IDH enzymes catalyze the conversion of isocitrate to α-ketoglutarate, a key component of the Krebs cycle [33•]. The enzymes utilize NADP + as a cofactor to generate α-ketoglutarate and NADPH in a reversible reaction. Over 90 % of the IDH mutations in gliomas affect IDH1 [34]. The IDH1 mutations target specific arginine residues and are exclusively heterozygous raising the possibility of a novel gain-of-function phenotype whereby the mutant enzymes produce high levels of what is ordinarily a minor metabolic product, R(-)-2-hydroxyglutarate, with relative depletion of α-ketoglutarate and NADPH [23, 24•, 34–36]. Whether there is a role of 2-hydroxglutarate in tumor development is unknown.
It is unknown whether therapy targeting IDH mutations would be beneficial. Studies have demonstrated that the IDH mutation is a positive prognostic factor independent of age, functional status, and MGMT promoter methylation status [32]. In fact IDH1 may be a better predictor of prognosis than histology. Patients with IDH1 wild type AA had worse prognosis than IDH1-mutated GB in one study [37•]. It is anticipated that IDH status will be an important consideration in future revisions of the WHO criteria for gliomas.
Treatment
Pharmacologic treatment: supportive care
-
Seizures, brain edema, and deep venous thrombosis are common medical issues encountered in brain tumor patients.
-
AA patients with history of seizure should be treated with an AED. The use of prophylactic AED in brain tumor patients is controversial. The American Academy of Neurology issued a practice guideline advising that AED should not be used in brain tumor patients who have never experienced a seizure because of the lack of beneficial evidence [38].
-
Antiepileptic drugs that induce hepatic cytochrome p-450 enzymes, such as phenytoin, carbamazepine, oxcarbamazepine, and phenobarbital, should be avoided because of interactions with many chemotherapeutic agents and other drugs. Although only approved by the FDA as add-on therapy, single agent levetiracetam is the most widely used, well tolerated, and best agent for brain tumor patients [39, 40] (class III) Other “non-enzyme inducing” AED include gabapentin, lacosamide, lamotrigine, topiramate, valproic acid, and zonisamide.
-
Corticosteroids reduce brain tumor associated vasogenic edema through restoration of the blood-brain-barrier via an unknown mechanism [41]. Reduction of vasogenic brain edema may improve neurologic dysfunction. Asymptomatic patients with brain edema do not need prophylactic corticosteroids. Because of their numerous side effects, patients should be treated with the lowest dose of corticosteroid that controls their symptoms and every effort should be made to discontinue the drug completely. For mostly historical reasons, dexamethasone is the most widely used corticosteroid in Neuro-Oncology [41].
-
Venous thromboembolism (VTE) is common in malignant glioma [42]. Prospective clinical trials report an annual risk of 17 %–22.9 % [43–45]. Venous ultrasound and CT angiography are the diagnostic imaging modalities of choice for the diagnosis of deep venous thrombosis and pulmonary embolism, respectively. To reduce the risk of post-operative VTE, prophylactic low molecular weight heparins (LMWH) should be started on the day after craniotomy. There is no indication for prophylactic anticoagulation beyond the post-operative period. Despite the fear of intracranial hemorrhage, the treatment of VTE disease with full therapeutic anticoagulation appears to be safe for primary brain tumor patients [42], (class IV). Compared to warfarin, LMWH may be safer and more effective and is preferable because of minimal drug and food interactions and lack of requirement for laboratory monitoring [46], (class IV). The use of therapeutic anticoagulation is not contraindicated in patients receiving anti-vascular endothelial growth factor (VEGF) therapy with bevacizumab [47], (class II). Because of their high complication rate, inferior venae cava filters are only recommended for patients with VTE disease and significant intracranial hemorrhage or some other anti-coagulation contraindication [48], (class IV).
Levetiracetam
- Standard dosage:
-
500–1500 mg by mouth twice a day.
- Contraindications:
-
Hypersensitivity to levetiracetam.
- Main drug interactions:
-
No significant drug interactions [49]. Specific to AA, there are no known drug interactions with corticosteroids, warfarin, LMWH, or chemotherapeutic agents.
- Main side effects:
-
The most common side effects include somnolence, asthenia, and dizziness. Behavioral abnormalities such as irritability, aggression and psychosis are less common. All AED may cause an increase in suicidal thoughts.
- Special points:
-
Anti-epileptic drug of choice for neuro-oncologic patients. The dosage should be reduced in patients with impaired renal function.
- Cost:
-
Moderate.
Dexamethasone
- Standard dosage:
-
In patients with symptomatic brain edema, start at 8 mg twice daily, tapering the dose to tolerance at a rate of 2 mg every 4 days. If 16 mg per day are ineffective, the dose can be doubled every 48 hours until there is maximal response.
- Contraindications:
-
Systemic fungal infection or hypersensitivity to dexamethasone.
- Main drug interactions:
-
Dexamethasone has been reported to increase and decrease phenytoin levels leading to alteration of seizure control. Phenytoin may reduce effective concentrations of dexamethasone. Co-administration with warfarin usually results in inhibition of response to warfarin so that coagulation indices should be monitored closely.
- Main side effects:
-
Common side effects include insomnia, tremor, weight gain, steroid myopathy (weakness of neck flexors and muscles of the shoulder and pelvic girdle), diabetes, behavioral changes (hyperactivity and irritability), urinary frequency (nocturia), and hiccups. Less common but serious side effects include osteoporosis, avascular necrosis of the hip, gastrointestinal (GI) bleeding, perforation of the GI tract, psychosis, depression, opportunistic infections (Pneumocystis), glaucoma, delirium, and pancreatitis [41].
- Special points:
-
Gastric protection with H2 blockers or proton pump inhibitors is not recommended unless a patient develops upper GI symptoms or there is history of gastric ulceration or evidence of bleeding. Patients treated with corticosteroids for longer than 6 weeks should receive prophylactic trimethoprim-sulfamethoxazole 3 times per week; the drug is continued until a month after corticosteroids are stopped [41], (class IV).
- Cost:
-
Inexpensive.
Tumor treatment at diagnosis
Surgery
-
Maximal safe surgical resection is recommended for high performance patients, although there has never been a prospective, randomized study to demonstrate an advantage over biopsy. Retrospective analyses suggest improved overall survival (OS) with more extensive surgical resection [4, 32], (class IV). Extensive resection also has the benefit of providing adequate tissue for histological diagnosis and reduces tumor mass effect which may improve neurologic dysfunction.
-
Surgery is not curative because of diffuse infiltration of tumor into the surrounding brain parenchyma.
-
Advances in neuroimaging have improved the ability to maximally resect tumor while minimizing adverse effects. Functional MRI and Diffusion Tensor Imaging allow localization of eloquent brain areas and white matter tracts, respectively, so that these areas can be avoided during tumor resection. Intraoperative MRI is used to depict residual tumor tissue during an operation, aiding neurosurgeons in achieving gross total resection [5, 50–52], (class IV).
Radiation Therapy (RT)
-
Following surgical resection, RT is standard treatment for MG. The benefit of RT was established in multiple prospective clinical studies [53–60], (class III).
-
RT is not curative because of the potential damage to the normal nervous system at the high radiation doses that would be required to sterilize the tumor [41].
-
The use of stereotactic radiosurgery boost in addition to standard RT failed to show benefit for newly diagnosed MG in randomized clinical trials [61].
-
Accelerated hyperfractionation radiotherapy (70.4 Gy in 44 fractions delivered twice daily) was equivalent to standard fractionated RT (total dose 59.4 Gy) [62], (class III).
RT
- Standard procedure:
-
RT is delivered to the contrast enhancing tumor plus the T2-weighted peritumoral surround and a 3 cm margin. This planned tumor volume receives approximately 50 Gray (Gy). The contrast enhancing tumor volume receives an additional 10 Gy; all administered in 18–20 Gy fractions per day, 5 fractions per week, for a total of 60 Gy.
- Contraindications:
-
There are no definitive contraindications, although elderly patients with poor performance status may have difficulty tolerating the therapy.
- Complications:
-
Side effects of RT can be divided into acute, early-delayed, and late complications. An acute encephalopathy characterized by headache, nausea, drowsiness, fever, and sometimes worsening of neurological signs can occur within 2 weeks of RT onset [63]. Early-delayed complications (2 weeks to 3–4 months after the completion of radiotherapy) include the “somnolence syndrome” which is characterized by hypersomnia, drowsiness, and irritability [63–65]. Radionecrosis, cognitive dysfunction, and leukoencephalopathy are the main delayed complications of brain irradiation [63]. A survey on cognitive deficits in progression free survivors of low grade glioma failed to confirm a generally assumed relationship between radiotherapy and cognitive deficits [66]. Radiation-induced, progressive endocrine dysfunction of hypothalamic origin has been reported [63].
- Cost:
-
Expensive.
Pharmacologic treatment: chemotherapy
-
Following surgery, newly diagnosed AA is sometimes treated with concurrent RT/TMZ and adjuvant TMZ as per the standard regimen for GB [67], (class IV). Although, it is unknown whether the survival benefit achieved with radiochemotherapy in GB can and should be extrapolated to AA; randomized prospective studies are lacking [32]. Further data regarding the use of chemoradiotherapy will be obtained from EORTC 26053-22054 (CATNON Intergroup Trial), an ongoing, prospective, randomized phase III study of RT with or without concurrent and/or adjuvant TMZ in patients with non-1p/19q deleted anaplastic glioma.
-
A meta-analysis of MG patients treated with nitrosurea-based therapy (lomustine or carmustine) suggested a survival benefit with chemotherapy [68], (class II).
-
A phase III study randomized newly diagnosed MG patients to (A) conventional RT; (B) procarbazine, lomustine, vincristine (PCV); or (C) TMZ [32]. At occurrence of unacceptable treatment toxicity or disease progression, patients in arm (A) were treated with PCV or TMZ (1:1 random assignment), whereas patients in (B) or (C) received radiotherapy. The primary endpoint was time to treatment failure (TTF) defined as progression after radiotherapy and one chemotherapy in either sequence. Median TTF was similar for all arms. In the AA subgroup, Progression-free survival (PFS) was 10.8 months with RT and 18.2 months with chemotherapy suggesting a role for first line chemotherapy (class II).
-
Pseudoprogression is a subacute (usually within 4 months of RT completion), treatment-related reaction with or without clinical deterioration and MRI changes suggestive of tumor progression. It is observed in 20 %–40 % of MG, particularly in patients treated with RT and concurrent TMZ compared with RT alone [69, 70]. Despite the clinical or radiological suggestion of tumor progression, patients recover or stabilize without additional treatment. Pseudoprogression appears to be more common in tumors with MGMT promoter methylation [71], Pseudoprogression is not easily differentiated from tumor progression by anatomic or advanced physiologic imaging. Recognition of this phenomenon is important to reduce inappropriate changes in therapy. It is recommended that patients with clinically asymptomatic progressive lesions on MRI within the first 3 months after TMZ chemoradiotherapy should continue with adjuvant TMZ. Symptomatic patients within this timeframe should be considered for a repeat surgical resection; corticosteroids or bevacizumab are options if surgery is contraindicated (class IV).
TMZ
- Standard dosage:
-
75 mg/m2 by mouth daily during RT and 150–200 mg/m2 on a 5/28 day schedule for 6 months following radiotherapy.
- Contraindications:
-
Patients who have a history of hypersensitivity to TMZ or inadequate bone marrow reserve.
- Main drug interactions:
-
Valproic acid decreases TMZ clearance by about 5 %. There is no interaction with cytochrome p450 inducers.
- Main side effects:
-
The most common side effects include nausea/vomiting, constipation, and fatigue. Grade 3–4 hematologic events (thrombocytopenia or neutropenia) occur in approximately 19 %.
- Special points:
-
Caution should be exercised in patients with hepatic or renal impairment.
- Cost:
-
Expensive.
Lomustine and carmustine
- Standard dosage:
-
Lomustine (110 mg/m2 by mouth) and carmustine (150–200 mg/m2 intravenously) on day 1 of a 42 day treatment cycle.
- Contraindications:
-
Hypersensitivity to the drug or inadequate bone marrow reserve.
- Main drug interactions:
-
No significant interactions with drugs frequently used in neuro-oncology.
- Main side effects:
-
Nausea, vomiting, and myelosuppression (usually occurs 4 to 6 weeks after drug administration); myelosuppression may be cumulative. The occurrence of acute leukemia and bone marrow dysplasia has been reported in patients on long term therapy. Pulmonary infiltrates or fibrosis has been reported rarely after an interval of 6 months or longer from the start of therapy with cumulative doses greater than 1100 mg/m2.
- Special points:
-
Baseline pulmonary function studies should be conducted along with pulmonary function tests during treatment to assess for risk of developing pulmonary fibrosis.
- Cost:
-
Expensive.
Procarbazine
- Standard dosage:
-
60 mg/m2 by mouth on days 8–21 of a 42 day treatment cycle.
- Contraindications:
-
Hypersensitivity to procarbazine or inadequate bone marrow reserve.
- Main drug interactions:
-
Ethyl alcohol should not be used since there may be a disulfiram-like reaction. Because procarbazine exhibits some monamine oxidase inhibitory (MAOI) activities, sympathomimetic drugs, and tricyclic antidepressants should be avoided.
- Main side effects:
-
Leukopenia, anemia, thrombocytopenia, nausea, and vomiting.
- Special points:
-
A low-tyramine diet is recommended due to the MAOI activity of procarbazine.
- Cost:
-
Expensive.
Vincristine
- Standard dosage:
-
1.4 mg/m2 intravenously (maximum dose, 2 mg) on days 8 and 29 of a 42 day cycle.
- Contraindications:
-
Patients with Charcot-Marie-tooth syndrome should not receive vincristine.
- Main drug interactions:
-
Cytochrome p450 inducers may alter the metabolism of vincristine.
- Main side effects:
-
Hair loss, leukopenia, constipation, neuritic pain, autonomic neuropathy (abdominal pain, constipation, and ileus) and peripheral neuropathy.
- Special points:
-
All patients receiving vincristine should follow a prophylactic bowel regimen of stool softeners and laxatives.
- Cost:
-
Expensive.
Treatment in the elderly
-
There is a perception that elderly (age >70 years) patients have more difficulty tolerating standard radiotherapy than younger patients.
-
Recommended treatment options for elderly patients include standard RT or RT/TMZ (for fit, otherwise healthy elderly patients), accelerated hypofractionated radiotherapy (34–40 Gy in10–15 fractions), and primary TMZ chemotherapy with deferred RT (class IV).
-
The NOA-08 trial randomized 373 patients, age > 65 years, with AA or GB to standard postsurgical RT (54–60 Gy) vs TMZ (100 mg/m2/day, 1-week-on/ 1-week-off) [15]. The TMZ arm had a similar outcome to RT suggesting that TMZ alone, particularly in those with a methylated MGMT promoter gene, is an option for newly diagnosed, elderly AA patients [72••] (class II).
Treatment at recurrence/progression
-
For tumors that progress following initial therapy, treatment options are limited.
-
Re-resection can be helpful in selected patients, particularly those symptomatic from tumor mass effect and with tumors in non-eloquent brain. Although surgery may improve performance, the benefit with respect to survival has not been evaluated (class IV).
-
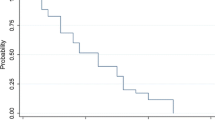
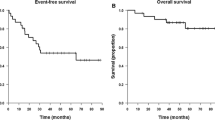
TMZ demonstrated efficacy in a multi-center, phase II study AA initially treated with RT alone [73], (class III). The study demonstrated 6-month progression free survival (PFS-6) of 46 %, objective radiologic response rate of 35 % and OS of 13.6 months [73].
-
Continuous dose-dense TMZ (50 mg/m2/day) is an option for recurrent AA, particularly those with early progression (before completion of 6 cycles of adjuvant therapy) and in previous responders (those who progressed more than 2 months after completing adjuvant therapy) [74•], (class III). The hypothesis is that protracted TMZ dosing overcomes drug resistance by reducing intra-tumoral MGMT activity and provides an anti-angiogenic effect (limit endothelial cell recovery, inhibit the activity of circulating endothelial precursors, and up-regulate thrombospondin-1). In the study by Perry et al. PFS-6, 1-year OS, and radiographic response rate were 35.7 %, 60.7 %, and 15.4 %, respectively [74•]. It remains uncertain whether metronomic TMZ is more effective than re-challenge with standard dose TMZ in previous responders.
-
The combination of bevacizumab and irinotecan was evaluated in patients with AA (n = 25/33) and anaplastic oligodendroglioma (n = 8/33) in a phase 2 study [75], (class III). The PFS-6, 6-month OS, and radiologic response rate were 55 %, 79 %, and 61 %, respectively, indicating that bevacizumab may have similar activity to that seen in GB. Kreisl et al. conducted a study of single agent bevacizumab in patients with recurrent MG (68 % were AA) [76•]. Median OS was 12 months. Median PFS was 2.93 months and PFS-6 (the primary endpoint) was 20.9 %. Forty-three percent of patients achieved a radiographic response. Despite the low PFS-6, patients experienced a significant clinical benefit; 67 % on corticosteroids at study onset were able to decrease the dose by an average reduction of 71 % (Class III). Forty-eight percent of patients had improved neurological symptoms with treatment.
-
Re-irradiation was found to be safe and have palliative benefit in 2 single institution retrospective studies; however both suffer from their retrospective nature and likely selection bias [77, 78], (Class IV). Large prospective studies demonstrating benefit are lacking, although the Radiation Therapy Oncology Group (RTOG) is conducting a phase II trial of concurrent bevacizumab and re-irradiation vs bevacizumab alone for recurrent GB (RTOG 1205).
-
Other options at recurrence include treatment with single-agent carmustine, lomustine, or PCV (Class IV).
-
Given the modest efficacy and need to define new AA treatments, enrollment on a clinical trial is encouraged at recurrence in eligible patients.
Bevacizumab
- Standard dosage:
-
10 mg/kg intravenous every weeks.
- Contraindications:
-
Hypersensitivity to bevacizumab or intracranial or systemic hemorrhage.
- Main drug interactions:
-
None.
- Main side effects:
-
Hypertension, epistaxis, proteinuria. Rare but serious side effects include infusion reaction, intracranial or systemic hemorrhage, VTE, wound dehiscence and healing impairment, and GI perforation.
- Cost:
-
Very expensive.
Irinotecan
- Standard dosage:
-
125 mg/m2 intravenous every 2 weeks.
- Contraindications:
-
Hypersensitivity to irinotecan.
- Main drug interactions:
-
Metabolism of irinotecan is affected by cytochrome p450 inducing drugs.
- Main side effects:
-
Diarrhea, myelosuppression and nausea.
- Cost:
-
Expensive.
Emerging therapies
-
Despite initial optimism, studies investigating agents that target the molecular pathology of MG have been overwhelmingly disappointing [79•]. Identifying subsets of AA with apparent oncogene addiction may permit improved efficacy of available targeted therapies. In addition, the use of correlative studies, that utilize post-treatment surgical specimens to determine if the targeted agent of interest enters the tumor and affects the targeted signaling pathway, is encouraged.
-
Other therapeutic strategies under active investigation include immunotherapies, antiangiogenic agents, and viral gene therapies [79•].
-
Since IDH mutations are highly prevalent and specific in AA and enzymatic defects are attractive candidates for therapeutic intervention, IDH-related therapy may play a novel role in the future treatment of AA [33•, 80]. However, the oncogenic mechanism associated with IDH mutations is yet to be determined and currently no therapy is available that specifically targets IDH mutations.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Stupp R, Reni M, Gatta G, Mazza E, Vecht C. Anaplastic astrocytoma in adults. Crit Rev Oncol Hematol. 2007;63(1):72–80.
Tanaka S, Meyer FB, Buckner JC, Uhm JH, Yan ES, Parney IF. Presentation, management, and outcome of elderly patients with newly-diagnosed anaplastic astrocytoma. J Neurooncol. 2012;110(2):227–35.
Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. Neuro Oncol. 2012;14 Suppl 5:v1–49.
Prados MD, Gutin PH, Phillips TL, Wara WM, Larson DA, Sneed PK, et al. Highly anaplastic astrocytoma: a review of 357 patients treated between 1977 and 1989. Int J Radiat Oncol Biol Phys. 1992;23(1):3–8.
Mechtler L. Neuroimaging in neuro-oncology. Neurol Clin. 2009;27(1):171–201. ix.
Thomas TL, Stolley PD, Stemhagen A, Fontham ET, Bleecker ML, Stewart PA, et al. Brain tumor mortality risk among men with electrical and electronics jobs: a case-control study. J Natl Cancer Inst. 1987;79(2):233–8.
Thomas TL, Stewart PA, Stemhagen A, Correa P, Norman SA, Bleecker ML, et al. Risk of astrocytic brain tumors associated with occupational chemical exposures. A case-referent study. Scand J Work Environ Health. 1987;13(5):417–23.
Heineman EF, Cocco P, Gomez MR, Dosemeci M, Stewart PA, Hayes RB, et al. Occupational exposure to chlorinated aliphatic hydrocarbons and risk of astrocytic brain cancer. Am J Ind Med. 1994;26(2):155–69.
Coble JB, Dosemeci M, Stewart PA, Blair A, Bowman J, Fine HA, et al. Occupational exposure to magnetic fields and the risk of brain tumors. Neuro Oncol. 2009;11(3):242–9.
Pace A, Bove L, Innocenti P, Pietrangeli A, Carapella CM, Oppido P, et al. Epilepsy and gliomas: incidence and treatment in 119 patients. J Exp Clin Cancer Res. 1998;17(4):479–82.
Behin A, Hoang-Xuan K, Carpentier AF, Delattre JY. Primary brain tumours in adults. Lancet. 2003;361(9354):323–31.
Moenninghoff C, Maderwald S, Theysohn JM, Kraff O, Ladd ME, El Hindy N, et al. Imaging of adult astrocytic brain tumours with 7 T MRI: preliminary results. Eur Radiol. 2010;20(3):704–13.
Jenkinson MD, Du Plessis DG, Walker C, Smith TS. Advanced MRI in the management of adult gliomas. Br J Neurosurg. 2007;21(6):550–61.
Henson JW, Gaviani P, Gonzalez RG. MRI in treatment of adult gliomas. Lancet Oncol. 2005;6(3):167–75.
Astrakas LG, Zurakowski D, Tzika AA, Zarifi MK, Anthony DC, De Girolami U, et al. Noninvasive magnetic resonance spectroscopic imaging biomarkers to predict the clinical grade of pediatric brain tumors. Clin Cancer Res. 2004;10(24):8220–8.
Walker C, Baborie A, Crooks D, Wilkins S, Jenkinson MD. Biology, genetics and imaging of glial cell tumours. Br J Radiol. 2011;84(Spec No 2):S90–106.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109.
Sarkar C, Jain A, Suri V. Current concepts in the pathology and genetics of gliomas. Indian J Cancer. 2009;46(2):108–19.
Jaros E, Perry RH, Adam L, Kelly PJ, Crawford PJ, Kalbag RM, et al. Prognostic implications of p53 protein, epidermal growth factor receptor, and Ki-67 labelling in brain tumours. Br J Cancer. 1992;66(2):373–85.
Coons SW, Johnson PC. Regional heterogeneity in the proliferative activity of human gliomas as measured by the Ki-67 labeling index. J Neuropathol Exp Neurol. 1993;52(6):609–18.
Karamitopoulou E, Perentes E, Diamantis I, Maraziotis T. Ki-67 immunoreactivity in human central nervous system tumors: a study with MIB 1 monoclonal antibody on archival material. Acta Neuropathol. 1994;87(1):47–54.
Cancer Genome Atlas Research, N. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008;455(7216):1061–8.
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321(5897):1807–12.
Brennan C. Genomic profiles of glioma. Curr Neurol Neurosci Rep. 2011;11(3):291–7. An excellent review of the genomic profiles of glioma.
Furnari FB, Fenton T, Bachoo RM, Mukasa A, Stommel JM, Stegh A, et al. Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev. 2007;21(21):2683–710.
Jaeckle KA, Decker PA, Ballman KV, Flynn PJ, Giannini C, Scheithauer BW, et al. Transformation of low grade glioma and correlation with outcome: an NCCTG database analysis. J Neurooncol. 2011;104(1):253–9.
Phillips HS, Kharbanda S, Chen R, Forrest WF, Soriano RH, Wu TD, et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell. 2006;9(3):157–73.
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, et al. Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med. 2000;343(19):1350–4.
Gilbert MR. RTOG 0525: a randomized Phase III trial comparing standard adjuvant temozolomide with a dose-dense schedule in newly diagnosed glioblastoma. J Clin Oncol. 2011;29(suppl).
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003.
Juratli TA, Kirsch M, Geiger K, Klink B, Leipnitz E, Pinzer T, et al. The prognostic value of IDH mutations and MGMT promoter status in secondary high-grade gliomas. J Neurooncol. 2012;110(3):325–33.
Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, et al. NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol. 2009;27(35):5874–80.
Gupta R, Webb-Myers R, Flanagan S, Buckland ME. Isocitrate dehydrogenase mutations in diffuse gliomas: clinical and aetiological implications. J Clin Pathol. 2011;64(10):835–44. A comprehensive review of isocitrate dehydrogenase mutations in diffuse gliomas.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–73.
Bleeker FE, Atai NA, Lamba S, Jonker A, Rijkeboer D, Bosch KS, et al. The prognostic IDH1( R132) mutation is associated with reduced NADP+-dependent IDH activity in glioblastoma. Acta Neuropathol. 2010;119(4):487–94.
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–44.
Hartmann C, Hentschel B, Wick W, Capper D, Felsberg J, Simon M, et al. Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas. Acta Neuropathol. 2010;120(6):707–18. Analysis of the role of isocitrate dehydrogenase 1 mutation status and prognosis of patients with anaplastic astrocytoma and glioblastoma.
Glantz MJ, Cole BF, Forsyth PA, Recht LD, Wen PY, Chamberlain MC, et al. Practice parameter: anticonvulsant prophylaxis in patients with newly diagnosed brain tumors. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;54(10):1886–93.
Brodie MJ, Perucca E, Ryvlin P, Ben-Menachem E, Meencke HJ, G. Levetiracetam Monotherapy Study. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Neurology. 2007;68(6):402–8.
van Breemen MS, Wilms EB, Vecht CJ. Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol. 2007;6(5):421–30.
DeAngelis LM, Posner JB, Posner JB. Neurologic complications of cancer. Contemporary neurology series. 2nd ed. Oxford: Oxford University; 2009.
Perry JR. Thromboembolic disease in patients with high-grade glioma. Neuro Oncol. 2012;14 Suppl 4:iv73–80.
Anderson F, Huang W, Sullivan C, et al. The continuing risk of venous thromboembolism following operation for glioma: findings from teh Glioma Outcomes Project. Throm Hemost. 2001;86(Suppl).
Brandes AA, Scelzi E, Salmistraro G, Ermani M, Carollo C, Berti F, et al. Incidence of risk of thromboembolism during treatment high-grade gliomas: a prospective study. Eur J Cancer. 1997;33(10):1592–6.
Perry JR, Julian JA, Laperriere NJ, Geerts W, Agnelli G, Rogers LR, et al. PRODIGE: a randomized placebo-controlled trial of dalteparin low-molecular-weight heparin thromboprophylaxis in patients with newly diagnosed malignant glioma. J Thromb Haemost. 2010;8(9):1959–65.
Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–53.
Norden AD, Bartolomeo J, Tanaka S, Drappatz J, Ciampa AS, Doherty LM, et al. Safety of concurrent bevacizumab therapy and anticoagulation in glioma patients. J Neurooncol. 2012;106(1):121–5.
Levin JM, Schiff D, Loeffler JS, Fine HA, Black PM, Wen PY. Complications of therapy for venous thromboembolic disease in patients with brain tumors. Neurology. 1993;43(6):1111–4.
Nicolas JM, Collart P, Gerin B, Mather G, Trager W, Levy R, et al. In vitro evaluation of potential drug interactions with levetiracetam, a new antiepileptic agent. Drug Metab Dispos. 1999;27(2):250–4.
Hall WA, Galicich W, Bergman T, Truwit CL. 3-Tesla intraoperative MR imaging for neurosurgery. J Neurooncol. 2006;77(3):297–303.
Liang D, Schulder M. The role of intraoperative magnetic resonance imaging in glioma surgery. Surg Neurol Int. 2012;3 Suppl 4:S320–7.
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V. Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol. 2011;12(11):997–1003.
Andersen AP. Postoperative irradiation of glioblastomas. Results in a randomized series. Acta Radiol Oncol Radiat Phys Biol. 1978;17(6):475–84.
Douglas BG, Worth AJ. Superfractionation in glioblastoma multiforme–results of a phase II study. Int J Radiat Oncol Biol Phys. 1982;8(10):1787–94.
Hochberg FH, Pruitt A. Assumptions in the radiotherapy of glioblastoma. Neurology. 1980;30(9):907–11.
Salazar OM, Rubin P, Feldstein ML, Pizzutiello R. High dose radiation therapy in the treatment of malignant gliomas: final report. Int J Radiat Oncol Biol Phys. 1979;5(10):1733–40.
Shapiro WR, Green SB, Burger PC, Mahaley Jr MS, Selker RG, VanGilder JC, et al. Randomized trial of three chemotherapy regimens and two radiotherapy regimens and two radiotherapy regimens in postoperative treatment of malignant glioma. Brain Tumor Cooperative Group Trial 8001. J Neurosurg. 1989;71(1):1–9.
Walker MD, Alexander Jr E, Hunt WE, MacCarty CS, Mahaley Jr MS, Mealey Jr J, et al. Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg. 1978;49(3):333–43.
Walker MD, Strike TA, Sheline GE. An analysis of dose-effect relationship in the radiotherapy of malignant gliomas. Int J Radiat Oncol Biol Phys. 1979;5(10):1725–31.
Wallner KE, Galicich JH, Krol G, Arbit E, Malkin MG. Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int J Radiat Oncol Biol Phys. 1989;16(6):1405–9.
Tsao MN, Mehta MP, Whelan TJ, Morris DE, Hayman JA, Flickinger JC, et al. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for malignant glioma. Int J Radiat Oncol Biol Phys. 2005;63(1):47–55.
Prados MD, Wara WM, Sneed PK, McDermott M, Chang SM, Rabbitt J, et al. Phase III trial of accelerated hyperfractionation with or without difluromethylornithine (DFMO) versus standard fractionated radiotherapy with or without DFMO for newly diagnosed patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2001;49(1):71–7.
Keime-Guibert F, Napolitano M, Delattre JY. Neurological complications of radiotherapy and chemotherapy. J Neurol. 1998;245(11):695–708.
Freeman JE, Johnston PG, Voke JM. Somnolence after prophylactic cranial irradiation in children with acute lymphoblastic leukaemia. Br Med J. 1973;4(5891):523–5.
Hoffman WF, Levin VA, Wilson CB. Evaluation of malignant glioma patients during the postirradiation period. J Neurosurg. 1979;50(5):624–8.
Klein M, Heimans JJ, Aaronson NK, van der Ploeg HM, Grit J, Muller M, et al. Effect of radiotherapy and other treatment-related factors on mid-term to long-term cognitive sequelae in low-grade gliomas: a comparative study. Lancet. 2002;360(9343):1361–8.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96.
Stewart LA. Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet. 2002;359(9311):1011–8.
Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ. Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol. 2008;9(5):453–61.
Fink J, Born D, Chamberlain MC. Pseudoprogression: relevance with respect to treatment of high-grade gliomas. Curr Treat Options Oncol. 2011;12(3):240–52.
Brandes AA, Franceschi E, Tosoni A, Blatt V, Pession A, Tallini G, et al. MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol. 2008;26(13):2192–7.
Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012;13(7):707–15. Prospective study that demonstrated that temozolomide chemotherapy alone is equivalent to radiotherapy in patients with malignant astrocytoma.
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS, et al. Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol. 1999;17(9):2762–71.
Perry JR, Belanger K, Mason WP, Fulton D, Kavan P, Easaw J, et al. Phase II trial of continuous dose-intense temozolomide in recurrent malignant glioma: RESCUE study. J Clin Oncol. 2010;28(12):2051–7. Prospective study demonstrating that continuous dose-intense temozolomide is an effective treatment option for some patients with recurrent anaplastic astrocytoma.
Desjardins A, Reardon DA, Herndon 2nd JE, Marcello J, Quinn JA, Rich JN, et al. Bevacizumab plus irinotecan in recurrent WHO grade 3 malignant gliomas. Clin Cancer Res. 2008;14(21):7068–73.
Kreisl TN, Zhang W, Odia Y, Shih JH, Butman JA, Hammoud D, et al. A phase II trial of single-agent bevacizumab in patients with recurrent anaplastic glioma. Neuro Oncol. 2011;13(10):1143–50. Prospective study demonstrating the improvement in quality of life and neurologic function in anaplastic astrocytoma patients treated with bevacizuamb.
Adkison JB, Tome W, Seo S, Richards GM, Robins HI, Rassmussen K, et al. Reirradiation of large-volume recurrent glioma with pulsed reduced-dose-rate radiotherapy. Int J Radiat Oncol Biol Phys. 2011;79(3):835–41.
Fogh SE, Andrews DW, Glass J, Curran W, Glass C, Champ C, et al. Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol. 2010;28(18):3048–53.
Quant EC, Drappatz J, Wen PY, Norden AD. Recurrent high-grade glioma. Curr Treat Options Neurol. 2010;12(4):321–33. An excellent review of treatment options for patients with recurrent malignant glioma.
Guo C, Pirozzi CJ, Lopez GY, Yan H. Isocitrate dehydrogenase mutations in gliomas: mechanisms, biomarkers and therapeutic target. Curr Opin Neurol. 2011;24(6):648–52.
Conflict of Interest
Sean A. Grimm has served on an advisory board and received grant support from Genentech.
Thomas J. Pfiffner declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grimm, S.A., Pfiffner, T.J. Anaplastic Astrocytoma. Curr Treat Options Neurol 15, 302–315 (2013). https://doi.org/10.1007/s11940-013-0228-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-013-0228-7