Opinion statement
To date, there are no approved and established pharmacologic treatment options for tauopathies, a very heterogenous group of neuropsychiatric diseases often leading to dementia and clinically diagnosed as atypical Parkinson syndromes. Among these so-called Parkinson plus syndromes are progressive supranuclear palsy (PSP), also referred to as Steele-Richardson-Olszewski syndrome; frontotemporal dementia (FTD); and corticobasal degeneration (CBD). Available treatment strategies are based mainly on small clinical trials, miscellaneous case reports, or small case-controlled studies. The results of these studies and conclusions about the efficacy of the medication used are often contradictory. Approved therapeutic agents for Alzheimer´s dementia, such as acetylcholinesterase inhibitors and memantine, have been used off-label to treat cognitive and behavioral symptoms in tauopathies, but the outcome has not been consistent. Therapeutic agents for the symptomatic treatment of Parkinson’s disease (levodopa or dopamine agonists) are used for motor symptoms in tauopathies. For behavioral or psychopathological symptoms, treatment with antidepressants—especially selective serotonin reuptake inhibitors—could be helpful. Antipsychotics are often not well tolerated because of their adverse effects, which are pronounced in tauopathies; these drugs should be given very carefully because of an increased risk of cerebrovascular events. In addition to pharmacologic options, physical, occupational, or speech therapy can be applied to improve functional abilities. Each pharmacologic or nonpharmacologic intervention should be fitted to the specific symptoms of the individual patient, and decisions about the type and duration of treatment should be based on its efficacy for the individual and the patient’s tolerance. Currently, no effective treatment is available that targets the cause of these diseases. Current research focuses on targeting tau protein pathology, including pathologic aggregation or phosphorylation; these approaches seem to be very promising.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
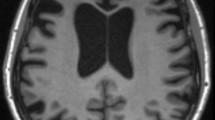
Current research in neuropathology suggests that tauopathies display a characteristic pattern of brain atrophy, such as frontotemporal or striatonigral degeneration, disintegration, and protein accumulation of tau-positive neurofibrillary tangles (NFTs) and inclusions, as well as non-tau forms with inclusions positive for ubiquitin and/or TDP-43 or α-synuclein [1, 2, 3•]. In tau-positive proteinopathies (tauopathies), glycogen synthase kinase 3β (GSK-3β)–dependent phosphorylation and aggregation of tau protein [4], a microtubule-associated protein, leads to the characteristic pathologic findings [5] and is associated with a typical clinical syndrome of cognitive and behavioral symptoms, with delayed motor symptoms in some cases. In the daily clinical routine these diseases appear as cognitive impairment, dementia with or without behavioral and psychopathological abnormalities like apathy and disinhibition [4], and parkinsonism, such as rigidity, gait disturbance, and postural instability.
Frontotemporal lobar degeneration
Traditionally, frontotemporal lobar degeneration (FTLD) is described mainly in three subtypes, depending on the leading clinical symptoms. Most common is frontotemporal dementia (FTD) with behavioral (bvFTD) and language-dominant (lvFTD) variants, followed by primary progressive aphasia (PPA) and semantic dementia [6, 7]. All types show a typical atrophy pattern in frontal and temporal brain regions. Leading symptoms are behavioral and psychopathological abnormalities like apathy, depression, disinhibition, language or speech deficits, and cognitive impairment with or without motor symptoms.
There is no clear evidence about treatment based on approved pharmacologic options. Assuming the presence of a serotonergic deficit in FTD, treatment with selective serotonin reuptake inhibitors (SSRIs), such as sertraline, paroxetine, and fluvoxamine, may improve behavioral and psychiatric symptoms but not cognitive impairment [8]. Atypical antipsychotics can help in patients with agitation, aggressive behavior, and psychotic reactions [9]. In a recently published small single-dose study with citalopram followed by a 6-week open-label extension, patients showed improvement in behavioral symptoms after treatment [10]. Acetylcholinesterase inhibitors (AChEIs) are well established in Alzheimer’s dementia (AD), but there is no evidence for efficacy in FTD patients [4]. Study results and observed effects are often contradictory [11], so their use in the daily clinical routine cannot be recommended. For memantine, an N-methyl-D-aspartate and serotonin-3 receptor antagonist, which has good efficacy in AD and neuroprotective characteristics [12], available data indicate that its application in FTD may improve behavioral symptoms [4] and increase metabolic activity in strategic brain areas [13]. In a case report, Fellgiebel et al. showed a significant and stable improvement of clinical symptoms during treatment with 10 mg/day of aripiprazole, with a significant increase in frontal glucose metabolism [14].
Progressive supranuclear palsy
Progressive supranuclear palsy (PSP) presents clinically with postural instability, frequent falls, supranuclear gaze palsy, and cognitive impairment of a subcortical pattern [15]. Disease-modifying or efficient symptomatic treatments are not yet available, so occupational, physical, and speech therapy is recommended [16]. As PSP is a Parkinson plus syndrome, treatment with levodopa appears to be promising, but only 20–40% of all PSP patients respond to it [17]. Serotonergic drugs can help to improve depressive symptoms but are ineffective in the treatment of cognitive and other symptoms of PSP [18]. In a small case study with five patients, rivastigmine produced a slight improvement in cognitive symptoms in patients with PSP [19].
Corticobasal degeneration
Corticobasal degeneration (CBD) is a tauopathy with a pattern of cortical and nigral brain atrophy. Leading clinical signs are unilateral or asymmetric parkinsonism, cortical sensory neglect, dementia with frontal executive deficits, aphasia, apraxia, and depression [2]. There is a clinical and pathological overlap between AD, FTD, PSP, and CBD, so the diagnosis of CBD is extremely challenging [20•, 21••]. Rivastigmine can help to improve neuropsychiatric symptoms, but it does not affect cognition [22]. Treatment with levodopa is ineffective because of unresponsiveness. So far, no available treatment addresses the cause of CBD [21••].
Treatment
Diet and lifestyle
-
Though a variety of epidemiologic studies suggest that diets rich in antioxidants and anti-inflammatory agents are associated with a reduced risk of age-related neurodegenerative diseases such as Parkinson’s disease and AD, no approved lifestyle-related recommendations exist for the prevention or therapy of neurodegenerative diseases.
-
Furthermore, there are no specific dietary recommendations for FTLD, PSP, or CBD. Assuming that mitochondrial dysfunction from oxidative stress may be a common pathological mechanism in other neurodegenerative diseases, such as Parkinson’s disease, AD, and amyotrophic lateral sclerosis (ALS) [23, Class IV], neuroprotective approaches with creatine and coenzyme Q10 supplementation are being tested for their neuroprotective efficacy in a series of in vitro and in vivo studies.
-
More general recommendations support a fiber-rich, well-balanced diet that is low in saturated fat and cholesterol, with sufficient fluid intake. Patients with all types of clinical dementia may suffer from poor appetite for various reasons (e.g., difficulties with chewing and swallowing, constipation, physical discomfort, or lack of exercise), leading to weight loss. Caregivers should be aware of changes in eating habits and encourage adequate nutrition.
Pharmacologic treatment
-
None of the following drugs have been approved by the US Food and Drug Administration (FDA) for any indication in FTD, CBD, or PSP. Nevertheless, their off-label use has been suggested on the basis of clinical experience, expert opinion, and small clinical trials.
Selective serotonin reuptake inhibitors (SSRIs)
-
A variety of autopsy, imaging, and CSF studies have shown serotonergic dysfunction in FTD. In open-label studies or case reports, SSRIs decreased neuropsychiatric symptoms such as disinhibition and repetitive or stereotypical behavior. SSRIs also may be helpful for food craving, inappropriate sexual behavior, and aggression [11] in FTD. Their antidepressive effect is useful to treat depressive symptoms in FTD, PSP, CBD, and dementia with Lewy bodies (DLB).
Sertraline
In 2005, Mendez et al. [24, Class III] showed that sertraline decreased verbal and motor stereotypies (including rubbing behaviors, self-injurious acts, and perseverations) in 18 patients with FTD, compared with 18 healthy controls. In a case report, Hargrave et al. [25, Class IV] showed a significant reduction of depressive symptoms in CBD (as measured with the Geriatric Depression Scale [GDS]) with the use of a stable dose of 50 mg per day of sertraline.
- Standard dosage :
-
The approved standard dose for depression or obsessive-compulsive disorder, for example, ranges from 50–200 mg per day. Sertraline is given once a day and initiated with 25 mg; the dose is increased in steps of 50 mg per week. Depending on the clinical aspect, the same dose range may be useful to treat depressive symptoms or stereotypical behavior in FTD or depressive symptoms in other Parkinson plus syndromes.
- Contraindications :
-
Sertraline must not be given with monoamine oxidase inhibitors (MAOIs) because of the risk of a serotonin syndrome, which is characterized by hyperthermia, autonomic instability, rigidity and myoclonus, fluctuations of vital signs, and mental status changes with possible progression to delirium and coma. Comedication with pimozide or disulfiram is also contraindicated.
- Main drug interactions :
-
Use with an MAOI may lead to an increase in serotonin levels, with the risk of serotonin syndrome. Sertraline inhibits coenzyme CYP2D6, leading to an increase of its substrates (e.g., metoprolol, haloperidol, desipramine, or imipramine).
- Main side effects :
-
Dry mouth, diarrhea, nausea, loss of appetite, headache, somnolence, insomnia, tremor, agitation, sexual dysfunction.
- Special points :
-
Withdrawal or discontinuation of sertraline may lead to characteristic side effects such as emotional lability, irritability, nervousness, agitation, dizziness, and headache for 5 to 8 days after disruption. During the initial weeks of the treatment, all patients being treated with antidepressants should be monitored carefully for clinical worsening, suicidality, and unusual changes in behavior.
Paroxetine
A few studies have reported that paroxetine may be used to treat repetitive and stereotypical behavior in FTD. (For an overview, see reference [11].) In a small, 14-month randomized study, paroxetine (20 mg/d) showed significant advantages with regards to behavioral symptoms, compared with 1,200 mg/day of piracetam [26, Class III]. In a study by Deakin et al. [27, Class II], 40 mg per day of paroxetine did not improve behavioral symptoms in FTD, and cognitive impairments were increased in patients with frontal variant FTD (fvFTD). Few studies have shown an improvement of motor symptoms or speech impairment in patients with Parkinson’s disease or multiple system atrophy [28, Class III], and this may also be the case for other Parkinson plus syndromes. Yet results seem to be contradictory for motor symptoms in Parkinson’s disease, and the antidepressive effects of paroxetine may resemble those produced by other SSRIs [29, Class II].
- Standard dosage :
-
20–40 mg per day, with a single dose in the morning.
- Contraindications :
-
Paroxetine should not be used in combination with an MAOI (including the antibiotic linezolid) or triptans because of the risk of serotonin syndrome.
- Main drug interactions :
-
Risk of a serotonin syndrome in combination with other SSRIs or SNRIs. Paroxetine is metabolized by cytochrome CYP2D6. Patients treated with paroxetine and tamoxifen have an increased risk for death from breast cancer. Other interactions have been reported for pimozide, thioridazine, tryptophan, or warfarin.
- Main side effects :
-
Asthenia, nausea, diarrhea, constipation, somnolence, headache, dry mouth, sweating, sexual dysfunction.
- Special points :
-
Among the SSRIs, paroxetine has the highest risk for a withdrawal syndrome. Symptoms can be nausea, dizziness, vertigo, insomnia, and anxiety.
Fluvoxamine
In a 12-week open-label study, Ikeda et al. administered fluvoxamine to 16 FTD patients. Scores on the Neuropsychiatric Inventory (NPI) and the Stereotypy Rating Inventory showed significant improvement in behavioral symptoms [30, Class III].
- Standard dosage :
-
Starting dosage is 50 mg per day. The therapeutic range is 100–300 mg per day. Doses exceeding 100 mg per day should be divided into two parts.
- Contraindications :
-
Coadministration of MAOIs, tizanidine, thioridazine, alosetron, or pimozide with fluvoxamine is contraindicated.
- Main drug interactions :
-
Fluvoxamine inhibits several cytochrome P450 isoenzymes, leading to increased serum levels of drugs administered together: CYP1A2 (e.g., warfarin, theophylline, propranolol, caffeine, clozapine, haloperidol, olanzapine, tizanidine), CYP2C9 (e.g., warfarin), CYP3A4 (e.g., alprazolam), and CYP2C19 (e.g., omeprazole). Inhibition of CYP2D6 seems to be rather weak.
- Main side effects :
-
Asthenia, nausea, somnolence or insomnia, dizziness, nervousness, anxiousness, headache. Sexual side effects are less pronounced than with other SSRIs.
- Special points :
-
Risk of discontinuation syndrome.
Citalopram
Herrmann et al. [10, Class III] treated 15 patients with FTD suffering from severe behavioral symptoms in a 6-week, open-label study. NPI scores were decreased significantly by a daily 30-mg dose of citalopram. The symptoms that could be improved were mainly disinhibition, irritability, and depressive symptoms.
- Standard dosage :
-
Initial dosage is 10–20 mg per day, with a maximum dose of 40 mg per day.
- Contraindications :
-
As with other SSRIs, coadministration with MAOIs or triptans is contraindicated because of the potential for serotonin syndrome.
- Main drug interactions :
-
All SSRIs can increase the risk of bleeding when given together with aspirin, warfarin, NSAIDs, or other anticoagulants. Additionally, citalopram causes dose-dependent QT prolongation, so ECG monitoring is recommended when it is administered together with other medications that prolong the QT interval.
- Main side effects :
-
Side effects are rare, compared with other SSRIs. Nausea, dry mouth, somnolence, insomnia, fatigue, increased sweating, and sexual dysfunction can occur.
- Special points :
-
Risk of discontinuation syndrome.
Trazodone
-
A dose of 300 mg per day of trazodone, which inhibits serotonin reuptake and also has an antagonistic effect to the serotonin receptor (5-HT2A/C), lowered NPI scores in a 12-week, crossover, placebo-controlled study by Lebert et al. [31, Class III]. Irritability, agitation, depressive symptoms, and eating disorders were especially improved.
- Standard dosage :
-
An initial dose of 150 mg per day can be titrated up to 400 mg per day in outpatients, depending on adverse effects.
- Contraindications :
-
No specific contraindications.
- Main drug interactions :
-
Serum levels of trazodone may be lowered when coadministered with a CYP3A4 inhibitor. Trazodone may increase serum digoxin or phenytoin levels. MAOIs should not be given together with trazodone because of a lack of clinical experience and a theoretical risk for serotonin syndrome.
- Main side effects :
-
Fatigue, dizziness, drowsiness, hypotension, somnolence.
- Special points :
-
Sedating side effects of trazodone can be beneficial in agitated or restless patients. Possibility of discontinuation syndrome, similar to SSRIs.
Acetylcholinesterase inhibitors
Donepezil
Donepezil does not seem to have a beneficial effect on cognition in FTD. In a study by Mendez et al, a subgroup of FTD patients experienced worsening of disinhibition and compulsive acts [32, Class II]. However a cholinergic deficit is reported in Parkinson’s disease dementia (PDD) and DLB [22], so treatment with AChEIs like donepezil or rivastigmine is recommended in patients with PDD [33, Class IV]. A randomized, double-blind, placebo-controlled study by Litvan et al. showed a positive effect on cognition in patients with PSP, but activities of daily living and mobility scores significantly worsened [34, Class II].
- Standard dosage :
-
Start with 5 mg per day in the evening and increase dosage to 10 mg per day after 4 weeks.
- Contraindications :
-
Because of their vagotonic effects on the sinoatrial and atrioventricular node, AChEIs could lead to bradycardia and AV block, especially when administered with drugs (e.g., beta blockers) that slow heart rate.
- Main drug interactions :
-
AChEIs have a low potential for enzyme induction and interactions. Because of their mechanism, they interact with anticholinergic drugs (antagonistic effect) and cholinergic agents (synergistic effect).
- Main side effects :
-
Nausea, diarrhea, insomnia, fatigue, vomiting, muscle cramps, anorexia.
- Special points :
-
Not recommended for FTD or PSP. No reliable data for CBD.
Rivastigmine
Rivastigmine can be administered in two forms, capsules or a transdermal patch. Compared with capsules, the transdermal system has a better pharmacokinetic profile, with lower peak plasma concentrations and reduced fluctuations leading to reduced gastrointestinal side effects. In an open-label study by Moretti et al., 20 FTD patients received 3–9 mg per day of rivastigmine [35, Class III]. After 12 months, behavioral and depressive symptoms were reduced, as were scores measuring caregiver burden. Similar to donepezil, a few studies report a beneficial effect of rivastigmine treatment in PDD [36, Class I] and DLB [37, Class I]. There are no data on rivastigmine in CBD. Recent clinical observations by Liepelt et al. of slight cognitive improvements in PSP patients after rivastigmine therapy may justify controlled studies in these patients [19, Class III].
- Standard dosage :
-
Capsules: 6–12 mg/day (3–6 mg given twice a day [BID]). The starting dose is 1.5 mg BID, to be increased to 3 mg BID after at least 2 weeks if the dose is well tolerated. Maximum dosage is 6 mg BID.
Transdermal system: Treatment is started with 4.6 mg per 24 hours. If the treatment is well tolerated, the dose can be increased to 9 mg per 24 hours after at least 4 weeks.
- Contraindications :
-
Bradycardia and AV block, sick sinus syndrome.
- Main drug interactions :
-
No major interactions with cytochrome P450 isoenzymes. Interference with anticholinergic drugs, synergistic effects with cholinergic drugs.
- Main side effects :
-
Nausea, vomiting (especially during the titration phase), diarrhea, loss of appetite, weight loss, abdominal pain, dizziness. Because of its cholinergic and vagotonic effect, the heart rate can be decelerated.
- Special points :
-
Because of its gastrointestinal side effects, treatment should be reinitiated with the lowest daily dose if the drug is discontinued for more than 3 days.
Galantamine
In 2008, Kertesz et al. [38, Class III] failed to find an improvement in behavior or language in a partly randomized, placebo-controlled study with galantamine (16–24 mg/day) in 36 patients with bvFTD or PPA. A trend of efficacy was shown in PPA patients.
- Standard dosage :
-
Starting dose is 8 mg per day. Increase to a maintenance dose of 16 mg per day after 4 weeks, depending on tolerability and clinical benefit. A further increase to 24 mg per day is possible. Administration should be twice a day.
- Contraindications :
-
Bradycardia and AV block.
- Main drug interactions :
-
CYP2D6 or CYP3A4 inhibitors (e.g., coadministration of ketoconazole or paroxetine) may increase serum levels of galantamine.
- Main side effects :
-
Side effects are dose dependent and include nausea, diarrhea, vomiting, weight loss, anorexia.
Memantine
-
In an open-label, 6-month treatment study with memantine (20 mg/day) in 16 patients with bvFTD and temporal variant FTD (tvFTD), behavior did not improve and cognitive function worsened [39, Class III]. A more recent study in bvFTD also failed to find a positive effect in the memantine group, but the daily dose was only 10 mg per day [40, Class II]. Clinical Global Impression of Change (CGIC) scores were slightly improved in a randomized controlled study of memantine (20 mg/day) versus placebo in 72 patients with DLB or PDD [41, Class I]. Another retrospective chart review also failed to show more than minimal effects on the Mini-Mental State Exam (MMSE) and behavior scores in FTD patients. A recent study by Boxer et al. [42, Class III] in patients with FTD, semantic dementia (SD), or PPA demonstrated a pronounced benefit for PPA patients, who remained relatively stable on the Alzheimer’s Disease Assessment Scale-Cognitive (ADAS-cog) and the NPI but showed a decline in the Unified Parkinson's Disease Rating Scale (UPDRS)-motor scale; patients with FTD or SD did not benefit from memantine. To our knowledge, there are no studies on memantine treatment in patients with PSP or CBD.
- Standard dosage :
-
Start with 5 mg per day and increase by 5 mg every week to a dosage of 20 mg per day, given as a single dose in the morning.
- Contraindications :
-
No contraindications.
- Main drug interactions :
-
Memantine has no substantial effect on the cytochrome 450 isoenzymes. Because of its renal elimination, plasma levels of coadministered drugs that also have renal elimination may be altered.
- Main side effects :
-
Memantine is generally well tolerated. In randomized controlled trials, no adverse events have occurred with a frequency of more than 5% or twice the placebo rate. In rare cases, insomnia (especially if the drug is administered before bedtime), confusion, dizziness, headache, agitation, or hallucinations have been reported.
Antipsychotics
-
In our experience, antipsychotics should be used very carefully because of potential severe adverse effects (e.g., worsening of motor symptoms, cardiovascular side effects, etc.) and higher risk of cerebrovascular incidents. If their use is necessary because of severe aggression, agitation, or psychotic symptoms, second-generation or third-generation antipsychotics should be preferred. In parkinsonian disorders, aripiprazole and quetiapine have become the most commonly used neuroleptic drugs [43, Class IV].
Aripiprazole
Aripiprazole is an atypical antipsychotic drug with partially serotonergic and dopaminergic effects besides the antipsychotic effect. It use in treating psychotic episodes in parkinsonian diseases has increased. A case report by Fellgiebel et al. [14, Class IV] showed an improvement in cognitive and behavioral symptoms of a 73-year-old patient with FTD after treatment with 10 mg per day of aripiprazole. In the same patient, the previously deteriorated regional cerebral glucose metabolism (as measured with FDG-PET) was observed to increase significantly.
- Standard dosage :
-
5 to 15 mg per day.
- Contraindications :
-
Liver dysfunction, convulsive diseases.
- Main drug interactions :
-
Drugs such as paroxetine or carbamazepine should not be used together with aripiprazole because of their CYP2D6 and CYP3A4 inhibition.
- Main side effects :
-
Fever, stiff muscles, confusion, sweating, fast or uneven heartbeats, akathisia, headache, confusion, problems with vision, speech or balance symptoms, drowsiness, dry skin, nausea, vomiting, convulsions.
- Special points :
-
It is of utmost importance to emphasize that aripiprazole is not officially approved for use in psychotic conditions accompanying dementia, so its use in these conditions is strictly off-label and an individual risk/benefit evaluation should always be performed and documented.
Quetiapine
Because of their relatively low level of extrapyramidal side effects, drugs with relatively low D2 receptor occupancy are preferred to treat agitation and psychosis in FTD [8], although no controlled trials have yet been reported.
- Standard dosage :
-
Start with 25 mg twice daily. In elderly patients, the maximum dosage should not exceed 300–400 mg per day.
- Contraindications :
-
None known.
- Main drug interactions :
-
Quetiapine may cause hypotension, so coadministration with antihypertensive drugs might increase antihypertensive effects. Serum levels of quetiapine may decrease if it is given with phenytoin or thioridazine. CYP3A inhibitors such as ketoconazole can lead to a threefold increase in the maximum plasma concentration of quetiapine.
- Main side effects :
-
Somnolence, dizziness, dry mouth, asthenia, constipation, abdominal pain, headache.
Levodopa
-
In parkinsonian diseases, the use of levodopa together with carbidopa or benserazide is very common. In tauopathies with motor symptoms, there are many nonresponders, but transient success may be achievable, justifying treatment attempts with levodopa [17, Class IV].
- Standard dosage :
-
Initial dosage is 0.5 g to 1 g daily, increased in steps not more than 0.75 mg per day every 3–7 days. Maximum dose is 8 g per day.
- Contraindications :
-
Coadministration with MAOIs.
- Main drug interactions :
-
None reported.
- Main side effects :
-
Dyskinesias (e.g., choreiform or dystonic movements), cardiac irregularities (e.g., palpitations), orthostatic hypotensive episodes, nausea, bradykinetic episodes (the "on-off" phenomenon), psychotic episodes, depression, urinary retention.
- Special points :
-
Levodopa should be administered together with benserazide or carbidopa in order to avoid peripheral conversion to dopamine, to reduce peripheral adverse effects and to improve passage across the blood–brain barrier.
Emerging therapies
-
According to the observation that tau-related pathology is a hallmark neuropathologic feature of these diseases, targeting tau pathology appears to be a promising disease-modifying approach. Valproate and lithium, which inhibit GSK-3β and thus reduce pathologic processing of neuronal tau protein, are currently being tested in clinical trials.
-
Many other experimental substances are in scientific evaluation, including tau vaccination [5]. Phosphatase inhibitors and neuroprotective compounds are also being discussed and seem to hold some promise, although there is only preclinical experimental evidence for their effects [44]. All of these efforts must be evaluated and further tested in well-designed, controlled clinical trials, potentially leading to more therapeutic options in the future.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wakabayashi K, Mori F, Tanji K, et al. Involvement of the peripheral nervous system in synucleinopathies, tauopathies and other neurodegenerative proteinopathies of the brain. Acta Neuropathol. 2010;120:1–12.
Sha S, Hou C, Viskontas IV, Miller BL. Are frontotemporal lobar degeneration, progressive supranuclear palsy and corticobasal degeneration distinct diseases? Nat Clin Pract Neurol. 2006;2:658–65.
Espay AJ, Litvan I. Parkinsonism and frontotemporal dementia: the clinical overlap. J Mol Neurosci. 2011;45(3):343–9.
Rabinovici GD, Miller BL. Frontotemporal lobar degeneration: epidemiology, pathophysiology, diagnosis and management. CNS Drugs. 2010;24:375–98.
Schneider A, Mandelkow E. Tau-based treatment strategies in neurodegenerative diseases. Neurotherapeutics. 2008;3:443–57.
Rankin KP, Mayo MC, Seeley WW, et al. Behavioral variant frontotemporal dementia with corticobasal degeneration pathology: phenotypic comparison to bvFTD with Pick’s disease. J Mol Neurosci. 2011;45(3):594–608.
Hu WT, Trojanowski JQ, Shaw LM. Biomarkers in frontotemporal lobar degenerations–progress and challenges. Prog Neurobiol. 2011;95(4):636–48.
Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66:17–22.
Piguet O, Hornberger M, Mioshi E, Hodges JR. Behavioural-variant frontotemporal dementia: diagnosis, clinical staging, and management. Lancet Neurol. 2011;10:162–72.
Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2011 Nov 4 (Epub ahead of print).
Mendez MF. Frontotemporal dementia: therapeutic interventions. Front Neurol Neurosci. 2009;24:168–78.
Kuszczyk M, Słomka M, Antkiewicz-Michaluk L, et al. 1-Methyl-1,2,3,4-tetrahydroisoquinoline and established uncompetitive NMDA receptor antagonists induce tolerance to excitotoxicity. Pharmacol Rep. 2010;62:1041–50.
Chow TW, Graff-Guerrero A, Verhoeff NP, et al. Open-label study of the short-term effects of memantine on FDG-PET in frontotemporal dementia. Neuropsychiatr Dis Treat. 2011;7:415–24.
Fellgiebel A, Müller MJ, Hiemke C, et al. Clinical improvement in a case of frontotemporal dementia under aripiprazole treatment corresponds to partial recovery of disturbed frontal glucose metabolism. World J Biol Psychiatry. 2007;8:123–6.
Hickey C, Chisholm T, Passmore MJ, et al. Differentiating the dementias. revisiting synucleinopathies and tauopathies. Curr Alzheimer Res. 2008;5:52–60.
Wenning GK, Krismer F, Poewe W. New insights into atypical parkinsonism. Curr Opin Neurol. 2011;24:331–8.
Geser F, Wenning GK. Klinik und Therapie der Multisystematrophie und progressiven supranukleären Paralyse. Psychopharmakotherapie. 2005;12:40–50. German
Barsottini OG, Felício AC, Aquino CC, Pedroso JL. Progressive supranuclear palsy: new concepts. Arq Neuropsiquiatr. 2010;68:938–46.
Liepelt I, Gaenslen A, Godau J, et al. Rivastigmine for the treatment of dementia in patients with progressive supranuclear palsy: clinical observations as a basis for power calculations and safety analysis. Alzheimers Dement. 2010;6:70–4.
Ludolph AC, Kassubek J, Landwehrmeyer BG, et al. Tauopathies with parkinsonism: clinical spectrum, neuropathologic basis, biological markers, and treatment options. Eur J Neurol. 2009;16:297–309.
Wenning GK, Litvan I, Tolosa E. Milestones in atypical and secondary Parkinsonisms. Mov Disord. 2011;26:1083–95.
Liepelt I, Maetzler W, Blaicher HP, et al. Treatment of dementia in parkinsonian syndromes with cholinesterase inhibitors. Dement Geriatr Cogn Disord. 2007;23:351–67.
Chaturvedi RK, Beal MF. Mitochondrial approaches for neuroprotection. Ann N Y Acad Sci. 2008;1147:395–412.
Mendez MF, Shapira JS, Miller BL. Stereotypical movements and frontotemporal dementia. Mov Disord. 2005;20:742–5.
Hargrave R, Rafal R. Depression in corticobasal degeneration. Psychosomatics. 1998;39:481–2.
Moretti R, Torre P, Antonello RM, et al. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. A randomized, controlled, open 14-month study. Eur Neurol. 2003;49:13–9.
Deakin JB, Rahman S, Nestor PJ, et al. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology. 2004;172:400–8.
Friess E, Kuempfel T, Modell S, et al. Paroxetine treatment improves motor symptoms in patients with multiple system atrophy. Parkinsonism Relat Disord. 2006;12:432–7.
Ceravolo R, Nuti A, Piccinni A, et al. Paroxetine in Parkinson’s disease: effects on motor and depressive symptoms. Neurology. 2000;55:1216–8.
Ikeda M, Shigenobu K, Fukuhara R, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Dement Geriatr Cogn Disord. 2004;17:117–21.
Lebert F, Stekke W, Hasenbroekx C, Pasquier F. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17:355–9.
Mendez MF, Shapira JS, McMurtray A, et al. Preliminary findings: behavioral worsening on donepezil in patients with frontotemporal dementia. Am J Geriatr Psychiatry. 2007;15:84–7.
Miyasaki JM, Shannon K, Voon V, et al. Practice parameter: evaluation and treatment of depression, psychosis, and dementia in Parkinson disease (an evidence-based review) – Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;66:966–1002.
Litvan I, Phipps M, Pharr VL, et al. Randomized placebo-controlled trial of donepezil in patients with progressive supranuclear palsy. Neurology. 2001;57:467–73.
Moretti R, Torre P, Antonello RM, et al. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21:931–7.
Emre M, Aarsland D, Albanese A, et al. Rivastigmine for dementia associated with Parkinson’s disease. N Engl J Med. 2004;351:2509–18.
McKeith I, Del Ser T, Spano P, et al. Efficacy of rivastigmine in dementia with Lewy bodies: a randomised, double-blind, placebo-controlled international study. Lancet. 2000;356:2031–6.
Kertesz A, Morlog D, Light M, et al. Galantamine in frontotemporal dementia and primary progressive aphasia. Dement Geriatr Cogn Disord. 2008;25:178–85.
Diehl-Schmid J, Förstl H, Perneczky R, et al. A 6-month, open-label study of memantine in patients with frontotemporal dementia. Int J Geriatr Psychiatry. 2008;23:754–9.
Vercelletto M, Boutoleau-Bretonnière C, Volteau C, et al. Memantine in behavioral variant frontotemporal dementia: negative results. J Alzheimers Dis. 2011;23:749–59.
Aarsland D, Ballard C, Walker Z, et al. Memantine in patients with Parkinson’s disease dementia or dementia with Lewy bodies: a double-blind, placebo-controlled, multicentre trial. Lancet Neurol. 2009;8:613–8.
Boxer AL, Lipton AM, Womack K, et al. An open-label study of memantine treatment in 3 subtypes of frontotemporal lobar degeneration. Alzheimer Dis Assoc Disord. 2009;23:211–7.
Weintraub D, Chen P, Ignacio RV, et al. Patterns and trends in antipsychotic prescribing for Parkinson disease psychosis. Arch Neurol. 2011;68:899–904.
Trojanowski JQ, Duff K, Fillit H, et al. New directions for frontotemporal dementia drug discovery. Alzheimers Dement. 2008;4:89–93.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karakaya, T., Fußer, F., Prvulovic, D. et al. Treatment Options for Tauopathies. Curr Treat Options Neurol 14, 126–136 (2012). https://doi.org/10.1007/s11940-012-0168-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-012-0168-7