Abstract
Purpose of Review
This review discusses factors affecting outcomes during ureteroscopy (URS) with laser lithotripsy (LL), explores specific clinical challenges to the efficacy of URS LL, and reviews the available literature comparing the dusting and basketing approaches to URS LL.
Recent Findings
Data show high stone-free rates with URS LL in all locations of the urinary tract and with all stone types and sizes. Recent data comparing LL with dusting versus basketing suggest higher rates of residual fragments with dusting but less utilization of ureteral access sheaths and potentially shorter operative times. Differences in postoperative complications, re-intervention rates, and other outcome parameters are not yet clear. Interpretation of published data is problematic due to variability in laser settings, follow-up intervals, and definitions for what constitutes stone-free status.
Summary
URS has overtaken shock wave lithotripsy in the last decade as the most commonly utilized surgical approach for treating urolithiasis. Two primary strategies have emerged as the most common techniques for performing LL: dusting and basketing. There is a relative paucity of data examining the difference in these techniques as it pertains to peri-operative outcomes and overall success. We attempt to synthesize this data into evidence-based and experience-based recommendations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For the past three decades, technological innovation has driven evolution in surgical management of urolithiasis. Flexible fiber-optic ureteroscopes, first introduced in the 1980s, simplified access into the ureter and kidney and allowed visualization of regions that were unreachable with the preexisting rigid and semi-rigid instruments [1]. Dual deflection mechanisms improved access to the lower and upper poles of the kidney. These ureteroscopes, however, were still relatively large with sizes up to 11.5 Fr and associated with a risk for significant complications, as high as 6.6% [2].
Extracorporeal shock-wave lithotripsy (SWL), developed in the early 1980s, was an attractive and less invasive alternative to ureteroscopy (URS) that ultimately became the mainstay of treatment for uncomplicated urolithiasis. However, harder stones (calcium oxalate monohydrate and cysteine) fragment poorly with SWL [3]. Since SWL only generates an equivalent volume of stone fragments, the patient must spontaneously pass all fragments to achieve stone-free status. This is particularly problematic for lower pole stones when the infundibulopelvic angle is acute, since gravity tends to trap fragments inferiorly. To facilitate passage of lower pole fragments after SWL, urologists developed a variety of complicated positional drainage maneuvers (i.e., total body inversion) [4,5,6]. Moreover, stone-free rates (SFR) with SWL for larger stones are low and multiple procedures are often required [7,8,9,10]. Consequently, the AUA guidelines recommend limiting SWL to stones <1.5 cm that are not located in the lower pole [11].
During the 1990s, miniaturization and improved mechanics fueled development of smaller flexible ureteroscopes with large working channels. These new instruments delivered effectors (i.e., baskets and lasers) to less accessible areas of the kidney, greatly improving the versatility of URS. Clearer visualization with digital ureteroscopes as compared to the original fiber-optic system shortened procedure times and improved safety [12, 13]. The result has been a nearly 20% drop in SWL usage among urologists in favor of URS, which has overtaken SWL in the last decade as the most commonly utilized surgical approach for urolithiasis [14]. Data demonstrating high SFR with URS for stones in all urinary tract locations have led to guideline statements encouraging URS for an expanding group of patients with various stone compositions and locations [11, 15].
Cost is a significant concern for flexible ureteroscopes, particularly due to the frequency of scope damage requiring costly repair [16,17,18]. Beyond good surgical technique, the use of less traumatic ball-tipped laser fibers may extend instrument life and lower the frequency of repairs [19]. High-quality, low-cost disposable ureteroscopes may also decrease the cost of ownership and improve general access to flexible URS [20, 21].
Intracorporeal lithotripsy can be accomplished by applying ultrasonic, mechanical, electrohydraulic, or laser energy to the stone under direct vision. Laser lithotripsy (LL) has become the recommended ureteroscopic energy source by the American Urologic Association (AUA) and the European Urologic Association (EUA) due to its compatibility with rigid, semi-rigid, and flexible ureteroscopes, relative safety with regards to adjacent tissue injury, lower risk of stone migration, and efficacy for fragmenting all types of stones.
“Basketing” and “dusting” have emerged as two alternative strategies for LL [22]. Basketing involves laser fragmentation of stones into smaller fragments using high-power, low-frequency laser pulses followed by active removal with retrieval devices, often through a ureteral access sheath (UAS). Dusting utilizes low-power, high-frequency laser pulses to melt stones into tiny, dust-like fragments that can be passed spontaneously. In this review, we will outline the important factors differentiating each technique, summarize the available data comparing them, and provide recommendations concerning the ideal clinical scenarios for each.
Physics of Laser Lithotripsy
A basic understanding of laser physics is a prerequisite to any discussion of basketing and dusting. Lasers optically or electrically excite a semi-conductive material and then oscillate photons released by uniform population inversion between two mirrors [23]. One of these mirrors is slightly less reflective, resulting in the release of a beam of photons of a specific wavelength from that end. The pulse energy is absorbed by the stone and generates an oscillating cavitation bubble, creating mechanical shockwaves that destabilize and fragment most types of stones [23].
The most commonly used laser type for LL is the holmium/YAG laser (Ho/YAG), a solid-state laser producing a 350 ms pulse with a wavelength of 2150 nm to deliver 200–4000 mJ. Small diameter fibers (≤200 μm) are widely available for this laser, allowing energy to be applied through ureteroscopes with small working channels. This maximizes scope deflection, flexibility, and irrigant flow for better maneuverability and visibility. The Ho/YAG destabilizes stones via a photothermal effect, as the energy is absorbed by water near the stone, creating a vaporization bubble around the tip of the laser that achieves stone destabilization and fragmentation. The Ho/YAG fiber tip should be kept 1 mm from ureteral and renal tissue with adequate irrigation to minimize risk of damage secondary to heat production or direct cutting action. Higher powered Ho/YAG lasers (120 W) provide greater flexibility in adjusting pulse parameters to customize the effect to an individual stone composition or technique of LL.
When purchasing a Ho/YAG laser generator for ureteroscopic LL (URS LL), recognize that total power is not necessarily the most critical feature. The versatility of a laser in treating stones is a function of three factors: total power, pulse frequency, and pulse width. Lower powered lasers (i.e., most 30 W units) are smaller, less costly, and more convenient to operate with standard 110 V power. Yet, they cannot usually support the high pulse frequencies (up to 80 Hz) used for stone dusting. Lasers of 100 and 120 W are more costly and often require 220 V power outlets, creating logistical problems in the operating room. However, the ability to use high-frequency pulses with these lasers, along with their utility for prostate surgery, may make the investment worthwhile. Another factor is the ability to control pulse width, a feature limited to a subset of 100–120 W units. Pulse width adjustment can minimize “retropulsion” which refers to backward bouncing movement of a stone in response to LL. Less retropulsion may make URS LL more convenient and efficient in the ureter, resulting in less “chasing” of the stone proximally.
Challenges to the Interpretation of the Literature
Investigators focus on SFR when comparing different forms of lithotripsy. However, SFR criteria are not standardized across studies and can differ greatly depending on the length of follow-up and the imaging modality. Non-contrast CT (NCCT) is most sensitive for stone detection and is particularly superior to other modalities such as ultrasound and plain abdominal films (KUB) for detecting stones <4 mm [24]. Ultrasound, in experienced hands, provides accurate information about renal stone burden but is poor for visualizing ureteral calculi, particularly in obese patients. The operator-dependent nature of ultrasound can lead to inconsistencies in determining SFR after lithotripsy. While inexpensive and convenient, KUB cannot detect radiolucent stones and may miss residual stones obscured by overlying abdominal contents, bowel gas, or stool.
SFR does not always reflect complete clearance of all stone fragments. Published studies use varying definitions of stone-free that include residual stones ranging from 1 to 4 mm. Variability in patient factors such as anatomy, stone location, stone composition, total stone burden, compliance (either with post-procedure medication and/or imaging follow-up), equipment, and surgeon skill/persistence can complicate comparisons across studies.
Factors Affecting Stone-Free Rate in Ureteroscopic Laser Lithotripsy
URS LL results in an excellent SFR for stones at all levels of the upper urinary tract [25,26,27]. However, two categories of patients warrant closer examination: those with stones >2 cm and those with lower pole calyceal stones [28].
For stones >2 cm, percutaneous nephrolithotomy (PCNL) is considered first-line therapy due to superior SFR [11, 29]. URS LL can be considered when patients are poor candidates for PCNL due to medical comorbidities, anatomic challenges to percutaneous access, or an inability to stop anticoagulation. Staged URS for large stones may be an option but can require several lengthy procedures. Multiple long ureteroscopic procedures may also carry an increased risk of infectious complications [30]. A 2010 meta-analysis of URS LL management of stones >2 cm found a 95% SFR after a mean of 1.46 procedures, but SFR definitions were not standardized across studies, and the follow-up interval was ≤3 months [31]. More recently, Al-Qahtani et al. and Cohen et al. reported SFR of 97 and 87% at 1 and 3 months, respectively, with mean 1.6 procedures [32, 33]. Hyams et al. investigated single-stage URS procedures and found SFR of 63% (no fragments >2 mm) or 47% (fragment-free) at 2-month follow-up [34].
Ureteroscopic access to lower pole stones poses challenges due to the greater deflection required. Instruments in the working channel can decrease deflection as much as 10–45° and limit clearance of residual fragments [35]. Retained fragments in the lower pole calyx may be less likely to pass into the renal pelvis due to gravity, especially in patients with an acute infundibulopelvic angle [36, 37]. Despite these factors, URS LL has achieved high SFR in the treatment of lower pole stones with lower retreatment rates compared to SWL (8 vs 60–85%) [38,39,40]. URS also allows repositioning of stones into upper pole calyces which can facilitate spontaneous passage of residual fragments created by LL.
Basketing
Basketing involves using URS LL to break stones into 2–4-mm fragments that can be actively removed using a retrieval device (usually a coaxial basket or grasper) rather than left in situ for spontaneous passage. This theoretically allows for complete stone removal under direct visualization. Retrieval also provides stone samples for chemical analysis, helping guide lifestyle recommendations and medical management to attenuate the ∼52% 10-year risk of stone recurrence in first-time formers [41,42,43,44].
The authors utilize higher power (0.8 to 1.2 J) and lower frequency (8–12 Hz) laser settings for basketing. These settings can fracture stones into larger fragments but also create significant stone movement and retropulsion [45]. Also, the high power of each individual pulse can potentially damage the laser fiber and contributes to “burn back,” the process by which the tip of the fiber becomes ablated during lithotripsy [46].
Unfortunately, there is a relative paucity of data comparing URS LL with basketing settings and active retrieval to in situ passage of residual fragments. In the only randomized controlled trial comparing the two strategies, Shatloff et al. treated 60 patients with ureteral stones by either active retrieval or more vigorous fragmentation to <2 mm followed by spontaneous passage. Stones were of mean size 9 and 10 mm, respectively. The number of ER visits was significantly higher (30 vs 3%, p < 0.01) at 1 month post-operation for the spontaneous passage treatment arm. Operative time was equivalent between the two arms at a mean of 26 min. Other measures including SFR (100% in the retrieval arm, 87% in the spontaneous passage arm) were not significantly different [47]. In a prospective study investigating active stone retrieval, Portis et al. treated kidney and proximal ureteral stones of mean size 9.4 mm with the basketing strategy. With residual stones defined as <2 and <4 mm, they reported an SFR of 85 and 97%, respectively, at 1 month with NCCT [48]. Using a more stringent definition of SFR as measured by NCCT 1–3 months postoperatively, two retrospective studies documented SFR of 55–60% for basketing vs 35% when URS was performed with basketing laser settings but without active fragment retrieval [28, 49]. The outcome is less clear for studies examining residual stones <2 and <3 mm [50, 51].
Use of a UAS can facilitate multiple passes to accomplish complete stone removal. Available in various diameters and lengths to suit particular patients and procedures, UASs provide a protective barrier between instrumentation and the ureteral wall. They may also keep intrarenal pressures lower during URS, decreasing the risk of post-procedure systemic inflammatory response or sepsis [52,53,54]. This dilation and barrier function facilitate removal of sizable stone fragments and efficient re-entry of the ureteroscope while minimizing ureteral trauma outside of the initial placement of the device. UASs also decrease operative time and double durability of ureteroscopes by protecting the tip and preventing kinking within the ureter [55, 56]. In cases with larger stone burdens, the use of UASs virtually eliminates the risk of scope entrapment by distally migrated stone fragments caught between the ureteroscope and ureteral wall.
Two studies have compared SFR in URS LL with and without UAS usage. In a retrospective analysis for stones of mean size 1–2 cm, Berquet et al. found that placing a UAS was not associated with a significant difference in SFR at any anatomic location when residual fragments were defined as <3 mm assessed by CT or US at 1 and 3 months [57]. In a comparable study of UAS usage for stones ranging from 5 to 10 mm, L’Esperance et al. found a statistically significant overall improvement in renal stone SFR with UAS usage at 2 months by IV urography (p = 0.04) [58]. Given limited comparative investigations, a definitive statement on SFR outcomes with UAS usage is not possible.
Potential intraoperative and postoperative complications specific to UAS use exist. Ureteral injury can result from shearing injury during UAS insertion into a narrow ureter or from ureteral wall ischemia [59]. A 2013 prospective study reported that 46.5% of 359 patients had visible ureter damage graded on a 4-point scale after 12 or 14 Fr UAS placement [60•]. This included 86% with mucosal injury, 10% with damage through the mucosa to the smooth muscle, and 3.3% with full-thickness ureteral injury. The factor with the greatest association ureteral injury with UAS use was the absence of preoperative double-J stent placement. Thus, pre-stenting remains a valid consideration in cases of difficult UAS placement or known damage and before URS in patients with prior complications [11]. The impact of the observed damage on future stricture development is unknown due to insufficient follow-up, although one study reported no increased risk when compared to no UAS usage [61]. Also, a 2015 prospective global collaboration study on 2239 patients comparing outcomes with and without UAS found no significant difference in intra-operative bleeding or ureteral perforation, nor in postoperative bleeding or infection [62]. However, a retrospective study including 298 URS LL patients found an association between increasing UAS diameter and younger age with unplanned symptomatic encounters [63]. These data may be representative of more recent widespread use of UASs and should serve as a reminder to approach UAS usage and sizing thoughtfully with awareness of the potential for injury.
Additional potential downsides to the basketing technique include the added cost of retrieval devices, increased technical challenge to manually remove stones, potentially longer operative times, and surgeon frustration due to the tedium of sequentially basketing many fragments. None of these factors have been studied.
Dusting
Dusting is a URS LL technique employing lower energy laser pulses (the authors recommend 0.2–0.4 J) at a much higher pulse rate (40–80 Hz), with the goal of reducing a stone to fine dust that can be spontaneously passed in a pain-free manner. These settings require a more powerful laser (100–120 W), which may not be available at all institutions. The difference between basketing and dusting lies primarily in the size of the residual fragments generated. With dusting, the stone is “painted” with the laser energy and dissolved into fine dust. Ideally, the dusting approach results in no residual fragments of a size that might require basket extraction. Larger fragments inadvertently created during dusting can be treated with similar settings by using a “popcorn technique.” This involves treating multiple small fragments with constant laser energy at a very high frequency directed in one area, causing the fragments to “bounce” around and contact the laser energy by chance, eventually reducing them to dust. Given the available data showing reduced SFR for lower pole stones following SWL, relocating lower pole calculi to another calyx using a basket prior to dusting could potentially improve clearance of dusting fragments [64].
Dusting has several potential advantages over basketing. It eliminates the need for multiple passes of the ureteroscope in and out of the ureter to remove multiple fragments and may lessen the need for UAS placement. Dusting may decrease the tedium of extracting a large number of stone fragments, possibly reducing operative time [65, 66]. However, stone composition may affect the efficiency of dusting. Laser settings for dusting seem to be most effective for stones under 1100 HU (i.e., calcium oxalate dihydrate, calcium phosphate, and uric acid). Dusting may be less effective for denser stones with higher HU, such as calcium oxalate monohydrate, which tend to fragment into large pieces that may require basket retrieval.
Ghani compared dusting efficiency with a 60–100-W holmium laser vs a 120-W holmium laser [67]. The more powerful laser generator enables higher-frequency settings up to 80 Hz and provides greater control over pulse width. Such versatility in laser parameters may allow for better fragmentation of various stone types and locations. This retrospective study included 63 patients with stones of mean size 11.1 and 12.2 mm for the 60–100- and 120-W groups, respectively. Settings of 0.2–0.5 J and 30–50 Hz were used with the lower powered lasers, and settings of 0.2–0.5 J and 30–80 Hz were utilized for the higher powered lasers. Popcorn settings of 0.5 J and 80 Hz were also utilized in the 120 W arm. The 120-W group had a statistically significant higher SFR as defined by zero fragments (66% in 120 W vs 39%, p < 0.05). However, when SFR was defined using a 2-mm threshold, the advantage for 120 W lost statistical significance. UAS usage was similar for both groups.
Dusting Versus Basketing
While there is limited published outcome data evaluating the practice of dusting, several abstracts have been presented at national and international meetings. The largest study to date is a multi-institutional, prospective trial by the Endourologic Disease Group for Excellence (EDGE) consortium. Final data has recently been made available but without statistical analysis [68••]. Across 8 centers, 152 patients with radio-opaque kidney stones 5–20 mm in size were treated with dusting (n = 70) or basketing (n = 82). Stone size was larger in the dusting group (122.6 ± 88.6 vs 82.3 ± 59 mm2), and densities for the dusting and basketing arms were 786 ± 362.8 and 978 ± 1150.9 HU, respectively. Three institutions involved utilized dusting and the remaining five institutions utilized basketing. Data collected included complete SFR by KUB and US within 3 months, operative time, UAS usage, and laser power. All patients were stented postoperatively and given 1 month of alpha-adrenergic blockers. SFR was higher in the basketing arm at 86.3 vs 59.2% in the dusting arm. There were no differences in stone type, rates of readmission, secondary procedures, symptoms, complications, or postoperative creatinine. In the dusting arm, 21.7% of patients had residual stones <2 mm, 10.9% 2–4 mm, and 12.5% >4 mm. Almost two-thirds had passed the residual stones between surgery and follow-up. In the basketing arm, 9.8, 7.3, and 0% had residual stones of <2, 2–4, and >4 mm, respectively. While the consortium reported early data showing a mean 19-min difference in operative time favoring dusting [65], final data results show a smaller difference in time favoring basketing, with a mean operation time of 57.8 ± 31.8 and 60.4 ± 141 min for basketing and dusting, respectively. As expected, UAS usage was much higher (100%) in the basketing group, compared to 18.2% in the dusting group. Total laser energy was higher in the dusting arm at 46.4 kJ, compared to 22.8 kJ in the basketing arm. Unfortunately, lack of statistical analysis limits definitive interpretation of this study in its current form.
Another randomized trial of dusting vs basketing by Gamal and Mamdoub examined 46 patients with <2-cm renal stones. Stone density was similar between the two groups [66]. Dusting and basketing settings were 0.2–0.4 J at 20–30 Hz and 1–2 J at 4–5 Hz, respectively. In contrast to the EDGE study, SFR was high and similar for both techniques (86% dusting vs 89% basketing). Also, dusting was associated with significantly lower operative time in this study (57 vs 70 min, p = 0.001). UAS usage was 0 and 100% in the dusting and basketing arms, and fewer intraoperative complications were experienced during dusting as compared to basketing. However, interpretation of this study is limited because the abstract makes no mention of a standardized follow-up period or imaging modality and does not give their definition of SFR. Importantly, the laser frequency in this study for both dusting and basketing settings is lower than typically described in the literature.
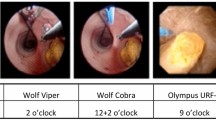
Although the lack of access to complete methods and statistical analysis limits the ability of these studies to guide management at this point, several summary points are worth making (Tables 1 and 2). There is a higher rate of residual stones with dusting in one of the studies, but without a corresponding increase in postoperative short-term complications. Concerning operative time, data from the comparative prospective studies are at odds [66, 68••]. UAS usage rates are lower and total laser energy is higher with dusting. Finally, if dusting is effective and there are no fragments to extract, stone analysis may not be obtained. These preliminary prospective studies have opened the door for comparison of the two URS LL techniques (Fig. 1).
More work is needed to compare long-term outcomes such as stone recurrence and ureteral stricture formation.
Residual Fragments
Residual fragments <4 mm have been traditionally considered insignificant, with the logic being that patients can pass these stones without significant complications [69]. However, some data challenge the validity of this concept. Streem et al. found a 43.1% rate of symptomatic events or need for secondary intervention in patients with <4-mm residual stones after surgery [70]. Subsequent comparable investigations have found similar rates of secondary intervention (21.4–54.3%) [69,71,, 71–73]. Across these studies, rates of stone growth were 10–48.7% with mean follow-up periods ranging from 12 to 40.6 months [69, 72, 74].
Rebuck et al. retrospectively studied 46 patients with ≤4 mm residual renal stones by NCCT for a mean follow-up of 18.9 months [49]. The investigators measured stone growth, stone passage, and “stone events,” defined as emergency department (ED) visits, admission, or secondary intervention for symptoms, obstruction, or removal of residual stone. Nearly 20% of patients experienced such an event, and another 21.7% of patients passed fragments symptomatically but without complication. The other 58.7% patients remained asymptomatic. Among patients with stone events requiring an additional encounter, stone growth over time was observed by NCCT: 2.5, 7.1, 5.8, and 6.3 mm at 3, 14.4, 21.8, and 26.8 months, respectively.
The EDGE Consortium attempted to study the natural history of residual stones both ≤4 and >4 mm [75•]. Stone events were defined as residual stone growth >1 mm by KUB or CT, stone passage, intervention, or complications (symptom recurrence, ED visit, admission, or acute kidney injury). They found a stone event rate of 44%. Re-intervention was required in 29%, and there was a complication rate of 15% at a mean follow-up of 16.7 months. Despite no significant difference between residual stones ≤4 and >4 mm in rates of spontaneous passage, residual fragments >4 mm were more likely to grow (p < 0.001), result in complications (p = 0.039), or experience re-interventions (p = 0.01). In further subset analysis, significantly higher rates of stone growth were seen in residual stones >2 mm when compared to ≤2 mm (p < 0.001), suggesting an incremental increase in morbidity with increasing residual fragment size. Preoperative stone size and lithotripsy technique (dusting vs basketing) were not associated with significant differences in outcomes. These data suggest that residual stones, even when ≤4 mm, should not be dismissed as clinically insignificant.
Conclusions
Over the past decade, indications for URS LL have greatly expanded to encompass larger stones and more diverse renal anatomy. New technologies such as high-frequency/high-wattage lasers, purpose-built UASs, improved endoscope optics/mechanics, and more durable laser fibers have driven urologists to push the envelope with URS. Despite somewhat impassioned debate concerning the relative risks and benefits of basketing vs dusting, post-URS SFR is still primarily a function of total stone burden and stone location.
Both basketing and dusting can provide excellent surgical outcomes for patients with urolithiasis in skilled hands. In the authors’ experience, a combination of dusting and basketing settings, tailored to an individual stone’s composition, can often be employed to provide optimal outcomes and efficiency. Today, the available data remains too limited to make firm conclusions about which technique is most advantageous and the choice remains one of surgeon preference. However, 100–120-W lasers are rapidly becoming more widely available. This provides a future opportunity for randomized controlled trials to definitively study the relative advantages and disadvantages of both URS LL techniques.
As more research examines surgical outcomes for urolithiasis, we urge investigators in this field to standardize definitions of SFR and postoperative surveillance techniques to better compare studies. This will allow better comparisons of techniques and improve recommendations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Seeger AR, Rittenberg MH, Bagley DH. Ureteropyeloscopic removal of ureteral calculi. J Urol. 1988;139(6):1180–3.
Harmon W, Sershon P, Blute M, et al. Ureteroscopy: current practice and long-term complications. J Urol. 1997;157(1):28–32.
Zhong P, Preminger G. Mechanisms of differing stone fragility in extracorporeal shock wave lithotripsy. J Endourol. 1994;8(4):263–8.
Brownlee N, Foster M, Griffith DP, Carlton Jr CE. Controlled inversion therapy: an adjunct to the elimination of gravity-dependent fragments following extracorporeal shock wave lithotripsy. J Urol. 1990;143(6):1096–8.
Pace KT, Tariq N, Dyer SJ, Weir MJRJDAH. Mechanical percussion, inversion and diuresis for residual lower pole fragments after shock wave lithotripsy: a prospective, single blind, randomized controlled trial. J Urol. 2001;166(6):2065–71.
Chiong E, Hwee ST, Kay LM, Liang S, Kamaraj R, Esuvaranathan K. Randomized controlled study of mechanical percussion, diuresis, and inversion therapy to assist passage of lower pole renal calculi after shock wave lithotripsy. Urology. 2005;65(6):1070–4.
Matlaga BR, Lansen JP, Meckley LM, Byrne TW, Lingeman JE. A systematic review and meta-analysis of randomized. Contrl Trials J Urol. 2012;188(1):130–7.
Pearle MS, Lingeman JE, Leveillee R, Kuo R, Preminger GM, et al. Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J Urol. 2005;173(6):2005–9.
Pearle MS, Nadler R, Bercowsky E, Chen C, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for management of distal ureteral calculi. J Urol. 2001;166(4):1255–60.
Salem HK. A prospective randomized study comparing shock wave lithotripsy and semirigid ureteroscopy for the management of proximal ureteral calculi. J Urol. 2009;74(6):1216–21.
Nelson CP, Pace KT, Pais VM, Pearle MS, Preminger GM. American Urological Association (AUA) guideline surgical management of stones: American Urological Association Surgical Management 2016; April:1–50.
Humphreys MR, Miller NL, Williams Jr JC, Evan AP, Munch LC, Lingeman JE. A new world revealed: early experience with digital ureteroscopy. J Urol. 2008;179(3):970–5.
Somani BK, Al-Qahtani SM, de Medina SD, Traxer O. Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology. 2013;82(5):1017–9.
Oberlin DT, Flum AS, Bachrach L, Matulewicz RS, Flury SC. Contemporary surgical trends in the management of upper tract calculi. J Urol. 2015;193(3):880–4.
Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T. EUA Guidelines on Interventional Treatment for Urolithiasis. 2016;69(3)475–82.
Ziemba JB, Matlaga BR. Understanding the costs of flexible ureteroscopy. Minerva Urol Nefrol. 2016.
Tosoian JJ, Ludwig W, Sopko N, Mullins JK, Matlaga BR. The effect of repair costs on the profitability of a ureteroscopy program. J Endourol. 2015;29(4):406–9.
Carey RI, Martin CJ, Knego JR. Prospective evaluation of refurbished flexible ureteroscope durability seen in a large public tertiary care center with multiple surgeons. Urology. 2014;84(1):42–5.
Shin RH, Lautz JM, Cabrera FJ, Shami CJ, Goldsmith ZG, Kuntz NJ, et al. Evaluation of novel ball-tip holmium laser fiber: impact on ureteroscope performance and fragmentation efficiency. J Endourol. 2016;30(2):189–94.
Doizi S, Kamphuis G, Giusti G, Andreassen KH, Knoll T, Osther PJ, et al. First clinical evaluation of a new single-use flexible ureteroscope (LithoVue): a European prospective multicentric feasibility study. World J Urol. 2016.
Leveillee RJ, Kelly EF. Impressive performance: new disposable digital ureteroscope allows for extreme lower pole access and use of 365 mum holmium laser fiber. J Endourol Case Rep. 2016;2(1):114–6.
Torricelli FC, Marchini GS, Pedro RN, Monga M. Ureteroscopy for management of stone disease: an up to date on surgical technique and disposable devices. Minerva Urol Nefrol. 2016;68(6):516–26.
Vij DR, Mahesh K. Medical applications of laser. In: Technology & Engineering. Springer: Science & Business Media; 2013.
Brisbane W, Bailey MR, Sorensen MD. An overview of kidney stone imaging techniques. Nat Rev Urol. 2016;13:654–62.
Perez Castro E, Osther PJ, Jinga V, et al. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol. 2014;66:102.
Hyams E, Monga M, Pearle MS, et al. A prospective, multi-institutional study of flexible ureteroscopy for proximal ureteral stones smaller than 2 cm. J Urol. 2015;193:165.
Mi Y, Ren K, Huang Y, et al. Flexible Ureterorenoscopy (F-URS) with Holmium laser versus Extracorporeal Shock Wave Lithotripsy (ESWL) for treatment of renal stone <2 cm: a meta-analysis. Urolothiasis. 2016;44:353–65.
Ito H, Sakamaki K, Matsuzaki J, et al. Development and validation of a nomogram for predicting stone-free status after flexible ureteroscopy for renal stones. BJU Int. 2014;115:446–551.
Bryniarski P, Paradysz A, Zyczkowski M, et al. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J Endourol. 2012;26:52.
Moses RA, Ghali FM, Vernon MPJ, Hyams E. Unplanned hospital return for infection following ureteroscopy- can we identify modifiable risk factors? J Urol. 2016;195(4):931–6.
Aboumarzouk O, Monga M, Kata S, Traxer O, Somani M. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol. 2012;26:10.
Al-Qahtani SM, Gil-Deiz-de-Medina S, Traxer O. Predictors of clinical outcomes of flexible ureterorenoscopy with holmium laser for renal stone greater than 2 cm. Adv Urol. 2012, 543537
Cohen J, Cohen S, Grasso M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int. 2013;111:E127–31.
Hyams ES, Munver R, Bird VG, Uberoi J, Shah O. Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: a multi-institutional experience. J Endourol. 2010;24:1583–8.
Preminger G. Management of lower pole calculi: shock wave lithotripsy versus percutaneous nephrolithotomy versus flexible ureteroscopy. Urol Res. 2006;34:108–11.
Sampaio FJ, Aragao AH. Inferior pole collecting system anatomy: its probable role in extracorporeal shock wave lithotripsy. J Urol. 1992;147(2):322–4.
Resorlu B, Oguz U, Resorlu EB, Oztuna D, Unsal A. The impact of pelvicaliceal anatomy on the success of retrograde intrarenal surgery in patients with lower pole renal stones. J Urol. 2012;79(1):61–6.
Singh BP et al. Retrograde intrarenal surgery vs extracorporeal shock wave lithotripsy for intermediate size inferior pole calculi: a prospective assessment of objective and subjective outcomes. Urology. 2014;83:1016–22.
El-Nahas AR, Ibrahim HM, Youssef RF, Sheir KZ. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10–20 mm. BJU Int. 2012;110(6):898–902.
Ghani KR, Wolf Jr JS. What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Rev Urol. 2015;12(7):363.
Borghi L, Meschi T, Amato F, Briganti A, Novarini A, Giannini A. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol. 1996;155(3):839–43.
Curhan GC, Willett WC, Rimm EB, Stampfer MJ. A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. NEJM. 1993;328:833–8.
Taylor EN, Fung TT, Curhan GC. DASH-style diet associates with reduced risk for kidney stones. J Am Soc Nephrol. 2009;20(10):2253–9.
Uribarri J, Oh MS, Carrol HJ. The first kidney stone. Ann Intern Med. 1989;111(12):1006.
Molina WR, Marchini GS, Monga M, et al. Determinants of holmium:yttrium-aluminum-garnet laser time and energy during ureteroscopic laser lithotripsy. Endourol Stones. 2014;83(4):738–44.
Ackerman A, Chen T, Young B, Lipkin M, et al. The effect of variable pulse duration on stone communition, fiber tip degradation, and stone retropulsion in a “Dusting” model. J Urol. 2016;195(4S):e472–3.
Schatloff O, Lindner U, Ramon J, Winkler H. Randomized trial of stone fragment active retrieval versus spontaneous passage during holmium laser lithotripsy for ureteral stones. J Urol. 2010;183:1031–5.
Portis A, Laliberte M, Drake S, Rosenberg M, Bretzke C. Intraoperative fragment detection during percutaneous nephrolithotomy: evaluation of high magnification rotational fluoroscopy combined with aggressive nephroscopy. J Urol. 2006;175:162–5.
Rebuck DA, Macejko A, Bhalani V, Ramos P, Nadler RB. The natural history of renal stone fragments following ureteroscopy. Urology. 2011;77:564–8.
Hussain M, Acher P, Penev B, Cynk M. Redefining the limits of flexible ureterorenoscopy. J Endourol. 2011;25:45–9.
Cocuzza M et al. Outcomes of flexible ureteroscopic lithotripsy with holmium laser for upper urinary tract calculi. Int Braz J Urol. 2008;34:143–9.
Auge BK, Pietrow PK, Lallas CD, Raj GV, Santa-Cruz RW, Preminger GM. Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation. J Endourol. 2004;18(1):33–6.
Zhong W, Leto G, Wang L, Zeng G. Systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy: a study of risk factors. J Endourol. 2015;29(1):25–8.
Ng YH, Somani BK, Dennison A, Kata SG, Nabi G, Brown S. Irrigant flow and intrarenal pressure during flexible ureteroscopy: the effect of different access sheaths, working channel instruments, and hydrostatic pressure. J Endourol. 2010;24(12):1915–20.
Kourambas J, Byrne RR, Preminger GM. Does a ureteral access sheath facilitate ureteroscopy? J Urol. 2001;165(3):789–93.
Pietrow PK, Auge BK, Delvecchio FC, Silverstein AD, Weizer AZ, Albala DM, et al. Techniques to maximize flexible ureteroscope longevity. Urology. 2002;60(5):784–8.
Berquet G, Prunel P, Verhoest G, Mathieu R, Bensalah K. The use of a ureteral access sheath does not improve stone-free rate after ureteroscopy for upper urinary tract stones. World J Urol. 2014;32:229–32.
L’Esperance JO, Ekeruo WO, Scales Jr CD, et al. Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology. 2005;66:252–5.
Lallas CD, Auge BK, Raj GV, et al. Laser Doppler flow- metric determination of ureteral blood flow after ureteral access sheath placement. J Endourol. 2002;16:583–90.
• Traxer O, Thomas A. Prospective evaluation and classifi- cation of ureteral wall injuries resulting from insertion of a ure- teral access sheath during retrograde intrarenal surgery. J Urol. 2013;189:580–4. Large prospective study for renal stones treated by URS LL. With placement of a 12/14 Fr UAS. 46.5% had visible ureter damage on 4 point scale. Of these, 86% of which had mucosal injury and 10% with damage through mucosa to smooth muscle. Absence of pre-operative double-J stent placement was the greatest risk factor for ureteral injury.
Delvecchio FC, Auge BK, Brizuela RM, et al. Assessment of stricture formation with the ureteral access sheath. Urology. 2003;61:518–22.
Traxer O, Wendt-Nordahl G, de la Rosette JJ, et al. Differences in renal stone treatment and outcomes for patients treated either with or without the support of a ureteral access sheath: the clinical research office of the endourological society ureteroscopy global study. World J Urol. 2015;33:2137–44.
Morgan MSC, Antonelli JA, Pearle MS, et al. Use of an electronic medical record to assess patient-report morbidity following ureteroscopy. J Endourol. 2016;30(S1):S45–51.
Schuster TG, Hollenbeck BK, Faerber GJ, Wolf Jr JS. Ureteroscopic treatment of lower pole calculi: comparison of lithotripsy in situ and after displacement. J Urol. 2002;168:43–5.
Chew BH et al. Dusting versus basketing during ureteroscopic lithotripsy—what is more efficacious? Interim analysis from a multi-centre prospective trial from the EDGE Research Consortium [abstract]. J Urol. 2015;193(4S):e261–2.
Gamal W, Mamdouh A. Flexible URS Holmium laser stone dusting vs fragmentaion for <2 cm single renal stone [abstract]. J Urol. 2015;193(4S):e312–3.
Tracey J, Gagin G, Ghani K, et al. Flexible ureteroscopy and laser lithotripsy for renal stones using ‘pop-dusting’: comparison of outcomes between traditional dusting settings versus ultra-high frequency settings [abstract]. J Urol. 2016;195(4S):e683.
•• Chew BH et al. Dusting versus basketing during ureteroscopic lithotripsy—what is more efficacious? final results from the EDGE Research Consortium [abstract]. J Urol. 2016;195(4S):e407. Prospective comparison of dusting to basketing for renal stones 5–20 mm. Initial data shows lower SFR and higher residual fragments in the dusting arm with similar post-operative complications and re-interventions. However, final data analysis is not yet available.
Candau C, Saussine C, Lang H, Roy C, Faure F, Jacqmin D. Natural history of residual renal stone fragments after ESWL. Eur Urol. 2000;37(1):18–22.
Streem SB, Yost A, Mascha E. Clinical implications of clinically insignificant store fragments after extracorporeal shock wave lith- otripsy. J Urol. 1996;155(4):1186–90.
Osman MM, Alfano Y, Kamp S, et al. 5-Year follow-up of patients with clinically insignificant residual fragments after extracorporeal shock wave lithotripsy. Eur Urol. 2005;47(6):860–4.
El-Nahas AR, El-Assmy AM, Madbouly K, et al. Predictors of clinical significance of residual fragments after extracorporeal shock wave lithotripsy for renal stones. J Endourol. 2006;20(11):870–4.
Khaitan A, Gupta NP, Hemal AK, et al. Post-ESWL, clinically insignificant residual stones: reality or myth? Urology. 2002;59(1):20–4.
Zanetti G, Seveso M, Montanari E, et al. Renal stone fragments following shock wave lithotripsy. J Urol. 1997;158(2):352–5.
• Chew BH, Brotherhood HL, Sur RL, Humphreys MR. Natural history, complications and re-intervention rates of asymptomatic residual stone fragments after ureteroscopy: a report from the EDGE Research Consortium. J Urol. 2016;195(4):982–6. 232 patients with residual fragments >4 or <4 mm after URS LL for renal stones were evaluated for “stone events” and complications. Residual fragments >4 mm were more likely to grow (p<0.001), result in complications (p=0.039), and re-interventions (p=0.01). Subset analysis also suggests step-wise increase in morbidity with increasing residual fragment size >2 mm.
Tracey J, Gagin G, Ghani K, et al. Stone dusting: outcomes of ureteroscopic lithotripsy using a multi-cavity high-power Holmium laser [abstract]. J Urol. 2016;195(4S):e510.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Javier E. Santiago, Adam B. Hollander, and Samit D. Soni each declare no potential conflicts of interest.
Richard E. Link reports occasional consulting for Boston Scientific.
Wesley A. Mayer reports reimbursement from Boston Scientific for a trip to the Boston Scientific Plant.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Endourology
Electronic supplementary material
Below is the link to the electronic supplementary material.
Dusting vs. Cracking (MP4 200329 kb)
Rights and permissions
About this article
Cite this article
Santiago, J.E., Hollander, A.B., Soni, S.D. et al. To Dust or Not To Dust: a Systematic Review of Ureteroscopic Laser Lithotripsy Techniques. Curr Urol Rep 18, 32 (2017). https://doi.org/10.1007/s11934-017-0677-8
Published:
DOI: https://doi.org/10.1007/s11934-017-0677-8