Abstract
The diagnosis and treatment of prostate cancer continue to evolve with advances in science and technology. The utilization of multiparametric MRI (mp-MRI) to identify lesions in the prostate has given clinicians the ability to visualize malignancy in the prostate with greater confidence. With this new ability came the advancement of fusion biopsy platforms, which allow for direct targeting of these lesions. As with any new technology in medicine, the proper use of these modalities and how they fit into current clinical practice need to be addressed. This review summarizes the current knowledge on how to best optimize which men undergo mp-MRI and fusion biopsies both in the screening and treatment settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most commonly diagnosed non-cutaneous cancer and second leading cause of cancer death of men in the USA [1]. Despite this, prostate cancer screening has been scrutinized because of the overdiagnosis and overtreatment of clinically insignificant disease. The US Preventative Services Task Force (USPSTF) in 2012 gave prostate-specific antigen (PSA) screening a grade D recommendation—meaning the harms outweighed the benefits of screening [2]. To address these issues, both smarter screening and smarter treatment approaches need to be developed. One of the modalities that has been studied extensively over the last decade to address these shortcomings has been multiparametric MRI (mp-MRI) [3].
Multiparametric MRI is both an anatomical and functional imaging modality of the prostate. Mp-MRI consists of T2-weighted (T2W) images, diffusion-weighted images (DWI), dynamic contrast enhanced imaging (DCE), and at some centers, MR spectroscopy. T2W images provide anatomic detail of the prostate including the zonal anatomy, prostatic capsule, urethra, and seminal vesicles. Prostate malignancies appear hypointense on T2W images. DCE relies on the fact that prostate cancers preferentially uptake contrast. DWI assesses the random Brownian motion of water molecules within the prostate. The more densely the cells are arranged, as seen in cancer, the more restricted the movement of water molecules. A quantitative apparent diffusion coefficient (ADC) value can be calculated from these DWI sequences, with a lower ADC value corresponding to more densely packed cells in the affected area. Studies have evaluated the relationship between ADC values and Gleason score and have found a significant negative correlation between ADC and Gleason scores, which could help risk stratify these patients [4]. Any of these different sequences alone perform poorly in identifying cancer. However, when these sequences are combined, as mp-MRI, the benefits of each sequence complement each other and improve the accuracy in detecting prostate cancer [5].
Historically, MRI of the prostate was used as a staging tool to assess for extraprostatic extension (EPE) and seminal vesicle invasion (SVI) [6]. With the advancement of imaging technology, the focus was turned towards identifying and characterizing prostatic lesions. The last step in validating the mp-MRI as a diagnostic tool was to correlate the images seen with whole mount pathology after radical prostatectomy. Turkbey et al. developed 3D molds of the prostate base on the MRI which allowed the prostate to be aligned with the MRI images. Tumors were then mapped on histopathology and MRI and correlated with each other. They found that the positive predictive value (PPV) of mp-MRI to detect prostate cancer was 98, 98, and 100 % in the overall prostate, peripheral zone, and central gland, respectively. The sensitivity was higher for tumors larger than 5 mm in diameter as well as for those with higher Gleason score >7, p <0.05 [7].
As MRI technology improved to detect prostate cancer, the way biopsies was performed needed to advance as well. New biopsy techniques have been developed to directly biopsy the lesions seen on MRI, similarly to how other solid organ malignancies are diagnosed [8].
Fusion Biopsy Platforms
Three different modalities have been evaluated to use MRI to improve prostate cancer detection during biopsy: cognitive registration, in-bore biopsy, and MRI-transrectal ultrasound (TRUS) fusion biopsy.
Cognitive registration allows the practitioner to review the MRI images and apply this knowledge while performing the TRUS biopsy. The areas in the prostate where the lesions were identified on MRI are targeted on TRUS by cognitively fusing the two images. The first report of prostate MRI being used in conjunction with a cognitive biopsy is from 1999. They found correct correlation with the site of positive biopsy and suspicious areas seen on MRI [9]. This technique is heavily operator dependent and relies on the expertise of the person performing the biopsy. It does not however require any additional training, equipment, or computer software. Studies evaluating the effectiveness of cognitive registration have shown it does increase the cancer detection rate and identifies significant prostate cancer better than random 12 core biopsies [10, 11].
In-bore MR-guided biopsies were the first type of guided biopsies performed on MRI-identified lesions. These biopsies are performed while the patient is in the MRI scanner and can be performed by different approaches—transrectal, perineal, or transgluteal [12]. MRI during the biopsy allows for precise localization of the prostate lesions. This resource-intensive technique however often requires anesthesia, can be time consuming, requires additional training, and relies on the operator’s expertise [13, 14]. A systematic review of in-bore biopsy reported a median cancer detection rate of 42 % and the majority detected were clinically significant (81–93 %) [15].
Software Registration Platforms
Software registration platforms were developed as an alternative to in-bore MRI-guided biopsy, which could be performed in the office setting. In addition, it utilizes TRUS, which is the most utilized method to perform prostate biopsies. These platforms take a 2D ultrasound image and reconstruct the prostate into a 3D model. The contours of the US and MRI images are fused and allow the physician to see the MRI lesion location on real time US imaging.
Once the prostate images are fused, different tracking devices give the practitioner real time guidance as to where the biopsy is being taken. Three different types of tracking approaches have been approved—external magnetic field generators, real time 3D TRUS, and angle sensing robotic arms. For the external magnetic field generator approach, a tracker located in the tip of the US probe communicates with a magnetic field, which gives real time information of the probe location in relation to the prostate. Biopsies of the MRI-identified targets are biopsied in the axial and sagittal plane to accommodate for potential spatial inaccuracy of the system [16]. The 3D TRUS approach utilizes a 3D US probe which creates a 3D reference model. After the biopsies are taken, the needle is left in place and a new image is taken to register the location of the biopsy. This can lead to targeting error as the needle location is confirmed after the biopsy has been taken. In the third tracking platform, angle sensing robot arms track the precise location of the probe and needle in relation to the prostate.
MRI fusion biopsy platforms have been shown to outperform standard sextant biopsies [17, 18]. A recent meta-analysis evaluated the cancer detection rate on a per core basis and a per patient basis [19]. They found on a per core basis cancer was detected in 30 % of targeted cores (375 of 1252) versus 7 % of standard cores (368 of 5441). On a per patient basis, cancer was detected in 36 % for standard biopsy and in 48 % for targeted biopsy. The overall cancer detection rate however is not as important as identifying the significant cancers while minimizing the insignificant cancer found.
Siddiqui et al. evaluated the utility of performing targeted biopsies in regard to upgrading the cancer and finding significant disease versus standard sextant biopsy. Targeted biopsy led to upgrading in 32 % and detected 67 % more Gleason ≥4 + 3 tumors than standard biopsy alone. Standard sextant biopsy led to upgrading in 26 % over targeted biopsy alone but only detected 8 % more Gleason ≥4 + 3 tumors [20].
The remainder of this review will focus on how MRI-TRUS fusion biopsy can be utilized in different clinical populations.
No Prior Biopsy-Screening Population
Prostate-specific antigen (PSA) testing has been the mainstay of prostate cancer screening since its development in the late 1980s. Depending on what threshold PSA level is used, the sensitivity and specificity of the test to detect prostate cancer change. Other clinical parameters such as digital rectal exam, age, family history of prostate cancer, race, PSA doubling time, and PSA velocity have been incorporated into prostate cancer risk nomograms which help the practitioner decide on whether to recommend biopsy.
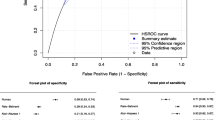
One of these is the Prostate Cancer Prevention Trial (PCPT) risk calculator [21]. A recent study compared the PCPT calculator to mp-MRI in detecting clinically significant prostate cancer in men with either elevated PSA or abnormal digital rectal examination (DRE) and suspicious lesions seen on MRI, defining significant cancer as Gleason ≥7. They observed an area under curve (AUC) of 0.769 (95 % CI, 0.703–0.834) for lesion suspicion level on mp-MRI in predicting high-grade prostate cancer, which was 10 percentage points better than the PCPT AUC of 0.676 (95 % CI, 0.592–0.751; p = 0.091 [22]).
Mp-MRI has also been used as a screening test to detect clinically significant prostate cancer with transperineal template mapping as the reference standard. Clinically significant cancer was defined at Gleason ≥3 + 4 = 7 and/or maximum cancer core length ≥4 mm, and their outcome analysis focused on lesions with suspicion scores ≥3 out of a 5 point. They reported a sensitivity of 94 %, specificity of 23 %, positive predictive value (PPV) of 34 %, negative predictive value (NPV) of 89 %, and AUC of 0.72 [23]. A negative MRI is this study performed well with a NPV of 89 %, but as a screening test, there still was a considerable amount of men with false-positives highlighted by the decreased specificity.
One criticism of using mp-MRI as a screening test is the increased time and cost incurred by the patient and health care system at large. This was addressed in a study by Rais-Bahrami et al. in which they evaluated biparametric MRI, consisting of T2-weighted and diffusion-weighted images, in men with elevated PSA levels and no prior biopsy. These scans could be performed in approximately 15 min, and the elimination of DCE obviates the need for intravenous contrast reducing the overall cost and invasiveness of testing. They found that the AUC for prostate cancer detection was 0.66 for PSA alone and 0.80 for biparametric MRI. The diagnostic performance was increased when PSA density (PSAD) and biparametric MRI were taken together with an AUC of 0.87. Overall, they found a positive MRI with more than one screen positive lesion (positive on both parameters examined) had a sensitivity of 89 % and specificity of 54 % [24]. Again seen in this study, MRI increases the diagnostic yield of finding prostate cancer, and specifically higher grade disease, a significant improvement over PSA alone.
During the period of PSA screening, reference ranges have been developed based on a man’s age, race, and body weight index. A recent study sought to identify a PSA threshold, which optimized the detection of clinically significant cancer by MRI-TRUS fusion biopsy. In men with no prior biopsy, using a PSA cutoff of 6.5 ng/ml identified 90 % of the patients who were upgraded to significant disease by targeted biopsy versus standard sextant biopsy, corresponding to 64 % of the men who had a mp-MRI [25]. Thus, using a PSA threshold could identify patients most likely to benefit from mp-MRI, and as noted, 36 % of the men could have avoided a mp-MRI and targeted biopsy.
Prior Negative Biopsy
A common clinical dilemma faced by urologists is a patient with elevated or rising PSA and a prior negative prostate biopsy. The repeated use of TRUS sextant biopsies is limited by the fact that cancer detection rates decrease with each subsequent biopsy [26]. Saturation biopsies of the prostate have been evaluated in the repeat biopsy setting, with cancer detection rates around 30 %, similar to repeat sextant biopsies, but with potentially increased morbidity of the procedure [27]. Multiparametric MRI in this setting allows for the visualization of lesions in areas of the prostate under sampled by standard biopsy techniques: the subcapsular, apical, anterior, and the transition zones of the prostate [28].
One study evaluated 105 men with prior negative biopsy and elevated PSA who underwent targeted fusion biopsies as well as standard systematic biopsies. They found that 91 % of the men with cancer found by targeted biopsy were significant versus only 54 % of the cancer found on systematic biopsies. The MRI lesion degree of suspicion was the most powerful predictor of finding significant cancer on biopsy. Interestingly, they also found no relationship between the number of prior negative biopsies and cancer detection rate [29]. Similar results were seen in another study of men with prior negative biopsy and elevated PSA. Kaufmann et al. found that cancer detection rate was 20 % higher with fusion biopsy and all cancers identified by targeted biopsy met the criteria for significant cancer [30]. The ability of mp-MRI to identify significant cancer in men with prior negative biopsies was studied. In this study, they used transperineal template biopsies as the standard and defined clinically significant cancer as any Gleason grade 4 or maximum cancer core length ≥4 mm. They found mp-MRI accuracy at detection of clinically significant cancer showed sensitivity of 76 %, specificity of 42 %, positive predictive value of 38 %, and negative predictive value of 79 %. Their conclusion was that this may allow some men to avoid unnecessary repeat biopsies [31].
As the previously stated studies point out, MRI fusion-guided biopsies are able to identify significant cancers after prior negative biopsy because the mp-MRI is able to identify lesions suspicious for cancer taking away the “randomness” of the biopsy. The standard sextant biopsy can miss significant cancers by chance or by undersampling of the apex, midline, and anterior regions of the prostate (see Fig. 1). Park et al. reported that in men with a prior negative biopsy, 76 % of the cancers identified by MRI targeted biopsies were located in the transition zone [32]. Another study found that in men who had at least two prior negative prostate biopsies, 68 % of the cancer identified were in the ventral transition zone or anterior horns of the peripheral zone [33]. Likely explaining why their previous biopsies were all negative. Similarly, targeted biopsies of the distal apical prostate have been found to detect significantly more cancer than random sextant biopsies [34]. Larger prostates are more prone to undersampling as a smaller percentage of the overall volume of the prostate is sampled. Walton-Diaz et al. showed that although the cancer detection rate of fusion biopsy does decrease with increasing prostate size, the cancer detection rate of fusion biopsy in these larger prostates was considerably higher compared to standard sextant biopsy rates [35].
Mp-MRI of a 62-year-old male with PSA of 4.99 ng/ml and low apical lesion. The T2-weighted image (a) shows a hypointense lesion in the distal left apical transition zone with restricted diffusion seen on diffusion-weighted images (DWI) (b). Targeted fusion biopsy of this lesion revealed Gleason 3 + 4 = 7 adenocarcinoma of the prostate; all standard sextant biopsies were negative for malignancy. A 60-year-old male with PSA of 44.8 ng/ml had a sextant biopsy with found Gleason 3 + 3 + 6 adenocarcinoma in 2 % of 1 core. Mp-MRI showed on T2-weighted images (c) an over 4 cm anterior transition zone lesion which extends across the midline. The lesion had restricted diffusion seen on DWI images (d) as well as hyper-enhancement seen on dynamic contrast enhancement (DCE) images (e). Targeted biopsy of this lesion revealed Gleason 4 + 4 = 8 adenocarcinoma
Prior to implementation of MRI as diagnostic adjunct, clinical parameters such as age, race, family history, and PSA level were used to help determine if a repeat biopsy should be performed. More recently, newer tests such as prostate cancer antigen (PCA3) and prostate health index (PHI), a mathematical formula that combines total PSA, free PSA, and [−2] proPSA, have been utilized to determine a man’s risk of prostate cancer on repeat biopsy. A study by Porpiglia et al. evaluated the efficacy of PCA3, PHI, and mp-MRI in the repeat biopsy setting. On receiver operating characteristic (ROC) analysis, they found the most significant contribution of these tests to detect prostate cancer was provided by mp-MRI (AUC 0.936). This was greater than the contribution of the PHI combined with PCA3 (p < 0.001) [36].
Surgical Planning
Many patients today who have chosen to have a radical prostatectomy will already have had a mp-MRI performed, and in those that have not, many clinicians are obtaining them before surgery. There are many findings, which can be evaluated on mp-MRI which help guide surgical planning. Normally, there is a layer of perirectal fat posterior to the prostate. This normal anatomic space can become obliterated with cancer growing towards and into the rectum. A finding such as this could drastically alter how the patient is counseled regarding his treatment options and risk of potential complications.
Mp-MRI can also be used to assess for extraprostatic extension (EPE) [37]. Somford et al. evaluated 183 men who underwent a radical prostatectomy and compared final pathology to preoperative extracapsular extension (ECE) on mp-MRI. The overall sensitivity of mp-MRI to detect ECE on final pathology was 73.8 %. On multivariate analysis, only PSA and stage on mp-MRI were associated with ECE on final pathology with mp-MRI being the strongest predictor (OR 1.1 versus 10.3) [38].
Historically, Partin tables were used to evaluate a patient’s risk of extraprostatic spread based on clinical and pathological findings. One study compared the Partin tables to mp-MRI in their ability to detect organ-confined disease. They concluded the accuracy of mp-MRI in predicting organ-confined disease on pathological analysis is significantly greater than that of the Partin tables. Mp-MRI had a high PPV (91.2 %) when predicting organ-confined disease and a high NPV (89.7 %) with regard to ECE [39].
It has been our institutional experience to use the preoperative MRI findings to help us guide our extent and laterality of our nerve sparing technique. This approach has been reported by Park and colleagues in 353 men who underwent radical prostatectomy and had mp-MRI data included. The urologists determine preoperatively the degree of nerve sparing (bilateral, unilateral, no nerve sparing) they would use without incorporating the mp-MRI findings. After reviewing the MRI reports, 26 % of the patients had a change in surgical plan. Of these patients, 57 % changed to a more preservable nerve sparing approach and the other 43 % changed to a wider margin of resection [40].
Seminal Vesicle Invasion
In patients with high-risk disease, seminal vesicles can also be evaluated with mp-MRI. In a recent study, 131 patients had a mp-MRI followed by radical prostatectomy. Comparing the final pathology to mp-MRI findings, they reported a specificity of 96–98 % and a positive predictive value of 70–79 % in identifying seminal vesicle invasion (SVI) [41]. In men with clinically high-risk prostate cancer, mp-MRI in combination with clinical variables is able to more accurately predict SVI and ECE than clinical variables alone [42]. The preoperative identification of SVI can have important implications in treatment recommendations and presurgical planning. The fusion biopsy platform can be extended to target suspicious lesions seen in the seminal vesicles on MRI. A study using fusion biopsy to target seminal vesicle lesions reported a cancer detection rate of 71 % for moderate and highly suspicious lesions [43].
Local Recurrence
Another clinical scenario where mp-MRI is gaining utilization is in men with rising PSA after radical prostatectomy. The differentiation between local and systemic recurrence is an important distinction to make before salvage or adjuvant treatments are administered. The functional component as well as the detailed anatomic information obtained from mp-MRI can be used to help differentiate between local recurrence, residual normal prostate tissue, scar/fibrosis, and granulation tissue [44]. Current evidence suggests that for salvage radiation therapy, lower preradiation PSA levels correspond to more durable responses [45]. A recent study of men with biochemical recurrence after radical prostatectomy and PSA ≤0.4 ng/ml reported the sensitivity of mp-MRI to identify local recurrence was 86 % [46]. At our institution, we use MRI fusion biopsy to target lesions identified on mp-MRI. This has allowed us to more accurately diagnose local recurrences and as a result has allowed us to better identify patients who will benefit from salvage treatments.
Active Surveillance
Active surveillance (AS) is a treatment option for men with low-risk prostate cancer, which addresses the overtreatment of indolent cancers [47]. Many different AS protocols exist, which are based on multiple clinical parameters as well as the pathology results from standard sextant biopsy sessions. These previously used protocols become less applicable when using MRI fusion biopsies because they are based on standard sextant biopsy findings, which correlated to low risk findings at the time of radical prostatectomy. MRI fusion biopsy detects higher grade and more significant cancer; and therefore, based on historical protocols, fewer men undergoing this image-guided biopsy would be eligible for AS. One could argue however that men who undergo MRI fusion biopsy are more accurately staged and thus more accurately identified to have indolent disease with a low risk of progression. In addition, there is recent evidence to support that fusion biopsy provides a more representative assessment of the overall disease burden [48]. To date, there are no AS protocols which strictly incorporate prostate cancer findings using MRI fusion biopsy techniques. Hu et al. evaluated men who met Epstein AS criteria based on standard sextant biopsies and used MRI fusion biopsy findings to confirm their eligibility. They reclassified 36 % of the men overall who no longer met AS criteria and 100 % of the men with highly suspicious lesions seen on MRI no longer met Epstein AS criteria after confirmatory fusion biopsy [49]. Similarly, Da Rosa et al. found that MRI suspicion level significantly predicted identifying clinically significant cancer on multivariate analysis in men on AS [50]. Another study took these findings one step further and identified the MRI suspicion score, number of suspicious lesions identified, and lesion density (total lesion volume/prostate volume) as significant for reclassifying men on AS using Epstein criteria. Based on these findings, they developed a nomogram to predict which men would be reclassified no longer meeting Epstein AS criteria based on these three MRI factors [51]. The NCI group recently published only series to date in AS patients who have undergone serial imaging and fusion biopsy. They reported the negative predictive value of a stable MRI to be 80%, with the number needed to biopsy being 8.7 and 2.9 for fusion biopsy and standard biopsy, respectively [52]. Finally, serial MRI and targeted biopsy allow for retargeting of prior areas of concern, which can be assigned as new targets based on the prior findings [53]. Though the role of MRI and targeted biopsy in AS is evolving, currently, the ability to identify ideal candidates is promising, and work on its ability to detect progression in continued monitoring is being studied.
Conclusion
The use of mp-MRI and fusion biopsy has changed how clinicians now diagnose and treat prostate cancer. The use of these modalities allows for more accurate identification of tumor burden within the prostate as well as possible extraprostatic disease. This information is crucial when counseling a patient on his treatment options, especially when recommending active surveillance versus active treatment. Also, now that these lesions can be seen within the prostate, it makes focal ablative therapy a treatment option just as it is in many other solid organ malignancies.
References
What are the key statistics about prostate cancer? American Cancer Society, 2014.
Moyer VA. Screening for prostate cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 2012;157(2):120–34.
George AK, Pinto PA, Rais-Bahrami S. Multiparametric MRI in the PSA screening era. Biomed Res Int. 2014;2014:465816.
Turkbey B et al. Is apparent diffusion coefficient associated with clinical risk scores for prostate cancers that are visible on 3-T MR images? Radiology. 2011;258(2):488–95.
Hegde JV et al. Multiparametric MRI of prostate cancer: an update on state-of-the-art techniques and their performance in detecting and localizing prostate cancer. J Magn Reson Imaging. 2013;37(5):1035–54.
Poon PY et al. Magnetic resonance imaging of the prostate. Radiology. 1985;154(1):143–9.
Turkbey B et al. Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol. 2011;186(5):1818–24.
Rothwax JT et al. Multiparametric MRI in biopsy guidance for prostate cancer: fusion-guided. Biomed Res Int. 2014;2014:439171.
Perrotti M et al. Prospective evaluation of endorectal magnetic resonance imaging to detect tumor foci in men with prior negative prostatic biopsy: a pilot study. J Urol. 1999;162(4):1314–7.
Park BK et al. Prospective evaluation of 3-T MRI performed before initial transrectal ultrasound-guided prostate biopsy in patients with high prostate-specific antigen and no previous biopsy. AJR Am J Roentgenol. 2011;197(5):W876–81.
Haffner J et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int. 2011;108(8 Pt 2):E171–8.
Susil RC et al. System for prostate brachytherapy and biopsy in a standard 1.5T MRI scanner. Magn Reson Med. 2004;52(3):683–7.
Bodelle B et al. 1.5-T magnetic resonance-guided transgluteal biopsies of the prostate in patients with clinically suspected prostate cancer: technique and feasibility. Investig Radiol. 2013;48(6):458–63.
Engelhard K et al. Prostate biopsy in the supine position in a standard 1.5-T scanner under real time MR-imaging control using a MR-compatible endorectal biopsy device. Eur Radiol. 2006;16(6):1237–43.
Overduin CG, Futterer JJ, Barentsz JO. MRI-guided biopsy for prostate cancer detection: a systematic review of current clinical results. Curr Urol Rep. 2013;14(3):209–13.
Hong, C.W., et al. Comparison of MR-US fusion-guided prostate biopsies obtained from axial and sagittal approaches. BJU Int, 2014. doi:10.1111/bju.12871
Rastinehad AR et al. Improving detection of clinically significant prostate cancer: magnetic resonance imaging/transrectal ultrasound fusion guided prostate biopsy. J Urol. 2014;191(6):1749–54.
Siddiqui MM, Rais-Bahrami S, Turkbey B et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the detection of prostate cancer. JAMA. 2015;313(4):390–7.
Valerio M, Donaldson I, Emberton M et al. Detection of Clinically Significant Prostate Cancer Using Magnetic Resonance Imaging-Ultrasound Fusion Targeted Biopsy: A Systematic Review. Eur Urol 2014; pii: S0302-2838(14)01040–9. doi:10.1016/j.eururo.2014.10.026.
Siddiqui MM et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol. 2013;64(5):713–9.
Thompson IM et al. Assessing prostate cancer risk: results from the prostate cancer prevention trial. J Natl Cancer Inst. 2006;98(8):529–34.
Salami SS et al. Multiparametric magnetic resonance imaging outperforms the prostate cancer prevention trial risk calculator in predicting clinically significant prostate cancer. Cancer. 2014;120(18):2876–82.
Abd-Alazeez M et al. Performance of multiparametric MRI in men at risk of prostate cancer before the first biopsy: a paired validating cohort study using template prostate mapping biopsies as the reference standard. Prostate Cancer Prostatic Dis. 2014;17(1):40–6.
Rais-Bahrami, S., et al. Diagnostic value of biparametric magnetic resonance imaging (MRI) as an adjunct to prostate-specific antigen (PSA)-based detection of prostate cancer in men without prior biopsies. BJU Int, 2014. doi:10.1111/bju.12639
Shakir, N.A., et al. Identification of threshold prostate specific antigen levels to optimize the detection of clinically significant prostate cancer by magnetic resonance imaging/ultrasound fusion guided biopsy. J Urol, 2014. doi:10.1016/j.juro.2014.08.002
Roehl KA, Antenor JA, Catalona WJ. Serial biopsy results in prostate cancer screening study. J Urol. 2002;167(6):2435–9.
Shinohara K, Nguyen H, Masic S. Management of an increasing prostate-specific antigen level after negative prostate biopsy. Urol Clin N Am. 2014;41(2):327–38.
Sankineni S, George AK, Brown AM et al. Posterior subcapsular prostate cancer: identification with mpMRI and MRI/TRUS fusion-guided biopsy. Abdom Imaging 2015; doi:10.1007/s00261-015-0426-8
Sonn GA et al. Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. Eur Urol. 2014;65(4):809–15.
Kaufmann, S., et al. Direct comparison of targeted mri-guided biopsy with systematic transrectal ultrasound-guided biopsy in patients with previous negative prostate biopsies. Urol Int, 2014. doi:10.1159/000365397
Abd-Alazeez M et al. The accuracy of multiparametric MRI in men with negative biopsy and elevated PSA level—can it rule out clinically significant prostate cancer? Urol Oncol. 2014;32(1):45. e17–22.
Park BK et al. Lesion localization in patients with a previous negative transrectal ultrasound biopsy and persistently elevated prostate specific antigen level using diffusion-weighted imaging at three Tesla before rebiopsy. Investig Radiol. 2008;43(11):789–93.
Hambrock T et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010;183(2):520–7.
Nix JW et al. Very distal apical prostate tumours: identification on multiparametric MRI at 3 Tesla. BJU Int. 2012;110(11 Pt B):E694–700.
Walton Diaz A et al. Can magnetic resonance-ultrasound fusion biopsy improve cancer detection in enlarged prostates? J Urol. 2013;190(6):2020–5.
Porpiglia, F., et al. The roles of multiparametric magnetic resonance imaging, PCA3 and prostate health index—which is the best predictor of prostate cancer after a negative biopsy? J Urol, 2014. doi:10.1016/j.juro.2014.01.030
Raskolnikov D, George AK, Rais-Bahrami S et al. The Role of Magnetic Resonance Image Guided Prostate Biopsy in Stratifying Men for Risk of Extracapsular Extension at Radical Prostatectomy. J Urol 2015; pii: S0022-5347(15)00161–5. doi:10.1016/j.juro.2015.01.072.
Somford DM et al. The predictive value of endorectal 3 Tesla multiparametric magnetic resonance imaging for extraprostatic extension in patients with low, intermediate and high risk prostate cancer. J Urol. 2013;190(5):1728–34.
Gupta, R.T., et al. Comparing 3-T multiparametric MRI and the Partin tables to predict organ-confined prostate cancer after radical prostatectomy. Urol Oncol, 2014. doi:10.1016/j.urolonc.2014.04.017
Park, B.H., et al. Influence of magnetic resonance imaging in the decision to preserve or resect neurovascular bundles at robotic assisted laparoscopic radical prostatectomy. J Urol, 2014. doi:10.1016/j.juro.2014.01.005
Soylu FN et al. Seminal vesicle invasion in prostate cancer: evaluation by using multiparametric endorectal MR imaging. Radiology. 2013;267(3):797–806.
Jeong IG et al. Incremental value of magnetic resonance imaging for clinically high risk prostate cancer in 922 radical prostatectomies. J Urol. 2013;190(6):2054–60.
Raskolnikov D et al. Multiparametric magnetic resonance imaging and image-guided biopsy to detect seminal vesicle invasion by prostate cancer. J Endourol. 2014;28(11):1283–9.
Vargas HA et al. MR imaging of treated prostate cancer. Radiology. 2012;262(1):26–42.
Siegmann A et al. Salvage radiotherapy after prostatectomy—what is the best time to treat? Radiother Oncol. 2012;103(2):239–43.
Linder BJ et al. Early localization of recurrent prostate cancer after prostatectomy by endorectal coil magnetic resonance imaging. Can J Urol. 2014;21(3):7283–9.
Eggener SE, Badani K, Barocas DA et al. Gleason 6 Prostate Cancer: Translating Biology into Prostate Health. J Urol. 2015; pii: S0022-5347(15)03689–7. doi:10.1016/j.juro.2015.01.126.
Okoro C, George AK, Siddiqui MM et al. MR/TRUS Fusion Prostate Biopsy Significantly Outperforms Systematic 12-core Biopsy for Prediction of Total MRI Tumor Volume in Active Surveillance Patients. J Endourol. 2105; doi:10.1089/end.2015.0027.
Hu JC et al. Targeted prostate biopsy in select men for active surveillance: do the Epstein criteria still apply? J Urol. 2014;192(2):385–90.
Da Rosa, M.R., et al. A prospective comparison of MRI-US fused targeted biopsy versus systematic ultrasound-guided biopsy for detecting clinically significant prostate cancer in patients on active surveillance. J Magn Reson Imaging, 2014. doi:10.1002/jmri.24710
Stamatakis L et al. Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer. 2013;119(18):3359–66.
Walton-Diaz A, Shakir NA, George AK et al. Use of serial multiparametric magnetic resonance imaging in the management of patients with prostate cancer on active surveillance. Urol Oncol 2015;33(5): 202.e1–7. )
Raskolnikov, D., et al. The role of image guided biopsy targeting in patients with atypical small acinar proliferation. J Urol, 2014. doi:10.1016/j.juro.2014.08.083
Acknowledgments
Conflict of Interest
Thomas P. Frye and Arvin K. George each declare no potential conflicts of interest.
Peter A. Pinto reports a patent (US8447384B2).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on New Imaging Techniques
Rights and permissions
About this article
Cite this article
Frye, T.P., Pinto, P.A. & George, A.K. Optimizing Patient Population for MP-MRI and Fusion Biopsy for Prostate Cancer Detection. Curr Urol Rep 16, 50 (2015). https://doi.org/10.1007/s11934-015-0521-y
Published:
DOI: https://doi.org/10.1007/s11934-015-0521-y