Abstract
Renal cell carcinoma (RCC) extension into the renal vein or the inferior vena cava occurs in 4 %–10 % of all kidney cancer cases. This entity shows a wide range of different clinical and surgical scenarios, making natural history and oncological outcomes variable and poorly characterized. Infrequency and variability make it necessary to share the experience from different institutions to properly analyze surgical outcomes in this setting. The International Renal Cell Carcinoma–Venous Tumor Thrombus Consortium was created to answer the questions generated by competing results from different retrospective studies in RCC with venous extension on current controversial topics. The aim of this article is to summarize the experience gained from the analysis of the world's largest cohort of patients in this unique setting to date.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) represents the most lethal urologic malignancy, accounting for 3 % of all cancer deaths. Despite a stage migration toward more localized disease with the routine use of imaging tests in diagnosis, approximately 30 % of RCC patients still present today with locally advanced or metastatic stages of the disease [1, 2]. RCC extension into the renal vein or the inferior vena cava (IVC), a unique form of locally advanced disease called “tumor thrombus,” occurs in 4 %–10 % of cases [3]. Radical nephrectomy and tumor thrombectomy remains the mainstay of treatment in this particular setting [2]. However, low-frequency presentation rates, coupled with a wide range of different clinical and, thus, surgical scenarios, make natural history and oncological outcomes of this disease very variable and poorly characterized [4].
Under these circumstances, multi-institutional collaborative models may be used for better characterization of the impact of prognostic factors, perioperative complications, and specific disease-profile therapeutic approaches on oncological outcomes [5–7]. In 2006, an international consortium of 11 institutions, established to retrospectively review a combined cohort of 1,215 patients undergoing radical nephrectomy and tumor thrombectomy for RCC throughout the period 1971–2012, was tailored with this purpose (2006–2012), thus giving birth to the International Renal Cell Carcinoma–Venous Thrombus Consortium (IRCC-VTC). Later on in 2012, the IRCC-VTC was expanded to 22 institutions including a total of 2,147 patients from Europe and the U.S. (Table 1). The aim of this article is to summarize the experience gained from the analysis of the world's largest cohort of patients to date in this unique setting. From the beginning, we focused our research on four areas: RCC prognostic factors, surgical issues, perioperative complications, and predictive nomograms.
RCC Prognostic Factors
Tumor Thrombus Level
Pathologic stage has been shown to be the most important prognostic factor in RCC [8, 9]. However, the impact of tumor thrombus anatomic level on survival rates remains one of the most controversial issues in patients with venous extension, being extensively discussed in the literature [6, 7, 10•, 11–13, 14••, 15–17].
At present, the tumor node metastasis (TNM) staging system remains the most reliable classification system in determining the probability of overall survival (OS) and cancer-specific survival (CSS) rates in these cases. However, this system has lacked a suitable prognostic approach regarding the anatomic level of tumor thrombus inside the venous lumen, and several reports have highlighted the need for a reclassification as significant differences on long-term survival rates had been described for patients with exclusive renal vein involvement or supradiaphragmatic extension [9, 10•, 13, 15]. Therefore, venous involvement limited to the renal vein and supradiaphragmatic extension were finally restaged in separated categories (i.e., T3a and T3c, respectively) when, in 2009, the RCC staging system provided by the American Joint Committee on Cancer (AJCC) and the Union International Contre le Cancer (UICC) was updated (Table 2) [9, 14••, 18].
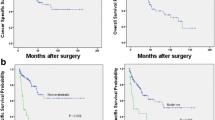
On the basis of the above-mentioned statements, Martínez-Salamanca et al. [14••] attempted to evaluate the accuracy with respect to survival prediction of the updated version of the TNM classification system in patients with RCC with IVC involvement by investigating the impact of renal vein and different categories of IVC involvement (i.e., pT3b and pT3c) on survival rates. Tumor thrombus level was reported to be an independent predictor of survival in this study (43.2 vs. 37.3 vs. 22.2 months for pT3a, pT3b, and T3c, respectively), thus supporting the use of the revised TNM staging system (Fig. 1a).
Metastasis
Presence of metastasis has been reported to be a strong predictor of survival (10.7 % vs. 51.7 % for N0M0 vs. N+/M+, respectively) [10•] in RCC with venous extension, regardless of tumor thrombus anatomic level [6, 19, 20]. The analysis provided by Tosco et al. [21] revealed multiple and nonpulmonary metastases as independent pretreatment prognostic factors, while single-site pulmonary metastasis was shown to be of better prognostic significance when compared with distant metastasis in other sites [22].
A recent analysis from IRCC-VTC on the impact of metastatic spreading on survival [23] confirmed the presence of metastasis at presentation as a significant predictor of survival (52 % vs. 21 % for M0 and M1, respectively) in these patients. Conversely, no significant difference regarding metastasis location was found. Lymph node spreading or synchronous metastases were not correlated with venous involvement in this study. According to these results, it would be better to base the indication for surgery on the presence of metastases at initial presentation, rather than on their location.
Histological RCC Subtype
Several studies have evaluated the prognostic impact of histological subtype in patients with RCC [24–26]. However, the prognostic significance of this pathologic feature in patients with additional renal vein or IVC involvement has rarely been studied and remains unclear [15, 27–30].
The lack of data on this particular issue favored a recent initiative by Tilki et al. [31••] to evaluate the impact of histologic subtype on survival rates in these particular cases. This study showed that patients with papillary histology had significantly worse outcomes and higher tumor thrombus levels, when compared with patients with other histological subtypes. Five-year CSSrates estimated in this study were 59.5 %, 54.8 %, and 36.8 % for chromophobe, clear-cell, and papillary subtypes, respectively, thus supporting the presence of papillary histology as an independent predictor of cancer-specific death (HR 1.62, CI 1.01–2.61, p < .05) with independence of nodal status and presence of distant metastasis (Fig. 1b).
Operative Issues
Presurgical Renal Artery Embolization
Since its first description with palliative intent in 1973 [32], presurgical renal artery embolization (RAE) has broadened its indications in the last 2 decades, mainly due to steady improvements in imaging, percutaneous approaches, embolic agents, surgical techniques, and perioperative care.
Benefits to be gained by this procedure include decreased operative blood loss, ease of dissection secondary to the development of perirrenal tissue edema, decrease in tumor thrombus size favoring less aggressive surgical approaches and morbidity, and overall operative time reduction [6]. However, the frequency (up to 89 %) [33] and the severity of postembolization symptoms have, in many cases, limited the use of this surgical adjunct in many institutions.
On other hand, the effect of RAE on survival rates had been under debate, since different retrospective studies had shown competing outcomes [33, 34]. Therefore, Latal et al. aimed to analyze the impact on perioperative mortality, OS, and CSS in a cohort of 228 patients with RCC and venous extension in whom RAE had been used preoperatively [35]. This study reported no additional benefit in OS or CSS for patients receiving RAE, and no significant difference in perioperative mortality was noted. However, an important issue regarding the time interval from RAE to surgery could not be conveniently raised due to the variability of the temporary margins observed among the patients included in the cohort (0–6 weeks).
The IRCC-VTC has studied the impact of RAE on perioperative mortality and OS/CSS [36]. We analyzed a total of 1,042 patients, 228 (77 %) with and 728 (23 %) without RAE. Perioperative mortality was similar between the two groups (4 %). RAEs were performed on the basis of level of thrombus: level I (15 %), level II (29 %), level III (28 %), and level IV (60 %). Five-year OS and CSS were 39 % (33–47) and 49 % (42–56), respectively, for RAE patients and 36 % (32–40) and 48 % (43–51) for non-RAE patients (OS p = .21 and CSS p = .43).
In conclusion, on the basis of the IRCC-VTC experience, patients with/without preoperative RAE showed similar OS, CSS, and periooperative mortality rates [36].
Presurgical RAE used as an adjuvant procedure for patients requiring nephrectomy and tumor thrombectomy may have operative advantages. However, preoperative RAE acute toxicity may delay surgical intervention in patients with poor performance status. In addition, time interval between the RAE and nephrectomy may impact survival rates. Therefore, it is difficult to draw reliable conclusions about the role of preoperative RAE in the management of patients with RCC and venous involvement.
Cardiopulmonary Bypass
Supradiaphragmatic and intraatrial tumor thrombi pose a challenge for the treating surgeon given the operative difficulty and the possibility for potential intraoperative complications, including massive blood loss and pulmonary embolism [11, 36–38].
Cardiopulmonary bypass (CBP) is used as a surgical adjunct in RCC invading the IVC to provide continuous cardiac venous return, thus preserving cardiovascular output when the IVC is cross-clamped for thrombus withdrawal. The use of CPB meant a technical revolution in radical nephrectomy and tumor thrombectomy, since up to its emergence in the mid-1960s, the rate of intra- and postoperative complications in the excision of suprahepatic and supradiaphragmatic tumor thrombi was extremely high. Conversely, the utilization of this surgical system has recently been associated with morbidity rates that cannot be overstated, including haematological, hepatic, renal, neurological, and septic, among others [36, 39, 40]. This set of potential surgical sequelae has favored the development of procedures with the intention of avoiding the use of sternotomy and CPB (i.e., liver transplantation techniques) [41] or to permit a decrease in the number and severity of CPB-related complications (i.e., minimally invasive thoracotomy, “beating-heart” techniques, antegrade cerebral perfusion, and mild hypothermia) in this particular setting [42•].
Despite the theoretical benefits associated with the reduction in CPB-related morbidity, the impact of this surgical adjunct on RCC with venous involvement survival rates had remained unclear since the first reports on this subject. Thus, the IRCC-VTC aimed to evaluate the effect of CPB on cancer-specific mortality, in a large cohort of 271 patients with tumor thrombus levels III and IV. Mean follow-up in this study was 39.8 (0–258) months, with a median survival of 30 months. The 5-year cancer-specific mortality rates observed were 31 % (level III with CPB), 31 % (level III without CPB), and 28 % (level IV with CPB). Level IV without CPB group did not reach the minimum time period to calculate. These findings support the conclusion that from the oncological outcomes perspective, both approaches (i.e., with or without the use of CPB) are safe for the treatment of RCC with level III and IV tumor thrombus [44].
Perioperative Complications
Radical nephrectomy and tumor thrombectomy have been shown to be associated with major perioperative morbidity (up to 70 %) and mortality (3 %–16 %) in several retrospective series [16, 36, 43, 44]. A number of factors influencing perioperative mortality have been also identified, including patient comorbid conditions, performance status [45], distant metastatic spreading, and tumor thrombus extension above the diaphragm [20]. Although perioperative morbidity (i.e., complication rate) according to the anatomic level of tumor thrombus has been studied [6], no correlation between preoperative mortality and cephalad extent of the thrombus has been reported up to the present.
The IRCC-VTC evaluated the association between tumor thrombus level according to the Mayo Clinic classification system [43] and perioperative complications observed after the procedure. Thereafter, both variables were correlated with perioperative mortality [46]. Postoperative complications were recorded for a 30-days period and graded according to the Clavien–Dindo postoperative complication grading system [47–50]. Postoperative complications were observed in 183 patients (34 %), which in 69 patients (13 %) were recorded as high grade (grades 3–5). The overall 30-day mortality rate was 1.8 %. Level of tumor thrombus according to the Mayo Clinic classification system was shown to be an independent predictor of complications (pooled p = .001), and high-grade complications (pooled p = .029) [51].
Predictive Nomograms for Cancer-Specific Survival
Surgical treatment outcomes in patients with RCC depend on multiple factors. Various clinical and pathological features have been shown to influence prognosis. Different attempts to create models in order to stratify the risk of recurrence and predict survival in these patients have been conducted.
Nomograms derived from large multi-institutional series, integrating all independent prognostic variables that influence a particular oncological setting, have been shown to be more accurate than the TNM staging system for predicting outcomes following treatment. These predictive models combine numerous clinical features to provide a better prediction of survival and recurrence.
The predictive nomogram proposed by Kattan et al. [52] and the stage, size, grade, and necrosis (SSIGN) score from the Mayo Clinic [53, 54] were the first initiatives in the field of RCC. These tables include different factors significantly involved in the risk of recurrence following nerphrectomy for localized RCC. Anatomic tumor extent, histologic tumor subtype and grade, evidence of intratumoral necrosis, presence of clinical symptoms, performance status, and laboratory test parameters were included in these analyses. Models were prospectively validated showing accuracy prediction rates varying from 78 % to 87 % [55–57].
Locally advanced RCC presents multiple clinical scenarios involving a wide range of prognostic situations. Appropriate treatment selection and timely follow-up depend mainly on accurate prediction of survival and disease recurrence. Therefore, the experience gained from the initial attempts in localized RCC gave rise to prognostic tables to be used in the locally advanced setting [52, 53]. Likewise, a predictive model for assessing CSS has been designed and conducted recently using the surgical experience provided by the IRCC-VTC data set [58]. This model was based initially on previously confirmed postoperative prognostic variables, including age, gender, presurgical RAE, nodal status, presence of metastasis, tumor thrombus level, pathologic fat invasion and primary tumor size, stage, and grade. Visible metastasis at the time of surgery (HR 2.5, p < .001), tumor size (HR 1.1, p < .001), and presence of pathologic fat invasion (HR 2.1 p < .001) achieved the independent predictor status to be included in the multivariate analysis. Thereafter, the nomogram was internally validated with a 200-repetition bootstrap analysis. The internal-bootstrapped concordance index was 0.69. This three-variable-based nomogram may be used to predict accurately the probability of 5-year CSS in RCC patients involving the renal vein or the IVC following surgical treatment. In addition, this predictive table may be useful in counseling patients considering surgery for RCC and venous extension.
Conclusions
Involvement of the renal vein or the IVC by tumor is relatively infrequent, accounting for 4 %–10 % of all RCC cases. This unique form of locally advanced RCC presents a wide range of clinical scenarios and different prognostic situations, for which specific surgical approaches have been described. Despite the great clinical and technical variability, complete removal of neoplastic tissue remains the mainstay of treatment in all these cases.
Infrequency and variability make it necessary to share the experience from different institutions to properly analyze surgical outcomes in this setting. IRCC-VTC was created to answer the questions generated by competing results from different retrospective studies in RCC with venous extension on current controversial topics.
On the basis of the analysis of a clinical, surgical, and pathological data set from the world´s largest cohort of patients with RCC and venous involvement to date, several issues concerning prognostic factors, operative procedures, and surgical outcomes in this setting have been addressed. Lessons learned from the IRCC-VTC include the recognition of tumor thrombus anatomic level as an independent survival predictive factor, the confirmation of radical surgery as the mainstay of treatment for these patients even in the metastatic setting, the identification of papillary histological subtype as a magnifier of the oncological risk when compared with other pathological subtypes, and the description of a direct relationship between the tumor thrombus level and the number and severity of complications, making thrombus level according to the Mayo Clinic classification system a strong predictor of perioperative complications in patients with RCC and venous extension.
Abbreviations
- RCC:
-
renal cell carcinoma
- IRCCVTC:
-
international renal cell carcinoma-venous thrombus consortium
- IVC:
-
inferior vena cava
- CPB:
-
cardiopulmonary bypass
- RAE:
-
renal artery embolization
- (AJCC):
-
American Joint Committee on Cancer
- (UICC):
-
Union International Contre le Cancer
- SSIGN:
-
Stage, Size, Grade, Necrosis score
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Siegel R, Naishadham D, Jemal A. Cancer Statistics, 2013 Leido. CA Cancer J Clin. 2013;63(1):11–30.
Ljungberg B, Cowan NC, Hanbury DC, Hora M, Kuczyk MA, Merseburger AS, et al. EAU guidelines on renal cell carcinoma: the 2010 update. European urology. Eur Assoc Urol. 2010;58(3):398–406.
Ljungberg B, Campbell SC, Choi HY, Cho HY, Jacqmin D, Lee JE, et al. The epidemiology of renal cell carcinoma. Eur Urol. 2011;60(4):615–21.
Whitson JM, Reese AC, Meng MV. Population based analysis of survival in patients with renal cell carcinoma and venous tumor thrombus. Urol Oncol. 2013;31(2):259–63. Elsevier Inc.
Méjean A, Oudard S, Thiounn N. Prognostic factors of renal cell carcinoma. J Urol. 2003;169(3):821–7.
Blute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int. 2004;94(1):33–41.
Hatcher P a, Anderson EE, Paulson DF, Carson CC, Robertson JE. Surgical management and prognosis of renal cell carcinoma invading the vena cava. The Journal of urology. 1991. p. 20–3; discussion 23–4.
Ljungberg B, Hanbury D. Guidelines on renal cell carcinoma. European urology.
Ficarra V, Novara G, Iafrate M, Cappellaro L, Bratti E, Zattoni F, et al. Proposal for reclassification of the TNM staging system in patients with locally advanced (pT3-4) renal cell carcinoma according to the cancer-related outcome. Eur Urol. 2007;51(3):722–9. discussion 729–31.
Haferkamp A, Bastian PJ, Jakobi H, Pritsch M, Pfitzenmaier J, Albers P, et al. Renal cell carcinoma with tumor thrombus extension into the vena cava: prospective long-term followup. J Urol. 2007;177(5):1703–8. Long-term follow-up for locally advanced RCC was analyzed representing radical surgery as the only treatment option with benefit in survival. Tumor thrombus level and metastatic disease were independent prognostic factors.
Glazer AA, Novick AC. Long-term followup after surgical treatment for renal cell carcinoma extending into the right atrium. J Urol. 1996;155(2):448–50.
Kim HL, Zisman A, Han K-R, Figlin RA, Belldegrun AS. Prognostic significance of venous thrombus in renal cell carcinoma. Are renal vein and inferior vena cava involvement different? J Urol. 2004;171(2 Pt 1):588–91.
Moinzadeh A, Libertino JA. Prognostic significance of tumor thrombus level in patients with renal cell carcinoma and venous tumor thrombus extension. Is all T3b the same? J Urol. 2004;171(2 Pt 1):598–601.
Martínez-Salamanca JI, Huang WC, Millán I, Bertini R, Bianco FJ, Carballido JA, et al. Prognostic impact of the 2009 UICC/AJCC TNM staging system for renal cell carcinoma with venous extension. Eur Urol. 2011;59(1):120–7. Tumor thrombus renal vein-only involvement had significant CSS difference with IVC involvement. In N0M0 setting, there was no difference in survival for RV and level 1 extent. Thus N+ and M+ remain strong independent predictors for survival of RCC with venous involvement.
Wagner B, Patard J-J, Méjean A, Bensalah K, Verhoest G, Zigeuner R, et al. Prognostic value of renal vein and inferior vena cava involvement in renal cell carcinoma. Eur Urol. 2009;55(2):452–9.
Sosa RE, Muecke EC, Vaughan ED, McCarron JP. Renal cell carcinoma extending into the inferior vena cava: the prognostic significance of the level of vena caval involvement. The Journal of urology. 1984. p. 1097–100.
Klaver S, Joniau S, Suy R, Oyen R, Van Poppel H. Analysis of renal cell carcinoma with subdiaphragmatic macroscopic venous invasion (T3b). BJU Int. 2008;101(4):444–9.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–4.
Gettman MT, Boelter CW, Cheville JC, Zincke H, Bryant SC, Blute ML. Charlson co-morbidity index as a predictor of outcome after surgery for renal cell carcinoma with renal vein, vena cava or right atrium extension. J Urol. 2003;169(4):1282–6.
Spiess PE, Kurian T, Lin H-Y, Rawal B, Kim T, Sexton WJ, et al. Preoperative metastatic status, level of thrombus and body mass index predict overall survival in patients undergoing nephrectomy and inferior vena cava thrombectomy. BJU Int. 2012;110(11 Pt B):E470–4.
Tosco L, Van Poppel H, Frea B, Gregoraci G, Joniau S. Survival and impact of clinical prognostic factors in surgically treated metastatic renal cell carcinoma. Eur Urol. 2013;63(4):646–52.
Naitoh J, Kaplan A, Dorey F, Figlin R, Belldegrun A. Metastatic renal cell carcinoma with concurrent inferior vena caval invasion: long-term survival after combination therapy with radical nephrectomy, vena caval thrombectomy and postoperative immunotherapy. J Urol. 1999;162(1):46–50.
Wu J, Durbin-Johnson B, Martínez-Salamanca JI, Bertini R, Bianco FJ, Carballido J. a, et al. 959 the Impact of Local and Distant Metastasis on Survival in Patients With Renal Cell Carcinoma Undergoing Nephrectomy With Tumor Thrombectomy. J Urol. 2011;185(4):e386.
Capitanio U, Cloutier V, Zini L, Isbarn H, Jeldres C, Shariat SF, et al. A critical assessment of the prognostic value of clear cell, papillary and chromophobe histological subtypes in renal cell carcinoma: a population-based study. BJU Int. 2009;103(11):1496–500.
Keegan KA, Schupp CW, Chamie K, Hellenthal NJ, Evans CP, Koppie TM. Histopathology of surgically treated renal cell carcinoma: survival differences by subtype and stage. J Urol. 2012;188(2):391–7.
Cheville JC, Lohse CM, Zincke H, Weaver AL, Blute ML. Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol. 2003;27(5):612–24.
Ciancio G, Manoharan M, Katkoori D, De Los Santos R, Soloway MS. Long-term survival in patients undergoing radical nephrectomy and inferior vena cava thrombectomy: single-center experience. Eur Urol. 2010;57(4):667–72.
Kaushik D, Linder BJ, Thompson RH, Eisenberg MS, Lohse CM, Cheville JC, et al. The Impact of Histology on Clinicopathologic Outcomes for Patients With Renal Cell Carcinoma and Venous Tumor Thrombus: A Matched Cohort Analysis. Urology. Elsevier Inc.; 2013 May 1.
Kim KH, You D, Jeong IG, Kwon T-W, Cho YM, Hong JH, et al. Type II papillary histology predicts poor outcome in patients with renal cell carcinoma and vena cava thrombus. BJU Int. 2012;110(11 Pt B):E673–8.
Margulis V, Tamboli P, Matin SF, Swanson DA, Wood CG. Analysis of clinicopathologic predictors of oncologic outcome provides insight into the natural history of surgically managed papillary renal cell carcinoma. Cancer. 2008;112(7):1480–8.
Tilki D, Nguyen HG, Dall’era MA, Bertini R, Carballido JA, Chromecki T, et al. Impact of Histologic Subtype on Cancer-specific Survival in Patients with Renal Cell Carcinoma and Tumor Thrombus. European urology. 2013 Jul 10; pii: S0302-2838(13)00663-5. Histologic subtype analysis was performed by the IRCC-VTC, papilar RCC had worse survival outcome when compared with clear cell RCC. Fat invasion and tumor thrombus level were indepedent prognostic factors.
Almgård LE, Fernström I, Haverling M, Ljungqvist A. Treatment of renal adenocarcinoma by embolic occlusion of the renal circulation. Br J Urol. 1973;45(5):474–9.
May M, Brookman-Amissah S, Pflanz S, Roigas J, Hoschke B, Kendel F. Pre-operative renal arterial embolisation does not provide survival benefit in patients with radical nephrectomy for renal cell carcinoma. Br J Radiol. 2009;82(981):724–31.
Zielinski H, Szmigielski S, Petrovich Z. Comparison of preoperative embolization followed by radical nephrectomy with radical nephrectomy alone for renal cell carcinoma. Am J Clin Oncol. 2000;23(1):6–12.
Latal D, Kautzky W, Wanek R, Kumpan W. [Effect of kidney occlusion on survival in renal cell carcinoma: a 10-year retrospective study]. Z Urol Nephrol. 1990;83(1):27–31.
Martínez Salamanca J.I., Bianco, F., Libertino, J., Novick, A., Carballido Rodríguez, J., Russo, P., Pontes, E., Soloway, M., Ciancio, G., Lane, B., Montorsi, F., Terrone, C., Volpe, A., Briganti A. Prognostic significance of preoperative renal artery embolization in renal cell carcinoma with venous extension: a multiinstitutional experience. SUO annual meeting. 2008. p. Abstract.
Novick AC, Kaye MC, Cosgrove DM, Angermeier K, Pontes JE, Montie JE, et al. Experience with cardiopulmonary bypass and deep hypothermic circulatory arrest in the management of retroperitoneal tumors with large vena caval thrombi. Ann Surg. 1990;212(4):472–6. discussion 476–7.
Casey RG, Raheem OA, Elmusharaf E, Madhavan P, Tolan M, Lynch TH. Renal cell carcinoma with IVC and atrial thrombus: A single centre’s 10 year surgical experience. Surgeon: J R Coll Surg Edinb Irel. 2013;44(0):5–9. Elsevier Ltd.
Kuczyk M. a, Münch T, Machtens S, Grünewald V, Jonas U. The impact of extracorporal circulation on therapy-related mortality and long-term survival of patients with renal cell cancer and intracaval neoplastic extension. World J Urol. 2002;20(4):227–31.
Stewart JR, Carey JA, McDougal WS, Merrill WH, Koch MO, Bender HW. Cavoatrial tumor thrombectomy using cardipulmonary bypass without circulatory arrest. The Annals of Thoracic Surgery. Soc Thorac Surg. 1991;51(5):717–22.
Langenburg SE, Blackbourne LH, Sperling JW, Buchanan SA, Mauney MC, Kron IL, et al. Management of renal tumors involving the inferior vena cava. J Vasc Surg. 1994;20(3):385–8.
Ciancio G, Livingstone AS, Soloway M. Surgical management of renal cell carcinoma with tumor thrombus in the renal and inferior vena cava: the University of Miami experience in using liver transplantation techniques. Eur Urol. 2007;51(4):988–94. discussion 994–5. Surgery still remains the most effective therapeutic option, and aggressive approaches have to be considered. Proper assessment of the level of the thrombus is mandatory; a transabdominal approach can be performed for higher levels when combined with liver transplant techniques.
Shuch B, Crispen PL, Leibovich BC, Larochelle JC, Pouliot F, Pantuck AJ, et al. Cardiopulmonary bypass and renal cell carcinoma with level IV tumour thrombus: can deep hypothermic circulatory arrest limit perioperative mortality? BJU Int. 2011;107(5):724–8.
Martinez-Salamanca JI, Huang W, Capitanio U, Millan I, Bertini R, Bianco F, et al. 1760 Impact of Cardiopulmonary By-Pass in Cancer-Specific Survival in Patients With Renal Cell Carcinoma and Level Iii/Iv Thrombus. International Renal Cell-Carcinoma-Venous Thrombus Consortium. J Urol. 2011;185(4):e706.
Neves RJ, Zincke H. Surgical treatment of renal cancer with vena cava extension. Br J Urol. 1987;59(5):390–5.
Libertino J a, Zinman L, Watkins E. Long-term results of resection of renal cell cancer with extension into inferior vena cava. The Journal of urology. 1987. p. 21–4.
Donat SM. Standards for surgical complication reporting in urologic oncology: time for a change. Urology. 2007;69(2):221–5.
Yoon PD, Chalasani V, Woo HH. Use of Clavien-Dindo Classification in reporting and grading of complications after urologic surgical procedures; Analysis of 2010-2012. The Journal of urology. 2013.
Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–26.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Martínez-Salamanca JI, Novara G, Bertini R, Carballido J, Chromecki T, Ciancio G, et al. 1907 Level of Thrombous According To Mayo Clinic Classification Is an Independent Predictor of Perioperative Complications and Cancer-Related Outcome: Data of the Ircvt Rcc Venous Thrombus Consortium. J Urol. 2013;189(4):e782. Elsevier Inc.
Kattan MW, Reuter V, Motzer RJ, Katz J, Russo P. A postoperative prognostic nomogram for renal cell carcinoma. J Urol. 2001;166(1):63–7.
Cindolo L, Patard J-J, Chiodini P, Schips L, Ficarra V, Tostain J, et al. Comparison of predictive accuracy of four prognostic models for nonmetastatic renal cell carcinoma after nephrectomy: a multicenter European study. Cancer. 2005;104(7):1362–71.
Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol. 2002;168(6):2395–400.
Karakiewicz PI, Briganti A, Chun FK-H, Trinh Q-D, Perrotte P, Ficarra V, et al. Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol: Off J Am Soc Clin Oncol. 2007;25(11):1316–22.
Sorbellini M, Kattan MW, Snyder ME, Reuter V, Motzer R, Goetzl M, et al. A postoperative prognostic nomogram predicting recurrence for patients with conventional clear cell renal cell carcinoma. J Urol. 2005;173(1):48–51.
Veeratterapillay R, Rakhra S, El-sherif A, Johnson M, Soomro N, Heer R. Can the Kattan nomogram still accurately predict prognosis in renal cell carcinoma using the revised 2010 tumor – nodes – metastasis reclassification ? 2012;773–6.
Martinez-Salamanca JI, Capitanio U, Huang W, Millan I, Bertini R, Bianco F, et al. 534 Cancer-Specific Survival Nomogram for Renal Tumors With Venous Extension:International Renal Cell-Carcinoma-Venous Thrombus Consortium. J Urol. 2011;185(4):e217.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Juan I. Martínez-Salamanca, Dr. Estefania Linares, Dr. Javier González, Dr. Roberto Bertini, Dr. Joaquín A. Carballido, Dr. Thomas Chromecki, Dr. Sia Daneshmand, Dr. Christopher P. Evans, Dr. Paolo Gontero, Dr. Axel Haferkamp, Dr. Markus Hohenfellner, Dr. William C. Huang, Dr. Theresa M. Koppie, Dr. Viraj A. Master, Dr. Rayan Matloob, Dr. James M. McKiernan, Dr. Carrie M. Mlynarczyk, Dr. Francesco Montorsi, Dr. Hao G. Nguyen, Dr. Giacomo Novara, Dr. Sascha Pahernik, Dr. Juan Palou, Dr. Raj S. Pruthi, Dr. Krishna Ramaswamy, Dr. Oscar Rodriguez Faba, Dr. Paul Russo, Dr. Shahrokh F. Shariat, Dr. Martin Spahn, Dr. Carlo Terrone, Dr. Derya Tilki, Dr. Daniel Vergho, Dr. Eric M. Wallen, Dr. Evanguelos Xylinas, Dr. Richard Zigeuner, and Dr. John A. Libertino each declare no potential conflicts of interest relevant to this article.
Dr. Gaetano Ciancio is a section editor for Current Urology Reports.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Kidney Diseases
Rights and permissions
About this article
Cite this article
Martínez-Salamanca, J.I., Linares, E., González, J. et al. Lessons learned from the International Renal Cell Carcinoma-Venous Thrombus Consortium (IRCC-VTC). Curr Urol Rep 15, 404 (2014). https://doi.org/10.1007/s11934-014-0404-7
Published:
DOI: https://doi.org/10.1007/s11934-014-0404-7