Abstract
Statin medications have recently been shown to cause not only a toxic myopathy but also an immune-mediated necrotizing myositis. Before the discovery of a specific anti-HMG-CoA reductase antibody occurring in conjunction with a necrotizing myopathy, many of these patients may have been classified as polymyositis. They present similarly with proximal muscle weakness, elevated muscle enzymes, persistence of symptoms despite cessation of the statin, with need for immunosuppression. This article provides an overview of this novel disease entity by placing it in the context of existing idiopathic inflammatory myopathy (IIM) classification criteria, and in the range of statin-associated muscle toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Our understanding of the autoimmune myopathies has evolved rapidly in recent years because of new discoveries, particularly in relation to myositis-related antibodies. Whereas, traditionally, autoimmune myopathies had been subdivided into polymyositis (PM) and dermatomyositis (DM), additional distinct subgroups are now recognized.
The discovery of statin-associated myositis among patients with antibodies recognizing HMG-CoA reductase is an example of pathologic and clinicoserologic correlations leading to the recognition of a new disease. Whether we classify this disease within the range of PM is largely a matter of which criteria are used. We will discuss this novel entity in the context of two classification schemes, the classic Bohan and Peter criteria [1, 2] and a more recent set of criteria published by the European Neuromuscular Center [3].
The Bohan and Peter Criteria
The most widely accepted classification scheme for myositis remains the Bohan and Peter criteria published in 1975 [1, 2]. In this iteration, both PM and DM are recognized as inflammatory myopathies presenting with subacute symmetrical muscle weakness; they are differentiated primarily by the presence of skin involvement in the latter. Five major criteria are used to confirm the diagnosis of PM and DM: the presence of symmetric proximal weakness, consistent muscle biopsy findings, elevated muscle enzymes, electromyographic findings of myopathy, and characteristic skin rashes (Table 1). Patients can be categorized as having definite (four criteria for PM, three or four criteria plus rash for DM), probable (three criteria for PM, two criteria plus rash for DM), or possible (two criteria for PM, one criterion plus rash for DM) disease. However, muscle biopsy findings were not used to differentiate between PM and DM. Further work has shown that, although DM and PM have many similarities, each seems to be a distinct pathophysiological entity. Histologically, the characteristic feature of DM is perifascicular atrophy, perhaps the result of a microangiopathy [4] associated with C5b-9 membrane attack complex deposition in the intramuscular microvasculature [5]. In DM, there is a paucity of lymphocytic invasion of non-necrotic fibers. Rather, inflammatory infiltrates are located in the perimysial area with a large number of CD4+ compared with CD8+ cells. These findings have led some to speculate that humoral processes drive DM. In contrast, PM seems to be mediated by CD8+ T cells, which surround and invade non-necrotic fibers [6]. In both PM and DM, there may be upregulation of MHC class I antigen in muscle fibers [7].
Based on advances in our understanding of the autoimmune myopathies, alternative classification criteria have been proposed to improve the original set of Bohan and Peter [4, 8–12]. Still, none has been as widely accepted for use in research studies or for enrollment in clinical trials.
Immune-Mediated Necrotizing Myopathy: A Newly Recognized Form of Autoimmune Myopathy
In 2003, a working group of the ENMC met and proposed a classification scheme relying heavily on muscle biopsy findings as developed by Anthony Amato and the Muscle Study Group [3]. In this scheme, the idiopathic inflammatory myopathies were divided into DM, PM, inclusion body myositis (IBM), and non-specific myositis (among patients with non-specific perimysial and/or perivascular infiltrates but without features diagnostic of PM or DM). Furthermore, immune-mediated necrotizing myopathy (IMNM) was recognized as a distinct form of autoimmune muscle disease in which muscle biopsies reveal muscle cell necrosis and degeneration with a lack of significant inflammatory infiltrates.
Importantly, because muscle cell necrosis is a non-specific feature that can occur in many muscle-damaging processes, immune-mediated necrotizing myopathies must be differentiated from toxic myopathies, endocrinopathies, and muscular dystrophies. In a recent study comparing immune versus non-immune necrotizing myopathy [13•], diffuse and strong MHC-1 up-regulation in normal fibers was seen only in the immune-mediated form. In contrast, only necrotic fibers had increased MHC-1 expression in non-immune-mediated necrotizing myopathies. Other features seen mainly in IMNM include the presence of complement deposition on capillaries and decoration of the sarcolemma of non-necrotic fibers by membrane attack complex. Although a relative paucity of inflammatory infiltrates have marked the necrotizing myopathies, small numbers of perimysial and endomysial CD4+ and CD8+ cells and predominantly CD68 macrophages, irrespective of myophagocytosis, may be seen. IMNM muscle tissue also included high levels of IFN-γ, TNF-α, IL-12, and STAT-1, suggesting a Th1-mediated disease [13•].
Myositis Autoantibodies
As with other autoimmune diseases, autoantibodies in myositis are linked to unique phenotypic expressions. To date, at least fifteen myositis-specific antibodies have been found, each with a characteristic clinical syndrome [14–16] (Table 2). Tests for most of these antibodies are now available commercially. Although muscle biopsy has been regarded as essential for diagnosis of inflammatory myopathies, much heterogeneity in clinical presentation is seen, even among those with similar appearing biopsies. For example, in one study including 38 patients with necrotizing muscle biopsies [17], four had the anti-synthetase syndrome (characterized by the presence of interstitial lung disease and other systemic manifestations of autoimmunity), six had anti-SRP associated myopathy (a severe autoimmune myopathy with minimal extramuscular manifestations), and 10 had statin-associated autoimmune myopathy with anti-HMGCR antibodies (see below). Thus, basic histological features may be of limited utility in distinguishing different forms of autoimmune myopathy, and myositis autoantibodies may provide important complementary information regarding diagnosis, prognosis, and etiology. Not surprisingly then, novel classification schemes incorporating myositis autoantibody profiles have been proposed [10–12, 18].
What Happened to Polymyositis?
The reader may note that although there are anti-synthetase antibodies, DM-specific antibodies, and antibodies associated with IMNM, there are no PM-specific antibodies. Rather, PM has become a disease of exclusion, defined by the presence of inflammatory cells on muscle biopsy in those without DM rash, genetic muscle disease, endocrinopathy, myotoxic drug exposure, or IBM [4]. The ENMC criteria include more strict histologic criteria that require the presence of CD8+ T cells surrounding and invading non-necrotic muscle fibers [3] for diagnosis of PM. In clinical practice, however, diagnosis of PM is frequently made when the muscle biopsy shows inflammation and when DM, IBM, and other non-immune-mediated conditions have been excluded.
It is now clear that PM may be an over-diagnosed entity. In 2003, a study investigated the applicability of diagnostic features for diagnosing PM and DM in a large unselected group of patients previously diagnosed to have myositis [19]. Of 165 patients, nine were initially diagnosed as having Bohan and Peter definite PM on the basis of clinical, laboratory, and biopsy findings. After a follow-up period of at least one year, five of the nine patients had typical IBM features, and none of the remaining four continued to have typical signs of PM. Similarly, another group noted that of 46 cases with a PM pattern on biopsy, 36 were associated with another disease [20]. Of the remaining ten with isolated PM, only one continued to carry that diagnosis after follow-up and re-evaluation. This emphasizes that pure PM is probably even more rare than previously appreciated.
Statin Induced Myopathy
Self-Limited Statin Myopathy
The statin medications used by millions of patients to reduce serum cholesterol levels, have long been known to cause muscle-related side effects. These range in severity from asymptomatic muscle enzyme elevation to life-threatening rhabdomyolysis. Myalgias are the most common side effect with prevalence estimated to be approximately 10 % [21, 22]. Myopathy, defined as elevated muscle enzymes accompanied by symptoms of pain, cramps, or weakness, can also occur. Myopathy with creatine kinase >10 times the upper limit of normal occurs in five patients per 100,000 person years and increases with high-dose statin use [23]. Rhabdomyolysis, the most ominous complication of statin use, is marked elevation of creatine kinase (>10 × ULN) as a result of acute and massive destruction of muscle fibers resulting in release of muscle fiber contents into the bloodstream. It is a clinical syndrome that can result in renal failure and death, with incidence of 0.44 per 10,000 person years of use [24].
The mechanisms by which statins exert direct muscle toxicity are complex and not yet fully understood [25]. Potential mechanisms for the toxic effect of statins include a change in muscle membrane excitability, because of modulation in membrane cholesterol, impaired mitochondrial function and calcium signaling, induction of apoptosis, and increased lipid peroxidation [26]. Factors that predispose patients to developing statin toxicity include high statin dose, advanced patient age, co-administration of drugs that interfere with statin metabolism, and concurrent hypothyroidism. Furthermore, individuals may have genetic susceptibility to statin toxicity. Specifically a genome-wide association study revealed a strong association between a single nucleotide polymorphism within the SLCO1B1 gene and myopathy with statins [27]. SLCO1B1 encodes a protein that is involved in hepatic uptake of statins, thereby controlling the blood level of statins. Patients homozygous for the C allele of the gene had the highest risk for myopathy [27]. These findings provided strong evidence that genetic susceptibility factors are significant in predisposing patients to statin-induced myopathy.
The range of muscle-related effects described above are regarded as toxic, non-inflammatory, and self-limiting. Importantly, discontinuation of the drug results in cessation of muscle damage and resolution of symptoms. In contrast, progressive immune-mediated myopathy related to statin use has also recently been described [17, 28, 29].
Statin-Associated Immune-Mediated Myopathy
Reports of patients developing an autoimmune myopathy in the context of statin use have been published since the late 1980s [30–32]. However, the cases were isolated and the link to statin use was never proven. In 2007, eight patients were described by Needham et al. who had been exposed to statins and developed progressive muscle weakness despite cessation of the drug [29]. Their muscle biopsies revealed prominent myofiber necrosis with a paucity of inflammatory infiltrate. The presence of increased MHC-1 expression on biopsy and a clear requirement for immunosuppressive therapy suggested an immune-mediated mechanism. In 2010, Esposito and colleagues reported a group of 25 patients that developed a necrotizing myopathy while on statins [28], had progressive symptoms after stopping statins, and required treatment with steroids and immunosuppressants. This cohort of patients had a significantly higher frequency of statin use than age-matched control patients with dermatomyositis, polymyositis, or inclusion body myositis.
Working in parallel, investigators at the Johns Hopkins Myositis Center performed screening for novel autoantibodies among a group of patients with necrotizing myopathy on biopsy without a known underlying etiology [17]. A subgroup of these patients had autoantibodies recognizing 200 and 100-kD proteins. These antibodies were specific for patients with a necrotizing myopathy and were not found in controls or patients with PM, DM, or IBM. Surprisingly, a much higher proportion of anti-200/100 positive patients over the age of 50 had been exposed to statins (83 %) compared with age-matched patients with DM (25 %), PM (37 %), and IBM (33 %). This finding suggested that this may be an immune-mediated myopathy frequently associated with statin use.
A follow-up study identified the 200 and 100-kD proteins targeted in statin-associated immune-mediated necrotizing myopathy [33•]. Remarkably, the 100-kD protein was determined to be HMG-CoA reductase (HMGCR), the pharmacologic target of the statins, with the 200-kD protein likely to be an HMGCR dimer. This antibody was found in ~6 % of patients seen at the Myositis Center, with most positive patients having a necrotizing myopathy on biopsy. Although some anti-HMGCR positive subjects did not have a history of statin exposure, among those who were 50 years old and above, 92.3 % had been on a statin. Importantly, anti-HMGCR autoantibodies are not found in statin-exposed subjects without myopathy and are not found in patients with self-limited statin myopathy [34•].
Risk factors for developing the self-limited statin myopathy and for the immune-mediated myopathy appear distinct. Whereas patients with self-limited statin myopathy have an increased frequency of a SLCO1B1 single nucleotide polymorphism, those with progressive anti-HMGCR myopathy do not [33•]. Rather, HLA typing has shown that the class II allele DRB1*11:01 confers an increased risk for the anti-HMGCR among both whites and African Americans [35•]. In contrast, HLA class II alleles DQA1 and DQB6 seemed to be protective.
Of note, statin exposure has been shown to increase expression of HMGCR [33•]. For patients positive for the antibody, expression of HMGCR was also found to be upregulated in the regenerating muscle fibers, even after statins were discontinued. It has been suggested that exposure to statins upregulates expression of HMGCR, triggering an autoimmune response against the antigen. Because expression of HMGCR continues in regenerating muscle tissue, this constant source of antigen could perpetuate the immune response even when the medications are discontinued. This serves as an interesting model for the mechanism by which a drug can provoke an autoimmune response.
Clinical Features
Patients with anti-HMGCR myopathy have a similar presentation to other patients with autoimmune muscle disease, developing symmetric proximal weakness over the course of weeks to months [17, 28, 29]. Symptoms can occur at any point in statin treatment with an average duration of three years of statin use before the onset of weakness (range two months to three years). Because myalgias are common, occurring in ~75 % of patients, many of these individuals are initially diagnosed with self-limited statin myopathy. However, persistence and progression of symptoms is the rule even after discontinuation of the medication. If the weakness is severe, dysphagia and distal involvement are also observed. Other systemic manifestations, for example arthralgias and Raynaud’s phenomenon, are infrequently noted.
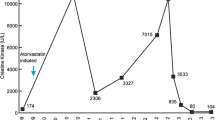
Muscle enzymes are strikingly high with a mean CPK value of 10,000 IU L−1 at initial presentation [17]. Interestingly, some patients maintain normal strength despite markedly elevated muscle enzymes, with a threshold CPK of 3,000–7,000 at which weakness begins to occur (personal observation). Inflammatory markers need not be elevated and the association with other antibodies, for example ANA, is not often seen. Muscle MRI typically shows muscle edema, with atrophy, fatty replacement, and fascial edema occurring in some cases. EMG of an involved muscle reveals an irritable myopathy in most cases and a non-irritable myopathy in a few.
Muscle biopsy for patients with anti-HMGCR reveals prominent necrotic and regenerating fibers [28]. As in other forms of autoimmune myopathy, diffuse or focal upregulation of MHC-1 expression may be observed [29]. Although scarce endomysial and perivascular inflammatory cells may be present, the degree of inflammation is much less than for patients with typical DM or PM biopsies. These findings are consistent with the diagnosis of IMNM as detailed in the ENMC criteria.
It is important to note that a subgroup of patients with anti-HMGCR necrotizing myopathy have never been exposed to statins. This statin naïve group tended to be younger at diagnosis, have higher CPK levels, and were more frequently non-white [33•]. Other genetic or environmental factors may be the cause of increased HMGCR expression in these patients. Importantly, these non-statin-exposed anti-HMGCR-positive subjects may be less responsive to treatment than those anti-HMGCR subjects who developed myopathy after statin exposure [36].
Management
When statin-exposed patients have muscle symptoms and CK elevation that do not resolve with discontinuation of the statin, statin-associated IMNM should be suspected and an anti-HMGCR antibody should be checked. This is now commercially available through the RDL reference laboratory. For patients with antibody-confirmed statin-associated IMNM, the statin should be discontinued and immunosuppressive treatment should be commenced. Most patients respond favorably to immunosuppression with steroids or another immunosuppressants [17, 28, 29]. Immunosuppressants that have been used include methotrexate, azathioprine, mycophenolate mofetil, rituximab, and intravenous immunoglobulin (IVIG). Although the optimum treatment has yet to been defined for this disease, our experience is that IVIG is particularly beneficial. Relapses can occur with tapering of immunosuppression, and with re-exposure to statins. Whether some anti-HMGCR-positive patients with significant cardiovascular risk factors can ever be safely re-exposed to statins remains to be determined.
Conclusions
Statin-associated myositis can be defined as an autoimmune myopathy, on the basis of the presence of a specific autoantibody, upregulation of MHC-1 expression on biopsy, immunogenetic risk factors, and response to immunosuppression. Using the Bohan and Peter criteria, the vast majority of these patients would be classified as having probable or definite PM. However, according to the more modern ENMC diagnostic scheme, these patients would be classified has having IMNM and not PM. Irrespective of nomenclature, testing for the anti-HMGCR antibody should be considered for those who develop a progressive myopathy after statin exposure and for those with predominantly necrotizing myopathies when an immune-mediated process is included in the differential diagnosis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292(7):344–7.
Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975;292(8):403–7.
Hoogendijk JE, Amato AA, Lecky BR, Choy EH, Lundberg IE, Rose MR, et al. 119th ENMC international workshop: Trial design in adult idiopathic inflammatory myopathies, with the exception of inclusion body myositis, 10–12 October 2003, Naarden, The Netherlands. Neuromuscul Disord. 2004;14(5):337–45.
Dalakas M. Polymyositis, dermatomyositis and inclusion body myositis. N Engl J Med. 1991;325(21):1487–98.
Kissel JT, Mendell JR, Rammohan KW. Microvascular Deposition of Complement Membrane Attack Complex in Dermatomyositis. N Engl J Med. 1986;314(6):329–34.
Arahata K, Engel AG. Monoclonal antibody analysis of mononuclear cells in myopathies. I: Quantitation of subsets according to diagnosis and sites of accumulation and demonstration and counts of muscle fibers invaded by T cells. Ann Neurol. 1984;16(2):193–208.
Emslie-Smith A, Arahata K, Engel AG. Major histocompatibility complex class 1 antigen expression, immunolocalization of interferon subtypes, and T cell-mediated cytotoxicity in myopathies. Hum Pathol. 1989;20(3):224–31.
Tanimoto K, Nakano K, Kano S, Mori S, Ueki H, Nishitani H, et al. Classification criteria for polymyositis and dermatomyositis. J Rheumatol. 1995;22(4):668–74.
Linklater H, Pipitone N, Rose M, Norwood F, Campbell R, Salvarani C, et al. Classifying idiopathic inflammatory myopathies: comparing the performance of six existing criteria. Clin Exp Rheumatol. 2013;31(5):767–9.
Fernandez C, Bardin N, De Paula AM, Salort-Campana E, Benyamine A, Franques J, et al. Correlation of Clinicoserologic and Pathologic Classifications of Inflammatory Myopathies: Study of 178 Cases and Guidelines for Diagnosis. Medicine (Baltimore). 2013;92(1):15–24.
Troyanov Y, Targoff IN, Tremblay J-L, Goulet J-R, Raymond Y, Senecal J-L. Novel Classification of Idiopathic Inflammatory Myopathies Based on Overlap Syndrome Features and Autoantibodies: Analysis of 100 French Canadian Patients. Medicine (Baltimore). 2005;84(4):231–49.
Targoff IN, Miller FW, Medsger TA, Oddis CV. Classification criteria for the idiopathic inflammatory myopathies. Curr Opin Rheumatol. 1997;9(6):527–35.
Preuße C, Goebel HH, Held J, Wengert O, Scheibe F, Irlbacher K, et al. Immune-Mediated Necrotizing Myopathy Is Characterized by a Specific Th1-M1 Polarized Immune Profile. Am J Pathol. 2012;181(6):2161–71. This study demonstrated that a difference in cellular and molecular characteristics can distinguish immune-mediated necrotizing myopathies from non-immune-mediated necrotizing myopathies.
Tansley SL, Betteridge ZE, McHugh NJ. The diagnostic utility of autoantibodies in adult and juvenile myositis. Curr Opin Rheumatol. 2013;25(6):772–7.
Ghirardello A, Bassi N, Palma L, Borella E, Domeneghetti M, Punzi L, et al. Autoantibodies in Polymyositis and Dermatomyositis. Curr Rheumatol Rep [Internet]. 2013. [cited 2014 May 21];15(6). Available from: 10.1007/s11926-013-0335-1
Cruellas M, Viana V, Levy-Neto M, Souza F, Shinjo S. Myositis-specific and myositis-associated autoantibody profiles and their clinical associations in a large series of patients with polymyositis and dermatomyositis. Clinics. 2013;68(7):909–14.
Christopher-Stine L, Casciola-Rosen LA, Hong G, Chung T, Corse AM, Mammen AL. A novel autoantibody recognizing 200-kd and 100-kd proteins is associated with an immune-mediated necrotizing myopathy. Arthritis Rheum. 2010;62(9):2757–66.
Tansley S, Gunawardena H. The Evolving Spectrum of Polymyositis and Dermatomyositis—Moving Towards Clinicoserological Syndromes: A Critical Review. Clin Rev Allergy Immunol [Internet]. 2013. [cited 2014 Mar 1]; Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s12016-013-8387-6
Van der Meulen MFG, Bronner IM, Hoogendijk JE, Burger H, van Venrooij WJ, Voskuyl AE, et al. Polymyositis: An overdiagnosed entity. Neurology. 2003;61(3):316–21.
Milisenda JC, Selva-O’Callaghan A, Grau JM. The diagnosis and classification of polymyositis. J Autoimmun [Internet]. 2014 [cited 2014 Mar 1]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S0896841114000286
Harris LJ, Thapa R, Brown M, Pabbathi S, Childress RD, Heimberg M, et al. Clinical and laboratory phenotype of patients experiencing statin intolerance attributable to myalgia. J Clin Lipidol. 2011;5(4):299–307.
Bruckert E, Hayem G, Dejager S, Yau C, Bégaud B. Mild to Moderate Muscular Symptoms with High-Dosage Statin Therapy in Hyperlipidemic Patients —The PRIMO Study. Cardiovasc Drugs Ther. 2006;19(6):403–14.
Law M, Rudnicka AR. Statin Safety: A Systematic Review. Am J Cardiol. 2006;97(8):S52–60.
Graham DJ, Staffa JA, Shatin D, et al. INcidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs. JAMA. 2004;292(21):2585–90.
Mammen A, Amato AA. Statin myopathy: a review of recent progress. Curr Opin Rheumatol. 2010;22(6):644–50.
Sirvent P, Mercier J, Lacampagne A. New insights into mechanisms of statin-associated myotoxicity. Curr Opin Pharmacol. 2008;8(3):333–8.
SLCO1B1 Variants and Statin-Induced Myopathy — A Genomewide Study. N Engl J Med. 2008;359(8):789–99.
Grable-Esposito P, Katzberg HD, Greenberg SA, Srinivasan J, Katz J, Amato AA. Immune-mediated necrotizing myopathy associated with statins. Muscle Nerve. 2010;41(2):185–90.
Needham M, Fabian V, Knezevic W, Panegyres P, Zilko P, Mastaglia FL. Progressive myopathy with up-regulation of MHC-I associated with statin therapy. Neuromuscul Disord. 2007;17(2):194–200.
Goldman J, Fishman A, Lee J, Johnson R. The role of cholesterol-lowering agents in drug-induced rhabdomyolysis and polymyositis. Arthritis Rheum. 1989;32(3):358–9.
Schalke B, Schmidt B, Toyka K, Hartung H. Pravastatin-Associated Inflammatory Myopathy. N Engl J Med. 1992;327(9):649–50.
Giordano N, Senesi M, Mattii G, Battisti E, Villanova M, Gennari C. Polymyositis associated with simvastatin. Lancet. 1997;349(9065):1600–1.
Mammen AL, Chung T, Christopher-Stine L, Rosen P, Rosen A, Doering KR, et al. Autoantibodies against 3-hydroxy-3-methylglutaryl-coenzyme A reductase in patients with statin-associated autoimmune myopathy. Arthritis Rheum. 2011;63(3):713–21. This study identified the autoantigen involved in statin-associated autoimmune myopathy and provided a mechanistic link between the drug and development of sustained autoimmunity.
Mammen AL, Pak K, Williams EK, Brisson D, Coresh J, Selvin E, et al. Rarity of anti-3-hydroxy-3-methylglutaryl-coenzyme A reductase antibodies in statin users, including those with self-limited musculoskeletal side effects. Arthritis Care Res. 2012;64(2):269–72. This study demonstrated that anti-HMGCR is infrequently seen in patients who take statins, including those with self-limited statin intolerance, and is specific for an autoimmune myopathy.
Mammen AL, Gaudet D, Brisson D, Christopher-Stine L, Lloyd TE, Leffell MS, et al. Increased frequency of DRB1*11:01 in anti-HMG-CoA reductase-associated autoimmune myopathy. Arthritis Care Res. 2012;1233–7. This study identified class II HLA loci that confer susceptibility to and protection from anti-HMGCR myopathy.
Werner JL, Christopher-Stine L, Ghazarian SR, Pak KS, Kus JE, Daya NR, et al. Antibody levels correlate with creatine kinase levels and strength in anti-3-hydroxy-3-methylglutaryl-coenzyme A reductase-associated autoimmune myopathy. Arthritis Rheum. 2012;64(12):4087–93.
Cabot RC, Harris NL, Rosenberg ES, Shepard J-AO, Cort AM, Ebeling SH, et al. Case 37-2012: A 21-Year-Old Man with Fevers, Arthralgias, and Pulmonary Infiltrates. N Engl J Med. 2012;367(22):2134–46.
Compliance With Ethics Guidelines
ᅟ
Conflict of Interest
Jemima Albayda declares that she has no conflict of interest. Andrew L. Mammen reports grants from NIH during the conduct of the study. In addition, Dr Mammen has patented an anti-HMGCR antibody test from which he is entitled to receive royalties from INOVA Diagnostics.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Topical Collection on Inflammatory Muscle Disease
Rights and permissions
About this article
Cite this article
Albayda, J., Mammen, A.L. Is Statin-Induced Myositis Part of the Polymyositis Disease Spectrum?. Curr Rheumatol Rep 16, 433 (2014). https://doi.org/10.1007/s11926-014-0433-8
Published:
DOI: https://doi.org/10.1007/s11926-014-0433-8