Abstract
Systemic sclerosis (SSc) is a heterogeneous condition characterized by the deposition of excess collagen in skin and internal organs due to vasculopathy, immune activation, low grade inflammation, and fibrosis. Progressive diffuse cutaneous SSc with organ involvement has a poor prognosis. The employment of autologous hematopoietic stem cell transplantation (HSCT) as a means to escalate immunosuppressive therapy has resulted in rapid and sustained improvement of skin thickening and functional ability, stabilization of major organ function with some improvement of vital capacity in pilot studies, registry analyses, and the phase II ASSIST trial. Results from the phase III ASTIS trial corroborate these findings and show long-term survival benefit of HSCT. The ASTIS and SCOT trials will determine whether the benefits of HSCT outweigh the risks of serious adverse events including treatment-related mortality of around 6–10 % and potential long-term complications. Better patient selection and safer transplant regimens may improve the outcome of HSCT for SSc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a heterogeneous condition characterized by the deposition of excess collagen in skin and internal organs. The prevailing concept is that SSc starts as a diffuse vasculopathy, followed by immune activation, low grade inflammation, and subsequent tissue fibrosis [1].
There are two major clinical subsets of the disease: limited cutaneous (lcSSc) and diffuse cutaneous (dcSSc) forms, which can be differentiated by the extent of the skin involvement, the autoantibody profile, and the pattern of organ involvement [2]. Patients with dcSSc with organ involvement have a poor prognosis with high mortality. Disease-related causes, in particular pulmonary fibrosis, pulmonary arterial hypertension and cardiac causes, account for the majority of deaths in SSc [3]. SSc is amenable to treatment with immunosuppressive therapy, and outcomes have improved due to better care and more optimal use of immunosuppressive medication such as mycophenolate mofetil [4]. The results of the Scleroderma Lung Study, a double-blind, randomized, placebo-controlled trial with oral cyclophosphamide in158 US patients, showed that oral cyclophosphamide when compared with placebo had a statistically significant but modest beneficial effect on lung function, dyspnea, skin thickening, and the health-related quality of life [5]. A follow-up trial of the SLS I trial (SLS II) is in progress to compare efficacy of cyclophosphamide with mycophenolate mofetil (NCT00883129). More recently, in an observational study, the effectiveness of tocilizumab and abatacept was assessed in 20 SSc patients with refractory polyarthritis and myopathy from the EUSTAR (European League Against Rheumatism, EULAR, Scleroderma Trials and Research) network [6]. The results showed that, although tocilizumab and abatacept appear to be safe and effective on joints in patients with refractory SSc, there was no significant change in skin or lung fibrosis. A phase II/III, multicenter, randomized, double-blind, placebo-controlled study on the efficacy and safety of tocilizumab versus placebo in patients with SSc is ongoing (EudraCT Number: 2011-001460-22) [7]. Rituximab has also been used in several open label trials with variable success [8]. The use of biologicals has recently been subjected to systematic review [9], with the conclusion that there is at the moment insufficient evidence to recommend any in particular in SSc and that further studies are needed.
Autologous Hematopoietic Stem Cell Transplantation in SSc
Hematopoietic stem cell transplantation (HSCT) has been increasingly employed as a potential alternative treatment for severe autoimmune diseases, including progressive dcSSc [10–12]. Autologous HSCT is the most widely used form of HSCT [13, 14]. Allogeneic HSCT, though potentially curative, carries significant risk of rejection and graft-versus-host disease and has therefore not been extensively studied [15].
The rationale for autologous HSCT in autoimmune diseases (AD) is the ablation of an aberrant or self-reactive immune system by high-dose chemotherapy and/or lymphoablative antibodies or total body irradiation and regeneration of a new and hopefully self-tolerant immune system from hematopoietic stem cells [16]. HSCT is a complex, multistep procedure involving mobilization and harvesting of hematopoietic stem cells (HSCs) from blood or bone marrow, immunoablative therapy (referred to as ‘conditioning’), and reinfusion of HSCs (Fig. 1) [13, 17]. In autologous HSCT, conditioning with high-dose cyclophosphamide, anti-thymocyte globulin (ATG), and/or total body irradiation (TBI) deletes the majority of autoreactive effector cells of the host. Both adaptive and innate immune cells, including B and T lymphocytes, monocytes, natural killer cells, and dendritic cells, are affected. This intensive immunosuppressive effect is considered to be the key effect of HSCT on autoimmune disease at least in the short term, although there are also intriguing data on other mechanisms of action [18].
Autologous hematopoietic stem cell transplantation (HSCT) is a complex multistep procedure. The treatment starts with mobilisation of CD34+ hematopoietic stem cells (HSC) from peripheral blood by treatment with granulocyte colony-stimulating factor (G-CSF) and cyclophosphamide. HSC are collected by leukapheresis and the resulting product is then enriched for CD34+ HSC using immunomagnetic beads and cryopreserved. After several weeks to months patients undergo ‘conditioning’ with high dose chemotherapy ± antithymocyte globuline (ATG) and/or total body irradiation (TBI), followed by reinfusion of CD34+ progenitor cells. The combination of high dose cyclophosphamide and ATG is nonmyeloablative, leaving bone marrow stem cells intact, whereas the use of TBI and chemotherapeutic agents such as busulfan renders conditioning myeloablative, depending on the doses used. I.v., intravenous; s.c., subcutaneous. [20] (Figure adapted from Hügle T, van Laar JM: Stem cell transplantation for rheumatic autoimmune diseases. Arthritis Res Ther 2008;10:217)
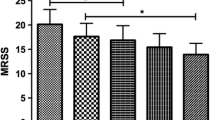
Consensus indications for autologous HSCT in AD were first published in 1997 and have recently been updated [19]. These stipulated that HSCT should only be done in patients in whom conventional therapy had failed, but in whom enough reversible pathology still remained to ensure a decent quality of life if treatment were successful. The early results from the various phase I/II clinical trials showed that autologous stem cell transplantation is feasible in carefully selected patients with dcSSc [20–22]. The trials showed a significant reduction in the modified Rodnan skin score (mRSS) in a large proportion of patients although early transplant-related mortality (TRM) was also high (17 %) in the first European Group for Blood and Marrow Transplantation (EBMT) Working Party analysis [20]. As a result, inclusion criteria and screening process for patient selection in HSCT in SSc were further refined. In a subsequent analysis on 57 transplanted SSc patients from the EBMT/EULAR Registry, durable improvement in skin score was reported in two-thirds of the patients after HSCT, yet with a TRM of 8.7 % [23]. A long-term follow-up study of 26 transplanted SSc patients from the Netherlands and France showed sustained improvement of mRSS and stabilisation of organ function (heart, lung, kidney) up to 7 years after HSCT [24]. All patients were selected by using uniform eligibility criteria and a single transplantation protocol based on high-dose cyclophosphamide for mobilization and conditioning and CD34 selection of autologous grafts. No TBI or in vivo administration of lymphoablative antibodies was employed. After a median follow-up of 5.3 (1–7.5) years, 81 % (n = 21/26) of the patients demonstrated a clinically beneficial response. The Kaplan–Meier estimated survival at 5 years and 7 years were 96.2 and 84.8 %, respectively. Event-free survival, defined as survival without mortality, relapse or progression of SSc, resulting in major organ dysfunction, was 64.3 % at 5 years and 57.1 % at 7 years. A significant decrease in mRSS was observed in 73 % of the patients after 1 year and in 94 % after 5 years. In this study, 65 % of the patients with severe SSc had significant lung involvement at inclusion (defined as a vital capacity (VC)) or diffusion capacity of lung for carbon monoxide (DLCO) <70 %, or a mean pulmonary artery pressure (PAP) >40 mmHg on echocardiography. The median VC (% predicted) was 76 % at inclusion and 73 % after 5 years of follow-up. In comparison with baseline values for all patients, there was no significant change in forced expiratory volume in first second (FEV1) or DLCO during follow-up. The strongest effect of treatment by HSCT was observed on functional status, as assessed by the WHO performance status, which was possibly attributed to improvement of the skin condition. Five years after transplantation, the percentage of patients with a normal WHO status had increased to 56 % compared to 4 % at baseline.
More recently, the results from a single-center study in Germany of autologous HSCT in a cohort of 26 SSc patients (2 with lcSSc and 24 with dcSSc) who received the transplant as a rescue therapy were published [25•]. Patients were eligible for HSCT if they had an inadequate response to cyclophosphamide or rapidly progressive diffuse disease with strong indicators for a bad prognosis. The main exclusion criteria were a Karnofsky index <70 %, pulmonary arterial hypertension with systolic pulmonary arterial pressure >50 mm Hg, and DLCO <40 %. The transplant regimen consisted of mobilization with cyclophosphamide (2 × 2 g/m2) and granulocyte colony-stimulating factor (G-CSF: 10 μg/kg/day) followed by leukapheresis and CD34 selection of the stem cell harvest 10 days after mobilization therapy. Conditioning was performed with cyclophosphamide (4 × 50 mg/kg body weight) plus rabbit ATG (rbATG 4 × 10 mg/kg). The primary endpoint was response to treatment at 6 months defined as 25 % improvement in the mRSS. Twenty-three patients completed the HSCT of whom 18 (78.3 %) patients had improvement of >25 % in the mRSS at 6 months. The change in DLCO was minimal but the mean inspiratory vital capacity improved significantly: 66.0 % at 6 months and 76.1 % at 12 months. TRM was 11 %. Seven patients experienced a relapse during 4.4 years of follow-up.
The results of a retrospective analysis of a cohort of dcSSc patients treated with autologous HSCT in the US and Brazil, either as part of a study or on a compassionate basis, have also been published recently [26•]. Unselected peripheral blood stem cells were harvested with cyclophosphamide (2 g/m2) and filgrastim (G-CSF). The transplant regimen was a non-myeloablative regimen of cyclophosphamide (200 mg/kg) and rbATG (4·5–6·5 mg/kg). Patients were followed up to 5 years for overall survival, relapse-free survival, mRSS, and pulmonary function tests. Sustained improvement in skin thickness and forced vital capacity (FVC) were observed. Total lung capacity (TLC) and DLCO were not improved significantly. However, overall mean DLCO was significantly improved in patients with normal baseline echocardiograms or electrocardiographs. TRM was 6 % which was predominantly related to cardiac events. The investigators pointed at the benefit of extensive cardiac screening at baseline and provided data suggesting that pretransplantation cardiac structure, function, and electrophysiology affect DLCO after transplantation.
Autologous HSCT in SSc: Randomized Clinical Trials
Since 2001, the efficacy, safety and long-term (side) effects of autologous HSCT in SSc have been studied in one phase II and two phase III randomized control trials in Europe and North America.
ASSIST Trial
The American Scleroderma Stem Cell versus Immune Suppression Trial (ASSIST) was a North American phase II trial to assess the efficacy and safety of autologous non-myeloablative HSCT versus monthly pulse intravenous (IV) cyclophosphamide in patients with SSc [27•]. The study was stopped early for benefit. Over a period of 46 months, 45 patients with SSc were screened against the trial eligibility criteria and 19 patients were enrolled. The main inclusion criteria were dcSSc, age (<60 years), mRSS >14 and internal organ involvement or mRSS <14 plus pulmonary involvement. The main exclusion criteria were TLC < 45 % of predicted value, left ventricular ejection fraction (LVEF) <40 %, symptomatic cardiac disease, serum creatinine >177 μmol/L, 6 previous IV cyclophosphamide pulses and disease duration >4 years. Ten patients were randomised to receive HSCT while 9 patients received 6 monthly pulses of cyclophosphamide (Table 1). Patients in the control group were allowed to switch to HSCT 12 months after enrolment if they had experienced >25 % increase in mRSS or a decrease >10 % in FVC. All ten patients who were randomly allocated to receive HSCT improved within the first 12 months compared with none of nine controls (odds ratio 100, 95 % CI 14.04–∞; p = 0.0001). On the other hand, treatment failure (disease progression without interval improvement) occurred in eight of nine controls compared with none of ten patients treated by HSCT (p = 0.0001). One year after start of treatment, the mean mRSS decreased in the transplant group and increased in the control group, respectively. Over the same period, mean predicted FVC and TLC increased in the HSCT group but decreased in the cyclophosphamide group. DLCO did not differ between two groups. One year after start of treatment, high-resolution chest CT volumetric measurement of interstitial lung disease decreased after HSCT but increased in controls. After long-term follow-up (mean 2.6 years), eight of ten patients who were randomly allocated to receive HSCT had sustained improvement in mRSS and FVC. At 1 year after start of treatment, the total 36-item Short Form general health survey (SF-36) score improved from 39 to 56 in the transplant group (p = 0.004) but declined from 50 to 40 in the control group (p = 0.04). Seven of nine patients randomly allocated to receive cyclophosphamide underwent HSCT at a mean of 14 months after enrolment and all of them subsequently improved. No deaths were recorded in the ASSIST trial as of 2011.
The results of the ASSIST I trial formed the basis for the development of the ASSIST II trial, a North American phase 3 trial which started in 2011 with the aim of comparing the ASSIST trial conditioning regimen of cyclophosphamide and rbATG to the same regimen (rbATG, cyclophosphamide) with rituximab (termed rituximab sandwich regimen) [28]. The authors postulate that the latter regimen will improve response rate and duration in patients receiving autologous HSCT.
ASTIS Trial
The Autologous Stem cell Transplantation International Scleroderma trial (ASTIS) was the first phase III trial to be launched in the field. From 2001 to 2009, 156 patients were recruited in 28 centers in Europe and one in Canada [29]. Seventy nine and 77 patients were randomized into high-dose immunoablation followed by HSCT and 12 monthly pulses of IV cyclophosphamide respectively (Table 1) [30, 31]. The primary endpoint of the ASTIS trial was event-free survival, defined as the time in days from the day of randomization until the occurrence of death due to any cause or the development of persistent major organ failure (heart, lung, kidney). The results of the ASTIS trial demonstrated a better event-free survival and overall survival in the HSCT group (time-varying hazard ratios; p = 0.002). As of March 2012, 40 deaths had been recorded: 16 in the transplant group, 24 in the control group. Eight deaths (10 %) in the transplant group were deemed treatment-related by the independent data monitoring committee. In the control group, none died from treatment-related causes and most deaths were due to progressive disease. Two additional patients in the transplant arm developed irreversible major organ failure (renal), while one additional patient in the control group became oxygen dependent.
SCOT Trial
The ‘Scleroderma: Cyclophosphamide Or Transplantation’ (SCOT) trial is a North American randomized, controlled phase III trial which was designed to compare high-dose immunosuppressive therapy and hematopoietic cell transplantation to monthly pulse cyclophosphamide. Recruitment started in 2005 and was completed in 2011 [32]. The SCOT shares similar endpoints and control treatment with the ASTIS trial and this may allow a future inter-trial comparison. However, the transplant protocol in the SCOT trial differs from both the ASTIS and ASSIST trials because of its use of TBI and equine anti-thymocyte globulin as part of conditioning (Table 1). To reduce the risk of treatment-related complications, notably potential pulmonary and renal toxicities from TBI, bilateral lung and kidney shielding were employed [33•]. The SCOT trial’s primary endpoint is the Global Rank Composite Score (GRCS) at 54 months post- randomization. The GRCS reflects each subject's "order" relative to every other subject based on the following hierarchy of component outcomes: death, event-free survival, FVC, modified Scleroderma Health Assessment Questionnaire (SHAQ), and mRSS.
Conclusions
Autologous HSCT in severe SSc has resulted in rapid and sustained improvement of skin thickening and functional ability, stabilization of major organ function with possible improvement of VC and lung disease on High Resolution Computed Tomography (HRCT). Long-term survival and functional ability have also significantly improved with HSCT. Treatment-related mortality varied between different studies but was 10 % in the prospective phase III ASTIS trial where each fatality was carefully subjected to independent review. TRM so far has been difficult to predict in individual SSc patients who as a group seem prone to develop cardiorespiratory complications, especially during the conditioning step of HSCT. This may be related to cardiotoxicity from high-dose cyclophosphamide, capillary leak syndrome from ATG, in patients at risk because of compromised cardiopulmonary function. A recent study suggested that fluid challenge during right heart catheterization may help identify at-risk patients [26•]. HSCT is associated with potential long-term complications such as infertility, secondary AD, and secondary malignancy, so long-term, structured follow-up is essential [34, 35•]. Moreover, HSCT is an expensive treatment. Risk factors such as smoking may also play an important role in the outcome of HSCT in SSc and need to be considered as part of the future selection criteria [36]. So far, the ASSIST trial is the only randomized, controlled trial that has been published. This trial was stopped early for benefit, which carries the risk that its treatment effects are overestimated [37, 38].
The results of the ASTIS trial are awaiting publication while the SCOT trial is ongoing. The long-term follow-up data from these two prospective, controlled trials will help optimize patient selection and transplant protocols. Further prospective, controlled studies are needed to evaluate the importance of CD34 selection, the need for immunosuppressive maintenance treatment post-HSCT, and last but not least, the best timing of HSCT in the treatment of SSc patients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Varga J, Abraham D. Systemic sclerosis: a prototype multisystem fibrotic disorder. J Clin Invest. 2007;117:557–67.
Ferri C, Valentini G, Cozzi F, et al. Systemic sclerosis: demographic, clinical, and serologic features and survival in 1012 Italian patients. Medicine. 2002;81:139–53.
Tyndall AJ, Bannert B. Causes and risk factors for death in systemic sclerosis: a study from the EULAR Scleroderma Trials and Research (EUSTAR) database. Ann Rheum Dis. 2010;69:1809–15.
Nihtyanova SI, Tang SI, Coghlan JG, Wells AU, Black CM, Denton CP. Improved survival in systemic sclerosis is associated with better ascertainment of internal organ disease: a retrospective cohort study. QJM. 2010;103:109–15.
Tashkin DP, Elashoff R, Clements PJ, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354:2655–66.
Elhai M, Meunier M, Matucci-Cerinic M, et al. on behalf of EUSTAR (EULAR Scleroderma Trials and Research group): Outcomes of patients with systemic sclerosis-associated polyarthritis and myopathy treated with tocilizumab or abatacept: a EUSTAR observational study. Ann Rheum Dis. 2012. [Epub ahead of print].
EU Clinical Trials Register: A phase II/III, multicenter, randomized, double blind, placebo-controlled study to assess the efficacy and safety of tocilizumab versus placebo in patients with systemic sclerosis. Available at https://www.clinicaltrialsregister.eu/ctrsearch/search?query=systemic+sclerosis+and+tocilizumab. Accessed January 2013.
van Laar JM. B-cell depletion with rituximab: a promising treatment for diffuse cutaneous systemic sclerosis. Arthritis Res Ther. 2010;12:112–6.
Phumethum V, Jamal S, Johnson SR. Biologic therapy for systemic sclerosis: a systematic review. J Rheumatol. 2011;38:289–96.
Marmont A, Tyndall A, Gratwohl A, Vischer T. Hematopoietic precursor-cell transplants for autoimmune-diseases. Lancet. 1995;345:978.
van Laar JM, Tyndall A. Intense immunosuppression and stem-cell transplantation for patients with severe rheumatic autoimmune disease: a review. Cancer Control. 2003;10:57–65.
Burt RK, Milanetti F. Hematopoietic stem cell transplantation for systemic sclerosis: history and current status. Curr Opin Rheumatol. 2011;23:519–29.
Hügle T, van Laar JM. Stem cell transplantation for rheumatic autoimmune diseases. Arthritis Res Ther. 2008;10:217.
The European Group for Blood and Marrow transplantation: EBMT activity survey 2010. Available at http://www.ebmt.org/Contents/Research/TransplantActivitySurvey/Results/Documents/Survey_2010_website_set_Final_Nov2011%20(1).pdf. Accessed January 2013.
Hügle T, van Laar JM. Allogeneic stem cell transplantation for rheumatic autoimmune diseases. F1000 Med Rep. 2010;2:22.
Cipriani P, Carubbi F, Liakouli V, et al. Stem cells in autoimmune diseases: implications for pathogenesis and future trends in therapy. Autoimmun Rev. 2012. doi:10.1016/j.autrev.2012.10.004 [Epub ahead of print].
Tyndall A, Saccardi R. Haematopoietic stem cell transplantation in the treatment of severe autoimmune disease: results from phase I/II studies, prospective randomized trials and future directions. Clin Exp Immunol. 2005;141:1–9.
Fleming JN, Nash RA, McLeod DO, et al. Capillary regeneration in scleroderma: stem cell therapy reverses phenotype? PLoS One. 2008;3:e1452.
Snowden JA, Saccardi R, Allez M, et al. Haematopoietic stem cell transplantation in severe autoimmune diseases: updated guidelines of the European Group for Blood and Bone Marrow Transplantation. Bone Marrow Transpl. 2012;47:770–90.
Binks M, Passweg JR, Furst D, et al. Phase I/II trial of autologous stem cell transplantation in systemic sclerosis: procedure related mortality and impact on skin disease. Ann Rheum Dis. 2001;60:577–84.
McSweeney PA, Nash RA, Sullivan KM, et al. High-dose immunosuppressive therapy for severe systemic sclerosis: initial outcomes. Blood. 2002;100:1602–10.
Farge D, Marolleau JP, Zohar S, et al. Autologous bone marrow transplantation in the treatment of refractory systemic sclerosis: early results from a French multicentre phase I–II study. Br J Haematol. 2002;119:726–39.
Farge D, Passweg J, van Laar JM, et al. Autologous stem cell transplantation in the treatment of systemic sclerosis: report from the EBMT/EULAR Registry. Ann Rheum Dis. 2004;63:974–81.
Vonk MC, Marjanovic Z, van den Hoogen FH, et al. Longterm follow-up results after autologous haematopoietic stem cell transplantation for severe systemic sclerosis. Ann Rheum Dis. 2008;67:98–104.
• Henes JC, Schmalzing M, Vogel W, et al. Optimization of autologous stem cell transplantation for systemic sclerosis - a single-center longterm experience in 26 patients with severe organ manifestations. J Rheumatol. 2012;39:269–75. Single center, long-term follow-up study in 26 transplanted SSc patients.
• Burt RK, Oliveira MC, Shah SJ, et al. Cardiac involvement and treatment-related mortality after non-myeloablative haemopoietic stem-cell transplantation with unselected autologous peripheral blood for patients with systemic sclerosis: a retrospective analysis. Lancet. 2013. doi:10.1016/S01406736(12)62114-X. [Epub ahead of print]. Retrospective analysis of 2 cohorts of SSc patients treated with the same transplant regimen making the case for fluid challenge during right heart catheterization as a means to optimize patient selection.
• Burt RK, Shah SJ, Dill K, et al. Autologous non-myeloablative haemopoietic stem-cell transplantation compared with pulse cyclophosphamide once per month for systemic sclerosis (ASSIST): an open-label, randomised phase 2 trial. Lancet. 2011;378:498–506. Small, randomized, controlled trial showing superior efficacy on skin thickening and lung function of HSCT when compared to a short course of intravenous pulse cyclophosphamide.
ClinicalTrials.gov: Autologous stem cell systemic sclerosis immune suppression trial (DISclRituxan). Available at http://www.clinicaltrials.gov/ct2/show/record/NCT01445821?term=ASSIST+Trial+systemic+sclerosis&rank=1. Accessed January 2013.
van Laar JM, Farge D, Tyndall A. Stem cell transplantation: a treatment option for severe systemic sclerosis? Ann Rheum Dis. 2008;67 Suppl 3:iii35–8.
van Laar JM, Farge D, Sont JK, et al. The ASTIS trial: autologous stem cell transplantation versus IV pulse cyclophosphamide in poor prognosis systemic sclerosis, first results. EULAR, Annual Congress of the European League Against Rheumatism. Ann Rheum Dis. 2012;71 suppl 3:151.
Farge D, van Laar JM, Sont JK, et al. Autologous hematopoietic stem cell transplantation versus intravenous pulse therapy cyclophosphamide for severe or rapidly progressive systemic sclerosis, the ASTIS Trial. Blood (ASH Ann Meet Abstr). 2012;120:964.
ClinicalTrials.gov: Scleroderma: Cyclophosphamide or Transplantation (SCOT). Available at http://www.clinicaltrials.gov/ct2/show/NCT00114530?term=SCOT+trial&rank=6. Accessed January 2013.
• Craciunescu OI, Steffey BA, Kelsey CR, et al. Renal shielding and dosimetry for patients with severe systemic sclerosis receiving immunoablation with total body irradiation in the scleroderma: cyclophosphamide or transplantation trial. Int J Radiat Oncol Biol Phys. 2011;79:1248–55. Detailed study discussing the rationale and practicalities of renal shielding and dosimetry related to total body irradiation as used in the SCOT trial.
Daikeler T, Tichelli A, Passweg J. Complications of autologous hematopoietic stem cell transplantation for patients with autoimmune diseases. Pediatr Res. 2012;71:439–44.
• Daikeler T, Labopin M, Di Gioia M, et al. Secondary autoimmune diseases occurring after HSCT for an autoimmune disease: a retrospective study of the EBMT Autoimmune Disease Working Party. Blood. 2011;118:1693–8. Comprehensive retrospective analysis of secondary autoimmune diseases in patients transplanted for primary autoimmune diseases including systemic sclerosis.
Chang G, Orav EJ, McNamara T, et al. Depression, cigarette smoking, and hematopoietic stem cell transplantation outcome. Cancer. 2004;101:782–9.
Montori VM, Devereaux PJ, Adhikari NKJ, et al. Randomized trials stopped early for benefit. A systematic review. JAMA. 2005;294:2203–9.
Tyndall A. Stem cells: HSCT for systemic sclerosis–swallows and summers. Nat Rev Rheumatol. 2011;7:624–6.
Conflict of Interest
Kamran Naraghi declares no conflict of interest.
Jacob M. van Laar has received speakers’ fees/honoraria from Roche, Genentech, Pfizer, Abbott Laboratories, Menarini, Bristol-Myers Squibb, and Miltenyi-Biotec; has received grant support from Amgen, Roche, Genentech, and Trubion; has served as a consultant for Roche UK; has received payment for development of educational presentations from Tonic and Benecke; has had travel/accommodations expenses covered/reimbursed by Roche, Genentech, Pfizer, Abbott Laboratories, Menarini, Bristol-Myers Squibb, and Miltenyi-Biotec; and received discounts on CliniMACS columns for the ASTIS trial.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Scleroderma
Rights and permissions
About this article
Cite this article
Naraghi, K., van Laar, J.M. Update on Stem Cell Transplantation for Systemic Sclerosis: Recent Trial Results. Curr Rheumatol Rep 15, 326 (2013). https://doi.org/10.1007/s11926-013-0326-2
Published:
DOI: https://doi.org/10.1007/s11926-013-0326-2