Abstract
Psoriatic arthritis is associated with a broad range of problems from the perspective of the patient. These include symptoms relating to skin and musculoskeletal disease to difficulties with day-to-day activities, social interactions, paid employment, and community participation. Additional problems related to frequent comorbidities impose further impact. It has been shown that individuals with psoriatic arthritis have similar or worse disability than men older than 75 years of age in the general population, and psoriatic arthritis confers worse health status than many other common chronic diseases. The World Health Organization International Classification of Functioning, Disability, and Health provides a useful framework for considering the impact of this disease. Ideal clinical management of psoriatic arthritis would provide access to an interdisciplinary team with expertise in functional, social, vocational, and community issues, as well as to medical expertise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psoriatic arthritis (PsA) is an immune-mediated disease characterized by an inflammatory skin and nail disease or family history of psoriasis in association with a pluralistic inflammatory musculoskeletal disease that can involve entheses, the spine, and peripheral joints. Until fairly recently, PsA was considered to be a less severe disease than other kinds of inflammatory arthritis, especially rheumatoid arthritis, as the condition often affects fewer joints than other diseases and was thought to lead less often to destructive disease. It has become clearer that such notions are incorrect and that PsA leads to significant joint damage and disability, impaired quality of life, and cardiovascular disease. It is not surprising that a condition with such diverse manifestations and high burden of symptoms can lead to significantly impaired quality of life. This review article aims to summarize the published literature concerning the myriad ways in which PsA impacts the lives of individuals with this condition.
The term impact, in the context of the effects of disease burden, is relatively ill-defined, although it has an immediate common use meaning as the totality of the patient experience due to the disease. Recently, Sanderson and Kirwan [1] proposed that “personal impact” represents a critically important approach to understanding the patient’s perspective, to the extent of suggesting that the patient-reported outcomes be replaced by measures that more truly capture the patient perspective: personal life impact measures [1]. This emphasizes not only the extent or nature of the consequences of disease, but also the personal importance attached to those consequences. This is a useful way to think about the consequences of disease, and has long been echoed in the literature concerning quality of life.
The impact of a disease could also be understood from a societal perspective in terms of resources required to treat the disease effectively and the costs of illness, which include not only treatment costs but also costs due to lost productivity and disability pensions. However, this review is only concerned with the impact of PsA from the patient’s personal perspective.
From a methodologic standpoint, it can be difficult to tease out whether problems that are reported by patients are necessarily important to them. In qualitative studies, in which participants are free to talk about anything they like, it is usually implicit that any problems or issues raised by participants are important to them (otherwise, why would they be mentioned?), whereas in survey studies that use standardized questionnaires, items that are not important may still be rated as problematic because participants are constrained to answer only the questions that are asked (and to answer every one, irrespective of the importance of the question to the individual). Only from those questionnaires that ask about the importance of an area of difficulty, not only the extent of that difficulty, can the impact of the disease be best appreciated. However, even then, the relative importance of life areas can change over time or in response to adaptation, so disease can still have a significant impact on a particular life area without it currently being reported as important. Understanding the longitudinal impact of disease is an area of study that is very challenging, particularly because nearly all published studies in PsA are cross-sectional in nature.
This paper discusses how PsA affects the lives of patients with this disease and partly draws upon the framework of the International Classification of Functioning, Health, and Disability (ICF) of the World Health Organization to organize the different ways we can consider the impact of this disease, but also reviews the extent to which the importance of those consequences has been investigated in patients with PsA.
The World Health Organization International Classification of Functioning, Disability, and Health
Briefly, the ICF (Fig. 1) conceives the impact of disease to be expressed as a disturbance of “functioning” [2]. Functioning is considered at three levels: the organ level (body structures or physiologic functions [eg, joint range of motion]), the whole-person level (limitations in activities [eg, dressing]) and societal level (restrictions in community participation [eg, employment]). In addition, the ICF model considers that the functional expression of disease is modified not only by the disease, but by personal factors (including age, gender, and other personal factors [eg, psychological attributes]) and by environmental context (eg, health care system, access to effective treatment, societal attitudes). Such a model offers a helpful way to consider how PsA affects the individual, although it is also necessary to consider other concepts, such as quality of life and ability to cope or successfully self-manage. As body structures and functions are generally considered as pathological manifestations of the disease, this review focuses more on how PsA leads to activity limitations and participation restrictions.
In addition to the model, the ICF also refers to a taxonomy of individual categories of how life can be affected by health. Each of the ICF components (except “personal factors”) has been carefully categorized into approximately 1,400 particular items (eg, d4751 is the category of “driving a car”).
Activity Limitations
The musculoskeletal component of PsA has a major functional expression as difficulties in day-to-day activities. The range of such problems experienced by people with PsA was elicited in a study across North America, the United Kingdom, and Australasia, with direct reference to categories of the ICF [3]. This showed that a large number of categories of the activities and participation component were rated as being affected. About half (53 %) of the categories that were assessed were considered to be affected in at least 30 % of the participants in this study, which compares with 33 % of assessed categories in a study of patients with rheumatoid arthritis and 45 % in a study of patients with ankylosing spondylitis. Such findings support other data that suggest PsA is at least as disabling as other inflammatory rheumatic diseases.
Using the physical functioning subscale of the Medical Outcomes Survey Short Form 36 (SF-36), it has been shown that patients with PsA have considerably worse physical functioning than the general population. For example, in Hong Kong, the average Physical Functioning subscale score was 65.54 for patients with PsA, compared to 91.83 for the general population (P < 0.001) [4]. In this study, the Physical Component score (mainly, a weighted aggregation of the Physical Functioning, Role Physical, Bodily Pain, and General Health subscales) was only 62 % of the general population average, whereas the Mental Health Component score was 90 % of the general population average. This level of physical health is worse than the average reported for a US population with chronic allergies, anemia, back pain, cancer, depression, dermatitis, diabetes, hearing impairment, heart disease, hypertension, kidney disease, liver disease, lung disease, osteoarthritis, rheumatoid arthritis, ulcer, vision impairment, and the general population older than 75 years of age [5].
Qualitative research also confirms that PsA is associated with problems in day-to-day activities that range from basic movements and skills to more complex activities such as driving and sports [6]. In this study, it was also determined that no single standardized questionnaire covered every area of difficulty, but that each area was covered by part of at least one or several other questionnaires. Such a finding supports the need for a specific instrument designed for PsA that will have sufficient breadth to properly represent the disability associated with this disease.
Participation Restrictions
Possibly some of the most devastating effects of psoriasis are in the domains of social relationships, intimacy, and community participation. A common theme from studies that ask patients with psoriasis about what it is like to live with this condition is the social embarrassment and perceived stigmatization associated with scaling and appearance of the skin lesions. For example, in a qualitative study that asked people with psoriasis about how their condition affected their life, a patient said the following:
“The worst thing is that I cannot walk on a beach in the summer. I like very much to swim and I need to sunbathe, but others look at me there so I do not do that. But there are special beaches where I can be by myself. During the summer, there are other situations when it is not that fun as well. Mostly I cannot wear short-sleeved shirts. It is very ugly and there are scales falling everywhere … In addition, it is hard not being able to wear a short skirt or trousers. I cannot show myself because I usually have a lot of rashes in the spring” [7].
Such feelings of “being marked and discredited” [7] lead to high rates of depression, anxiety, impaired interpersonal relationships, and lack of confidence [8]. Thoughts of suicide occur in 5.5 % of patients with psoriasis [9], compared with a rate of 0.12 % of attempted or successful suicide in the United States (Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System [WISQARS]: [http;//www.cdc.gov/ncipc/wisqars]).
In comparison with some other diseases, psoriasis confers a greater impact on well-being. A novel approach asked patients with severe psoriasis with and without other diseases (diabetes, asthma, chronic bronchitis) which condition they would rather have [10]. About twice as many patients with a comorbid condition than those without the comorbid condition indicated that they would rather have the comorbidity than have psoriasis. In comparison with respondents to the National Survey of Functional Health Status, patients with psoriasis report worse physical health status (Physical Component score of the SF-36) than patients with arthritis, cancer, chronic lung disease, hypertension, myocardial infarction, diabetes, and depression (psoriasis ranking 10th out of 11 health conditions). Moreover, patients with psoriasis report worse mental health than all examined health conditions except depression (again ranking 10th out of 11 health conditions).
It is reasonably clear that the severity of the cutaneous disease is associated with worse mental health in patients with psoriasis alone and those with PsA [11].
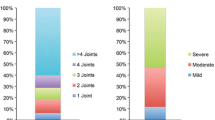
People with PsA report high rates of difficulties with paid employment. In a Norwegian study, work disability (defined as having received a national work disability pension awarded to people who are unable to work full-time because of their health) was observed in 33 % of women and 17 % of men 18 to 45 years of age [12••]. In a multivariate analysis from this study, less education, longer disease duration, having erosive disease, greater physical disability measured by modified Health Assessment Questionnaire, and being female were independently associated with work disability. The strongest associations with work disability were with education level and physical disability.
Contextual Factors
The ICF model specifies that the functional impact of a health condition is modified by the context of the environment (external factors) and by the context of the individual (internal factors). A nice example of this is provided by the previously mentioned study of work disability in PsA patients living in Norway, in which education level (a personal factor) was found to have as strong an association with work disability as having erosive disease (a direct indicator of the severity of the disease). In general, there is a large body of literature concerning the influence of psychological factors on the lived experience of other diseases that includes concepts such as coping, optimism, self-efficacy, anxiety, locus of control, and many others. However, such factors have scarcely been examined in PsA, and the subject provides an area ripe for inquiry.
Personal factors have not yet been categorized within the ICF, although environmental factors have, and these have been examined in relation to their relevance for people with PsA in two studies. Both studies confirmed that the attitudes of family, friends, and health professionals are important to people with PsA [3, 6]. Other relevant environmental factors that can modify the impact of the disease are medical treatment (especially drug therapy), climate, assistive devices, and the built environment. Such environmental factors are infrequently represented in self-report questionnaires but might add useful information to the interpretation of patient-reported outcomes.
Quality of Life
Given the clear detrimental effects on quality of life in people with psoriasis alone, it is of interest to know whether the additional burden of musculoskeletal disease for people with PsA contributes to additional loss in life quality. The available information is somewhat conflicting but overall favors the notion that PsA is associated with worse health-related quality of life (HRQoL) compared with psoriasis alone. An analysis of data collected during the 2005 Spring US National Psoriasis Foundation survey found no differences in the Psoriasis Quality of Life 12 (PQOL-12) instrument between those with psoriasis alone and those with PsA but did observe that people with PsA were much more likely to report negative effects on employment (41 % vs 14 % of respondents; P < 0.001) [13]. The finding of no significant difference in PQOL-12 contrasts with that of other studies. For example, Lundberg et al. [14] found that patients with PsA had significantly worse SF-36 scores (all subscales) and worse Dermatology Life Quality Index (DLQI) scores than patients with psoriasis alone [14]. Another study of patients admitted for inpatient rehabilitation found a significant difference in physical functioning between those with and without arthritis using the SF-12, but no difference in mental health indices [15]. Furthermore, a large study of dermatology clinic patients with psoriasis, some of whom had PsA, found that the HRQoL measured with the EQ-5D was worse for PsA patients than for patients with just psoriasis after controlling for age and gender (EQ-5D scores, 0.56 vs 0.82; P < 0.0005). In addition, work problems were more common in PsA than in patients with just psoriasis [16•]. A likely explanation for the discrepant findings is that the PQOL-12 is too specific for skin disease and fails to represent the additional problems conferred by having arthritis. Generic HRQoL instruments such as SF-36 or EQ-5D are likely best to detect differences in HRQoL across different diseases.
One way to integrate the importance of an affected life area and the extent to which it is affected is to use a utilities approach. This involves asking a patient to quantify his or her current life situation by asking that patient to make choices, typically with standard gamble or willingness-to-pay methods. A study of patients with PsA elicited the dollar amount that they were willing to pay for cure from their disease with respect to each of eight domains [17•]. In this way, the relative importance of each domain could be assessed. The most important to least important life areas as judged by higher to lower amounts of money for cure were physical comfort, sleep, work (equally valued), self-care, concentration, intimacy, emotional health, and social comfort.
Comparison with Other Rheumatic Diseases
A number of studies have compared scores on generic health status or HRQoL measures in patients with PsA, rheumatoid arthritis, or ankylosing spondylitis. These are summarized in Table 1. In general, few differences in HRQoL are observed, yet patients with rheumatoid arthritis typically are found to have more destructive arthritis.
Comorbidities
The personal impact of PsA also includes comorbidities often associated with this disease. These include obesity, accelerated atherosclerosis leading to premature vascular disease, and depression. Recently, Husted and colleagues [18••] have shown that these and a number of other comorbidities are more common in patients with PsA than psoriasis, especially hypertension (present in 37 %), peptic ulcer disease or irritable bowel syndrome (7.2 %), neurologic disease (8.4 %), and autoimmune disease (9 %). These latter associations were present after adjustment for age, sex, severity of skin disease, smoking status, and use of specific drugs that could be associated with these diseases. The high prevalence of comorbidities in PsA is not altogether well-explained, but it certainly contributes to additional impact from the perspective of the patient and may contribute to the very poor HRQoL discussed earlier.
Conclusions
PsA is not a trivial disease and has significant impact on the well-being of patients that is at least as significant or more so than that observed in a number of other chronic diseases, including other kinds of inflammatory arthritis. The range of problems experienced by people with PsA is broad and includes basic day-to-day activities, work and leisure activities, and community participation roles. However, there are several gaps in the literature concerning the impact of PsA. In particular, the role of personal factors in modifying the functional impact of the disease in patients with PsA is not at all studied. Also, the quantification of impact in terms of importance as well as degree to which particular life areas are affected is relatively less well-understood.
Given the broad range of physical, psychological, and social impacts that people with PsA face, there is a clear need for clinical management approaches that address these kinds of issues rather than an exclusive focus on medical treatment. Access to an interdisciplinary team of health professionals who have expertise in the medical, functional, vocational, social, and psychological aspects of the disease is an ideal to which health services should strive.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sanderson T, Kirwan J. Patient-reported outcomes for arthritis: time to focus on personal life impact measures? Arthritis Rheum. 2009;61(1):1–3.
World Health Organization. International classification of functioning, disability and health: ICF: WHO; 2001.
Taylor WJ, Gladman DD, Mease PJ, Adebajo A, Nash P, Feletar M. The impact of psoriatic arthritis (PsA) according to the International Classification of Functioning, Health and Disability (ICF). J Rheumatol. 2010;37:1885–91.
Leung YY, Ho KW, Zhu TY, Tam LS, Kun EW, Li EK. Testing scaling assumptions, reliability and validity of Medical Outcomes Study Short-Form 36 health survey in psoriatic arthritis. Rheumatology (Oxford). 2010;49(8):1495–501.
Ware JE, Kosinski M, Bjorner JB, Turner, Bowker DM, Gandek B, et al. User’s manual for the SF-36v2 Health Survey. 2nd edition ed. Lincoln, RI: QualityMetric Incorporated; 2007.
Stamm TA, Nell V, Mathis M, Coenen M, Aletaha D, Cieza A, et al. Concepts important to people with psoriatic arthritis are not adequately covered by standard measures of functioning. Arthritis Rheum (Arthritis Care Res). 2007;57(3):487–94.
Uttjek M, Nygren L, Stenberg B, Dufaker M. Marked by visibility of psoriasis in everyday life. Qual Health Res. 2007;17(3):364–72.
Feldman S, Behnam SM, Behnam SE, Koo JYM. Involving the patient: impact of inflammatory skin disease and patient-focused care. J Am Acad Dermatol. 2005;53:S78–85.
Gupta MA, Gupta AK. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol. 1998;139(5):846–50.
Finlay AY, Coles EC. The effect of severe psoriasis on the quality of life of 369 patients. Br J Dermatol. 1995;132:236–44.
Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcome. 2009;7:25.
•• Wallenius M, Skomsvoll JF, Koldingsnes W, Rodevand E, Mikkelsen K, Kaufmann C, et al. Work disability and health-related quality of life in males and females with psoriatic arthritis. Ann Rheum Dis. 2009;68:685–9. This was the first study to document the extent of work disability in people with PsA; it showed that a large percentage of people with PsA aged 18 to 45 years are work disabled. In this population, work disability was mainly associated with physical disability, level of education, and female sex.
Ciocon DH, Horn EJ, Kimball AB. Quality of life and treatment satisfaction among patients with psoriasis and psoriatic arthritis and patients with psoriasis only: results of the 2005 Spring US National Psoriasis Foundation Survey. Am J Clin Dermatol. 2008;9(2):111–7.
Lundberg L, Johannesson M, Silverdahl M, Hermansson C, Lindberg M. Health-related quality of life in patients with psoriasis and atopic dermatitis measured with SF-36, DLQI and a subjective measure of disease activity. Acta Derm Venereol. 2000;80(6):430–4.
Ruschenschmidt C, Somberg B, Haussler G, Lohmann J. Comparison of patients with psoriasis vulgaris vs. psoriatic arthritis with regard to the reported quality of life. Die Rehabilitation. 2008;47(6):343–9.
• Christophers E, Barker JN, Griffiths CE, Dauden E, Milligan G, Molta C, et al. The risk of psoriatic arthritis remains constant following initial diagnosis of psoriasis among patients seen in European dermatology clinics. J Eur Acad Dermatol Venereol: JEADV. 2010;24(5):548–54. This large study of patients attending dermatology outpatient clinics across Europe yielded a number of interesting findings. Of relevance to this review was the finding of considerably worse HRQoL in people with PsA compared with people with psoriasis alone.
• Hu SW, Holt EW, Husni ME, Qureshi AA. Willingness-to-pay stated preferences for 8 health-related quality-of-life domains in psoriatic arthritis: a pilot study. Sem Arthritis Rheum. 2010;39:384–97. This novel paper determined the relative importance of several domains of well-being for people with PsA using the econometric method of willingness-to-pay. In this group, the most significant area of life was physical comfort, whereas the least significant was self-care. This approach integrates the notion of degree of the problem with the notion of personal importance of the problem and is one of only a few studies to have addressed that concept.
•• Husted JA, Thavaneswaran A, Chandran V, Eder L, Rosen CF, Cook RJ, et al. Cardiovascular and other comorbidities in patients with psoriatic arthritis: a comparison with patients with psoriasis. Arthritis Care Res. 2011;63(12):1729–35. This study was the first to adequately compare comorbidities between psoriasis and PsA and extends the range of possible comorbidities associated with PsA considerably. Depression and hypertension were common, but this study also found autoimmune, gastrointestinal, and neurological disorders to be more common in PsA patients.
Borman P, Toy GC, Babaoglu S, Bodur H, Deniz C, Alli N. A comparative evaluation of quality of life and life satisfaction in patients with psoriatic and rheumatoid arthritis. Clin Rheumatol. 2007;26:330–4.
Zink A, Thiele K, Huscher D, Listing J, Sieper J, Krause A, et al. Healthcare and burden of disease in psoriatic arthritis. A comparison with rheumatoid arthritis and ankylosing spondylitis. J Rheumatol. 2006;33(1):86–90.
Husted JA, Gladman DD, Farewell VT, Cook RJ. Health-related quality of life of patients with psoriatic arthritis: a comparison with patients with rheumatoid arthritis. Arthritis Rheum. 2001;45(2):151–8.
Disclosure
Dr. Taylor has had travel expenses covered for travel to conferences by Abbott Laboratories and Schering-Plough.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taylor, W.J. Impact of Psoriatic Arthritis on the Patient: Through the Lens of the WHO International Classification of Functioning, Health, and Disability. Curr Rheumatol Rep 14, 369–374 (2012). https://doi.org/10.1007/s11926-012-0263-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-012-0263-5