Abstract
Purpose of Review
We identify the recent evidence for gene-by-environment interaction studies in relation to psychiatric disorders. We focus on the key genotypic data as well as environmental exposures and how they interact to predict psychiatric disorders and psychiatric symptomatology. We direct our focus on the psychiatric outcomes that were focused on by the Psychiatric Genetics Consortium.
Recent Findings
Many of the studies focus on candidate gene approaches, with most of the studies drawing upon previous literature to decide the genes of interest. Other studies used a genome-wide approach. While some studies demonstrated positive replication of previous findings, replication is still an issue within gene-by-environment interaction studies.
Summary
Gene-by-environment interaction research in psychiatry globally suggests some susceptibility to environmental exposures based on genotype; however, greater clarity is needed around the idea that genetic risk may not be disorder specific.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gene-by-environment interaction (GxE) in psychiatry was brought to the limelight with a key paper by Caspi and colleagues (2003), which focused on the interaction between a functional candidate gene polymorphism and stressful life events in depression [1]. Since that seminal paper, genetic epidemiology has evolved from the study of functional polymorphisms to the unbiased query of common and rare variation across the genome. This perspective has translated into broader approaches to characterize the “gene” part of gene-by-environment research. This might include investigating gene-environment interactions on a genome-wide scale in a genome-wide gene-environment interaction study (GE-WIS) [2]. Alternatively, existing genome-wide association studies (GWAS) results might be leveraged to create cumulative measures of common genomic burden via a polygenic risk score (PRS)—a summary measure where the number of risk alleles in a target dataset associated with a particular phenotype are summed across independent loci and weighted according to effect size [3]. The complexity of psychiatric disorders is such that the role of genetics is likely also complex and that multiple genetic pathways are generally involved. Further, alongside GxE, we also must consider gene environment correlation, which likely plays a role in psychiatric conditions [4]. The genetic focus of many GxE examinations varies widely based on the specific hypothesis the study is exploring, whether it be a candidate gene polymorphism or a genome-wide analysis. The environmental piece has remained somewhat more consistent across psychiatric conditions. Interaction with stressful life events has remained of interest with many researchers focusing their attention on understanding how stress or key events interact with genetics to increase risk for psychiatric conditions.
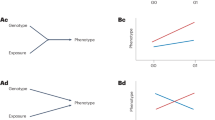
The two primary theoretical frameworks utilized in gene-by-environment interaction research are the stress-diathesis model and the differential susceptibility framework. The stress-diathesis model suggests that individuals are born genetically vulnerable to psychiatric disorders and that those disorders manifest only if an individual experiences some sort of stress in his or her environment [5]. The model posits that the vulnerability of an individual is static and that the severity of the stressor required to instigate the disorder is inversely proportional to the degree of vulnerability. In a similar vein, the differential susceptibility model extends the stress-diathesis model by suggesting that genetics may lead to heightened susceptibility to both negative and positive environments [6].
Like other gene-by-environment studies of complex diseases, those of psychiatric illness face numerous challenges. Common challenges include large samples required in gene-by-environment studies, and even larger sample size requirements in GWAS studies as a result of multiple comparisons; limited interpretations of variants in risk loci identified in GWAS studies; and exposure measurement across time and place [7]. In gene-by-environment studies in psychiatry, measurement of complex exposures, such as stress and adversity, deserves further comparison across studies.
While gene-by-environment research in psychiatry has come a long way, many questions remain unanswered. This review summarizes the last nearly given years of gene-by-environment interaction research, with a focus on major depressive disorder, anxiety disorder, schizophrenia, attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD), bipolar disorder, substance use disorder, and suicide.
Methods
This scoping review sought to rapidly identify key concepts and current evidence on gene-environment interactions in psychiatry. In keeping with the scoping review process [8], we defined a research question (What is known in the literature from the past five years about the role of gene-environment interactions in major depressive disorder, anxiety disorder, schizophrenia, attention deficit hyperactivity disorder, autism spectrum disorder, bipolar disorder, substance use disorder, and suicide?), identified and selected relevant studies, charted the data, and summarized the results. The mental disorders reviewed span common disorders and severe mental illness and were selected through a consensus process among authors.
A systematic search of the literature from January 1, 2014 through November 1, 2018 was carried out in PubMed separately for each mental disorder. Searches included gene-by-environment interaction terms: gene by environment interaction OR gene environment interaction OR gene X environment. Terms for mental disorders were major depressive disorder OR depression OR MDD, anxiety disorder OR anxiety, schizophrenia, attention deficit hyperactivity disorder OR attention deficit disorder OR ADHD, autism OR autism spectrum disorder OR ASD, bipolar disorder OR bipolar, substance use disorder AND alcohol use disorder OR drug use disorder, suicide OR suicidality OR suicidal. Records were screened and relevant records retained initially on the basis of their titles and then based on their abstracts and full-texts. After a full-text review, studies were included if they were original research (i.e., not a review) and utilized molecular genetics methodology (i.e., not twin studies). Information from the retained full texts was charted and summarized by mental disorder. Of particular interest for this review were the genetic data explored and the environmental exposure of interest.
Results
Searches resulted in 184 records for major depressive disorder (60 screened in), 173 records for anxiety disorder (31 screened in), 78 records for schizophrenia (11 screened in), 86 records for attention deficit hyperactivity disorder (35 screened in), 58 records for autism spectrum disorder (6 screened in), 36• records for bipolar disorder (9 screened in), 7 records for substance use disorders (4 screened in), and 11 records for suicide (4 screened in). Summaries of results for each mental disorder are described below.
Major Depressive Disorder
Major depressive disorder (MDD) is a mood disorder characterized by persistent feelings of sadness and loss of interest. Individuals also frequently report somatic symptoms, sleep problems, and difficulty concentrating. MDD was the focus of the seminal paper by Caspi and colleagues (2003) who demonstrated a significant gene-by-environment interaction, sparking further research on candidate genes and stressful life events in relation to MDD [1]. Results from this study showed that individuals carrying the short allele (either one or two copies) of the serotonin transporter gene had greater depressive symptoms and were more likely to have an MDD diagnosis when exposed to life stress as compared to individuals homozygous for the long allele. Researchers have focused on extending and replicating these findings, and in the last 4 years, this scoping review identified 56 studies that have studied gene-by-environment interactions with MDD.
A majority of the papers included in this review focused on the same environmental exposure as Caspi and colleagues (2003), with 21 papers focused on stressful life events or stress in general, and 17 focused on trauma exposure such as child maltreatment [1]. Other research (15 papers) has focused on other psychosocial factors such as familial support, parenting behaviors, and peer relationships. All of the studies identified in this scoping review focused on environmental exposures that have previously been associated with risk for MDD diagnosis or more severe depressive symptomatology.
Similarly, many of the studies included in this review focused on the same genetic exposure as Caspi and colleagues (2003), with 21 exploring serotonin related genes including the commonly studied serotonin transporter polymorphism [1]. Unlike many of the other psychiatric disorders explored, a greater percentage of the studies included in the review focused on polygenic approaches (8 studies) [9,10,11,12,13,14,15,16] and polygenic risk scores (3 studies) [17,18,19]. The other common candidate genes explored in these studies were the brain-derived neurotrophic factor (BDNF) gene, dopamine-related genes such as DRD4 and DAT1, and tryptophan hydroxylase 2 (TPH2) gene. Many of the included studies used the stress-diathesis model or the differential susceptibility framework. For example, Åslund and colleagues (2018) examined an interaction between the serotonin transporter polymorphism and the family environment (both positive and negative) [20]. Results did not strongly support the differential susceptibility hypothesis; the authors suggest that prior work with this gene that supports this hypothesis is due to measuring and controlling for positive environmental factors not often included in gene-by-environment interaction models. Conversely, Dalton and colleagues (2014) found support for the differential susceptibility framework such that particular plasticity gene genotypes were associated with more or less symptoms depending on positive or negative family environment [21]. Several meta-analyses have also been done related to the serotonin transporter polymorphism and stress. In one meta-analysis that included 14 studies, the interaction between the genetic polymorphism and stressful life events was non-significant [22]. A later meta-analysis, which included 54 studies, found a significant GxE effect [23].
Anxiety Disorders
This scoping reviewed covered social anxiety disorders, generalized anxiety disorder, and anxiety symptomatology described in 29 studies on gene-environment interactions and anxiety disorders published within the last 4.5 years. A vast majority of the studies focused on stressful life events [24,25,26,27, 28•, 29,30,31,32,33,34], childhood trauma [35, 36••, 37,38,39,40,41,42], and childhood adversity [43]. No studies explored environmental toxicants, but several focused on psychosocial factors such as parenting and family context [44,45,46,47,48, 49•, 50]. A majority of the studies found evidence for gene-by-environment interactions, particularly in relation to stressful life events, trauma exposure, and maltreatment. One study, however, presented a null finding. Musci and colleagues (2016) found no evidence of a significant gene-by-environment interaction with a polygenic score and life stress variable (death or divorce of a caregiver) [28••].
A vast majority of the included studies utilized a candidate gene approach, with no single gene or gene pathway identified as most important in terms of genes explored. The two most common genes included serotonin-related genes [25, 29, 36••, 37, 42, 49•, 51] and variants within the BDNF gene [24, 36•, 39, 44, 48, 52]. These particular genes have been linked to other psychiatric symptoms and disorders, including major depressive disorder and ADHD. Results from these studies suggest that individuals with genetic susceptibility are more likely to be impacted environmental exposures including stressful life events and childhood trauma. Only one study focused on testing a differential susceptibility approach, examining both positive and negative environmental exposures, and found significant support for the BDNF gene acting as a susceptibility gene such that exposure to positive environments was beneficial and exposure to negative environments was detrimental for a particular genotype [24].
Schizophrenia
Schizophrenia is considered a serious mental disorder, and prior research has demonstrated not only strong genetic underpinnings but significant gene-by-environment interplay [53]. In a review of the past 4.5 years of literature, we found 11 studies that explored gene-by-environment interactions. Many of the included studies focused on stressful life events [54, 55] and adversity [56,57,58]. Others focused on cannabis use [59, 60] and prenatal or perinatal exposures [61,62,63]. Many found significant main effects for these key environmental risk factors, wherein exposure to stressful life events significantly increase risk for first episode psychosis, auditory hallucinations, and diagnosis of schizophrenia.
Among the 11 studies reviewed, many took a genome-wide or polygenic approach. For example, French and colleagues (2015) used a polygenic risk score, created with SNPs that have enriched risk for schizophrenia in large genome-wide association studies [60]. This type of genetic risk score was also used in two of other studies [58, 61]. Other studies focused more on candidate gene or candidate pathway approaches [55,56,57, 59, 62, 64]. Other works by Condre and colleagues have explored the role of living in urban and populated areas in schizophrenia risk and how genetics may interact [65]. This work, however, is complicated because it explores both gene environment interaction and gene environment correlation, which certainly could be the focus of an entirely different review. While there has been some research demonstrating that significant gene-by-environment interactions increase the risk for schizophrenia, a majority of molecular genetics studies have indicated that polygenic approaches are likely the best methodological option for understanding how genetics may increase one’s susceptibility to environmental risk factors for schizophrenia.
Attention Deficit Hyperactivity Disorder
Attention deficit hyperactivity disorder (ADHD) is a psychiatric disorder characterized by persistent inattention, hyperactivity, and frequently high levels of impulsivity. A prior review of gene-by-environment interactions in relation to ADHD described how psychosocial factors are likely to interact with genotype to increase the risk for ADHD [66]. A review of the last 4.5 years of the literature included 34 studies that focused on ADHD diagnosis and related symptoms. A majority of studies focused their environmental exposure on related to psychosocial [67,68,69,70,71,72,73,74,75,76,77], stress and adversity [27, 75, 77,78,79,80,81,82,83,84], and trauma-related exposures [85]. Very few focused on toxicant exposure such as blood lead levels [86, 87••, 88], phthalate metabolites [89], and organophosphate pesticide exposure [90].
All of the included ADHD-related papers focused on candidate genes or candidate systems. For example, Tung and colleagues (2017) focused on SNPs within a number of dopaminergic genes [91]. A majority of the studies, however, included SNPs within the serotonin transporter gene as part of their gene-by-environment interaction [67, 68, 72,73,74, 76, 79,80,81,82, 84,85,86, 87•, 90, 92,93,94,95]. Like the previously discussed psychiatric disorders, it seems likely that multiple genetic pathways play a role in increasing risk and susceptibility for diagnosis or more severe symptoms. A majority of included studies found significant gene-by-environment interactions wherein individuals with a particular genotype was found to be more susceptible to environmental adversity of any sort such that exposure will lead to increased ADHD symptomatology.
Autism Spectrum Disorder
Autism spectrum disorder (ASD) is characterized by deficits in social interaction and communication, often accompanied by repetitive behaviors. The heritability of ASD is approximately 50%, with a sibling recurrence risk of over 18% (substantially greater than general population risk) [96, 97]. While genetic studies of ASD are numerous, there have been far fewer investigations in GxE effects. We found six studies that have jointly quantified the effects of genes and environment in ASD. Three have used copy number burden to summarize genetic risk, analyzed jointly with maternal infection during pregnancy, first trimester ultrasound, and air pollution exposure, respectively [98,99,100]. Two have evaluated specific functional polymorphisms with environmental factors: one carbon metabolism gene with prenatal vitamin use [101] and MET receptor tyrosine kinase gene variants with prenatal air pollution [102]. The most recent gene-environment (GxE) report examined maternal prenatal antidepressant use with likely gene disrupting (LGD) mutations (from Simons Simplex Collection (SSC) exome sequencing data) on ASD severity [103]. All of these found increased genetic risk among those with the prenatal risk factor [103].
Bipolar Disorder
Bipolar disorder is a psychiatric condition characterized by unusual shifts in mood. While many heritability studies utilizing twin samples have reported estimates well over 50%, the literature potentially suggests that gene-by-environmental interactions may underlie mechanisms through which individuals develop bipolar disorder. After a review of the literature, we found nine studies that explored gene-by-environment interactions predicting risk for bipolar disorder, psychosis, and age of onset of bipolar disorder. Similar to the review of gene-by-environment interactions in relation to anxiety-related outcomes, we found that a majority of the studies on bipolar disorder focused on environmental exposures of stressful life events [104,105,106] and trauma [107, 108•, 109]. Other exposures included psychosocial factors and birth complications [110], smoking [111], and infectious disease [106].
While a majority of the studies reviewed focused on candidate genes, several expanded their genetic variation of interest to include genome-wide associations [104] and genetic pathway analyses [108•]. Candidate genes explored include the catechol-O-methyltransferase (COMT) gene [105, 110] and the toll-like receptor 2 (TLR2) gene [106, 112] among others. A majority of these studies utilized a case-control design and the stress-diathesis framework to explore potential gene-by-environment interactions. No study included utilized or tested SNPs found to be significantly related to bipolar disorder in studies done by the Psychiatric Genetics Consortium.
Substance Use Disorder
Substance use disorders refer to recurrent use of alcohol or drugs that results in clinical and functional impairments, including impaired control, social impairment, risky use, and pharmacological metrics [113]. Common substance use disorders include alcohol, tobacco, cannabis, stimulant, hallucinogen, and opioid use disorders. Research has identified a generalized genetic vulnerability for substance use disorders (previously referred to as alcohol and drug dependence using DSM IV criteria) with heritability estimates of 30–60% in addition to evidence of contributing environmental factors [113]. Our review identified four studies exploring gene-environment interactions in the past 5 years. A study examining trauma exposure and dependence on alcohol, nicotine, cocaine, cannabis, and other illicit drugs using self-reported symptoms of alcohol and drug dependence according to DSM IV criteria found shared additive effects for both interpersonal trauma and drug dependence suggesting that common SNPs may underlie a genetic tendency toward both trauma and substance use disorders [113]. A shared genetic liability between first use of tobacco, alcohol, and cannabis and later substance use disorder was also identified in a twin study [114]. Gene-by-environment genome-wide interaction studies have identified S100A10 and S100B as significant risk loci for cannabis use and risky sexual behavior and LHPP as a risk locus for alcohol dependence and risky sexual behavior [115, 116]. The role of gender and ancestry in substance use and risky sexual behavior has also been explored, suggesting potentially different risk loci and mechanisms [115]. A previous systematic review that examined gene-by-environment interactions and substance use disorders found that studies on gene-by-environment interactions in alcohol use disorder largely examined genes thought to modulate functioning of the HPA axis and genes with a glucocorticoid response element in a promoter region, and relative to alcohol use, the authors noted a paucity of studies examining nicotine, cannabis, and opioid use disorders [117]. This systematic review found a number of environmental factors and community characteristics that were associated with the influence of genetics on alcohol use (i.e., urban, higher levels of migration, higher proportion of older adolescents and young adults).
Suicide
Suicidal ideation refers to thoughts or plans to end one’s own life. Suicidal behavior refers to self-injurious behavior, including suicide attempts. This review identified four studies exploring gene-environment interactions in relation to suicide over the past 5 years. Findings from a Danish sample of adoptees and their siblings found that the rate of suicidal behavior was three times higher among biological siblings of adoptee suicide attempters relative to siblings of adoptees who had not attempted suicide [118]. These findings and other similar findings point to a genetic basis for suicidal behavior. Early life adversity may increase the risk of suicide through epigenetic modulation of HPA axis functioning [119, 120]. The interaction between genes SKA2, cRHBP, FKBP5, and childhood trauma, such as child abuse, has been identified as a potential predictor of suicidal behavior later in life. Though, replication of these gene-by-environment interacts have been limited. Similar to findings from the literature on gene-environment interactions and depression, gene polymorphisms associated with serotonergic functioning, such as 5-HTTLPR, may serve as effect measure modifiers of the association between early childhood adversity and suicidal behavior [119, 121]. Preliminary evidence from another study among an inpatient sample of adolescents has shown that DRD4L, a genetic polymorphism associated with the dopaminergic system, may moderate the association between experiences of sexual trauma and suicidal ideation and behavior [122]. Using a stress-diathesis framework, a review by Brodsky and colleagues described how early life events and suicidal behavior are thought to be mediated by genetic risk [119]. The updated framework presented points to the potential role of epigenetics where early childhood adversity may inform genetic polymorphisms that modify neurological expression, impacting trait development and increasing the diathesis for suicide risk.
Conclusions
This scoping review charted the current state of the science in relation to gene-by-environment interactions in psychiatry research. This field of research has been underway for almost two decades and many questions remain. Nonetheless, the set of studies presented here suggest that there is evidence that genetics interact with environments and that this interaction plays a role in the diagnosis and (perhaps less so) severity of many psychiatric disorders. Through this scoping review, we have identified a few areas that warrant attention in future gene-by-environment interaction studies.
The first area is one closely related to gene-by-environment interaction analyses, and that is gene environment correlation (rGE). Gene environment correlation occurs when an individual’s genetic makeup influences (or is correlated with) a particular environmental exposure. In this area, researchers focus on passive, evocative, and active correlation, but many studies included in our scoping review did not explicitly test or control for rGE. This is clearly a gap in the area of gene-by-environment interaction research in psychiatry and should be explored further.
The most common environmental exposure explored in the included studies was stressful life events, or factors related to adversity. While intuitively we know that exposure to stressful life events increases risk for psychiatric disorders in general, more research is needed to explore risk and resilience in relation to this exposure to stressful life events. What makes an individual more susceptible to the influence of a particular environment could be a result of genetic effects or candidate genes. There are, however, other contextual factors that could play an important role in gene-by-environment interaction studies and therefore researchers may want to expand their list of environmental factors beyond those most commonly explored in the field.
A majority of the studies explored in this scoping review focused entirely on candidate gene polymorphisms. Early molecular genetics research was focused on single-gene-phenotype associations under the one-gene one-disease model. This approach was successful at identifying genetic liability for single-gene disorders governed by Mendelian inheritance. However, many would argue that psychiatric disorders, in particular, are more complex with multiple genes underlying them. While single-gene—candidate—approaches can be useful for identifying probable mechanisms, researchers also must consider the various benefits of polygenic approaches. In general, the field of molecular genetics has moved past simple candidate gene studies, but we as researchers would be remiss to completely discount the findings. Instead, the field of research should focus on strengthening methodology and emphasizing replication of findings.
The GWAS results from the Psychiatric Genetics Consortium (PGC) represent one potential source for future research using a polygenic approach. The PGC, led by top psychiatric genetics researchers, have completed a number of large-scale GWA studies within and across all of the psychiatric disorders explored in this review [123]. Despite that, very few of the included studies utilized results from the PGC GWA studies to create a polygenic risk score for a particular disorder. As a field, if we understand the complexity of these psychiatric disorders and their biological mechanisms, then we must move away from candidate gene approaches that ignore this complexity.
Relatedly, many of the candidate genes explored in these studies were explored across disorder. For example, the serotonin transporter gene polymorphism was examined within multiple psychiatric disorders including in this review. This may suggest a common biological mechanism related to all psychiatric disorders. This may also suggest that there are general mental health polymorphisms that confer risk for more than one type of mental illness. Further, the PCGs have explored a cross disorder GWAS and developed a cross disorder polygenic risk score [123]. These polygenic approaches lend support to the idea that individuals may be genetically susceptible to psychiatric disorders in general. Future research should focus on this potential cross disorder approach, particularly given high rates of comorbidity among many psychiatric disorders.
One of the key findings of this scoping review was evidence of publication bias in the past 4.5 years of gene-by-environment research, a concept gaining attention across psychiatry research. A majority of the studies included in our review published statistically significant interaction effects, even in the presence of non-significant main effects. To combat publication bias, we must move toward a focus on reproducible science wherein researchers are completely transparent in their data and analytic models, journals are willing to publish papers with null findings, and where adequately powered replication studies are valued. Along with these key elements of reproducible research, gene-by-environment interaction researchers in particular should focus on identifying causal mechanisms through which genes interact with the environment to increase risk for or severity of mental health outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT Gene. 2003;301:5.
Thomas DC, Lewinger JP, Murcray CE, Gauderman WJ. Invited commentary: GE-whiz! Ratcheting gene-environment studies up to the whole genome and the whole exposome. Am J Epidemiol. 2012;175:203–7.
Dudbridge F. Power and predictive accuracy of polygenic risk scores. Wray NR, editor. PLoS Genet. 2013;9:e1003348.
Caspi A, Moffitt TE. Gene–environment interactions in psychiatry: joining forces with neuroscience. Nat Rev Neurosci. 2006;7:583–90.
Kendler KS, Myers J, Prescott CA. The etiology of phobias: an evaluation of the stress-diathesis model. Arch Gen Psychiatry. 2002;59:242–8.
Belsky J, Bakermans-Kranenburg MJ, van IJzendoorn MH. For better and for worse: differential susceptibility to environmental influences. Curr Dir Psychol Sci. 2007;16:300–4.
McAllister K, Mechanic LE, Amos C, Aschard H, Blair IA, Chatterjee N, et al. Current challenges and new opportunities for gene-environment interaction studies of complex diseases. Am J Epidemiol. 2017;186:753–61.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Cohen-Woods S, Fisher HL, Ahmetspahic D, Douroudis K, Stacey D, Hosang GM, et al. Interaction between childhood maltreatment on immunogenetic risk in depression: discovery and replication in clinical case-control samples. Brain Behav Immun. 2018;67:203–10.
Dunn EC, Wiste A, Radmanesh F, Almli LM, Gogarten SM, Sofer T, et al. Genome-wide association study (GWAS) and genome-wide by environment interaction study (GWEIS) of depressive symptoms in African American and Hispanic/Latina women: 2015 Donald F Klein investigator award winner: GWAS and GWEIS of depressive symptoms. Depress Anxiety. 2016;33:265–80.
Gonda X, Hullam G, Antal P, Eszlari N, Petschner P, Hökfelt TG, et al. Significance of risk polymorphisms for depression depends on stress exposure. Scientific Reports. 2018;8(1):3946. Available from: http://www.nature.com/articles/s41598-018-22221-z
Pishva E, Drukker M, Viechtbauer W, Decoster J, Collip D, van Winkel R, et al. Epigenetic genes and emotional reactivity to daily life events: a multi-step gene-environment interaction study. Dang Y, editor. PLoS One. 2014;9:e100935.
Van Assche E, Moons T, Cinar O, Viechtbauer W, Oldehinkel AJ, Van Leeuwen K, et al. Gene-based interaction analysis shows GABAergic genes interacting with parenting in adolescent depressive symptoms. J Child Psychol Psychiatry. 2017;58:1301–9.
Ware EB, Smith JA, Mukherjee B, Lee S, Kardia SLR, Diez-Roux AV. Applying novel methods for assessing individual- and neighborhood-level social and psychosocial environment interactions with genetic factors in the prediction of depressive symptoms in the multi-ethnic study of atherosclerosis. Behav Genet. 2016;46:89–99.
Cattaneo A, Cattane N, Malpighi C, Czamara D, Suarez A, Mariani N, et al. FoxO1, A2M, and TGF-β1: three novel genes predicting depression in gene X environment interactions are identified using cross-species and cross-tissues transcriptomic and miRNomic analyses. Mol Psychiatry. 2018;23(11):2192 [cited 2018 Nov 21]; Available from: http://www.nature.com/articles/s41380-017-0002-4
Van der Auwera S, Janowitz D, Schulz A, Homuth G, Nauck M, Völzke H, et al. Interaction among childhood trauma and functional polymorphisms in the serotonin pathway moderate the risk of depressive disorders. Eur Arch Psychiatry Clin Neurosci. 2014;264:45–54.
Mullins N, Power RA, Fisher HL, Hanscombe KB, Euesden J, Iniesta R, et al. Polygenic interactions with environmental adversity in the aetiology of major depressive disorder. Psychol Med. 2016;46:759–70.
Peterson RE, Cai N, Dahl AW, Bigdeli TB, Edwards AC, Webb BT, et al. Molecular genetic analysis subdivided by adversity exposure suggests etiologic heterogeneity in major depression. Am J Psychiatr. 2018;175:545–54.
Peyrot WJ, Milaneschi Y, Abdellaoui A, Sullivan PF, Hottenga JJ, Boomsma DI, et al. Effect of polygenic risk scores on depression in childhood trauma. Br J Psychiatry. 2014;205:113–9.
Åslund C, Nilsson KW. Individual biological sensitivity to environmental influences: testing the differential susceptibility properties of the 5HTTLPR polymorphism in relation to depressive symptoms and delinquency in two adolescent general samples. J Neural Transm. 2018;125:977–93.
Dalton ED, Hammen CL, Najman JM, Brennan PA. Genetic susceptibility to family environment: BDNF Val66met and 5-HTTLPR influence depressive symptoms. J Fam Psychol. 2014;28:947–56.
Risch N, Herrell R, Lehner T, Liang K-Y, Eaves L, Hoh J, et al. Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA. 2009;301:2462.
Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation. Arch Gen Psychiatry. 2011;68:444–54.
Chen Y, Brody GH. Family economic hardship, corticotropin-releasing hormone receptor polymorphisms, and depressive symptoms in rural African-American youths. J Adolesc Health. 2015;57:235–40.
Hettema JM, Chen X, Sun C, Brown TA. Direct, indirect and pleiotropic effects of candidate genes on internalizing disorder psychopathology. Psychol Med. 2015;45:2227–36.
Kovacs D, Eszlari N, Petschner P, Pap D, Vas S, Kovacs P, et al. Effects of IL1B single nucleotide polymorphisms on depressive and anxiety symptoms are determined by severity and type of life stress. Brain Behav Immun. 2016;56:96–104.
Laas K, Reif A, Akkermann K, Kiive E, Domschke K, Lesch K-P, et al. Interaction of the neuropeptide S receptor gene Asn107Ile variant and environment: contribution to affective and anxiety disorders, and suicidal behaviour. Int J Neuropsychopharmacol. 2014;17:541–52.
•• Musci RJ, Masyn KE, Benke K, Maher B, Uhl G, Ialongo NS. The effects of the interplay of genetics and early environmental risk on the course of internalizing symptoms from late childhood through adolescence. Dev Psychopathol. 2016;28:225–37. One of the few studies to utilize a polygenic approach, with the score being derived from the psychiatric genetics consortium, and one of the few studies to publish null findings for gene by environment interactions.
Nobile M, Greco A, Perna G, Colombo P, Bianchi V, Bellina M, et al. Effect of the serotonin transporter gene and of environment on the continuity of anxiety and depression traits throughout adolescence. Epidemiol Psychiatr Sci. 2014;23:399–409.
Pagliaccio D, Luby JL, Bogdan R, Agrawal A, Gaffrey MS, Belden AC, et al. Amygdala functional connectivity, HPA axis genetic variation, and life stress in children and relations to anxiety and emotion regulation. J Abnorm Psychol. 2015;124:817–33.
Scheuer S, Ising M, Uhr M, Otto Y, von Klitzing K, Klein AM. FKBP5 polymorphisms moderate the influence of adverse life events on the risk of anxiety and depressive disorders in preschool children. J Psychiatr Res. 2016;72:30–6.
Sheikh HI, Kryski KR, Kotelnikova Y, Hayden EP, Singh SM. Catechol-O-methyltransferase gene (val158met) polymorphisms and anxious symptoms in early childhood: the roles of hypothalamus-pituitary-adrenal axis reactivity and life stress. Neurosci Lett. 2017;659:86–91.
Tabak BA, Vrshek-Schallhorn S, Zinbarg RE, Prenoveau JM, Mineka S, Redei EE, et al. Interaction of CD38 variant and chronic interpersonal stress prospectively predicts social anxiety and depression symptoms over 6 years. Clin Psychol Sci. 2016;4:17–27.
Pérez-Pérez B, Cristóbal-Narváez P, Sheinbaum T, Kwapil TR, Ballespí S, Peña E, et al. Interaction between FKBP5 variability and recent life events in the anxiety spectrum: evidence for the differential susceptibility model. Branchi I, editor. PLoS One. 2018;13:e0193044.
de Castro-Catala M, Peña E, Kwapil TR, Papiol S, Sheinbaum T, Cristóbal-Narváez P, et al. Interaction between FKBP5 gene and childhood trauma on psychosis, depression and anxiety symptoms in a non-clinical sample. Psychoneuroendocrinology. 2017;85:200–9.
•• Cicchetti D, Rogosch FA. Genetic moderation of child maltreatment effects on depression and internalizing symptoms by serotonin transporter linked polymorphic region (5-HTTLPR), brain-derived neurotrophic factor (BDNF), norepinephrine transporter (NET), and corticotropin releasing hormone receptor 1 (CRHR1) genes in African American children. Dev Psychopathol. 2014;26:1219–39. This study utilized an understudied population in genetics research to explore gene by environment interactions for a number of candidate genes.
Hemmings SMJ, Martin LI, van der Merwe L, Benecke R, Domschke K, Seedat S. Serotonin transporter variants play a role in anxiety sensitivity in South African adolescents. World J Biol Psychiatry. 2016;17:66–75.
Klauke B, Deckert J, Zwanzger P, Baumann C, Arolt V, Pauli P, et al. Neuropeptide S receptor gene ( NPSR ) and life events: G × E effects on anxiety sensitivity and its subdimensions. World J Biol Psychiatry. 2014;15:17–25.
Martin L, Hemmings SMJ, Kidd M, Seedat S. No gene-by-environment interaction of BDNF Val66Met polymorphism and childhood maltreatment on anxiety sensitivity in a mixed race adolescent sample. Eur J Psychotraumatol. 2018;9:1472987.
McGregor NW, Hemmings SMJ, Erdman L, Calmarza-Font I, Stein DJ, Lochner C. Modification of the association between early adversity and obsessive-compulsive disorder by polymorphisms in the MAOA. MAOB and COMT genes Psychiatry Research. 2016;246:527–32.
Min J-A, Lee H-J, Lee S-H, Park Y-M, Kang S-G, Park Y-G, et al. RORA polymorphism interacts with childhood maltreatment in determining anxiety sensitivity by sex: a preliminary study in healthy young adults. Clin Psychopharm Neu. 2017;15:402–6.
Schiele MA, Ziegler C, Holitschke K, Schartner C, Schmidt B, Weber H, et al. Influence of 5-HTT variation, childhood trauma and self-efficacy on anxiety traits: a gene-environment-coping interaction study. J Neural Transm. 2016;123:895–904.
Lazary J, Eszlari N, Juhasz G, Bagdy G. Genetically reduced FAAH activity may be a risk for the development of anxiety and depression in persons with repetitive childhood trauma. Eur Neuropsychopharmacol. 2016;26:1020–8.
Ibarra P, Alemany S, Fatjó-Vilas M, Córdova-Palomera A, Goldberg X, Arias B, et al. The BDNF-Val66Met polymorphism modulates parental rearing effects on adult psychiatric symptoms: a community twin-based study. Eur Psychiatry. 2014;29:293–300.
Nelemans SA, van Assche E, Bijttebier P, Colpin H, van Leeuwen K, Verschueren K, et al. Parenting interacts with oxytocin polymorphisms to predict adolescent social anxiety symptom development: a novel polygenic approach. J Abnorm Child Psychol [Internet]. 2018 [cited 2018 Nov 21]; Available from: https://doi.org/10.1007/s10802-018-0432-8
Notzon S, Domschke K, Holitschke K, Ziegler C, Arolt V, Pauli P, et al. Attachment style and oxytocin receptor gene variation interact in influencing social anxiety. World J Biol Psychiatry. 2016;17:76–83.
Olofsdotter S, Åslund C, Furmark T, Comasco E, Nilsson KW. Differential susceptibility effects of oxytocin gene (OXT) polymorphisms and perceived parenting on social anxiety among adolescents. Dev Psychopathol. 2018;30:449–59.
Park S, Nam Y-Y, Sim Y, Hong JP. Interactions between the apolipoprotein E ɛ 4 allele status and adverse childhood experiences on depressive symptoms in older adults. Eur J Psychotraumatol. 2015;6:25178.
• Reinelt E, Aldinger M, Stopsack M, Schwahn C, John U, Baumeister SE, et al. High social support buffers the effects of 5-HTTLPR genotypes within social anxiety disorder. Eur Arch Psychiatry Clin Neurosci. 2014;264:433–9. This study explored the potential resilience factors in place for individuals who are carriers of a particular genotype demonstrated to be associated with negative outcomes.
Schiele MA, Costa B, Abelli M, Martini C, Baldwin DS, Domschke K, et al. Oxytocin receptor gene variation, behavioural inhibition, and adult separation anxiety: role in complicated grief. World J Biol Psychiatry. 2018;19:471–9.
Lahat A, van Lieshout RJ, Mathewson KJ, Mackillop J, Saigal S, Morrison KM, et al. Extremely low birth weight babies grown up: gene–environment interaction predicts internalizing problems in the third and fourth decades of life. Dev Psychopathol. 2017;29:837–43.
O’Donnell KJ, Glover V, Holbrook JD, O’Connor TG. Maternal prenatal anxiety and child brain-derived neurotrophic factor (BDNF) genotype: effects on internalizing symptoms from 4 to 15 years of age. Dev Psychopathol. 2014;26:1255–66.
van Os J, Rutten BP, Poulton R. Gene-environment interactions in schizophrenia: review of epidemiological findings and future directions. Schizophr Bull. 2008;34:1066–82.
Bernardo M, Bioque M, Cabrera B, Lobo A, González-Pinto A, Pina L, et al. Modelling gene-environment interaction in first episodes of psychosis. Schizophr Res. 2017;189:181–9.
Mandelli L, Toscano E, Porcelli S, Fabbri C, Serretti A. Age of onset in schizophrenia spectrum disorders: complex interactions between genetic and environmental factors. Psychiatry Investig. 2016;13:247.
Hoffmann C, Van Rheenen TE, Mancuso SG, Zalesky A, Bruggemann J, Lenroot RK, et al. Exploring the moderating effects of dopaminergic polymorphisms and childhood adversity on brain morphology in schizophrenia-spectrum disorders. Psychiatry Res Neuroimaging. 2018;281:61–8.
McCarthy-Jones S, Green MJ, Scott RJ, Tooney PA, Cairns MJ, Wu JQ, et al. Preliminary evidence of an interaction between the FOXP2 gene and childhood emotional abuse predicting likelihood of auditory verbal hallucinations in schizophrenia. J Psychiatr Res. 2014;50:66–72.
Trotta A, Iyegbe C, Di Forti M, Sham PC, Campbell DD, Cherny SS, et al. Interplay between schizophrenia polygenic risk score and childhood adversity in first-presentation psychotic disorder: a pilot study. Walss-Bass C, editor. PLoS One. 2016;11:e0163319.
Colizzi M, Iyegbe C, Powell J, Ursini G, Porcelli A, Bonvino A, et al. Interaction between functional genetic variation of DRD2 and cannabis use on risk of psychosis. Schizophr Bull. 2015;41:1171–82.
French L, Gray C, Leonard G, Perron M, Pike GB, Richer L, et al. Early cannabis use, polygenic risk score for schizophrenia and brain maturation in adolescence. JAMA Psychiatry. 2015;72:1002.
Liuhanen J, Suvisaari J, Kajantie E, Miettunen J, Sarin A-P, Järvelin M-R, et al. Interaction between compound genetic risk for schizophrenia and high birth weight contributes to social anhedonia and schizophrenia in women. Psychiatry Res. 2018;259:148–53.
Ursini G, Cavalleri T, Fazio L, Angrisano T, Iacovelli L, Porcelli A, et al. BDNF rs6265 methylation and genotype interact on risk for schizophrenia. Epigenetics. 2016;11:11–23.
Børglum AD, Demontis D, Grove J, Pallesen J, Hollegaard MV, Pedersen CB, et al. Genome-wide study of association and interaction with maternal cytomegalovirus infection suggests new schizophrenia loci. Mol Psychiatry. 2014;19:325–33.
Mihaljevic M, Zeljic K, Soldatovic I, Andric S, Mirjanic T, Richards A, et al. The emerging role of the FKBP5 gene polymorphisms in vulnerability–stress model of schizophrenia: further evidence from a Serbian population. Eur Arch Psychiatry Clin Neurosci. 2017;267:527–39.
Colodro-Conde L, Couvy-Duchesne B, Whitfield JB, Streit F, Gordon S, Rietschel M, et al. Higher genetic risk for schizophrenia is associated with living in urban and populated areas. Eur Neuropsychopharmacol. 2017;27:S488.
Nigg J, Nikolas M, Burt SA. Measured gene-by-environment interaction in relation to attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:863–73.
Baptista J, Belsky J, Mesquita A, Soares I. Serotonin transporter polymorphism moderates the effects of caregiver intrusiveness on ADHD symptoms among institutionalized preschoolers. Eur Child Adolesc Psychiatry. 2017;26:303–13.
Elmore AL, Nigg JT, Friderici KH, Jernigan K, Nikolas MA. Does 5HTTLPR genotype moderate the association of family environment with child attention-deficit hyperactivity disorder symptomatology? J Clin Child Adolesc Psychol. 2016;45:348–60.
Morgan JE, Caplan B, Tung I, Noroña AN, Baker BL, Lee SS. COMT and DAT1 polymorphisms moderate the indirect effect of parenting behavior on youth ADHD symptoms through neurocognitive functioning. Child Neuropsychology. 2018;24:823–43.
Nikitopoulos J, Zohsel K, Blomeyer D, Buchmann AF, Schmid B, Jennen-Steinmetz C, et al. Are infants differentially sensitive to parenting? Early maternal care, DRD4 genotype and externalizing behavior during adolescence. J Psychiatr Res. 2014;59:53–9.
Nikolas MA, Momany AM. DRD4 variants moderate the impact of parental characteristics on child attention-deficit hyperactivity disorder: exploratory evidence from a multiplex family design. J Abnorm Child Psychol. 2017;45:429–42.
Richards JS, Hartman CA, Franke B, Hoekstra PJ, Heslenfeld DJ, Oosterlaan J, et al. Differential susceptibility to maternal expressed emotion in children with ADHD and their siblings? Investigating plasticity genes, prosocial and antisocial behaviour. Eur Child Adolesc Psychiatry. 2015;24:209–17.
Richards JS, Arias Vásquez A, von Rhein D, van der Meer D, Franke B, Hoekstra PJ, et al. Adolescent behavioral and neural reward sensitivity: a test of the differential susceptibility theory. Transl Psychiatry. 2016;6:e771–1.
Richards JS, Arias Vásquez A, van Rooij D, van der Meer D, Franke B, Hoekstra PJ, et al. Testing differential susceptibility: plasticity genes, the social environment, and their interplay in adolescent response inhibition. World J Biol Psychiatry. 2017;18:308–21.
Riva V, Battaglia M, Nobile M, Cattaneo F, Lazazzera C, Mascheretti S, et al. GRIN2B predicts attention problems among disadvantaged children. Eur Child Adolesc Psychiatry. 2015;24:827–36.
Stenseng F, Li Z, Belsky J, Hygen BW, Skalicka V, Guzey IC, et al. Peer problems and hyperactivity-impulsivity among Norwegian and American children: the role of 5-HTTLPR. Child Dev. 2018;89:509–24.
van der Meer D, Hartman CA, van Rooij D, Franke B, Heslenfeld DJ, Oosterlaan J, et al. Effects of dopaminergic genes, prenatal adversities, and their interaction on attention-deficit/hyperactivity disorder and neural correlates of response inhibition. J Psychiatry Neurosci. 2017;42:113–21.
Boecker-Schlier R, Holz NE, Buchmann AF, Blomeyer D, Plichta MM, Jennen-Steinmetz C, et al. Interaction between COMT Val 158 met polymorphism and childhood adversity affects reward processing in adulthood. NeuroImage. 2016;132:556–70.
Brinksma DM, Hoekstra PJ, de Bildt A, Buitelaar JK, van den Hoofdakker BJ, Hartman CA, et al. ADHD symptoms in middle adolescence predict exposure to person-related life stressors in late adolescence in 5-HTTLPR S-allele homozygotes. J Abnorm Child Psychol. 2018;46:1427–37.
Morgan JE, Hammen C, Lee SS. Parental serotonin transporter polymorphism (5-HTTLPR) moderates associations of stress and child behavior with parenting behavior. J Clin Child Adolesc Psychol. 2016:1–12.
van der Meer D, Hoekstra PJ, Zwiers M, Mennes M, Schweren LJ, Franke B, et al. Brain correlates of the interaction between 5-HTTLPR and psychosocial stress mediating attention deficit hyperactivity disorder severity. Am J Psychiatr. 2015;172:768–75.
van der Meer D, Hoekstra PJ, Bralten J, van Donkelaar M, Heslenfeld DJ, Oosterlaan J, et al. Interplay between stress response genes associated with attention-deficit hyperactivity disorder and brain volume: interplay between stress response genes in ADHD. Genes Brain Behav. 2016;15:627–36.
Zohsel K, Bianchi V, Mascheretti S, Hohm E, Schmidt MH, Esser G, et al. Monoamine oxidase a polymorphism moderates stability of attention problems and susceptibility to life stress during adolescence: monoamine oxidase a polymorphism moderates stability. Genes Brain Behav. 2015;14:565–72.
Sánchez-Mora C, Richarte V, Garcia-Martínez I, Pagerols M, Corrales M, Bosch R, et al. Dopamine receptor DRD4 gene and stressful life events in persistent attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2015;168:480–91.
Park S, Kim B-N, Kim J-W, Shin M-S, Yoo HJ, Cho S-C. Interactions between early trauma and catechol-O-methyltransferase genes on inhibitory deficits in children with ADHD. J Atten Disord. 2017;21:183–9.
Gu X, Yuan F, Huang X, Hou Y, Wang M, Lin J, et al. Association of PIK3CG gene polymorphisms with attention-deficit/hyperactivity disorder: a case-control study. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;81:169–77.
•• Kim JI, Kim J-W, Lee J-M, Yun HJ, Sohn C, Shin M-S, et al. Interaction between DRD2 and lead exposure on the cortical thickness of the frontal lobe in youth with attention-deficit/hyperactivity disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;82:169–76. A study demonstrating that an environmental toxicant is associated with changes in brain morphology among individuals with a particular genotype.
Yuan F, Gu X, Huang X, Zhong Y, Wu J. SLC6A1 gene involvement in susceptibility to attention-deficit/hyperactivity disorder: a case-control study and gene-environment interaction. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;77:202–8.
Park S, Kim B-N, Cho S-C, Kim Y, Kim J-W, Lee J-Y, et al. Association between urine phthalate levels and poor attentional performance in children with attention-deficit hyperactivity disorder with evidence of dopamine gene-phthalate interaction. Int J Environ Res Public Health. 2014;11:6743–56.
Chang C-H, Yu C-J, Du J-C, Chiou H-C, Chen H-C, Yang W, et al. The interactions among organophosphate pesticide exposure, oxidative stress, and genetic polymorphisms of dopamine receptor D4 increase the risk of attention deficit/hyperactivity disorder in children. Environ Res. 2018;160:339–46.
Tung I, Morgan JE, Noroña AN, Lee SS. Prenatal programming of postnatal plasticity for externalizing behavior: testing an integrated developmental model of genetic and temperamental sensitivity to the environment. Dev Psychobiol. 2017;59:984–96.
Brinksma DM, Hoekstra PJ, van den Hoofdakker B, de Bildt A, Buitelaar JK, Hartman CA, et al. Age-dependent role of pre- and perinatal factors in interaction with genes on ADHD symptoms across adolescence. J Psychiatr Res. 2017;90:110–7.
van der Meer D, Hartman CA, Richards J, Bralten JB, Franke B, Oosterlaan J, et al. The serotonin transporter gene polymorphism 5-HTTLPR moderates the effects of stress on attention-deficit/hyperactivity disorder. J Child Psychol Psychiatry. 2014;55:1363–71.
van der Meer D, Hartman CA, Pruim RHR, Mennes M, Heslenfeld D, Oosterlaan J, et al. The interaction between 5-HTTLPR and stress exposure influences connectivity of the executive control and default mode brain networks. Brain Imaging Behav. 2017;11:1486–96.
Waldie KE, Cornforth CM, Webb RE, Thompson JMD, Murphy R, Moreau D, et al. Dopamine transporter ( DAT1/SLC6A3 ) polymorphism and the association between being born small for gestational age and symptoms of ADHD. Behav Brain Res. 2017;333:90–7.
Gaugler T, Klei L, Sanders SJ, Bodea CA, Goldberg AP, Lee AB, et al. Most genetic risk for autism resides with common variation. Nat Genet. 2014;46:881–5.
Ozonoff S, Young GS. Recurrence risk for autism spectrum disorders: a baby siblings research consortium study. 2018;128:10.
Webb SJ, Garrison MM, Bernier R, McClintic AM, King BH, Mourad PD. Severity of ASD symptoms and their correlation with the presence of copy number variations and exposure to first trimester ultrasound: ultrasound exposure and ASD severity. Autism Res. 2017;10:472–84.
Mazina V, Gerdts J, Trinh S, Ankenman K, Ward T, Dennis MY, et al. Epigenetics of autism-related impairment: copy number variation and maternal infection. J Dev Behav Pediatr. 2015;36:61–7.
Kim D, Volk H, Girirajan S, Pendergrass S, Hall MA, Verma SS, et al. The joint effect of air pollution exposure and copy number variation on risk for autism: genetic and environment interaction in autism. Autism Res. 2017;10:1470–80.
Schmidt RJ, Tancredi DJ, Ozonoff S, Hansen RL, Hartiala J, Allayee H, et al. Maternal periconceptional folic acid intake and risk of autism spectrum disorders and developmental delay in the CHARGE (CHildhood Autism Risks from Genetics and Environment) case-control study. Am J Clin Nutr. 2012;96:80–9.
Volk HE, Kerin T, Lurmann F, Hertz-Picciotto I, McConnell R, Campbell DB. Autism spectrum disorder: interaction of air pollution with the MET receptor tyrosine kinase gene. Epidemiology. 2014;25:44–7.
Ackerman S, Schoenbrun S, Hudac C, Bernier R. Interactive effects of prenatal antidepressant exposure and likely gene disrupting mutations on the severity of autism spectrum disorder. J Autism Dev Disord. 2017;47:3489–96.
Anand A, Koller DL, Lawson WB, Gershon ES, Nurnberger JI. Genetic and childhood trauma interaction effect on age of onset in bipolar disorder: an exploratory analysis. J Affect Disord. 2015;179:1–5.
Hosang GM, Fisher HL, Cohen-Woods S, McGuffin P, Farmer AE. Stressful life events and catechol-O-methyl-transferase (COMT) gene in bipolar disorder: H osang et al. Depress Anxiety. 2017;34:419–26.
Oliveira J, Etain B, Lajnef M, Hamdani N, Bennabi M, Bengoufa D, et al. Combined effect of TLR2 gene polymorphism and early life stress on the age at onset of bipolar disorders. PLoS One. 2015;13.
Aas M, Haukvik UK, Djurovic S, Tesli M, Athanasiu L, Bjella T, et al. Interplay between childhood trauma and BDNF val66met variants on blood BDNF mRNA levels and on hippocampus subfields volumes in schizophrenia spectrum and bipolar disorders. J Psychiatr Res. 2014;59:14–21.
• Breen ME, Seifuddin F, Zandi PP, Potash JB, Willour VL. Investigating the role of early childhood abuse and HPA axis genes in suicide attempters with bipolar disorder. Psychiatr Genet. 2015;25:106–11. A gene pathway approach goes beyond candidate genes to focus on genes within a particular mechanism (HPA Axis) to explore the role of early childhood abuse among suicide attempters with bipolar disorder.
Karanović J, Ivković M, Jovanović VM, Šviković S, Pantović-Stefanović M, Brkušanin M, et al. Effect of childhood general traumas on suicide attempt depends on TPH2 and ADARB1 variants in psychiatric patients. J Neural Transm. 2017;124:621–9.
Fraguas D, Díaz-Caneja CM, Corripio I, González-Pinto A, Lobo A, Bioque M, et al. Gene-environment interaction as a predictor of early adjustment in first episode psychosis. Schizophr Res. 2017;189:196–203.
Bortolasci CC, Vargas HO, Souza-Nogueira A, Barbosa DS, Moreira EG, Nunes SOV, et al. Lowered plasma paraoxonase (PON)1 activity is a trait marker of major depression and PON1 Q192R gene polymorphism–smoking interactions differentially predict the odds of major depression and bipolar disorder. J Affect Disord. 2014;159:23–30.
Oliveira J, Kazma R, Le Floch E, Bennabi M, Hamdani N, Bengoufa D, et al. Toxoplasma gondii exposure may modulate the influence of TLR2 genetic variation on bipolar disorder: a gene–environment interaction study. International Journal of Bipolar Disorders. 2016;4(1). Available from: https://doi.org/10.1186/s40345-016-0052-6
Palmer RHC, Nugent NR, Brick LA, Bidwell CL, McGeary JE, Keller MC, et al. Evidence of shared genome-wide additive genetic effects on interpersonal trauma exposure and generalized vulnerability to drug dependence in a population of substance users: genetics of drug dependence and trauma. J Trauma Stress. 2016;29:197–204.
Richmond-Rakerd LS, Slutske WS, Lynskey MT, Agrawal A, Madden PAF, Bucholz KK, et al. Age at first use and later substance use disorder: shared genetic and environmental pathways for nicotine, alcohol, and cannabis. J Abnorm Psychol. 2016;125:946–59.
Polimanti R, Zhao H, Farrer LA, Kranzler HR, Gelernter J. Ancestry-specific and sex-specific risk alleles identified in a genome-wide gene-by-alcohol dependence interaction study of risky sexual behaviors. Am J Med Genet B Neuropsychiatr Genet. 2017;174:846–53.
Polimanti R, Meda SA, Pearlson GD, Zhao H, Sherva R, Farrer LA, et al. S100A10 identified in a genome-wide gene × cannabis dependence interaction analysis of risky sexual behaviours. J Psychiatry Neurosci. 2017;42:252–61.
Prom-Wormley EC, Ebejer J, Dick DM, Bowers MS. The genetic epidemiology of substance use disorder: a review. Drug Alcohol Depend. 2017;180:241–59.
Petersen L, Sørensen TIA, Kragh Andersen P, Bo Mortensen P, Hawton K. Genetic and familial environmental effects on suicide attempts: a study of Danish adoptees and their biological and adoptive siblings. J Affect Disord. 2014;155:273–7.
Brodsky BS. Early childhood environment and genetic interactions: the diathesis for suicidal behavior. Current Psychiatry Reports. 2016;18(9):86. Available from: https://doi.org/10.1007/s11920-016-0716-z
Turecki G, Ota VK, Belangero SI, Jackowski A, Kaufman J. Early life adversity, genomic plasticity, and psychopathology. Lancet Psychiatry. 2014;1:461–6.
Benedetti F, Riccaboni R, Poletti S, Radaelli D, Locatelli C, Lorenzi C, et al. The serotonin transporter genotype modulates the relationship between early stress and adult suicidality in bipolar disorder. Bipolar Disord. 2014;16:857–66.
Doorley J, Williams C, Mallard T, Esposito-Smythers C, McGeary J. Sexual trauma, the dopamine D4 receptor, and suicidal ideation among hospitalized adolescents: a preliminary investigation. Arch Suicide Res. 2017;21:279–92.
Cross-Disorder Group of the Psychiatric Genetics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Genetic Disorders
Rights and permissions
About this article
Cite this article
Musci, R.J., Augustinavicius, J.L. & Volk, H. Gene-Environment Interactions in Psychiatry: Recent Evidence and Clinical Implications. Curr Psychiatry Rep 21, 81 (2019). https://doi.org/10.1007/s11920-019-1065-5
Published:
DOI: https://doi.org/10.1007/s11920-019-1065-5