Abstract
Purpose of Review
We review the recent literature regarding the implications of gender on the diagnosis and treatment of autism spectrum disorder (ASD) in women and adolescent females. We also discuss important clinical observations in treating this population.
Recent Findings
Growing research supports gender specificity in ASD symptom presentation. Differing phenotypes, psychiatric co-morbidities, and level of “camouflaging” (behavioral coping strategies to conceal symptoms for use in social situations) are thought to further contribute to the discrepancy in prevalence rates and resulting misdiagnosis or delayed diagnosis in adolescent females and women.
Summary
Both nosological and cultural factors appear to be contributing to differences in the diagnosis of ASD in women. These differences in presentation have important implications for late diagnosis, treatment of ASD, and the quality of life for women with autism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a heterogeneous neurodevelopmental condition characterized by impairments in social communication skills and accompanying restricted and repetitive patterns of interests or behaviors [1]. While ASD affects both males and females, it is much more commonly diagnosed in boys, and girls and women are typically diagnosed later than boys and men. There is, however, growing recognition of the discrepancy between the sexes with regard to ASD prevalence rates, symptom presentation, diagnosis, treatment, and outcomes. To begin to understand the scope of any possible sex differences and their implications, it is imperative to first understand the nascency of ASD as a diagnosis. ASD was first described in the 1940s as a “disturbance of affective contact” and “autistic psychopathy” by Leo Kanner and Hans Asperger, respectively [2, 3]. Their initial, independent reports included samples of only three girls out of 11 total cases, and zero girls out of four total cases. The early epidemiological studies of ASD with co-morbid intellectual disability that followed also showed a strong male bias with a male-to-female gender ratio of 3–4:1 [4,5,6]. This ratio is even higher for individuals of average to above average intellect [7, 8]. However, early studies likely underestimated the number of females with ASD if they presented with symptoms uncharacteristic of the male presentation. Research studies have historically included participants based on these originally reported ratios or included only male participants. This longstanding underrepresentation of females in both research and clinical practice has led to a speculated male-biased understanding of ASD. As Lai and colleagues (2015) succinctly state in their seminal paper, “our understanding of ASD may have been substantially biased toward males.” Due to the higher prevalence rates of ASD in males, research that addresses phenotypic characterization has been conducted in primarily male samples, including the behavioral descriptions used to develop the current criteria for diagnosing ASD [1, 9].
Understanding the Male Bias
Prevalence varies by sex for ASD, as with many conditions affecting neurodevelopment, such that ASD is much more common in males than females, with an overall prevalence ratio reported as 4:1 [1]. In their most recent update, the US Autism and Developmental Disabilities Monitoring Network (ADDMN), for example, reported an overall male-to-female prevalence ratio of 4:1 among 8-year-old children across the 11 ADDMN sites [10•]. This represents a decrease from 4.5:1, which the ADDMN group attributes to a greater increase in prevalence rate among females as compared with males. Intellectual disability also appears to play a role in prevalence rate, with a greater proportion of females with ASD diagnosed with co-morbid intellectual disability than males with ASD [10•].
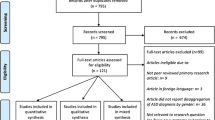
The 4:1 male-to-female prevalence ratio reported in ASD, however, is somewhat dependent on the population studied. Recently Loomes, Hull, and Mandy (2017) conducted a systematic review and meta-analysis to evaluate the male-to-female prevalence ratio further [11••]. They analyzed 54 studies and found an overall male-to-female ratio of 4.2:1, but found substantial variability across studies. The authors examined “active” versus “passive” studies, with “active studies” defined as those that involved screening a population-based sample with or without ASD, versus “passive studies” defined as those that involved reviewing an existing database of patients with a pre-established ASD diagnosis and found that “active” studies had a lower male-to-female ratio. This suggests that there is a subset of females who are not being diagnosed with ASD, despite having clinically significant symptoms. The authors concluded that the male-to-female ratio is likely to be lower than that of 4:1 that is generally reported, perhaps closer to 3:1.
Female Phenotype
This difference in prevalence rates between males and females points to the likelihood that females with ASD on the whole may present with slightly different symptoms than males with ASD, in particular among girls without intellectual or language impairments [1]. According to recent research conducted by Kreiser and White (2014), females diagnosed with ASD present with unique characteristics in each aspect of the diagnostic criteria when compared to their male counterparts. For example, regarding social communication, females tend to engage in imaginative and pretend play from a young age [12]. Their speech also contains more vocabulary words related to emotions, compared to traditional diagnostic criteria of ASD often found in males. It has also been observed that females with ASD tend to have greater awareness and desire for social interaction, propensity to mimic others in social interactions, tendency to camouflage difficulties by developing coping strategies, and develop one or two close friends compared to their male counterparts [12]. Different than the traditional restricted interests in inanimate objects often described within males with ASD, many females with ASD tend to have restricted interests related to people and animals (e.g., celebrities, pets). Additional characteristics found within women with ASD include perfectionist tendencies and disordered eating [13].
Delayed Diagnosis
As many females are undiagnosed or misdiagnosed, women diagnosed with ASD later in life report experiences involving barriers to gaining diagnosis, strategies used to try to fit in with peers, and victimization [14••]. In a qualitative research study by Bargiela and colleagues (2016), late-diagnosed women reported health professionals being dismissive and unfamiliar with the female phenotype. Many reported experiences of victimization, such as unhealthy relationships and emotional, physical, and sexual abuse due to passivity or social naiveté related to their ASD and a desire to feel accepted. Bargiela and colleagues also suggest a particular challenge for females related to role expectations within our culture and pressure to conform to traditional feminine roles that are often incompatible with how a person with ASD may want to live. Obtaining a diagnosis promoted a sense of belonging within a community and an improved self-view.
For clinicians, there are also often practical barriers in making a first-time diagnosis of ASD in adulthood that disproportionately affect female patients. Since ASD can often go undiagnosed or misdiagnosed in females, when individuals present for diagnostic evaluations later in life, it is often more challenging to obtain a valid and reliable report of the patient’s developmental history, which is indispensable to confirm a diagnosis. Adult patients may no longer have living caregivers to serve as informants, and when they do, the quality of the informant’s recall may not be detailed or may be inaccurate due to memory decay. Given that ASD is on average diagnosed later in females than males, these difficulties with diagnosis disproportionately affect women and can lead to inconclusive outcomes and present a further roadblock for treatment and services.
Camouflaging
Adults diagnosed with ASD in childhood tend to demonstrate a reduction in ASD symptoms over time [15]. Irrespective of age at diagnosis, individuals with ASD are thought to develop coping strategies over the course of their lives in response to treatment interventions, as well as due to pressures to conform to societal demands. One such strategy is camouflaging. Camouflaging refers to the behavior of using coping strategies in social situations to hide behaviors associated with ASD, through the use of explicit techniques to seem socially proficient, and through attempts to prevent others from seeing their social difficulties [16•]. Thus, camouflaging reflects the gap between how individuals with ASD behave and their true inclinations and abilities. Examples of camouflaging include active attempts to make eye contact despite resulting discomfort for the individual, using learned phrases or jokes in conversation, altering their speech volume, mimicking nonverbal affect including gestures and facial expressions, and not standing too close to others [13, 17••].
While camouflaging has been documented in both genders, it has been proposed as a possible explanation for misdiagnosis, delayed diagnosis, and gender disparity in the diagnosis of women with ASD [14••, 16•]. Recent research examining camouflaging in women suggest that it is a widespread but not universal behavior [14••]. Qualitative research indicates women repeatedly described, “pretending to be normal;” for women with ASD, camouflaging is reported as cognitively effortful, exhausting, and challenging to one’s identity and further led to being manipulated by others [14••]. Camouflaging differs from acquired skills gained through social skills training, in its aim. While both may produce a reduction in observable, external ASD behaviors, social skills training results in the development of successful and naturalistic use of social skills versus an anxiety-driven, rule-based use that, while reducing behaviors, results in a significant emotional and physical toll for individuals with ASD. The difference between these two phenomena can be difficult to fully assess as they largely reflect the internal experience of the individual. Nevertheless, it is important to not minimize internal distress that individuals with ASD may experience due to their desire to conform with societal expectations and rules.
Sex-Related Differences in Cognition, Neuroanatomy, and Functionality
Greater compensatory skills of females with ASD without intellectual disability has been associated with better observational learning of nonverbal communication, a better intellectual understanding of the rules associated with friendship, sociability, and emotionality, and adoption of social roles and using scripts [18•, 19]. However, research on a sex-related cognitive difference in ASD is still limited and has often shown heterogeneous results. Most cognitive research to date has focused on examining differences in executive functioning, with other cognitive domains often unexplored. Some research suggests that females with ASD display better processing speed abilities and worse visuospatial abilities than males with ASD [19,20,21].
Numerous studies have found individuals with ASD to have deficits in executive functioning compared to their neurotypical peers; however, these studies have largely focused on children. Given that brain maturation, particularly in the frontal and striatal regions, continues into early adulthood, research on executive functioning across the lifespan is imperative. The earliest work examining executive functioning in adults with ASD often did not include women or had too small a sample size to allow for comparison. The most consistent findings in these studies with predominantly male participants show deficits in working memory, cognitive flexibility, planning, self-monitoring, and verbal fluency. Only a few studies to date have explored executive functioning in adults while further examining for possible sex-related differences [22•]. In a study by Kiep and Spek (2017), gender differences in executive functioning were examined in a group of 99 men and 40 women with ASD compared to 35 neurotypical men and 25 neurotypical women, using instruments assessing planning, mental flexibility, working memory, generativity, and self-monitoring. The investigators found no differences in planning abilities between men and women with ASD or in comparison with neurotypical adults; this is inconsistent with prior work showing overall impairment for individuals with ASD [23]. Kiep and Spek (2017) found that individuals with ASD showed impairments in mental flexibility on the Wisconsin Card Sorting Test (i.e., switching between categories) compared to neurotypical individuals. Women with ASD made more perseverative errors but also successfully sorted more categories than their male counterparts, but intelligence appeared to mediate this performance. Women with ASD also had worse working memory performance than men with ASD, although this may reflect an overall gender difference observed in neurotypical persons [22•]. Lastly, Kiep and Spek (2017) found that women with ASD did not differ from neurotypical women in word generation, but could produce more names of animals than men with ASD. This is contrary to prior work [18•] that found no deficits in ASD, and Keip and Spek suggest that it may reflect women with ASD having more “common” special interests such as animals than men with ASD.
Differences in brain neuroanatomy, connectivity, and brain activation patterns have also been noted between genders [24,25,26]. A study by Lai and colleagues (2013) found evidence that neuroanatomy is sex-dependent in adults with ASD without intellectual disability, with women displaying neuroanatomical features, in both gray and white matter, that overlapped with sexually dimorphic structures in neurotypical controls. This was supported by prior studies in structural imaging that found attenuated sex differences in males and females with ASD in brain regions that typically show sex differences [27]. Females with ASD also showed altered connectivity, generally hyperconnectivity, consistent with patterns of neural masculinization, a pattern not observed in males [25]. The results from these studies support the “Extreme Male Brain” (EMB) theory that proposes that an extreme form of the typical “empathizing-systemizing” cognitive profile and “hyper-masculinization” of the brain characterizes individuals with ASD [28]. In a study examining functional activity during cognitive tests, there was no difference between men and women with ASD without intellectual disability on a verbal fluency test, although enhanced activation of the left occipitoparietal and inferior prefrontal regions was found in subjects with ASD compared to controls [26]. On a test of mental rotation, however, these investigators did find sex-by-diagnosis interactions across occipital, temporal, parietal, and middle frontal regions with greater activation in males with ASD compared to females.
Psychiatric Co-morbidities
Psychiatric co-morbid conditions occur frequently in individuals with ASD, as they do in neurotypical persons, although studies examining gender differences in co-morbid conditions in adults with ASD are far less frequent. Common co-morbid psychiatric disorders in adults with ASD include depressive disorders, anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder, eating disorders, and personality disorders [29, 30]. For neurotypical individuals, there are no differences in rates of depression between genders during childhood. However, after age 15 years, typically developing females have approximately twice the risk of developing depression [31]. Individuals with ASD demonstrate higher rates of internalizing disorders compared to neurotypical peers [32]. These findings suggest that adolescent females and women with ASD may be at exceptionally high risk for internalizing disorders, including depression, given the odds conferred by diagnostic influences and sex combined. A growing body of research suggests that females with ASD do experience heightened rates of internalizing disorders—anxiety, depression, eating disorders—as compared to males with ASD, who present with more externalizing problems—hyperactivity, inattention [14••, 33,34,35]. Adolescent females with ASD have been found to be at greater risk of developing internalizing disorders compared to neurotypical females and males with ASD [35]. During adolescence, female socialization tends to reflect smaller, more intimate groups with growing affiliative orientation [36] and has been suggested as a possible mechanism to explain the unmasking of relative social skills deficits in adolescent females with ASD, leading to greater isolation and internalizing symptoms [35]. Further, late-diagnosed individuals tend to suffer from co-morbid psychiatric issues, possibly related to a lifetime of stress associated with the need to adapt to daily life in one’s society [13].
Treatment Considerations
Treatment in females with ASD needs to take into account a variety of factors. First, females with ASD are often delayed in receiving a diagnosis, leading to missed opportunities for early intervention, including the treatment of potential psychiatric co-morbidities due to perceptions of feeling unheard and misunderstood in society [14••]. In addition, many have argued that there are increasingly complex social and cultural expectations for females in everyday life compared to their male counterparts. Specifically in the USA, typical expectations for women, also known as feminine gender norms, include the importance of developing caring relationships with others, being involved in romantic relationships, investment in one’s appearance, modesty, sexual fidelity, and responsibility for and enjoyment of domestic chores and childcare [37]. In the typically developing female population, conformity to these feminine norms has been related to depression throughout adolescence [38] and adulthood [39] as it can often feel overwhelming to be expected to value, act “nicely,” and be engaged in a plethora of relationships with family, friends, romantic partnerships, and children [40]. In balancing all of these relationships, it has been hypothesized that women can often set aside their own needs and opinions to instead serve others, which has also been linked to greater symptoms of depression [41, 42]. Our current sociopolitical climate also continues to foster a culture where women are much more likely to be victims of intimate partner abuse, including sexual assault, and violence compared to males [43]. Women with ASD may be even more vulnerable to this victimization given their challenges with social awareness and self-advocacy [44].
While a portion of women with ASD may not be interested in investing in interpersonal relationships and the associated societal expectations, many long for opportunities to build fulfilling and lasting relationships. The abovementioned intricate and complex social expectations for interpersonal relationships, coupled with many women’s experiences of late diagnosis and treatment, could help explain the increased rates of internalizing disorder and sleep difficulties among women with ASD [12]. Therefore, in order to support the overall mental health and well-being of these individuals, evidenced-based treatment should be infused with sociocultural psychoeducation.
Historically, interventions have been aimed, in part, to treat the core social communication deficits and cognitive inflexibility in ASD. As mentioned above, individuals with ASD, particularly those who are aware of their struggles, often experience co-morbid symptoms of anxiety and depression that also require treatment. Cognitive behavioral therapy (CBT) has been widely studied as an evidenced-based intervention to improve both social communication as well as depression and anxiety for both children and adults with ASD, particularly those individuals without intellectual disability (i.e., formerly diagnosed with Asperger’s disorder) [45•, 46].
“Third wave” approaches to CBT, including mindfulness, have also recently been researched among the autistic population. A recent randomized controlled study of mindfulness-based therapy included 42 adults with ASD who were randomized into treatment and control groups. The treatment group consisted of 9 weekly sessions of mindfulness-based therapy with take home practice; participants showed significant decreases in symptoms of depression, anxiety, and rumination as well as increases in overall positive affect [47]. Mindfulness-based therapy can help individuals become more aware of their inner dialog without judgment, while CBT gives one tools to “talk back to” or challenge one’s inner dialog, often confronting self-defeating or negative beliefs and replacing them with more healthy, balanced thoughts.
When exploring one’s inner dialog in treatment, it is important to consider the potential origin of these beliefs. Some women with ASD have had negative experiences with professionals who have denied the presence of their ASD, experienced shame due to their inability to manage their relationships, and/or have become victims of assault leading to negative self-beliefs and a sense of an insecure world. Therefore, women with ASD would benefit from consciousness raising to better understand the sociopolitical climate to ultimately help them untangle societal expectations with their own hopes, dreams, and goals [37]. This could occur through individual discussions; however, it can also be powerful to discuss societal attitudes in group settings to allow women to gain support from and provide validation for one another. As individuals with ASD often benefit from direct teaching and use of visual aids, using examples of societal attitudes in everyday media (e.g., television shows, commercials, magazines) can help aid in and put words to some of their confusing real-life experiences. After awareness has been raised, the next step is for women to openly discuss the benefits and costs of subscribing to these norms in everyday life. This could then inform future CBT and mindfulness-based skill instruction. For example, as women are becoming more aware of their automatic thoughts through mindfulness practice (e.g., “I’m a bad friend”), with consciousness raising they can view their thoughts through a critical lens and decide whether they wish to believe them outright or compassionately hear them and choose a cognitive restructuring strategy to produce an alternative thought (e.g., “Just because I’m too tired to meet my friend for coffee, I’m not a bad friend. She understands that by the end of the day my sensory system is on overdrive and I need to spend some quiet time at home.”)
In addition to this infusion of consciousness raising of feminine norms into more traditional CBT and mindfulness-based treatments, women with ASD also require direct teaching of both self-advocacy and safety skills to navigate their at-risk status for victimization in interpersonal relationships [44]. Additionally, women must also navigate their reproductive health, including the possibility of giving birth to children. Explicit instruction in skills related to caring for one’s menstrual cycle, birth control, and sexually transmitted diseases is also essential, as is working with women to build social awareness and communication skills useful for bonding with their babies. As society tells women that they need to take care of everyone before themselves, explicitly teaching women with ASD the importance of how to engage in self-care practice is essential to their overall well-being and health. Last, in light of recent findings regarding the relationship between ASD and transgender identity [48], particular interventions should also be afforded to those individuals who do not and have no desire to endorse feminine gender norms, as they will experience their own set of challenges in maintaining their overall health and well-being in today’s society.
Pharmacological Interventions
Non-drug, behaviorally oriented treatments have been found to be the most effective intervention for the core symptoms of ASD, especially in younger children. At times, however, maladaptive behaviors and the symptoms associated with psychiatric co-morbidities can lead to distress and impairment above and beyond the core symptom domains of ASD. These behaviors and symptoms can impede progress in educational, vocational, and therapeutic settings and cause significant distress for patients and their families. At these times, the use of pharmacological treatment can result in a significant reduction of interfering maladaptive behaviors and symptoms of psychiatric co-morbidities [49•]. Symptoms that are commonly targeted with pharmacotherapy include inattention, motor hyperactivity, impulsivity, aggression toward others, self-injurious behavior, property destruction, mood swings, depression, anxiety, and sleep disturbance.
To date, data that address sex differences in response to drug treatment for maladaptive behaviors and psychiatric co-morbidities in ASD do not exist. Although males and females with ASD are usually enrolled into larger multisite clinical trials, the sex ratio of participants is typically the same as the prevalence rate of the disorder by sex, approximately 4:1 (males:females) [50]. To examine the sex difference in response to drug treatment in ASD with adequate statistical power, an exorbitant number of study subjects would be needed. Recruitment of adequate numbers of subjects with ASD into randomized controlled trials, even with multiple study sites, can be challenging. Oversampling females for the trial would be necessary to determine if a sex difference existed in response to a particular drug treatment.
Special consideration should be given to the use of certain psychiatric medications in females with ASD. For example, aripiprazole, an atypical antipsychotic that is approved by the Food and Drug Administration for treating irritability in children and adolescents with ASD, is the only commonly used atypical antipsychotic that does not cause hyperprolactinemia [51]. Most antipsychotics block the dopamine 2 receptor, which results in a significant increase in prolactin. Aripiprazole is a partial agonist at the dopamine 2 receptor, which actually results in decreased prolactin levels. Increased levels of prolactin can cause swelling of the breasts (gynecomastia) and lactation (galactorrhea). While these side effects can occur in males, they may be more problematic and distressing when they occur in females. Valproic acid, which is often used to treat mood swings or co-morbid bipolar disorder in patients with ASD (as well as seizures), can cause polycystic ovary syndrome in females of child-bearing age. Polycystic ovary syndrome is associated with anovulation resulting in irregular or absent menstrual cycles, infertility, excess facial or body hair, obesity, ovarian cysts, heart disease, and diabetes with insulin resistance [52]. Finally, some medications used to treat persons with ASD can lower the effectiveness of birth control pills and make the individual more likely to become unexpectedly pregnant. These include modafinil, which is sometimes used to treat co-morbid ADHD, the anticonvulsants carbamazepine, lamotrigine and topiramate, and St. John’s Wart, an herbal compound sometimes used to treat depression.
Quality of Life
Although the severity of some ASD symptoms appears to decline with increasing age, adults with ASD generally never reach typical levels of social functioning. There have been very few studies to date that have looked at social and quality of life (QoL) outcomes in adults with ASD, [53, 54] and even fewer have examined differences between men and women [55]. In the largest study to date to examine QoL, Mason and colleagues (2018) confirmed previous work that individuals with ASD report lower QoL than the neurotypical population [56•]. Further, the main characteristics that were predictive of lower QoL were female gender, severity of ASD symptoms, and having a current mental health diagnosis. However, while previous work has also found QoL to be lower in females, there are mixed findings regarding the social domain of QoL, with Mason and colleagues finding slightly higher satisfaction in social QoL for females. This was suggested to be a reflection of females with ASD being more socially motivated and able to maintain friendships.
Conclusions
Growing research supports gender specificity in core ASD symptoms; however, many gaps in the evidence base, particularly around diagnosis and behavioral descriptors, remain to be addressed. Evidence to date suggests that women are commonly being undiagnosed or misdiagnosed based on descriptors that were developed from the behavioral presentation of males. Much of the work to date trying to understand the etiology of ASD has continued to be influenced by this gender bias. As such, the evidence is mixed with respect to prevalence rates. Most of the existing research has demonstrated that intelligence appears to modulate the male-to-female ratio, with more recent research suggesting that studies using “passive” ascertainment methods likely overestimate the male-to-female ratio and leave out a subset of females, who despite having clinically significant symptoms, are not being diagnosed. Further, more recent research indicates that gender differences in symptom presentation across diagnostic criteria also affect prevalence rates.
Evidence regarding sex-related differences in brain function and structure has been less consistent. While there is ample research that shows differences in executive functioning in individuals with ASD, these studies often excluded women or had only small, uneven samples of women. The few studies that have examined gender have shown mixed and, at times, conflicting results. There is some evidence to suggest that women with ASD display worse working memory and better word generation than men with ASD, although these performances are mediated by intelligence and may merely reflect gender differences observed in neurotypical persons. There does appear, however, to be slightly more support for possible differences in structure and connectivity than function.
Considerable evidence does exist demonstrating different rates of co-morbid disorders between adolescent and adult women with ASD compared to their male counterparts. Females consistently show higher rates of internalizing disorders, particularly anxiety, depression, and eating disorders, with age of diagnosis being an important moderator. These differences in presentation have important implications for treatment. Given the higher rate of missed and delayed diagnosis, females are more likely to miss opportunities for early intervention. Sociocultural factors including social expectations for women have often contributed to a climate that leaves women with ASD more likely to feel shame regarding their social or behavioral difficulties or fall victim to various forms of violence. As such, treatment targeting women with ASD will require more direct teaching in self-advocacy and safety skills. Data regarding sex differences in ASD in response to drug treatment is essentially non-existent, which is concerning given the differences in psychiatric co-morbidities between males and females. Ultimately, more research investigating the differences between men and women with ASD with regard to both diagnosis and treatment is essential for us in order to serve this growing population better.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association, American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, D.C: American Psychiatric Association; 2013.
Asperger H. Die “autistichen psychopathen” im kindersalter [Autistic psychopathy in childhood]. Archive fur Psychiatrie und Nervenkrankheiten. 1944;117:76–136.
Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217.
Ritvo ER, Cantwell D, Johnson E, Clements M, Benbrook F, Slagle S, et al. Social class factors in autism. J Autism Dev Disord. 1971;1:297–310.
Rutter M, Lockyer L. A five to fifteen year follow-up study of infantile psychosis: I. Description of sample. Br J Psychiatry. 1967;113:1169–82.
Lotter V. Epidemiology of autistic conditions in young children. Soc Psychiatry. 1966;1:124–35.
Fombonne E. The changing epidemiology of autism. J Appl Res Intellect Disabil. 2005;18:281–94.
Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet. 2006;368:210–5.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
• Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 Sites, United States, 2014. MMWR Surveill Summ. 2018;67:1–23 A very recent study examining the prevalence rate of ASD in a population cohort in London.
•• Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism Spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56:466–74 A systematic review and meta-analysis of prevalence studies examining the male-to-female ratio in ASD.
Kreiser NL, White SW. ASD in females: are we overstating the gender difference in diagnosis? Clin Child Fam Psychol Rev. 2014;17:67–84.
Lai M-C, Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions- ClinicalKey. Lancet Psychiatry. 2015;2:1013–27.
•• Bargiela S, Steward R, Mandy W. The experiences of late-diagnosed women with autism spectrum conditions: an investigation of the female autism phenotype. J Autism Dev Disord. 2016;46:3281–94 A qualitative study examining the female ASD phenotype and its effect on diagnosis.
Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. J Am Acad Child Adolesc Psychiatry. 2013;52:572–581.e1.
• Hull L, Petrides KV, Allison C, Smith P, Baron-Cohen S, Lai M-C, et al. “Putting on my best normal”: social camouflaging in adults with autism spectrum conditions. J Autism Dev Disord. 2017;47:2519–34 Qualitative study using thematic analysis to examine social camouflaging in adults with ASD and focusing on the nature, motivations, and consequences of camouflaging.
•• Lai M-C, Lombardo MV, Ruigrok AN, Chakrabarti B, Auyeung B, Szatmari P, et al. Quantifying and exploring camouflaging in men and women with autism. Autism. 2017;21:690–702 A quantitative analysis of camouflaging in ASD confirms gender disparities with women reporting greater camouflaging.
• Lai M-C, Lombardo MV, Pasco G, Ruigrok ANV, Wheelwright SJ, Sadek SA, et al. A behavioral comparison of male and female adults with high functioning autism spectrum conditions. PLoS ONE. 2011 [cited 2018 Jul 3];6. Available from: http://ezp-prod1.hul.harvard.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2011-14242-001&site=ehost-live&scope=site. A behavioral comparison between sexes found women with high-functioning ASD to show more lifetime sensory symptoms, fewer socio-communication difficulties, and more self-reported autistic traits.
Lehnhardt F-G, Falter C, Gawronski A, Pfeiffer K, Tepest R, Franklin J, et al. Sex-related cognitive profile in autism spectrum disorders diagnosed late in life: implications for the female autistic phenotype. J Autism Dev Disord. 2016;46:139–54.
Koyama T, Kamio Y, Inada N, Kurita H. Sex Differences in WISC-III profiles of children with high-functioning pervasive developmental disorders. J Autism Dev Disord. 2009;39:135–41.
Bölte S, Duketis E, Poustka F, Holtmann M. Sex differences in cognitive domains and their clinical correlates in higher-functioning autism spectrum disorders. Autism. 2011;15:497–511.
• Kiep M, Spek AA. Executive functioning in men and women with an autism spectrum disorder. Autism Res. 2017;10:940–8 This study demonstrated differences in executive functioning between men and women with ASD and discussed possible implications.
Hill EL. Evaluating the theory of executive dysfunction in autism. Dev Rev. 2004;24:189–233.
Lai M-C, Lombardo MV, Suckling J, Ruigrok ANV, Chakrabarti B, Ecker C, et al. Biological sex affects the neurobiology of autism. Brain. 2013;136:2799–815.
Alaerts K, Swinnen SP, Wenderoth N. Sex differences in autism: a resting-state fMRI investigation of functional brain connectivity in males and females. Soc Cogn Affect Neurosci. 2016;11:1002–16.
Beacher FDCC, Radulescu E, Minati L, Baron-Cohen S, Lombardo MV, Lai M-C, et al. Sex differences and autism: brain function during verbal fluency and mental rotation. PLoS One; San Francisco. 2012;7:e38355.
Beacher FD, Minati L, Baron-Cohen S, Lombardo MV, Lai M-C, Gray MA, et al. Autism attenuates sex differences in brain structure: a combined voxel-based morphometry and diffusion tensor imaging study. Am J Neuroradiol. 2012;33:83–9.
Baron-Cohen S. The extreme male brain theory of autism. Trends Cogn Sci. 2002;6:248–54.
Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism Spectrum disorders: a comparative study. J Autism Dev Disord. 2013;43:1314–25.
Lugnegård T, Hallerbäck MU, Gillberg C. Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Res Dev Disabil. 2011;32:1910–7.
Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–43.
Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: frequency and association with core autism symptoms and cognitive functioning. J Abnorm Child Psychol. 2008;36:117–28.
May T, Cornish K, Rinehart N. Does gender matter? A one year follow-up of autistic, attention and anxiety symptoms in high-functioning children with autism Spectrum disorder. J Autism Dev Disord. 2014;44:1077–86.
Mandy W, Chilvers R, Chowdhury U, Salter G, Seigal A, Skuse D. Sex Differences in autism spectrum disorder: evidence from a large sample of children and adolescents. J Autism Dev Disord. 2012;42:1304–13.
Solomon M, Miller M, Taylor SL, Hinshaw SP, Carter CS. Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. J Autism Dev Disord. 2012;42:48–59.
Larson R, Richards MH. Introduction: the changing life space of early adolescence. J Youth Adolesc. 1989;18:501–9.
Mahalik JR, Morray EB, Coonerty-Femiano A, Ludlow LH, Slattery SM, Smiler A. Development of the conformity to feminine norms inventory. Sex Roles. 2005;52:417–35.
Barrett AE, Raskin WH. Trajectories of gender role orientations in adolescence and early adulthood: a prospective study of the mental health effects of masculinity and femininity. J Health Soc Behav. 2002;43:451–68.
Broderick PC, Korteland C. Coping style and depression in early adolescence: relationships to gender, gender role, and implicit beliefs. Sex Roles. 2002;46:201–13.
Fiese BH, Skillman G. Gender differences in family stories: moderating influence of parent gender role and child gender. Sex Roles. 2000;43:267–83.
Danielsson UE, Bengs C, Samuelsson E, Johansson EE. “My greatest dream is to be normal”: the impact of gender on the depression narratives of young Swedish men and women. Qual Health Res. 2011;21:612–24.
Tolman DL, Impett EA, Tracy AJ, Michael A. Looking good, sounding good: femininity ideology and adolescent girls’ mental health. Psychol Women Q. 2006;30:85–95.
Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women. 2000;6:142–61.
Safety Skills for Asperger Women: How to Save a Perfectly Good Female Life by Liane Holliday Willey [Internet]. [cited 2018 Jul 31]. Available from: https://www.goodreads.com/book/show/11187137-safety-skills-for-asperger-women.
• Wood JJ, Klebanoff S, Renno P, Fujii C, Danial J. Chapter 7 - Individual CBT for anxiety and related symptoms in children with autism spectrum disorders. In: Kerns CM, Renno P, Storch EA, Kendall PC, Wood JJ, editors. Anxiety in Children and Adolescents with Autism Spectrum Disorder [Internet]. Academic Press; 2017 [cited 2018 Jul 31]. p. 123–41. Available from: http://www.sciencedirect.com/science/article/pii/B9780128051221000077 A chapter reviewing the effectiveness of CBT therapy in treating both children and adults with ASD.
Spain D, Blainey SH, Vaillancourt K. Group cognitive behaviour therapy (CBT) for social interaction anxiety in adults with autism spectrum disorders (ASD). Res Autism Spectr Disord. 2017;41–42:20–30.
Spek AA, van Ham NC, Nyklíček I. Mindfulness-based therapy in adults with an autism spectrum disorder: a randomized controlled trial. Res Dev Disabil. 2013;34:246–53.
Jones RM, Wheelwright S, Farrell K, Martin E, Green R, Di Ceglie D, et al. Brief report: female-to-male transsexual people and autistic traits. J Autism Dev Disord. 2012;42:301–6.
• Accordino RE, Kidd C, Politte LC, Henry CA, McDougle CJ. Psychopharmacological interventions in autism spectrum disorder. Expert Opin Pharmacother. 2016;17:937–52 Opinion piece on psychopharmacological treatment of core and associated symptoms of ASD.
McCracken JT, McGough J, Shah B, Cronin P, Hong D, Aman MG, et al. Risperidone in children with autism and serious behavioral problems. N Engl J Med. 2002;347:314–21.
Owen R, Sikich L, Marcus RN, Corey-Lisle P, Manos G, McQuade RD, et al. Aripiprazole in the treatment of irritability in children and adolescents with autistic disorder. Pediatrics. 2009;124:1533–40.
Pasquali R, Stener-Victorin E, Yildiz BO, Duleba AJ, Hoeger K, Mason H, et al. PCOS Forum: research in polycystic ovary syndrome today and tomorrow. Clin Endocrinol. 2011;74:424–33.
Oswald TM, Winder-Patel B, Ruder S, Xing G, Stahmer A, Solomon M. A pilot randomized controlled trial of the ACCESS program: a group intervention to improve social, adaptive functioning, stress coping, and self-determination outcomes in young adults with autism spectrum disorder. J Autism Dev Disord. 2018;48:1742–60.
Farley M, Cottle KJ, Bilder D, Viskochil J, Coon H, McMahon W. Mid-life social outcomes for a population-based sample of adults with ASD. Autism Res. 2018;11:142–52.
Kamio Y, Inada N, Koyama T. A nationwide survey on quality of life and associated factors of adults with high-functioning autism spectrum disorders. Autism. 2013;17:15–26.
• Mason D, McConachie H, Garland D, Petrou A, Rodgers J, Parr JR. Predictors of quality of life for autistic adults. Autism Research [Internet]. [cited 2018 Sep 23];0. Available from: http://onlinelibrary.wiley.com/doi/abs/10.1002/aur.1965 This study includes the largest study sample to date examining the quality of life of individuals with ASD and examines gender differences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Autism Spectrum Disorders: Treatment, Services, Outcomes, and Community Functioning in Adolescents and Adults
Rights and permissions
About this article
Cite this article
Green, R.M., Travers, A.M., Howe, Y. et al. Women and Autism Spectrum Disorder: Diagnosis and Implications for Treatment of Adolescents and Adults. Curr Psychiatry Rep 21, 22 (2019). https://doi.org/10.1007/s11920-019-1006-3
Published:
DOI: https://doi.org/10.1007/s11920-019-1006-3