Abstract
Purpose of Review
This review aims to give an overview on the current literature on sex differences in personality disorders and to highlight the potential of dimensional approaches.
Recent Findings
Empirical findings on sex differences in personality disorders are inconsistent and appear to be highly dependent on study settings. Current studies have mainly focused on borderline and antisocial personality disorder and the question whether these are sex-specific representations of a common substrate. In general, sexes differ in the manifestation of personality disorders as well as in comorbidities. Criticism of the established categorical model led to an additional dimensional model of personality disorders in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Summary
Investigations on sex differences in personality disorders are sparse and mainly limited to antisocial and borderline personality disorder. The introduction of a dimensional model offers the chance to re-think the construct of “personality disorder” and thereby also opens the possibility for a better understanding of sex differences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Personality disorders (PDs) belong to the “most severe” psychiatric diagnoses. Resulting impairments are not a temporary phenomenon. They are not limited to specific domains but apply to one’s personality itself. PDs are suggested to represent one end of the continuum of personality traits and are characterized by their enduring pattern of inflexible and inadequate inner experiences and behaviors. Beginning from adolescence or early adulthood on, they lead to severe impairments in relationships or working life [1].
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and based on the results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), around 15% of US adults suffer from at least one PD. Cross-national data estimate a prevalence of 6% [2]. This makes PDs a common phenomenon with severe consequences for patients and relatives as well as in terms of economic burden [3].
Other than the International Classification of Diseases (ICD), DSM-5 and its precursors subdivide PDs in three clusters: cluster A represents disorders with odd or eccentric behavior (prevalence 5.7%); cluster B includes dramatic, emotional, or erratic behavior (1.5%); and cluster C includes anxious or fearful behavior (prevalence 6.0%).
An ongoing topic of discussion in scientific research as well as in the general population is if there are differences in personality between sexes. Women are generally perceived as not only more emotional and neurotic than men but also more agreeable, while a male sex is associated with more assertive behavior [4, 5]. It is assumed that sex differences in personality traits in the general population are also reflected in the sex ratio of PDs [6, 7]. Indeed, some PDs are historically seen as “typically female” (borderline, histrionic, dependent) and some are suggested to be rather “male” (antisocial, paranoid) [8].
Table 1 depicts sex ratios and sex-related diagnostic issues in PDs reported in DSM-5. According to DSM-5, some of them indeed are more often diagnosed in one sex than the other (borderline PD in females and antisocial PD in males), while other PDs only differ “slightly” in their sex ratio. However, results depend highly on the study population and methods used and prevalence data on sex differences from other studies differ from sex ratios reported in DSM-5 [9, 10].
Prevalence differences seem to be additionally influenced by a diagnostic bias of clinicians to over- or underdiagnose specific PDs due to social and gender stereotypes [1, 11,12,13]. This has led to a specific note in DSM-5 stating that “Although these differences in prevalence probably reflect real gender differences in the presence of such patterns, clinicians must be cautious not to overdiagnose or underdiagnose certain personality disorders in females or in males (…).” Furthermore, it was pointed out that the DSM working groups have been predominately male (in the DSM-5 working group for example, 82% of contributors were male) and that diagnostic criteria might therefore be shaped by a masculine perspective [14].
Antisocial and borderline PD exhibit the largest differences in sex ratios. The majority of publications on pubmed.gov are also focusing on borderline and antisocial PD. The unbalanced number of publications might lead to a biased picture towards these PDs.
Summing up, results on sex differences in PDs are inconsistent and depend on study population as well as potential diagnostic biases. Prevalence differences between sexes are most prominent in antisocial and borderline PD.
Borderline Personality Disorder
DSM-5 states that borderline PD is a predominately “female” PD with a sex ratio of 3:1. Other studies report no sex differences in prevalence [9, 15]. These opposing results have been subject of multiple discussions. One explanation for the discrepancy is that the higher number of women with borderline PD is due to an increased seeking of treatment in females. This might have led to a selection bias of many studies conducted in clinical settings, as non-clinical samples tend to report less biased ratios [9, 16].
Apart from prevalence, it is of interest if and how borderline PD is differently expressed in males and females. According to a psychometric investigation using Item Response Theory, women are more likely to experience a chronic feeling of emptiness, suicidal behavior, self-mutilation, and affective instability while men are more likely to endorse impulsivity [17]. Others, however, argue that existing sex-related differences in borderline PD are rather small and restricted to a higher likelihood in women to engage in sexually abusive relationships [16]. One study even reported that the gender gap which is present in the normal population with respect to aggression, rates of substance abuse, major depression and PTSD seems to diminish in borderline patients with more similar levels in females and males [18•].
While 74% of borderline patients are assumed to be diagnosed with a second axis II PD [19], the subtype differs between sexes. Women mostly suffer from comorbid dependent PD, while in men, antisocial PD seems to be the most common comorbid PD [18•, 19].
Hence, despite the number of studies in borderline PD, sex-specific aspects have not been addressed sufficiently and it is still inconclusive to what extent prevalence differences as well differences in symptoms occur between the sexes.
Antisocial Personality Disorder
Most studies on antisocial PD have been conducted in men only, which is why we know relatively little how sex differences manifest here [20, 21].
A systematic review in 23,000 prisoners in 12 countries revealed that prisoners are ten times more likely to fulfill diagnostic criteria of an antisocial PD [22]. These numbers differ between men and women: Nearly 50% of male prisoners are diagnosed with antisocial PD, while “only” 20% of women have antisocial PD. The ratio in the general population of males and females with antisocial PD is 3:1 and accounts thereby for one of the most striking sex differences in PDs [23]. However, these numbers are questioned due to the following reasons: The less violent nature of antisocial PD in females (missing school/work), the lower number of committed antisocial acts that involve the police as well as higher emotionality than their male counterparts are thought to contribute to a lower prevalence of antisocial PD in women [20, 23, 24]. Moreover, women with antisocial PD tend to exhibit a higher number of symptoms and an increased severity which led to the “threshold of risk hypothesis”: This hypothesis states that women have a higher threshold to manifest antisocial PD, explaining that there may be a minority of antisocial females but those with the manifest disorder are characterized by an even more pronounced symptom pattern [23, 25].
A nationwide study including more than 1200 participants with antisocial PD revealed that sex differences relate to diverse preceding influencing factors: Women with antisocial PD report more childhood neglect, sexual and emotional abuse, as well as other adverse events during childhood and adulthood. Hence, they experience a higher level of victimization and lower support than men [20].
Sex differences are additionally based on diverse developmental trajectories: Already during childhood, boys manifest more externalizing impairments such as attention deficit disorder and conduct disorder, while girls develop more internalizing symptoms such as anxiety and affective symptoms. Criteria of antisocial PD and conduct disorder (the childhood precursor) reflect these developmental sex differences and trait profiles. Also, one of the most characteristic features of antisocial PD, impulsive aggression, is generally more common in men [6, 7].
Women and men with antisocial PD also differ in their comorbidities: Females with antisocial PD have higher rates of comorbid histrionic and borderline PD as well as comorbid mood disorders, while cocaine use disorder is more prevalent in male antisocial PD [20]. Both sexes have a high comorbidity for alcohol abuse.
Sex differences in antisocial PD are moreover reflected in different neural structures [26]. Middle and orbito-frontal volume reductions have been associated with more antisocial PD symptoms and crime perpetration in both males and females. However, males had smaller orbitofrontal and middle frontal gray matter volumes compared to females. Controlling for these differences in brain volume lowered the sex difference in the strength of antisocial personality and behavior by 77%. In men, significant interactions between the serotonin system and testosterone could be additionally linked to aggressive and impulsive behavior [27].
Summing up, established prevalence differences in antisocial PD are at least partly influenced by a less overt manifestation of symptoms in females as well as different developmental trajectories. Literature reports sex-specific comorbidities as well as different biological markers.
A Comparison of Borderline and Antisocial PD
Antisocial and borderline PDs have frequently been discussed as two sides of the same coin [28]. They are both cluster B PDs and their co-occurrence varies between 6 and 57%, depending on the setting [29•]. The PDs share many similarities (e.g., impulsivity, a much higher suicide risk than in the general population), and some researchers suggest a common underlying etiology. However, they differ largely in their prevalence in males and females. Moreover, borderline PD emphasizes affective symptoms (such as emotional instability and identity problems), while antisocial PD is further characterized by delinquent and non-normative behavior. Nevertheless, there is some evidence for a common core in genetics and environmental factors [30, 31].
Chun and colleagues investigated whether the high comorbidity is based on the same underlying construct by fitting factor analysis models to the covariance of borderline and antisocial PD indicators [29•]. The results suggested a two factor structure with disorder-specific factors as well as a common factor for both disorders with the latter factor explaining a large part of variance (60–66%). Results thereby support the notion of a common basis. Beauchaine’s conceptual work outlines an all-embracing model of the interaction between biology, sex, and environment in borderline and antisocial PD [32]. It points out that environmental factors such as traumatic experiences and disturbed attachment, as well as biological factors interact synergistically. Compromised central serotonergic and dopamine functioning in both PDs might be responsible for a heritable trait impulsivity, which in turn interacts with environmental factors. Sex differences are explained by a gene × sex interaction which results in a different behavior in males (externalizing) and females (internalizing behavior). Both PDs are additionally linked to functional abnormalities in orbitofrontal and anterior cingulate areas which might explain constraints in executive functioning and planning [32].
However, other researchers argue against the idea of one united syndrome and even reconsider earlier conclusions. Paris (2013), for example, suggests that the differences in DSM-5 diagnosis are based on different trait dimensions which are influenced by sex [28]. According to him, focus should be set on biological markers as a tool to separate these disorders, which share common risk factors. This debate is not over yet, and future studies are expected to shed further light on this question.
Lastly, according to some authors, men with borderline PD might be misdiagnosed with antisocial PD due to additional antisocial features in men with borderline PD [20, 33, 34].
Interestingly, 15 years ago, histrionic and antisocial PD were discussed to be the sex-specific manifestations of psychopathy [35]. Results of comparing their inhibition abilities did, however, not speak in favor of a common underlying disorder construct.
Other Personality Disorders
Findings regarding the other PDs are scarce. Literature on sex differences in these PDs is either quite old or focuses on very specific domains:
Paranoid Personality Disorder
Paranoid PD is one of the most common PDs with a prevalence in the range between 1.2 and 4.4% [10]. Clinical samples find higher rates of men, whereas epidemiological findings report a higher rate of women [10]. The reliability and validity of the concept of paranoid PD, however, were questioned repeatedly, which probably accounts for the sparse published literature [36]. It led to the suggestion to remove this disorder from the DSM.
Schizotypal Personality Disorder
While DSM-5 reports that schizotypal PD is slightly more common in males, other results suggest that lifetime prevalence of schizotypal PD is higher in females than in males (4.2% vs 3.9%) [1, 37]. A meta-analysis points out that schizotypal PD is differently expressed in males and females: Men score higher than women on “negative” features of schizotypal personality which seems to be a cross-cultural effect [38, 39]. Some studies report that women additionally tend to show more “positive” symptoms [40,41,42]. Sex-specific patterns of axis I comorbidities include more bipolar disorders, panic disorders, specific phobia, generalized anxiety disorders, and PTSD in women. The most prevalent comorbidities in males are alcohol abuse and dependence. Males with schizotypal PD are more likely to be additionally diagnosed with antisocial PD, while women with schizotypal PD manifest more frequently comorbid paranoid PD [37].
Schizoid Personality Disorder
The concept of schizoid PD was also questioned repeatedly and suggested to be removed from the DSM [43, 44]. Some criticize that symptoms largely overlap with Asperger’s syndrome [43]. In a clinical sample, more males than females fulfilled the criteria for a schizoid PD [43].
Histrionic Personality Disorder
According to NESARC, men and women share the same risk for histrionic PD [10]. Reported prevalence differences are often discussed in terms of diagnostic bias and less representative symptom presentation in males [45].
Narcissistic Personality Disorder
Lifetime prevalence of narcissistic PD was reported to be higher in males than in females [1, 46]. In men, narcissistic PD is associated with a higher prevalence of mental disability. Men with narcissistic PD have higher rates of alcohol abuse and dependence as well as any other drug use disorder and are more likely to be additionally diagnosed with antisocial PD. Females with narcissistic PD are suffering more frequently from depressive and anxiety disorders (except social phobia and panic disorder without agoraphobia) and are more likely to have comorbid borderline PD [46]. Sex differences were also reported in “subclinical” narcissistic individuals with women and men showing opposite results in the brain’s default mode and the task positive network [47]. Moreover, men have to show higher trait levels than women in order to be endorsed for the criterion “need for admiration” [48].
Avoidant Personality Disorder
Prevalence of avoidant PD ranges around 2.6%. Other than stated in the DSM-5, some report that the prevalence in females is higher than in males (prevalence of 2.8% in females compared to 1.2% in males) [10]. As one of the sparse findings, biological sex-specific markers have also been reported: Females but not males with avoidant PD have an increased sympathetic reaction to electric stimulation stress which co-occurs with heightened salivary cortisol responses [49], pointing to a heightened stress response in males with avoidant PD.
Dependent Personality Disorder
DSM-5 reports that the sex ratio for dependent PD is higher in females, at least in clinical settings (prevalence in females according to NESARC 0.6% vs in males 0.4%) [10]. According to Bornstein (1996), this might be explained in part by men’s unwillingness to “admit” dependent feelings, attitudes, and behaviors [50].
Obsessive-Compulsive Personality Disorder
Some evidence exists for an unbalanced sex ratio in obsessive-compulsive PD, with more males suffering from this PD [51]. This fits to the reported ratio in DSM-5 with men affected twice as often as women [1]. Other studies, however, reported equal rates for both sexes [52]. Males with obsessive-compulsive PD manifest a decreased parasympathetic activity and increased salivary amylase and cortisol responses upon social stress, while women do not [53].
Reported studies fail to draw a coherent picture regarding sex differences in prevalence rates as well as sex-specific symptom expression, biomarkers, and comorbidities.
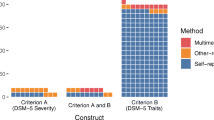
Outlook—Dimensional Approaches
DSM-5 states and it is commonly accepted that PDs are the “severe” forms of personalities [1]. Therefore, many argue that PDs may be better stated in a dimensional mode. The validity and reliability of the present cluster structure, which is according to DSM-5 based on descriptive similarities, were questioned repeatedly: Some argue that PD subtypes lack a research-based foundation (e.g., in schizoid PD) [44]. Furthermore, PDs have heterogeneous symptom profiles; therefore, within the current diagnostic approach one diagnosis can comprise a combination of many different symptoms. All the arguments indicate a dissatisfaction with the current system. DSM-5 picked up this criticism and proposed next to the “classic” approach of clusters A, B, and C, a dimensional research model. This reflects “the decision of the APA Board of Trustees to preserve continuity with current clinical practice, while also introducing a new approach that aims to address numerous shortcomings of the current approach to personality disorder.” [1, 54] The new approach characterizes impairments in individual functioning and pathological personality traits. The diagnoses are based on antisocial, avoidant, borderline, narcissistic, obsessive-compulsive, and schizotypal PD. It additionally includes the diagnosis “personality disorder-trait specified” which can be used if criteria for a specific PD are not met. The upcoming ICD-11 suggests in its proposal even more drastic changes such as to delete all specific types of PDs and put the focus on the severity of disturbances in interpersonal functioning. Traits appear to be secondary qualifiers [55•]. It is assumed that these changes regarding the established categorical classification will lead to a new approach in understanding PDs, which will hopefully be followed by new research advances. It is to wait if and how a dimensional model will focus on and reveal sex differences in prevalence and diagnosis, but it certainly poses a new chance.
Conclusion
Summing up, the current literature still mainly focuses on borderline and antisocial PD and their potential common core. Reasons for and against a common substrate are discussed. Sex differences in other PDs remain underinvestigated and are therefore underrepresented in the current literature.
From the current point of view, there is some evidence for sex differences in manifestation and comorbidities in PDs. Reported differences in prevalence seem to highly depend on the setting and methods. Sex-specific prevalence differs from study to study. PDs with stable findings of sex differences would benefit from the definition of sex-specific symptom profiles as well as the development of different treatment programs for males and females in order to address specific deficits and needs.
For now, it cannot be ensured that diagnoses and treatments are unaffected by sex-specific stereotypes. This might lead to false assumptions such that, e.g., a borderline diagnosis has to go along with affective instability and self-mutilation, though these are symptoms predominantly present in female patients.
Future research should follow two lines: First, research on the sparsely investigated PDs should be intensified to reliably understand how sexes differ in prevalence, manifestation, and therapeutic outcome of PDs. Second, it would be of special interest to follow up on borderline and antisocial PD as sex differences in these PDs have been replicated consistently. These disorders, therefore, could help understanding sex-specific alterations and communalities on social and emotional functioning [56, 57]. Studying borderline patients, Herpertz et al. showed that men with borderline PD tend to experience higher arousal by social rejection and tend to be more aggressive than women [58•]. Women with borderline PD seem to be more successful than their male counterpart in top-down behavioral control while imagining to act aggressively. Extending our knowledge on sex differences thereby helps developing sex-sensitive treatment programs: While females with borderline PD would benefit from a therapy focusing on strategies on affective instability, men might profit to a higher degree from a therapeutic focus on impulsivity and emotion-regulation skills.
Last but not least, the Research Domain Criteria (RDoC) define dimensional psychological constructs to higher-level domains of human behavior and functioning and could thereby serve as an alternative approach to investigate certain constructs (e.g., social communication) for their differential sex-specific contribution to psychopathology in PDs [59]. Altogether, new developments are expected with regard to upcoming dimensional approaches of PDs and will certainly change the current status quo as well as revive discussions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Association AP. Personality disorders. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC; 2013.
Huang Y, Kotov R, de Girolamo G, Preti A, Angermeyer M, Benjet C, et al. DSM-IV personality disorders in the WHO World Mental Health Surveys. Br J Psychiatry. 2009;195(1):46–53.
Soeteman DI, Hakkaart-van Roijen L, Verheul R, Busschbach JJV. The economic burden of personality disorders in mental health care. J Cli Psychiatry [Peer Reviewed]. 2008;69(2):259–65.
Feingold A. Gender differences in personality: a meta-analysis. Psychol Bull. 1994;116(3):429–56.
Costa PT, Jr., Terracciano A, McCrae RR. Gender differences in personality traits across cultures: robust and surprising findings. J Pers Soc Psychol. [Peer Reviewed]. 2001;81(2).
Paris J. An overview on gender, personality and mental health. Personal Ment Health. 2007;1(1):14–20.
Paris J. Gender differences in personality traits and disorders. Curr Psychiatry Rep. 2004 Feb;6(1):71–4.
Corbitt EM, Widiger TA. Sex differences among the personality disorders: an exploration of the data. Fal, 1995. Clin Psychol Sci Pract. [Peer Reviewed]. 1995;2(3).
Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry [Peer Reviewed]. 2001;58(6):590–6.
Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan W, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2004;65:948–58.
Crosby JP, Sprock J. Effect of patient sex, clinician sex, and sex role on the diagnosis of antisocial personality disorder: models of underpathologizing and overpathologizing biases. J Clin Psychol. 2004;60(6):583–604.
Ford MR, Widiger TA. Sex bias in the diagnosis of histrionic and antisocial personality disorders. J Consult Clin Psychol. 1989;57(2):301–5.
Braamhorst W, Lobbestael J, Emons WHM, Arntz A, Witteman CLM, Bekker MHJ. Sex bias in classifying borderline and narcissistic personality disorder. J Nerv Ment Dis. 2015;203:804–8.
Disney KL. Dependent personality disorder: a critical review. Clin Psychol Rev. 2013;33:1184–96.
Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:533–45.
Sansone RA, Wiederman MW. Sex and age differences in symptoms in borderline personality symptomatology. Int J Psychiatry Clin Pract. 2014;18:145–9.
Hoertel N, Peyre H, Wall MM, Limosin F, Blanco C. Examining sex differences in DSM-IV borderline personality disorder symptom expression using Item Response Theory (IRT). J Psychiatr Res. 2014;59:213–9.
• Silberschmidt A, Lee S, Zanarini M, Schulz SC. Gender differences in borderline personality disorder: results from a multinational, clinical trial sample. J Personal Disord. 2015;29:828–38 This recent study finds that gender differences converge in borderline PD.
Barrachina J, Pascual JC, Ferrer M, Soler J, Rufat MJ, Andión O, et al. Axis II comorbidity in borderline personality disorder is influenced by sex, age, and clinical severity. Compr Psychiatry. 2011;52:725–30.
Sher L, Siever LJ, Goodman M, McNamara M, Hazlett EA, Koenigsberg HW, et al. Gender differences in the clinical characteristics and psychiatric comorbidity in patients with antisocial personality disorder. Psychiatry Res. 2015;229:685–9.
Cale EM, Lilienfeld SO. Sex differences in psychopathy and antisocial personality disorder: a review and integration. Clin Psychol Rev. 2002;22:1179–207.
Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet. 2002;359:545–50.
Alegria AA, Blanco C, Petry NM, Skodol AE, Liu SM, Grant B, et al. Sex differences in antisocial personality disorder: results from the National Epidemiological Survey on Alcohol and Related Conditions. Personality Disorders: Theory, Research, and Treatment. 2013;4:214–22.
Rogstad JE, Rogers R. Gender differences in contributions of emotion to psychopathy and antisocial personality disorder. Clin Psychol Rev. 2008;28:1472–84.
Yang M, Coid J. Gender differences in psychiatric morbidity and violent behaviour among a household population in Great Britain. Soc Psychiatry Psychiatr Epidemiol. 2007;42:599–605.
Raine A, Yang Y, Narr KL, Toga AW. Sex differences in orbitofrontal gray as a partial explanation for sex differences in antisocial personality. Mol Psychiatry. 2011;16:227–36.
Kuepper Y, Alexander N, Osinsky R, Mueller E, Schmitz A, Netter P, et al. Aggression—interactions of serotonin and testosterone in healthy men and women. Behav Brain Res. 2010;206:93–100.
Paris J, Chenard-Poirier MP, Biskin R. Antisocial and borderline personality disorders revisited. Compr Psychiatry. 2013;54:321–5.
• Chun S, Harris A, Carrion M, Rojas E, Stark S, Lejuez C, et al. A psychometric investigation of gender differences and common processes across borderline and antisocial personality disorders. J Abnorm Psychol. 2017;126:76–88 This study examines the potential overlap between borderline and antisocial PD.
Hunt E, Bornovalova MA, Patrick CJ. Genetic and environmental overlap between borderline personality disorder traits and psychopathy: evidence for promotive effects of factor 2 and protective effects of factor 1. Psychol Med. 2015;45:1471–81.
Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am J Psychiatr. 2011;168(1):29–39.
Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: a biology × sex × environment interaction model of antisocial and borderline traits. Dev Psychopathol. 2009;21:735–70.
Sansone RA, Sansone LA. Gender patterns in borderline personality disorder. Innov Clin Neurosci. 2011;8(5):16–20.
Banzhaf A, Ritter K, Merkl A, Schulte-Herbrüggen O, Lammers C-H, Roepke S. Gender differences in a clinical sample of patients with borderline personality disorder. J Personal Disord. 2012;26:368–80.
Cale EM, Lilienfeld SO. Histrionic personality disorder and antisocial personality disorder: sex-differentiated manifestations of psychopathy? J Personal Disord. 2002;16:52–72.
Triebwasser J, Chemerinski E, Roussos P, Siever LJ. Paranoid personality disorder. J Personal Disord. 2013;27(6):795–805.
Pulay AJ, Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11:53–67.
Guo ME, Collinson SL, Subramaniam M, Chong SA. Gender differences in schizotypal personality in a Chinese population. Personal Individ Differ. 2011;50:404–8.
Miettunen J, Jääskeläinen E. Sex differences in Wisconsin schizotypy scales-a meta-analysis. Schizophr Bull. 2010;36:347–58.
Raine A. Sex differences in schizotypal personality in a nonclinical population. J Abnorm Psychol. 1992;101(2):361–4.
Bora E, Baysan Arabaci L. Effect of age and gender on schizotypal personality traits in the normal population. Psychiatry Clin Neurosci. 2009;63:663–9.
Badcock JC, Dragović M. Schizotypal personality in mature adults. Personal Individ Differ. 2006;40(1):77–85.
Hummelen B, Pedersen G, Wilberg T, Karterud S. Poor validity of the DSM-IV schizoid personality disorder construct as a diagnostic category. J Personal Disord. 2015;29:334–46.
Triebwasser J, Chemerinski E, Roussos P, Siever LJ. Schizoid personality disorder. J Personal Disord. 2012;26(6):919–26.
Sprock J. Gender-typed behavioral examples of histrionic personality disorder. J Psychopathol Behav Assess. 2000;22:107–22.
Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Smith SM, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69(7):1033–45.
Yang W, Cun L, Du X, Yang J, Wang Y, Wei D, et al. Gender differences in brain structure and resting-state functional connectivity related to narcissistic personality. Sci Rep. 2015;5.
Kubarych TS, Aggen SH, Kendler KS, Torgersen S, Ted RK, Neale MC. Measurement non-invariance of DSM-IV narcissistic personality disorder criteria across age and sex in a population based sample of Norwegian twins. Int J Methods Psychiatr Res. 2010;19:156–66.
Tanaka Y, Ishitobi Y, Inoue A, Oshita H, Okamoto K, Kawashima C, et al. Sex determines cortisol and alpha-amylase responses to acute physical and psychosocial stress in patients with avoidant personality disorder. Brain and Behavior. 2016;6:e00506.
Bornstein R. Sex differences in dependent personality disorder prevalence rates. Clin Psychol Sci Pract. 1996;3:1–12.
Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry. 2006;188(5):423–31.
Grant JE, Mooney ME, Kushner MG. Prevalence, correlates, and comorbidity of DSM-IV obsessive-compulsive personality disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Psychiatr Res. 2012;46:469–75.
Kanehisa M, Kawashima C, Nakanishi M, Okamoto K, Oshita H, Masuda K, et al. Gender differences in automatic thoughts and cortisol and alpha-amylase responses to acute psychosocial stress in patients with obsessive-compulsive personality disorder. J Affect Disord. 2017;217:1–7.
Skodol AE, Clark LA, Bender DS, Krueger RF, Morey LC, Verheul R, et al. Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 part I: description and rationale. Personality Disorders: Theory, Research, and Treatment. 2011;2:4–22.
• Herpertz SC, Huprich SK, Bohus M, Chanen A, Goodman M, Mehlum L, et al. The challenge of transforming the diagnostic system of personality disorders. J Personal Disord. 2017;31:577–89 This article critically reviews the radical changes of the diagnostic system proposed by ICD-11.
Bertsch K, Hillmann K, Herpertz SC. Behavioral and neurobiological correlates of disturbed emotion processing in borderline personality disorder. Psychopathology. 2018;51(2):76–82.
Domes G, Schulze L, Bottger M, Grossmann A, Hauenstein K, Wirtz PH, et al. The neural correlates of sex differences in emotional reactivity and emotion regulation. Hum Brain Mapp. 2009;31(5):758–69.
• Herpertz SC, Nagy K, Ueltzhoffer K, Schmitt R, Mancke F, Schmahl C, et al. Brain mechanisms underlying reactive aggression in borderline personality disorder-sex matters. Biol Psychiatry. 2017;82(4):257–66 This article describes sex-specific differences of borderline patients in aggression and emotion regulation.
Kozak MJ, Cuthbert BN. The NIMH Research Domain Criteria Initiative: background, Issues, and pragmatics. Psychophysiology. 2016;53(3):286–97.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Personality Disorders
Rights and permissions
About this article
Cite this article
Schulte Holthausen, B., Habel, U. Sex Differences in Personality Disorders. Curr Psychiatry Rep 20, 107 (2018). https://doi.org/10.1007/s11920-018-0975-y
Published:
DOI: https://doi.org/10.1007/s11920-018-0975-y