Abstract
Purpose of Review
This review examines the recent literature on biological factors that influence sex differences in posttraumatic stress disorder (PTSD) during childhood and adolescence, focusing on neurobiological, hormonal, and genetic factors that may increase risk in girls.
Recent Findings
More than 60% of children and adolescents are exposed to traumatic events, and many develop PTSD. There is increasing recognition of gender differences in PTSD, with women having double the rates of the disorder compared to men. These gender differences in symptoms and their underlying neurobiology appear to emerge during adolescence, although it is still unclear which biological mechanisms may play key roles in the development of sex difference.
Summary
The literature on gender effects in children and adolescents is still in the early stages, and more prospective and longitudinal work is needed; however, estrogen appears to play a key role in increasing risk for PTSD in girls, which emerges in adolescence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Exposure to traumatic events that harm or threaten the life or integrity of a person or someone close to the person can have long-lasting adverse outcomes for mental health, including posttraumatic stress disorder (PTSD). The impact of gender on the risk for developing PTSD in the aftermath of trauma has long been recognized, as women are twice as likely as men to suffer from the disorder [1]. While in many cases, the types of trauma may underlie this difference seen between the genders, in that women are more likely to be victims of sexual trauma [2], this is not always the case. A recent study of US Navy healthcare personnel found that women had double the odds of having PTSD compared to men after controlling for type of trauma, i.e., combat exposure [3]. In addition to higher prevalence rates, women may present with a different symptom profile or be susceptible to sociocultural biases that increase risk; however, there is substantial evidence suggesting that there may be biological underpinnings for the impact of sex on PTSD. The current report will primarily focus on biological factors.
A potential biological variable to consider is hormonal status, as phase of menstrual cycle is associated with exacerbation of symptoms in women with PTSD [4]. Further, neural circuitry involved in fear expression and regulation as well as physiological fear responses that have been associated with PTSD [5, 6] are influenced by female sex [7] as well as menstrual cycle [8, 9]. More importantly for informing prevention and early intervention strategies, there may also be developmental sex-dependent biological vulnerabilities that increase risk for PTSD in females even at a young age. Studies of child development have the potential to reveal mechanisms that produce the striking sex differences in trauma-related psychopathology in adults.
Development of PTSD in Children and Adolescents
While the detrimental effects of adverse childhood experiences on mental health in adulthood have been recognized for a long time [10], pediatric PTSD has come to greater attention in recent years in clinical settings [11, 12]. Epidemiological samples of children and adolescents show upwards of 60% exposure to traumatic events and up to 9% prevalence of PTSD diagnosis [13•, 14]. The high prevalence of trauma exposure and PTSD in children and adolescents is alarming and underscores the need for trauma-informed health services [11]. A recent study using machine learning, an innovative approach to data analysis using repeated cross-validation methods to extract key features from complex datasets, to predict child PTSD symptoms found that genetic and early environmental variables were causally associated with high symptoms [12].
Pediatric PTSD has also been linked with changes in the brain: a recent meta-analysis found that children and adolescents with PTSD have smaller cerebral gray matter volume and smaller cerebella [15]. Further, prefrontal cortex areas that regulate emotion are smaller in adolescents with PTSD compared to controls [16], while the amygdala, which is activated by emotion, is larger [17•]. Prospective studies in adolescents suggest that overactive fear networks, such as the amygdala, may represent a vulnerability to develop PTSD after trauma [18•]. Taking all these brain-related phenotypes together, it is clear that the neurobiology of adult-like PTSD is already evident in children and adolescents with the disorder. Similarly, deficits in learning to inhibit fear responses, such as during fear extinction and safety learning procedures, have repeatedly been associated with PTSD in adults [19,20,21]; a recent review of extinction learning in children and adolescents found similar deficits in fear inhibition in pediatric PTSD [22]. A limitation in the research to date is that there are very few prospective studies that have examined these neural phenotypes prior to trauma exposure during development; therefore, it is still unclear whether these represent risk factors, result from the disorder itself, or potentially a combination of both. The above mentioned prospective study in adolescents was fortuitous as the study was already ongoing prior to the Boston marathon bombing and there were neuroimaging data prior to and after the trauma; however, the sample was relatively small [18•]. Future prospective studies are needed to better understand predisposing factors during development. Importantly, gender differences are already present in adolescence, with girls having more than three times the odds of having the disorder compared to boys [14]. These gender differences may be related to differences in socialization or trauma exposure; however, there may also be emerging biological sex differences that may especially impact neurobiological biomarkers associated with PTSD.
Impact of Sex on Biomarkers of PTSD in Children and Adolescents
Although there is substantial evidence that females are at greater risk for PTSD than males, it is still unclear when during development this discrepancy in PTSD prevalence between the sexes arises. One of the difficulties with studying PTSD during childhood is that the diagnosis is dependent on a traumatic event occurring to a child. Therefore, it may be better to focus on risk factors and neurobiological biomarkers of PTSD that are present in children, which may be influenced by sex during development.
As mentioned above, brain regions associated with PTSD include areas involved in regulation of emotional responses to threat and fear, such as the amygdala, hippocampus, and insula. Exaggerated reactivity of the amygdala [18•] and an impairment in its connections with the prefrontal cortex [5] appear to be key neurobiological phenotypes for trauma-related psychopathology, and a meta-analysis of neuroimaging literature indicates that women show greater amygdala reactivity to negative emotional stimuli than men [23]. One major predictor of development of PTSD is early life stress. Herringa and colleagues [24] examined the effects of early childhood maltreatment on late adolescence and found that sex was a significant predictor of internalizing symptoms, with females having higher internalizing symptoms compared to males. This study examined the associations among resting state functional connectivity (rs-FC) of the amygdala and hippocampus, childhood maltreatment, and internalizing symptoms. The study showed that maltreatment predicted lower rs-FC between the hippocampus and the subgenual anterior cingulate cortex (sgACC). There were also sex differences, in that maltreatment reduced functional connectivity between the amygdala and sgACC only in females. Lower rs-FC predicted greater internalizing symptoms. In girls, the lower rs-FC of the amygdala and sgACC mediated the association between childhood trauma and symptoms, while in boys the association was with hippocampal connectivity rather than the amygdala [24]. Of note, this study used retrospective reporting on childhood trauma from young adults, and therefore did not capture sex-specific changes during development itself. Additional studies examining a broader age range, such as Hu and colleagues [25], found that sex differences in volume of hippocampal complex structures emerged only after puberty. Although not as prominent in the literature, insula activation has been associated with trauma-related symptoms, and insula development has been suggested to be sexually dimorphic [26•]. A study examining girls and boys with and without PTSD found opposing effects with PTSD symptoms and insula volume and surface area [26•]. Boys with PTSD showed larger volume and surface area of the insula’s anterior circular sulcus than control boys, while girls with PTSD demonstrated smaller volume and surface area than girls without PTSD [26•]. Although it is likely that most sexually dimorphic brain changes occur with the increase in gonadal hormone activity during puberty, it is possible that even before puberty, organizational effects of hormones in utero, may differentially impact girls and boys. For instance, some physiological measures of fear-related symptoms appear to be present in pre-pubertal children [27•].
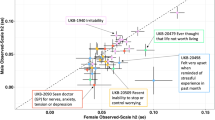
One key symptom of PTSD is hyper-arousal, easily accessed by measurement of an individual’s startle response. Specifically, fear-potentiated startle is a peripheral index of fear neurocircuitry, allowing researchers to noninvasively study psychophysiology associated with PTSD symptomology [28]. A recent study used fear-potentiated startle and skin conductance response (SCR) measurements to study boys and girls, aged 8 to 13, from a highly traumatized population in a fear conditioning paradigm [27•]. In this paradigm, one stimulus was conditioned as a danger cue through pairing with an aversive airblast, while a second stimulus was conditioned to be a safety signal. The results showed that females were physiologically less able to discriminate between danger and safety signals, shown through both skin conductance and fear-potentiated startle measurements. Unlike the association between fear responses and hyper-arousal in adults, the fear responses of the children in this study were associated with intrusive and avoidance symptoms, specifically intrusive symptoms in boys and avoidance in girls [27•]. These sex-specific patterns in PTSD symptoms and physiological fear phenotypes may be due to the differential traumatic experiences between boys and girls, as Soylu and colleagues reported among sexually abused children [29]. It should be noted that the study by Gamwell and colleagues mainly examined pre-pubertal children, and the differences between girls and boys were observed even when post-pubertal children were excluded from analyses [27•], suggesting that gender effects on PTSD symptoms may emerge in childhood. Given that the pattern of symptoms differed between genders, i.e., association between physiology and avoidance in girls vs. intrusive symptoms in boys, it is possible that these effects are rooted in sociocultural rather than biological development. This may explain why the gender differences were observed prior to puberty. On the other hand, stress experienced early in life may lead to long-lasting biological effects associated with development of PTSD. A recent study using an animal model of fear conditioning found that stress experienced prior to puberty led to sexually differentiated behavioral responses associated with the hippocampus when tested in adulthood [30]. This finding suggests sexually differentiated PTSD symptomology seen in adulthood may be rooted in the long-lasting effects of early childhood stress experiences.
Notwithstanding the pre-pubertal differences noted above, puberty may be an especially sensitive time for developmental change in fear neural circuitry [25]. Because puberty is a time of activational effects of gonadal hormones, which have been linked to increased female risk in adults, it could be a prime developmental stage for the emergence of biologically based sex differences in PTSD. The effects of puberty have been observed in fear-potentiated startle paradigms, suggesting undergoing puberty may alter mechanisms of the fear circuit associated with fear-potentiated startle [31•]. Specifically, advancement through pubertal stages is associated with increases in fear-potentiated startle, whereas baseline startle response actually decreases with pubertal stage [31•]. Further, girls have higher fear-potentiated startle in late stages of puberty compared to boys [31•]. The authors suggest this increase may be due to an increase in anxiety reactivity also seen in girls of this study [31•]. However, it is difficult to ascertain the effect of puberty on development of PTSD symptoms, as many studies of children and adolescence fail to include assessments that measure pubertal development and even fewer include measurements of hormonal status associated with pubertal development.
Neurobiological Basis of Sex Differences
Hormones
While sex differences in PTSD-related biomarkers are observed in childhood, there appears to be a shift in their prevalence between the sexes around puberty. Researchers examining age of puberty onset in a sample of American children found average age of puberty onset in females is around 10 years of age and around 11 years of age in males [32]. This corresponds with studies that show an increase in PTSD-related phenotypes around these ages. For example, in children with previous trauma exposure, trauma severity recall is greatest from age 10 to 11; this age has also been identified as a sensitive period for amygdala development [33]. Trauma exposure during this time has the greatest impact on amygdala function [33]. Further, while the amygdala and hippocampus are increasing in volume during puberty in both sexes, growth trajectories in some of these areas differ between males and females during this phase [34]. One study found that testosterone and estrogen predicted right amygdala growth during adolescence in both sexes, while hippocampal growth was not related to pubertal measures [35•]. The results also pointed to an interaction of estradiol levels and sex, as females with lower estradiol levels showed decreases in amygdala volumes, and females with high estradiol levels showed increases in right amygdala volumes across adolescence.
The above studies suggest that increases in estrogen during puberty could influence PTSD phenotypes. Due to the greater prevalence of PTSD in females relative to males, the most recent literature has focused on the effects of estradiol levels in adults. One recent study found that women in the high estrogen phase of the menstrual cycle had greater activation of fear-processing brain areas than both women in a low estrogen phase of the cycle and men [36]. There are also studies showing that women with low estrogen levels have greater connectivity between the amygdala and dorsal ACC, two regions involved in emotion and fear expression [37].
Studies have also explored the role of estrogen on fear psychophysiology, specifically with intermediate phenotypes of PTSD, such as fear inhibition and fear extinction [1]. Fear inhibition refers to the ability to suppress a previously acquired fear response in the presence of a safety signal. One study found that, in naturally cycling adult women, lower levels of estrogen were associated with impaired fear inhibition [38]. Similar effects were seen when examining fear extinction, which describes the ability to learn that a previously conditioned danger signal is no longer predictive of aversive outcomes after the signal is repeatedly presented in the absence of an aversive unconditioned stimulus [39]. In that study, low estrogen levels were associated with high fear-potentiated startle during fear extinction in women with PTSD—these extinction deficits in women with PTSD were attenuated with high estrogen [39]. Similar findings have been shown when examining SCR, as women with low estrogen levels show increased SCR during fear extinction [9]. Additionally, low levels of estrogen predict impairments in extinction recall, also measured through SCR [40]. The effect seems to translate when examining the interaction between stress and estrogen, as women that are stressed during the low estrogen phase show impaired extinction memory [41].
Based on the studies presented, there appears to be a discrepancy between the protective effects of high vs. low estrogen, as both high and low levels of estrogen have been associated with PTSD phenotypes. One possible explanation for this discrepancy is that women are most vulnerable to develop PTSD symptoms during periods of hormonal change, potentially explaining why puberty shows an increase sex difference in PTSD phenotypes. While estrogen appears to be playing an important role in adult women, to date, no studies have examined the effects of gonadal hormones on PTSD symptoms during development—this type of research is needed in order to understand the interplay of trauma, hormones, and development on PTSD.
Genotype
Estrogen may be acting to influence PTSD phenotypes through genetic mechanisms. For example, the gene coding for the pituitary adenylate cyclase-activating polypeptide (PACAP) receptor interacts with estrogen levels [42]. A single-nucleotide polymorphism (SNP) of the PACAP receptor 1 (ADCYAP1R1) is a risk genotype associated with an individual’s response to trauma. Importantly, this SNP is located in an estrogen response element, suggesting a mechanistic pathway for the influence of estrogen on PTSD symptoms. When estrogen levels are low, the risk allele is associated with a decrease in ADCAP1R1 mRNA expression, leading to higher PTSD symptoms [42]. One study found that this SNP risk genotype associates with increased amygdala and hippocampus reactivity to threat stimuli and decreased functional connectivity between the amygdala and hippocampus [43]. This risk SNP also interacts with childhood maltreatment to increase risk for PTSD development in adult females [44]. In addition, association between this genotype and PTSD phenotypes translates to psychophysiological measures, as the ADCAP1R1 SNP is associated with increased dark-enhanced startle in adult females [45]. Dark-enhanced startle is a putative sex-specific biomarker for anxiety response. These genetic effects seem to also be seen in children, as the ADCYAP1R1 risk allele is associated with dark-enhanced startle response in boys and girls; however, no sex difference is seen at this stage [46]. Therefore, some PTSD-related phenotypes show gene by sex by development interactions, further suggesting a change occurring during development to shift the sex difference in PTSD prevalence.
Conclusion
PTSD is more prevalent in women than men, and this gender difference seems to be observed as early as adolescence. While there are likely sociocultural factors related to this increased risk in female sex, there are also biological factors that may be driving the sex difference. The neurobiological biomarkers that have been linked to PTSD are sensitive to female gonadal hormones and menstrual cycle, suggesting that puberty may be the developmental time point when sex differences begin to emerge under the influence of gonadal steroids such as estrogen. Further, genetic studies point to estrogen pathways as part of the risk for PTSD. Both brain development and fear physiology show developmental sex differences; however, it is still unclear whether these are related to puberty. In fact, some physiological differences appear to emerge prior to puberty indicating that there may be multiple mechanisms by which gender may impact PTSD in children and adolescents. Given the high rates of trauma exposure in pediatric populations and the need for better early interventions, future studies should focus on biological underpinnings of these sex effects in order to improve outcomes in vulnerable children.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Briscione MA, Michopoulos V, Jovanovic T, Norrholm SD. Neuroendocrine underpinnings of increased risk for posttraumatic stress disorder in women. Vitam Horm. 2017;103:53–83.
Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–92.
MacGregor AJ, Clouser MC, Mayo JA, Galarneau MR. Gender differences in posttraumatic stress disorder among U.S. navy healthcare personnel. J Women’s Health. 2017;26:338–44.
Nillni YI, Pineles SL, Patton SC, Rouse MH, Sawyer AT, Rasmusson AM. Menstrual cycle effects on psychological symptoms in women with PTSD. J Trauma Stress. 2015;28:1–7.
Stevens JS, Jovanovic T, Fani N, Ely TD, Glover EM, Bradley B, et al. Disrupted amygdala-prefrontal functional connectivity in civilian women with posttraumatic stress disorder. J Psychiatr Res. 2013;47:1469–78.
Glover EM, Jovanovic T, Norrholm SD. Estrogen and extinction of fear memories:implications for posttraumatic stress disorder treatment. Biol Psychiatry. 2015;78:178–85.
Milad MR, Goldstein JM, Orr SP, Wedig MM, Klibanski A, Pitman RK. Fear conditioning and extinction: influence of sex and menstrual cycle in healthy humans. Behav Neurosci. 2006;120:1196–203.
Pineles SL, Nillni YI, King MW, Patton SC, Bauer MR, Mostoufi SM, et al. Extinction retention and the menstrual cycle: different associations for women with posttraumatic stress disorder. J Abnorm Psychol. 2016;125:349–55.
Wegerer M, Kerschbaum H, Blechert J, Wilhelm FH. Low levels of estradiol are associated with elevated conditioned responding during fear extinction and with intrusive memories in daily life. Neurobiol Learn Mem. 2014;116:145–54.
Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, et al. Adverse childhood experiences. Am J Prev Med. 2015;49:354–61.
Marsac ML, Kassam-Adams N, Hildenbrand AK, Nicholls E, Winston FK, Leff SS, et al. Implementing a trauma-informed approach in pediatric healthcare networks. JAMA Pediatr. 2016;170:70–7.
Saxe GN, Ma S, Ren J, Aliferis C. Machine learning methods to predict child posttraumatic stress: a proof of concept study. BMC Psychiatry. 2017;17:223.
• Tedeschi FK, Billick SB. Pediatric PTSD: clinical, forensic, and diagnostic understanding. Journal of the American Academy of Psychiatry and the Law Online. 2017;45:161–9. This study reviews results of epidemiological studies of trauma exposure and PTSD in children and adolescents, reporting high rates of exposure during development.
McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, et al. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:815–30.e14.
Milani ACC, Hoffmann EV, Fossaluza V, Jackowski AP, Mello MF. Does pediatric post-traumatic stress disorder alter the brain? Systematic review and meta-analysis of structural and functional magnetic resonance imaging studies. Psychiatry Clin Neurosci. 2017;71:154–69.
Keding TJ, Herringa RJ. Abnormal structure of fear circuitry in pediatric post-traumatic stress disorder. Neuropsychopharmacology. 2015;40:537–45.
• Weems CF, Klabunde M, Russell JD, Reiss AL, Carrión VG. Post-traumatic stress and age variation in amygdala volumes among youth exposed to trauma. Soc Cogn Affect Neurosci. 2015;10:1661–7. This study examined changes in amygdala volume in a cross-sectional study of children and adolescents between 8 and 18 years of age and found an age by PTSD interaction. The PTSD group showed an increase in amygdala volume with age, while the control group showed a decrease in amygdala volume with age.
• KA ML, Busso DS, Duys A, Green JG, Alves S, Way M, et al. Amygdala response to negative stimuli predicts PTSD symptom onset following a terrorist attack. Depression and Anxiety. 2014;31:834–42. This study collected PTSD symptoms related to the Boston marathon bombing in 15 adolescents who had participated in a neuroimaging study prior to the bombing. The results showed that amygdala reactivity to negative images were positively associated with PTSD symptoms, while hippocampus activity during emotion regulation was associated with fewer PTSD symptoms. This study is limited by small sample size; however, it is the only prospective study of trauma exposure and PTSD in an adolescent sample.
Jovanovic T, Kazama A, Bachevalier J, Davis M. Impaired safety signal learning may be a biomarker of PTSD. Neuropharmacology. 2012;62:695–704.
Norrholm SD, Glover EM, Stevens JS, Fani N, Galatzer-Levy IR, Bradley B, et al. Fear load: the psychophysiological over-expression of fear as an intermediate phenotype associated with trauma reactions. Int J Psychophysiol. 2015;98:270–5.
Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depression and Anxiety. 2015;32:239–53.
McGuire JF, Orr SP, Essoe JKY, McCracken JT, Storch EA, Piacentini J. Extinction learning in childhood anxiety disorders, obsessive compulsive disorder and post-traumatic stress disorder: implications for treatment. Expert Rev Neurother. 2016;16:1155–74.
Stevens JS, Hamann S. Sex differences in brain activation to emotional stimuli: a meta-analysis of neuroimaging studies. Neuropsychologia. 2012;50:1578–93.
Herringa RJ, Birn RM, Ruttle PL, Burghy CA, Stodola DE, Davidson RJ, et al. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc Natl Acad Sci U S A. 2013;110:19119–24.
Hu S, Pruessner JC, Coupé P, Collins DL. Volumetric analysis of medial temporal lobe structures in brain development from childhood to adolescence. NeuroImage. 2013;74:276–87.
• Klabunde M, Weems CF, Raman M, Carrion VG. The moderating effects of sex on insula subdivision structure in youth with posttraumatic stress symptoms. Depression and Anxiety. 2017;34:51–8. This study examined boys and girls ages 9–17 with and without trauma symptoms in a structural magnetic resonance imaging study, focusing on the insula. The authors found that boys with trauma symptoms showed larger bilateral volume and surface area than those without symptoms while girls with symptoms show smaller volume and surface area than controls specifically in the anterior circular sulcus.
• Gamwell K, Nylocks M, Cross D, Bradley B, Norrholm SD, Jovanovic T. Fear conditioned responses and PTSD symptoms in children: sex differences in fear-related symptoms. Dev Psychobiol. 2015;57:799–808. This study examined fear conditioning in children ages 8–13 in a highly traumatized population. The study used fear-potentiated startle and skin conductance response to measure discrimination between learned danger and safety signals. The study found that girls showed less discrimination compared to boys, a phenotype that has been associated with PTSD.
Orcutt HK, Hannan SM, Seligowski AV, Jovanovic T, Norrholm SD, Ressler KJ, et al. Fear-potentiated startle and fear extinction in a sample of undergraduate women exposed to a campus mass shooting. Front Psychol. 2017;7:2031.
Soylu N, Ayaz M, Gökten ES, Alpaslan AH, Dönmez YE, Özcan ÖÖ, et al. Gender differences in sexually abused children and adolescents: a multicenter study in Turkey. Journal of Child Sexual Abuse. 2016;25:415–27.
Brydges NM, Wood ER, Holmes MC, Hall J. Prepubertal stress and hippocampal function: sex-specific effects. Hippocampus. 2014;24:684–92.
• Schmitz A, Grillon C, Avenevoli S, Cui L, Merikangas KR. Developmental investigation of fear-potentiated startle across puberty. Biol Psychol. 2014;97:15–21. This study recruited both girls and boys around puberty for both cross-sectional and longitudinal analysis. Results showed a decrease in baseline startle in mid/late puberty across both sexes but an increase in fear-potentiated startle in mid/late puberty when compared to pre/early puberty, suggesting this increase across puberty is fear specific. The authors found sex-specific effects in that girls showed higher fear-potentiated startle in mid/late puberty while boys showed a trend toward lower fear-potentiated startle in mid/late puberty.
Kelly A, Winer KK, Kalkwarf H, Oberfield SE, Lappe J, Gilsanz V, et al. Age-based reference ranges for annual height velocity in US children. J Clin Endocrinol Metab. 2014;99:2104–12.
Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH. Sensitive periods of amygdala development: the role of maltreatment in preadolescence. NeuroImage. 2014;97:236–44.
Goddings A-L, Mills KL, Clasen LS, Giedd JN, Viner RM, Blakemore S-J. The influence of puberty on subcortical brain development. NeuroImage. 2014;88:242–51.
• Herting MM, Gautam P, Spielberg JM, Kan E, Dahl RE, Sowell ER. The role of testosterone and estradiol in brain volume changes across adolescence: a longitudinal structural MRI study. Hum Brain Mapp. 2014;35:5633–45. This study longitudinally studied various brain regions through structural magnetic resonance images of adolescents of both sexes while assessing their pubertal maturation. Pubertal development significantly predicted volume of the right amygdala, with boys showing an increase in volume with advanced puberty and girls showing a decrease. Testosterone levels were negatively correlated with increased amygdala volume.
Hwang MJ, Zsido RG, Song H, Pace-Schott EF, Miller KK, Lebron-Milad K, et al. Contribution of estradiol levels and hormonal contraceptives to sex differences within the fear network during fear conditioning and extinction. BMC Psychiatry. 2015;15:295.
Engman J, Linnman C, Van Dijk KR, Milad MR. Amygdala subnuclei resting-state functional connectivity sex and estrogen differences. Psychoneuroendocrinology. 2016;63:34–42.
Glover EM, Mercer KB, Norrholm SD, Davis M, Duncan E, Bradley B, et al. Inhibition of fear is differentially associated with cycling estrogen levels in women. Journal of Psychiatry and Neuroscience: JPN. 2013;38:341–8.
Glover EM, Jovanovic T, Mercer KB, Kerley K, Bradley B, Ressler KJ, et al. Estrogen levels are associated with extinction deficits in women with posttraumatic stress disorder. Biol Psychiatry. 2012;72:19–24.
White EC, Graham BM. Estradiol levels in women predict skin conductance response but not valence and expectancy ratings in conditioned fear extinction. Neurobiol Learn Mem. 2016;134(Part B):339–48.
Antov MI, Stockhorst U. Stress exposure prior to fear acquisition interacts with estradiol status to alter recall of fear extinction in humans. Psychoneuroendocrinology. 2014;49:106–18.
Mercer KB, Dias B, Shafer D, Maddox SA, Mulle JG, Hu P, et al. Functional evaluation of a PTSD-associated genetic variant: estradiol regulation and ADCYAP1R1. Transl Psychiatry. 2016;6:e978.
Stevens JS, Almli LM, Fani N, Gutman DA, Bradley B, Norrholm SD, et al. PACAP receptor gene polymorphism impacts fear responses in the amygdala and hippocampus. Proc Natl Acad Sci U S A. 2014;111:3158–63.
Uddin M, Chang S-C, Zhang C, Ressler K, Mercer KB, Galea S, et al. ADCYAP1R1 genotype, posttraumatic stress disorder, and depression among women exposed to childhood maltreatment. Depression and Anxiety. 2013;30:251–8.
Ressler KJ, Mercer KB, Bradley B, Jovanovic T, Mahan A, Kerley K, et al. Post-traumatic stress disorder is associated with PACAP and the PAC1 receptor. Nature. 2011;470:492–7.
Jovanovic T, Norrholm SD, Davis J, Mercer KB, Almli L, Nelson A, et al. PAC1 receptor (ADCYAP1R1) genotype is associated with dark-enhanced startle in children. Mol Psychiatry. 2013;18:742–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kristie Garza and Tanja Jovanovic receive support from National Institutes of Health (MH100122, MH111682), and the Brain and Behavior Research Foundation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sex and Gender Issues in Behavioral Health
Rights and permissions
About this article
Cite this article
Garza, K., Jovanovic, T. Impact of Gender on Child and Adolescent PTSD. Curr Psychiatry Rep 19, 87 (2017). https://doi.org/10.1007/s11920-017-0830-6
Published:
DOI: https://doi.org/10.1007/s11920-017-0830-6