Abstract
Knowledge of gonadal hormone-related influences on human brain anatomy, function, and chemistry is scarce. The present review scrutinized organizational and functional neuroimaging correlates of the menstrual cycle and premenstrual dysphoric disorder (PMDD). Supportive evidence of cyclic short-term structural and functional brain plasticity in response to gonadal hormonal modulation is provided. The paucity of studies, sparsity and discordance of findings, and weaknesses in study design at present hinder the drawing of firm conclusions. Ideal study designs should comprise high-resolution multimodal neuroimaging (e.g., MRI, DTI, rs-fMRI, fMRI, PET), hormones, genetic, and behavioral longitudinal assessments of healthy women and PMDD patients at critical time points of the menstrual cycle phase (i.e., early follicular phase, late follicular phase, mid-luteal phase) in a counter-balanced setup. Studies integrating large-scale brain network structural, functional, and molecular neuroimaging, as well as treatment data, will deepen the understanding of neural state, disorder, and treatment markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sex differences and hormone-related effects in psychiatry have been abundantly reported, if evaluated [1], but their psychoneuroendocrine underpinnings remain largely unknown [2••, 3, 4]. Distinct effects of gonadal hormones on the organizational makeup of the brain during development are well-established. Moreover, the effects of gonadal hormones in adult women (and men) are increasingly studied, and alterations in behavior, emotion processing, and cognitive functions, as well as mental illness have been reported [2••, 3–6]. However, the present knowledge of hormone-related influences on human brain anatomy, function, and chemistry is scarce, calling for further psychoneurobiological studies [2••, 7]. Neuroimaging comprises a set of techniques able to assess putative correlates of structure and function of the healthy and nonhealthy brain. In fact, neuroimaging has become the tool of choice to ascertain mechanistic markers of hormone effects in the brain and is the focus of the present review.
The Menstrual Cycle and PMDD
In a typical 28-day menstrual cycle, estrogen and progesterone levels fluctuate and are at lowest concentrations during the early follicular phase. Throughout the follicular phase, estrogen concentration increases, reaching a preovulatory peak in the late follicular phase, followed by a rapid decrease after the ovulation. During the luteal phase, estrogen and progesterone levels gradually increase to reach the highest concentration in the mid-luteal phase, and then again decrease to minimum levels in the late luteal phase [8]. It is plausible to hypothesize that intrinsic corrective mechanisms take place monthly to orchestrate brain reactivity to these menstrual cycle hormonal fluctuations. However, in certain women, maladaptive neural responsiveness may lead to hormone-related mental disorders [5, 6, 9]. Disrupted hormonal sensitiveness of affective–cognitive circuits, and the resulting impaired function of these circuits, is indeed expected to be involved in the etiology of premenstrual dysphoric disorder (PMDD) [2••, 3, 10].
While having been often confined in the past to something gynecologists should deal with, PMDD is now categorized as a mood disorder [11] with onset of functionally impairing or distressing mood and physical symptoms in the late luteal phase of ovulatory menstrual cycles. Depression, irritability, mood lability, and anxiety are the most commonly reported symptoms [10, 12–14]. The disorder is further characterized by a decline in symptom severity after onset of menstruation and absence of symptoms in the postmenstrual weeks [10, 12, 15, 16]. PMDD is in fact the prototypical sex-specific disorder in which a specific hormonal milieu is required for symptom onset and offset [10, 12, 16]. The disorder, which affects approximately 5 % of women of reproductive age [13, 14, 17], has a moderate heritability [18] and is efficaciously treated with serotonergic antidepressants [19]. Besides the fact that symptoms are present in ovulatory menstrual cycles and occur concomitantly with progesterone fluctuations, discrete biology-based correlates of PMDD are missing. Interestingly, the neural bases of luteal phase affective symptoms have only recently been investigated by means of neuroimaging studies, whereas the ones of symptom relief after efficacious serotonergic treatment are unknown. The availability of neuroimaging phenotypes with high accuracy, sensitivity, and specificity will lead to a nosology of PMDD informed by disease neurobiology beyond the DSM classification.
The modulatory role of estradiol and progesterone on brain structure, as well as cognitive–affective processing, is supported by the widespread presence of their targets; classical nuclear estrogen receptor α and β, progesterone receptor A and B, and nonclassical membrane-associated receptors (e.g., G-protein-coupled estrogen receptors and the progesterone receptor membrane component) [20, 21]. Studies of female brain structure and function, including magnetic resonance imaging (MRI, and associated voxel-based morphometry (VBM)), diffusion tensor imaging (DTI), resting-state MRI (rs-fMRI), functional MRI (fMRI), magnetic resonance spectroscopy (MRS), single-photon emission computed tomography (SPECT/SPET), and positron emission tomography (PET), are here scrutinized to provide an up-to-date critical overview of basic neurobiological functions [22–24] that might be affected by the menstrual cycle hormonal fluctuations.
Brain Organization
Alongside brain structural architecture, the characterization of brain network connectivity at rest is of greatest relevance as functional segregation and integration are key principles in the organization of brain functioning [25, 26]. Though preliminarily, MRI, VBM, DTI, and rs-MRI studies have started to provide supportive evidence of cyclic short-term structural and organizational plasticity in response to gonadal hormonal modulation.
Gray Matter Anatomy
Gray matter morphology, assessed through volumetric neuroimaging, is affected by the menstrual cycle in healthy women. The hippocampus is a candidate substrate for the hormonal effects, especially of estrogen, because of its relation to neurogenesis and synaptic plasticity [27–30]. Volumetric differences in within-subject study designs indicate gray matter volume to be increased in the hippocampus in the late follicular relative to the early follicular and mid-luteal phases [31••], in the right fusiform/ parahippocampal gyrus during early follicular compared to the mid-luteal phase [32], or in the right anterior hippocampus during the late follicular compared to late luteal phase [33]. These findings are in keeping with the commonly reported association between estrogen treatment and larger hippocampal volume, along with enhanced hippocampus function, in postmenopausal women (see review [34]).
Larger gray matter volumes have also been reported at the whole brain level at the time of ovulation [35], in the left dorsal amygdala during the late luteal relative to late follicular phase [36], and in various other regions relative to different menstrual cycle phases [33, 37]. In line with these longitudinal studies, a recent and relatively large cross-sectional study demonstrated thicker right lateral orbitofrontal cortex in the early follicular as compared to the luteal phase [38]. Finally, when association with hormonal levels have been investigated, a number of correlations has been found, although relatively sparsely and with variable results [31••, 35, 37, 38].
From a clinical point of view, women with PMDD have larger cerebellum [39], and left hippocampal gyrus [40], but smaller left parahippocampal gyrus [40] volumes compared to controls. However, better study designs and replication are needed before any conclusions can be drawn.
White Matter Connectivity
It is likely that brain microstructural changes are triggered by the monthly hormonal fluctuations, but studies are few. The microstructural properties of the connecting white matter fiber bundles can be assessed by profiling the diffusion of water molecules by use of diffusion tensor imaging (DTI). Diffusion-weighted magnetic resonance imaging by computing probabilistic tractography allows inferring white matter connectivity of the brain. The commonly computed quantitative parameters of the diffusion tensor are as follows: axial diffusivity, radial diffusivity, mean diffusivity, and fractional anisotropy.
Sex differences and pubertal changes in brain tractography correlates have been indicated, likewise in vitro effects of sex steroids on neuroendocrine tissue [41]. In one study of naturally cycling women, white matter organization of the fornix, measured as mean diffusivity, was shown to correlate negatively with estrogen levels [42]; however, white matter connectivity of PMDD remains unstudied [41]. Proxies of myelination as well as axo-somatic and axo-dendritic connections, such as DTI parameters, represent a basic brain functioning dimension that could reveal mechanistic biomarkers and should therefore be explored.
Brain Resting State Activity and Connectivity
Intrinsic neural activity can be measured as spontaneous low-frequency blood-oxygenation-level-dependent (BOLD) activity at rest (rs-fMRI) or resting state regional blood flow (PET-rCBF). While hormone replacement during menopause appears to increase cerebral blood flow in several cortical regions (review [34]), these measures have not really yet been employed to investigate hormonal influences in fertile women. The one and only existing resting-state PET-rCBF study indicates heightened local neuronal activity, measured as glucose metabolism, in the cingulate, insular, temporal, occipital, and cerebellar regions during the mid-luteal phase, and in prefrontal and temporal regions during the early follicular phase [43].
The so called resting-state networks (RSNs) are related to anatomical connectivity as well as task-evoked reactivity [44], and seem to be sexually dimorphic and thus likely to be influenced by hormonal fluctuations. Inter-regional functional connectivity is examined by computing seed-based analyses, performed using functional localizers, to identify key neural nodes. Connectivity within the network of coupled nodes of a neuronal system can subsequently be examined. Thus far, no effect of menstrual cycle phase has been found on intrinsic functional connectivity within frontoparietal networks at rest in women assessed during the follicular, luteal and menstrual phase [45].
The default mode network (DMN) encompasses communication between the medial prefrontal cortex and anterior cortex with the posterior cingulate cortex, precuneus and the inferior parietal cortex at rest. The degree of network connectivity within the DMN has been associated with depression and sex dimorphism. A one-subject longitudinal study demonstrated gonadal hormone-related effects on DMN, with progesterone being associated with global network connectivity of the dorsolateral prefrontal and sensorimotor cortex, and their connectivity with the hippocampus [46•]. While these findings remain to be replicated, they suggest a progesterone-dependent plasticity mechanism in the resting state connectivity, which may be of relevance in PMDD.
Moreover, higher connectivity at rest of the anterior DMN in the left angular gyrus and of the executive control network in the right anterior cingulate cortex was observed in a large cross-sectional study comparing early follicular to luteal phase women [47]. However, no correlation with hormonal levels was detected [47].
Independent replications are needed to draw conclusions, and studies to assess not only the DMN but also the salience (frontoinsular cortex) and reward networks should be performed. Furthermore, it remains unclear whether greater BOLD or rCBF indicates favorable or aversive phenotypes. While disturbances of network connectivity are supposed to be pathophysiological risk factors for impaired emotion processing and cognitive functioning, the neuropsychological underpinnings of the resting brain at the connectivity level linger uninvestigated in PMDD [2••].
Brain Function
At present, approximately 30 functional neuroimaging studies demonstrate the relevance of endogenous and exogenous ovarian hormones for emotion processing and cognitive functioning, systematically reviewed in [2••]. fMRI findings have indeed highlighted a number of task-dependent brain activation patterns throughout the menstrual cycle, although brain regions poorly overlap [2••]. However, while these studies are important, they have mainly been based on relatively small samples, region-of-interest (ROI)-based analyses, and, in many cases, uncorrected statistics for multiple comparison (e.g., FWE, FDR); three major limitations that hinder meta-analytical analyses and influences the robustness and replicability of the results.
Neural interactions between cognition and emotion circuitries, including a cortical–subcortical interactional network, seem to be modulated by menstrual cycle hormonal fluctuations [48]. This network has been shown to be recruited particularly when manipulating attentional control on emotional stimuli as well as when forcing a self-cognitive reinterpretation of the emotional perception, the so-called reappraisal [49]. Interaction between affective and cognitive processing might differ in PMDD compared to healthy subjects implicating a differential regulation of executive and affective neural circuitries during stimuli response. Only one study has evaluated the impact of emotional distractions on cognitive performance, demonstrating a stronger neural activity in the anterior cingulate cortex and right inferior frontal gyrus in the mid-luteal phase during response inhibition, and a positive correlation between the contralateral inferior frontal gyrus activity and mid-luteal estradiol levels [50].
Functional cerebral asymmetries (FCA) is a sex dimorphic phenotype, and a handful of studies suggest altered inter-hemispheric connectivity in concomitance with high gonadal hormone levels, although the findings so far are discordant as to the direction and as to which gonadal hormone that trigger this effect [51]. At present only one study has been performed, indicating an effect of menstrual cycle phase, not only on inter-hemispheric but also within-hemispheric connectivity, during a cognitive task [52]. As a final point, multimodal studies are almost absent, with the exception of a recent multimodal neuroimaging study combining PET and fMRI. This study suggested differential activation of the dorsolateral prefrontal cortex in women with PMDD during the performance of a working memory task, although independent of hormonal state [53•].
Emotional Stimuli Processing
The functional neuroanatomy of emotion reactivity in healthy naturally cycling women processing images with negative valence suggested some influence of menstrual cycle phase; however, discordantly in terms of direction of effect, on candidate-regions reactivity (e.g., amygdala, anterior cingulate cortex, medial prefrontal cortex, orbitofrontal cortex, dorsolateral prefrontal cortex, and inferior frontal gyrus), as reviewed in [2••]).
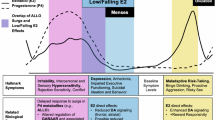
The amygdala is involved in the perception and generation of the emotion stimuli [54]. One of the most consistent menstrual cycle findings in healthy women is enhanced left amygdala activation in the mid- or late luteal phase of the menstrual cycle during negatively valenced picture processing [55, 56], corroborated by similar findings following a single-dose progesterone administration [57, 58]. Furthermore, whereas bilateral amygdala activity in healthy women negatively correlated with progesterone metabolite levels [59], in PMDD patients, the opposite pattern was found with luteal phase progesterone levels positively correlated with bilateral amygdala reactivity to social negative pictures [60]. The amygdala is involved in the bottom-up detection, filtering, encoding, and retrieving of saliency to emotional stimuli [61•]. It is regulated by cortical inputs, and blunted top-down inhibition has been suggested to be unfavorable [61•]. Indeed, in healthy subjects, decreased mPFC reactivity to stressful aversive movie clips has been found in the late luteal phase [59], while enhanced right ACC and OFC response to negatively valenced pictures has been detected in the early follicular phase [62]. Spatiotemporal connectivity of the amygdala with subcortico-subcortical and subcortico-cortical pathways has not been investigated in fMRI studies employing emotion-based tasks across the menstrual cycle. It is likely that the amygdala hyper-reactivity to aversive stimuli in the luteal phase disturbs the frontoinsular cortex activity (Fig. 1), since all are functional nodes forming the salience network (SN) [61•]. Aberrant functional integration and connectivity within the SN, which interconnects along the anterior–posterior axis with the central executive and default mode networks, consequently influences motor and behavioral correlates [61•]. Misattribution of emotional salience associates with increased anxiety or neuroticism, key symptoms of PMDD.
Theoretical outline of dysregulated brain functional brain architectural connectivity in PMDD and the late luteal phase: a pathological and a physiological state associated with affective symptomatology likely due to inappropriate assignment of saliency to emotional stimuli. Exaggerated bottom-up activation of the main hubs of the salience network (insula and amygdala) [55–58, 60], and blunted top-down activation of frontocingulate cortical regions [55, 59, 64•], accompanied by dysregulated coupling within the salience network and with the executive control network
Disrupted hormonal modulation of emotional circuits, such as the amygdala–frontoinsular circuit, and the resulting impaired function of these circuits, are presumably involved in the pathogenesis of PMDD, as well as other affective disorders [2••, 3, 15, 63] (Fig. 1). The neural substrates of affective symptoms during the late luteal phase of the menstrual cycle have indeed been preliminarily characterized in PMDD, however by only one research group (see review [2••]). Sundström-Poromaa and colleagues investigated brain emotion processing in PMDD and healthy controls, once in the mid-follicular and once in the late luteal phase which corresponds with minimum and maximum severity of mood symptoms, respectively. Interestingly, patients with PMDD had weakened frontocingulate cortex activation [64•], in line with the previously found increased amygdala activation in response to social aversive emotional stimuli, and anxiety-dependent increased emotion-induced amygdala reactivity in the luteal phase [56, 60, 65]. These findings are also consistent with neuroimaging findings of functional neural correlates of depression and anxiety [61•], as well as with the suggested late luteal phase–biased emotion processing of information [9, 15]. However, it should be noted that PMDD is presumably not only due to biased emotion processing in the luteal phase, as a psychophysiology study suggested heightened arousal in PMDD women at this time point [66]. Altogether, these studies provide evidence of a distorted affective perception and impaired anxiety regulation in PMDD.
Cognitive Stimuli Processing
Cognitive functioning encompasses visuospatial and verbal skills, memory, problem solving, and perceptual speed. Differences in cognitive functioning between females and males, and as an effect of hormonal variations, are small yet clearly present [6, 67, 68], and not entirely seen until puberty [67–70]. For instance, in mental rotation, which is the ability to imaginary move and rotate two- or three-dimensional objects visually [71], male superiority has been demonstrated. While it is often claimed that women perform better on the mental rotation task in the early follicular phase when estrogen and progesterone levels are low, a recent review found insufficient evidence for this assumption [6]. Furthermore, with the exception of tasks that specifically probe prefrontal cortex function, no influence of the menstrual cycle on cognitive tasks, such as verbal memory or verbal fluency, was demonstrated [6]. In light of this are results from menstrual cycle studies using cognitive paradigms even more difficult to interpret. Nevertheless, the underlying neural cognitive mechanisms regarding visuospatial, verbal, and attention and response inhibition skills affected by hormone/menstrual cycle phase have been preliminarily localized in the prefrontal and, to a lesser extent, temporal and parietal regions in a paradigm-dependent way (see review [2••]).
Furthermore, inter-regional effects within a neuronal system, the so called effective connectivity, have essentially been unexplored. Three studies in healthy women employed psychophysiological interaction analyses on cognitive tasks fMRI data [52, 72, 73]), but thus far, no study has used dynamic causal modeling to investigate interactions between functionally elicited brain responses across the menstrual cycle.
Cognitive disability is also integrated with negative emotion processing and psychiatric symptoms such as anxiety and depression [74]. Greater cognitive impairment is seen in patients with anxiety as well as depression in several domains such as processing speed, attention, reasoning, and verbal knowledge [74, 75]. PMDD is a mood disorder, predominantly emotion-driven, and most studies have failed to demonstrate cognitive deficits in women with PMDD [6]. However, it cannot be excluded that hormone-sensitive cognitive deficits are trigger factors of PMDD. To date, there is only one neuroimaging study investigating cognitive processing in PMDD showing a greater late luteal phase recruitment of the left insula in women with PMDD [76] (see review [2••]).
Brain Chemistry
Beside the monthly endocrine production of gonadal steroids, which pass the blood–brain barrier due to their high lipophilicity, brain-derived steroids are also synthesized (e.g., allopregnanolone, 17β-estradiol). Multiple neurobiological systems mediate the hormonal effects on brain structure and function (e.g., the glutamatergic, γ-aminobutyric acid (GABA)-ergic, cholinergic, serotonergic, noradrenergic, and dopaminergic neurotransmitter system) [77], as underlined by the widespread distribution of estrogen and progesterone receptors in the brain [20, 21]. In vivo studies of sex steroid hormone receptors in the brain are indispensable for breakdown into the mechanistic understanding of their effects; however, the limited availability of tracers targeting these receptors in the brain is hindering advancements hereabouts.
For the estrogen receptor alpha (ESR1), a first clinical trial (NCT01842217) is on-going to validate the 4F-M[18F]FES which has been studied in the rat brain [78•], but for the beta (ESR2), no tracer has been tested in the brain. The [18F]FFNP for the progesterone receptor (PGR), and [18F]FDHT for the androgen receptor (AR) seem promising tracers. Moreover, two probes are available for aromatase imaging in the brain, 11C-cetrozole and [N-methyl-11C]vorozole [79, 80]. This enzyme, through aromatization, converts androgens (i.e., androstenedione, testosterone, 16-hydroxytestosterone) to estrogens (i.e., estrone, 17β-estradiol, and estriol) [81], thus being among the mechanisms able to control local estrogen synthesis [82]. Since it is technically challenging to measure local concentration of estrogens in the brain, and even more to assess the turnover of the hormones, tracers for this enzyme can be seen as a lens on these dynamics [83]. Hence, radiosynthesis and evaluation of new suitable tracers for hormone-related brain imaging is highly desirable.
Acting as allosteric modulators, the effect of sex hormones on the brain chemistry has been preliminarily documented in MRS or SPECT studies of GABA [84–86], glutamate [87], cholin–creatine and N-acetyl-aspartate–creatine ratios [88], lactate–creatine, N-acetyl-aspartate–creatine, glutamate/glutamine–creatine [89], as well as in PET studies of the serotonin receptor 1A [90–92], the serotonin transporter [91], and the dopamine receptor D2 [93]. Importantly, interactions with the serotonergic [90, 94] and the GABAergic system [85••, 95], as well as with glutamate-glutamine [95] and myo-inositol–creatine [88], have been suggested in PMDD patients. Hypothesis-driven volume of interest (VOI)-based statistical analyses and scattered results call for well-powered studies including more than 20 subjects and considering if the magnitude of changes observed between different hormonal conditions is bigger than the one previously reported in test–retest variability.
Genetics
Adaptive sensitivity as well as the development of PMDD symptoms is likely based on the interaction between hormonal changes, individual vulnerability (i.e., genetics) and neurochemical processes. The relationship between genes, hormones, behavior, and PMDD has not really been explored [2••, 7]. Genotype data have rarely been included in neuroimaging studies. Discerningly, an fMRI study pointed to a modulatory role of catechol-o-metyltransferase (COMT) Val158Met genotype on the association between estradiol levels and prefrontal cortex activation during a working memory task [96]. Moreover, one study of emotion processing in PMDD provided preliminary evidence of an interaction between the less functional variant of the brain-derived neurotrophic factor polymorphism brain-derived neurotrophic factor (BDNF) Val66Met and decreased frontocingulate activity in PMDD patients during the luteal phase in response to emotional stimuli [64•]. This pattern of association is consistent with findings from a preclinical model on the role of this polymorphism in the developmental and estrous stage-specific expression of anxiety-like behavior in female mice [97]. However, other candidate functional genotypes (e.g., 5-HTTLPR and MAOA-uVNTR polymorphisms) are also likely to modulate the association between neural, behavioral, and hormonal correlates, and should be investigated.
PMDD Treatment
PMDD affects about 5 % of the women, with many more women suffering monthly of mild symptoms. Selective serotonin reuptake inhibitors (SSRIs) are effective first-line therapy for PMDD (see meta-analysis of [98]). In addition, the short onset of action of SSRIs in women with PMDD, manifesting within the first days of treatment, enables limiting the use of SSRIs to the symptomatic luteal phase of the menstrual cycle (i.e., intermittent dosing [13, 22]). Yet, the influence of SSRI treatment on emotional processing in women with PMDD, in relation to subjective emotional state, and treatment efficacy remains to be appraised. The serotonin system, through its widespread innervation, operates as a fine regulator of several brain functions, personality and behavior, and many psychiatric disorders [99]. Estrogen and progesterone influence the serotonergic function at the level of neurotransmitter synthesis, turnover, release, and receptor, pint-pointing to interactive effects on emotion processing, cognitive functioning, and affective regulation [77]. Consequently, double-blind, randomized, placebo-controlled, parallel, longitudinal pharmaco-neuroimaging studies investigating the neural basis of SSRI treatment in PMDD would progress mechanistic clarification of the disorder etiology and the psychoneurological underpinnings of symptoms relief .
In addition, while SSRIs are highly effective, this type of treatment is not suitable for all women, and long-term compliance to it is relatively low [19, 100]. PMDD is defined by the relation to the late luteal phase of the menstrual cycle. As progesterone is only present in the luteal phase, PMDD is commonly regarded as a disorder caused by the variation in (or mere presence of) progesterone levels. Research in support of this include findings of symptom relief during gonadotropin releasing hormone agonist-induced anovulatory cycles [101], the reinstatement of symptoms when add-back progesterone is administered together with GnRH agonists [102], and findings of progestagen-induced mood symptoms in postmenopausal women [103–105]. While the neural correlates of GnRH agonist treatment have been evaluated in healthy women [34], they remain to be established in women with PMDD.
Exogenous Sex Hormone Effects
Whereas monthly hormonal fluctuations seem on one hand to be both favorable and disadvantageous at the same time, maintenance of stable levels of estrogens and progestins, such as during hormonal contraceptive treatment or hormonal replacement therapy, is also having mixed brain-related outcomes. The altered brain activation patterns by estrogen-only or estrogen-progestagen treatment in therapeutic doses in postmenopausal women are quite scattered (see review [34]). Generally, though in many cases no difference in cognitive performance is present, estrogen treatment enhances activation of frontocingulate regions during cognitive functioning, and progestins seem to counteract these effects. Acute ovarian hormone withdrawal studies suggest corroborating evidence with a decrease in activation of the left inferior frontal gyrus. In contrast, studies on emotion processing in postmenopausal women are lacking. Hormonal replacement appears to increase cerebral blood flow at rest in several cortical regions, and the cholinergic and serotonergic systems seem to act as biological mediators of hormonal influences on the brain [34]. On the other hand, findings of exogenous hormone exposure in studies of women in childbearing ages suggest various sex hormone effects on brain function [2••] and structure [32, 38, 42, 106]. Hence, inadequate evidence is served up to estimate favorable versus disadvantageous effects of the ecological monthly hormonal fluctuations versus artificial steady levels on the brain.
Research Questions
More evidence is needed to meta-analytically aggregate the findings and provide robust neurofunctional models. To elucidate the psychoneurobiological correlates of menstrual hormonal effects and PMDD, two main questions remain to be answered: Are there mechanistic, diagnosis- and treatment-related markers of brain organization and functioning at rest? Do emotion processing and its neural correlates, in the late luteal phase, relate to case–control status, subjective emotional state, and treatment efficacy? The answers will be of relevance to the knowledge- and evidence-based practices in women’s health.
Conclusions
A multitude of neuroimaging findings suggest true alterations in brain structure and function as a result of the hormonal fluctuations of the menstrual cycle. However, higher brain region volume, activation, and connectivity can be interpreted as a less efficient use of resources, beneficial, as a compensatory outcome, and vice versa [107]. Generally, sparsity and discordance of the findings, as well as study limitations, hamper conclusions.
To advance our knowledge on female psychoneuroendocrinology, impact the theoretical framework of PMDD, and promote the development of sex-specific treatments [3, 5], future studies should tackle complementary research questions making use of a unique combination of tools: (1) treatment challenges to get insight into the molecular mechanisms that modulate a neural pathway instead of “static” measurements that merely depict brain chemistry in healthy and sick subjects; (2) complementary techniques—multi-modal neuroimaging, psychology, genetics, endocrinology—the gold standard approach to define intermediate phenotypes and mechanistic markers which are closer to the human biology and more objective than DSM symptoms; and (3) large-scale brain network approaches. This will provide the scientific community with further understanding of the multifaceted interaction between the female hormonal milieu and the brain organization and functioning in women.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Clayton JA, Collins FS. Policy: NIH to balance sex in cell and animal studies. Nature. 2014;509(7500):282–3.
Toffoletto S, Lanzenberger R, Gingnell M, Sundstrom-Poromaa I, Comasco E. Emotional and cognitive functional imaging of estrogen and progesterone effects in the female human brain: a systematic review. Psychoneuroendocrinology. 2014;50:28–52. Comprehensive review of fMRI studies of emotion processing and cognitive functioning in relation to endogenous and exogenous estrogen and progesterone in healthy and premenstrual dysphoric disorder women.
Savic I. Sex differences in the human brain, their underpinnings and implications. Progress in Brain Research. Elsevier; 2010.
Cahill L. Why sex matters for neuroscience. Nat Rev Neurosci. 2006;7(6):477–84.
Gillies GE, McArthur S. Estrogen actions in the brain and the basis for differential action in men and women: a case for sex-specific medicines. Pharmacol Rev. 2010;62(2):155–98.
Sundstrom Poromaa I, Gingnell M. Menstrual cycle influence on cognitive function and emotion processing-from a reproductive perspective. Front Neurosci. 2014;8:380.
Cosgrove KP, Mazure CM, Staley JK. Evolving knowledge of sex differences in brain structure, function, and chemistry. Biol Psychiatry. 2007;62(8):847–55.
Pletzer B. Sex-specific strategy use and global–local processing: a perspective toward integrating sex differences in cognition. Front Neurosci. 2014;8:425.
Wang J, Korczykowski M, Rao H, Fan Y, Pluta J, Gur RC, et al. Gender difference in neural response to psychological stress. Soc Cogn Affect Neurosci. 2007;2(3):227–39.
Epperson CN. Premenstrual dysphoric disorder and the brain. Am J Psychiatry. 2013;170(3):248–52.
A.P.A. Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) 2013.
Epperson CN, Steiner M, Hartlage SA, Eriksson E, Schmidt PJ, Jones I, et al. Premenstrual dysphoric disorder: evidence for a new category for DSM-5. Am J Psychiatry. 2012;169(5):465–75.
Pearlstein T, Steiner M. Premenstrual dysphoric disorder: burden of illness and treatment update. J Psychiatry Neurosci : JPN. 2008;33(4):291–301.
Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology. 2003;28 Suppl 3:1–23.
Cunningham J, Yonkers KA, O'Brien S, Eriksson E. Update on research and treatment of premenstrual dysphoric disorder. Harv Rev Psychiatry. 2009;17(2):120–37.
Yonkers KA, O'Brien PM, Eriksson E. Premenstrual syndrome. Lancet. 2008;371(9619):1200–10.
Wittchen HU, Becker E, Lieb R, Krause P. Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychol Med. 2002;32(1):119–32.
Kendler KS, Karkowski LM, Corey LA, Neale MC. Longitudinal population-based twin study of retrospectively reported premenstrual symptoms and lifetime major depression. Am J Psychiatry. 1998;155(9):1234–40.
Halbreich U. Selective serotonin reuptake inhibitors and initial oral contraceptives for the treatment of PMDD: effective but not enough. CNS Spectrums. 2008;13(7):566–72.
Brinton RD, Thompson RF, Foy MR, Baudry M, Wang J, Finch CE, et al. Progesterone receptors: form and function in brain. Front Neuroendocrinol. 2008;29(2):313–39.
Arevalo MA, Azcoitia I, Garcia-Segura LM. The neuroprotective actions of oestradiol and oestrogen receptors. Nat Rev Neurosci. 2015;16(1):17–29.
Meyer-Lindenberg A, Weinberger DR. Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nat Rev Neurosci. 2006;7(10):818–27.
Rasetti R, Weinberger DR. Intermediate phenotypes in psychiatric disorders. Curr Opin Gene Dev. 2011;21(3):340–8.
Pine DS, Leibenluft E. Biomarkers With a Mechanistic Focus. JAMA Psychiatry. 2015.
Friston KJ. Modalities, modes, and models in functional neuroimaging. Science. 2009;326(5951):399–403.
Fox PT, Friston KJ. Distributed processing; distributed functions? Neuroimage. 2012;61(2):407–26.
Gibbs RB. Estrogen therapy and cognition: a review of the cholinergic hypothesis. Endocr Rev. 2010;31(2):224–53.
Wnuk A, Korol DL, Erickson KI. Estrogens, hormone therapy, and hippocampal volume in postmenopausal women. Maturitas. 2012;73(3):186–90.
Voytko ML, Tinkler GP, Browne C, Tobin JR. Neuroprotective effects of estrogen therapy for cognitive and neurobiological profiles of monkey models of menopause. Am J Primatol. 2009;71(9):794–801.
Daniel JM. Estrogens, estrogen receptors, and female cognitive aging: the impact of timing. Horm Behav. 2013;63(2):231–7.
Lisofsky N, Martensson J, Eckert A, Lindenberger U, Gallinat J, Kuhn S. Hippocampal volume and functional connectivity changes during the female menstrual cycle. NeuroImage. 2015;118:154–62. Multimodal neuroimaging study of healthy women assessed longitudinally four times during the menstrual cycle for grey matter morphometry, white matter organization and functional connectivity.
Pletzer B, Kronbichler M, Aichhorn M, Bergmann J, Ladurner G, Kerschbaum HH. Menstrual cycle and hormonal contraceptive use modulate human brain structure. Brain Res. 2010;1348:55–62.
Protopopescu X, Butler T, Pan H, Root J, Altemus M, Polanecsky M, et al. Hippocampal structural changes across the menstrual cycle. Hippocampus. 2008;18(10):985–8.
Comasco E, Frokjaer VG, Sundstrom-Poromaa I. Functional and molecular neuroimaging of menopause and hormone replacement therapy. Front Neurosci. 2014;8:388.
Hagemann G, Ugur T, Schleussner E, Mentzel HJ, Fitzek C, Witte OW, et al. Changes in brain size during the menstrual cycle. PLoS One. 2011;6(2):e14655.
Ossewaarde L, van Wingen GA, Rijpkema M, Backstrom T, Hermans EJ, Fernandez G. Menstrual cycle-related changes in amygdala morphology are associated with changes in stress sensitivity. Hum Brain Mapp. 2013;34(5):1187–93.
De Bondt T, Jacquemyn Y, Van Hecke W, Sijbers J, Sunaert S, Parizel PM. Regional gray matter volume differences and sex-hormone correlations as a function of menstrual cycle phase and hormonal contraceptives use. Brain Res. 2013;1530:22–31.
Petersen N, Touroutoglou A, Andreano JM, Cahill L. Oral contraceptive pill use is associated with localized decreases in cortical thickness. Hum Brain Mapp. 2015;36(7):2644–54.
Berman SM, London ED, Morgan M, Rapkin AJ. Elevated gray matter volume of the emotional cerebellum in women with premenstrual dysphoric disorder. J Affect Disord. 2013;146(2):266–71.
Jeong HG, Ham BJ, Yeo HB, Jung IK, Joe SH. Gray matter abnormalities in patients with premenstrual dysphoric disorder: an optimized voxel-based morphometry. J Affect Disord. 2012;140(3):260–7.
Peper JS, van den Heuvel MP, Mandl RC, Hulshoff Pol HE, van Honk J. Sex steroids and connectivity in the human brain: a review of neuroimaging studies. Psychoneuroendocrinology. 2011;36(8):1101–13.
De Bondt T, Van Hecke W, Veraart J, Leemans A, Sijbers J, Sunaert S, et al. Does the use of hormonal contraceptives cause microstructural changes in cerebral white matter? Preliminary results of a DTI and tractography study. Eur Radiol. 2013;23(1):57–64.
Reiman EM, Armstrong SM, Matt KS, Mattox JH. The application of positron emission tomography to the study of the normal menstrual cycle. Hum Reprod. 1996;11(12):2799–805.
Deco G, Jirsa VK, McIntosh AR. Emerging concepts for the dynamical organization of resting-state activity in the brain. Nat Rev Neurosci. 2011;12(1):43–56.
Hjelmervik H, Hausmann M, Osnes B, Westerhausen R, Specht K. Resting states are resting traits--an FMRI study of sex differences and menstrual cycle effects in resting state cognitive control networks. PLoS One. 2014;9(7):e103492.
Arelin K, Mueller K, Barth C, Rekkas PV, Kratzsch J, Burmann I et al. Progesterone mediates brain functional connectivity changes during the menstrual cycle - a pilot resting state MRI study. Frontiers in neuroscience. 2015. One-subject study of resting state brain connectivity across the menstrual cycle.
Petersen N, Kilpatrick LA, Goharzad A, Cahill L. Oral contraceptive pill use and menstrual cycle phase are associated with altered resting state functional connectivity. NeuroImage. 2014;90:24–32.
Sacher J, Okon-Singer H, Villringer A. Evidence from neuroimaging for the role of the menstrual cycle in the interplay of emotion and cognition. Front Hum Neurosci. 2013;7(374):00374.
Ochsner KN, Gross JJ. The cognitive control of emotion. Trends Cogn Sci. 2005;9(5):242–9.
Amin Z, Epperson CN, Constable RT, Canli T. Effects of estrogen variation on neural correlates of emotional response inhibition. Neuroimage. 2006;32(1):457–64.
Weis S, Hausmann M. Sex hormones: modulators of interhemispheric inhibition in the human brain. Neuroscientist. 2010;16(2):132–8.
Weis S, Hausmann M, Stoffers B, Sturm W. Dynamic changes in functional cerebral connectivity of spatial cognition during the menstrual cycle. Hum Brain Mapp. 2011;32(10):1544–56.
Baller EB, Wei SM, Kohn PD, Rubinow DR, Alarcon G, Schmidt PJ, et al. Abnormalities of dorsolateral prefrontal function in women with premenstrual dysphoric disorder: a multimodal neuroimaging study. Am J Psychiatry. 2013;170(3):305–14. Multimodal PET and fMRI study indicating neural correlates of PMDD diagnosis and symptoms.
Phillips ML, Drevets WC, Rauch SL, Lane R. Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biol Psychiatry. 2003;54(5):504–14.
Andreano JM, Cahill L. Menstrual cycle modulation of medial temporal activity evoked by negative emotion. NeuroImage. 2010;53(4):1286–93.
Gingnell M, Morell A, Bannbers E, Wikstrom J, Sundstrom PI. Menstrual cycle effects on amygdala reactivity to emotional stimulation in premenstrual dysphoric disorder. Horm Behav. 2012;62(4):400–6.
van Wingen G, van Broekhoven F, Verkes RJ, Petersson KM, Backstrom T, Buitelaar J, et al. How progesterone impairs memory for biologically salient stimuli in healthy young women. J Neurosci. 2007;27(42):11416–23.
van Wingen GA, van Broekhoven F, Verkes RJ, Petersson KM, Backstrom T, Buitelaar JK, et al. Progesterone selectively increases amygdala reactivity in women. Mol Psychiatry. 2008;13(3):325–33.
Ossewaarde L, Hermans EJ, van Wingen GA, Kooijman SC, Johansson IM, Backstrom T, et al. Neural mechanisms underlying changes in stress-sensitivity across the menstrual cycle. Psychoneuroendocrinology. 2010;35(1):47–55.
Gingnell M, Ahlstedt V, Bannbers E, Wikstrom J, Sundstrom-Poromaa I, Fredrikson M. Social stimulation and corticolimbic reactivity in premenstrual dysphoric disorder: a preliminary study. Biol Mood Anxiety Disord. 2014;4(1):3.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15(10):483–506. A scholar review of functional brain networks: DMN, SN, and CEN.
Goldstein JM, Jerram M, Poldrack R, Ahern T, Kennedy DN, Seidman LJ, et al. Hormonal cycle modulates arousal circuitry in women using functional magnetic resonance imaging. J Neurosci. 2005;25(40):9309–16.
Landen M, Eriksson E. How does premenstrual dysphoric disorder relate to depression and anxiety disorders? Depress Anxiety. 2003;17(3):122–9.
Comasco E, Hahn A, Ganger S, Gingnell M, Bannbers E, Oreland L, et al. Emotional fronto-cingulate cortex activation and brain derived neurotrophic factor polymorphism in premenstrual dysphoric disorder. Human Brain Mapping. 2014;35(9):4450–8. First neuroimaging genetic study of PMDD showing an involvement of BDNF genotype on emotion processing in the anterior cingulate cortex during the luteal phase in PMDD patients.
Gingnell M, Bannbers E, Wikstrom J, Fredrikson M, Sundstrom-Poromaa I. Premenstrual dysphoric disorder and prefrontal reactivity during anticipation of emotional stimuli. Eur Neuropsychopharmacol. 2013;17(13):00215.
Epperson CN, Pittman B, Czarkowski KA, Stiklus S, Krystal JH, Grillon C. Luteal-phase accentuation of acoustic startle response in women with premenstrual dysphoric disorder. Neuropsychopharmacology. 2007;32(10):2190–8.
de Frias CM, Nilsson LG, Herlitz A. Sex differences in cognition are stable over a 10-year period in adulthood and old age. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2006;13(3–4):574–87.
Hampson E. Variations in sex-related cognitive abilities across the menstrual cycle. Brain Cogn. 1990;14(1):26–43.
Arnold AP. The organizational-activational hypothesis as the foundation for a unified theory of sexual differentiation of all mammalian tissues. Horm Behav. 2009;55(5):570–8.
Berenbaum SA, Beltz AM. Sexual differentiation of human behavior: effects of prenatal and pubertal organizational hormones. Front Neuroendocrinol. 2011;32(2):183–200.
Shepard RN, Metzler J. Mental rotation of three-dimensional objects. Science. 1971;171(3972):701–3.
Thimm M, Weis S, Hausmann M, Sturm W. Menstrual cycle effects on selective attention and its underlying cortical networks. Neuroscience. 2014;258:307–17.
Weis S, Hausmann M, Stoffers B, Vohn R, Kellermann T, Sturm W. Estradiol modulates functional brain organization during the menstrual cycle: an analysis of interhemispheric inhibition. J Neurosci. 2008;28(50):13401–10.
Okon-Singer H, Hendler T, Pessoa L, Shackman AJ. The neurobiology of emotion-cognition interactions: fundamental questions and strategies for future research. Front Hum Neurosci. 2015;9:58.
Lam RW, Kennedy SH, Mclntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. 2014;59(12):649–54.
Bannbers E, Gingnell M, Engman J, Morell A, Comasco E, Kask K, et al. The effect of premenstrual dysphoric disorder and menstrual cycle phase on brain activity during response inhibition. J Affect Disord. 2012;142(1–3):347–50.
Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37.
Khayum MA, de Vries EF, Glaudemans AW, Dierckx RA, Doorduin J. In vivo imaging of brain estrogen receptors in rats: a 16alpha-18F-fluoro-17beta-estradiol PET study. J Nuclear Med :Off Publ, Soc Nucl Med. 2014;55(3):481–7. PET tracer for neuroimaging of the estrogen receptor in the brain of rodents, and potentially humans.
Takahashi K, Hosoya T, Onoe K, Doi H, Nagata H, Hiramatsu T, et al. 11C-cetrozole: an improved C-11C-methylated PET probe for aromatase imaging in the brain. J Nucl Med : Off Publ, Soc Nucl Med. 2014;55(5):852–7.
Biegon A, Alexoff DL, Kim SW, Logan J, Pareto D, Schlyer D, et al. Aromatase imaging with [N-methyl-11C]vorozole PET in healthy men and women. J Nucl Med : Off Publ, Soc Nucl Med. 2015;56(4):580–5.
Balthazart J, Ball GF. New insights into the regulation and function of brain estrogen synthase (aromatase). Trends Neurosci. 1998;21(6):243–9.
Cornil CA. Rapid regulation of brain oestrogen synthesis: the behavioural roles of oestrogens and their fates. J Neuroendocrinol. 2009;21(3):217–26.
Roselli CE, Liu M, Hurn PD. Brain aromatization: classic roles and new perspectives. Semin Reprod Med. 2009;27(3):207–17.
Harada M, Kubo H, Nose A, Nishitani H, Matsuda T. Measurement of variation in the human cerebral GABA level by in vivo MEGA-editing proton MR spectroscopy using a clinical 3 T instrument and its dependence on brain region and the female menstrual cycle. Hum Brain Mapp. 2011;32(5):828–33.
Epperson CN, Haga K, Mason GF, Sellers E, Gueorguieva R, Zhang W, et al. Cortical y-aminobutyric acid levels across the menstrual cycle in healthy women and those with premenstrual dysphoric disorder: A 1H-MRS study. Arch Gene Psychiatry. 2002;59(9):851–8. The first study neuroimaging GABA in relation to the menstrual cycle and PMDD.
De Bondt T, De Belder F, Vanhevel F, Jacquemyn Y, Parizel PM. Prefrontal GABA concentration changes in women-Influence of menstrual cycle phase, hormonal contraceptive use, and correlation with premenstrual symptoms. Brain Res. 2015;1597:129–38.
Batra NA, Seres-Mailo J, Hanstock C, Seres P, Khudabux J, Bellavance F, et al. Proton magnetic resonance spectroscopy measurement of brain glutamate levels in premenstrual dysphoric disorder. Biol Psychiatry. 2008;63(12):1178–84.
Rasgon NL, Thomas MA, Guze BH, Fairbanks LA, Yue K, Curran JG, et al. Menstrual cycle-related brain metabolite changes using 1H magnetic resonance spectroscopy in premenopausal women: a pilot study. Psychiatry Res. 2001;106(1):47–57.
Chrzan R, Tomaszuk M, Urbanik A. The influence of the menstrual cycle on the result of brain examination with hydrogen magnetic resonance spectroscopy - a pilot study. Neurol Neurochir Pol. 2013;47(5):450–5.
Jovanovic H, Cerin A, Karlsson P, Lundberg J, Halldin C, Nordstrom AL. A PET study of 5-HT1A receptors at different phases of the menstrual cycle in women with premenstrual dysphoria. Psychiatry Res. 2006;148(2–3):185–93.
Jovanovic H, Karlsson P, Cerin A, Halldin C, Nordstrom AL. 5-HT(1A) receptor and 5-HTT binding during the menstrual cycle in healthy women examined with [(11)C] WAY100635 and [(11)C] MADAM PET. Psychiatry Res. 2009;172(1):31–7.
Moses-Kolko EL, Price JC, Shah N, Berga S, Sereika SM, Fisher PM, et al. Age, sex, and reproductive hormone effects on brain serotonin-1A and serotonin-2A receptor binding in a healthy population. Neuropsychopharmacology. 2011;36(13):2729–40.
Nordstrom AL, Olsson H, Halldin C. A PET study of D2 dopamine receptor density at different phases of the menstrual cycle. Psychiatry Res. 1998;83(1):1–6.
Eriksson O, Wall A, Marteinsdottir I, Agren H, Hartvig P, Blomqvist G, et al. Mood changes correlate to changes in brain serotonin precursor trapping in women with premenstrual dysphoria. Psychiatry Res. 2006;146(2):107–16.
Liu B, Wang G, Gao D, Gao F, Zhao B, Qiao M, et al. Alterations of GABA and glutamate-glutamine levels in premenstrual dysphoric disorder: a 3T proton magnetic resonance spectroscopy study. Psychiatry Res. 2015;231(1):64–70.
Jacobs E, D'Esposito M. Estrogen shapes dopamine-dependent cognitive processes: implications for women's health. J Neurosci. 2011;31(14):5286–93.
Bath KG, Chuang J, Spencer-Segal JL, Amso D, Altemus M, McEwen BS, et al. Variant brain-derived neurotrophic factor (Valine66Methionine) polymorphism contributes to developmental and estrous stage-specific expression of anxiety-like behavior in female mice. Biol Psychiatry. 2012;72(6):499–504.
Brown J, O' Brien PM, Marjoribanks J, Wyatt K. Selective serotonin reuptake inhibitors for premenstrual syndrome. Cochrane Database Syst Rev. 2009;2:CD001396.
Nordquist N, Oreland L. Serotonin, genetic variability, behaviour, and psychiatric disorders—a review. Ups J Med Sci. 2010;115(1):2–10.
Sundstrom-Poromaa I, Bixo M, Bjorn I, Nordh O. Compliance to antidepressant drug therapy for treatment of premenstrual syndrome. J Psychosom Obstet Gynaecol. 2000;21(4):205–11.
Wyatt KM, Dimmock PW, Ismail KM, Jones PW, O'Brien PM. The effectiveness of GnRHa with and without 'add-back' therapy in treating premenstrual syndrome: a meta analysis. BJOG. 2004;111(6):585–93.
Segebladh B, Borgstrom A, Nyberg S, Bixo M, Sundstrom-Poromaa I. Evaluation of different add-back estradiol and progesterone treatments to gonadotropin-releasing hormone agonist treatment in patients with premenstrual dysphoric disorder. Am J Obstet Gynecol. 2009;201(2):139 e1–8.
Andreen L, Bixo M, Nyberg S, Sundstrom-Poromaa I, Backstrom T. Progesterone effects during sequential hormone replacement therapy. Eur J Endocrinol. 2003;148(5):571–7.
Andreen L, Sundstrom-Poromaa I, Bixo M, Andersson A, Nyberg S, Backstrom T. Relationship between allopregnanolone and negative mood in postmenopausal women taking sequential hormone replacement therapy with vaginal progesterone. Psychoneuroendocrinology. 2005;30(2):212–24.
Andreen L, Sundstrom-Poromaa I, Bixo M, Nyberg S, Backstrom T. Allopregnanolone concentration and mood—a bimodal association in postmenopausal women treated with oral progesterone. Psychopharmacology (Berl). 2006;187(2):209–21.
Baroncini M, Jissendi P, Catteau-Jonard S, Dewailly D, Pruvo JP, Francke JP, et al. Sex steroid hormones-related structural plasticity in the human hypothalamus. NeuroImage. 2010;50(2):428–33.
Henderson VW, Greicius MD. Functional magnetic resonance imaging and estrogen effects on the brain: cautious interpretation of a BOLD finding. Menopause. 2010;17(4):669–71.
Acknowledgments
The work was partially supported by funds from the Swedish Society of Medicine (SLS-331991), Marta Lundqvist and Tore Nilson foundation, and the Swedish Council for Working Life and Social Research to E.C. (FAS: 2011–0627), and the Swedish Research Council to I.SP. (VR: 521-2013-2339).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Erika Comasco has no conflict of interest to declare.
Inger Sundström-Poromaa serves occasionally on advisory boards or act as invited speaker at scientific meetings for MSD, Novo Nordisk, Bayer Health Care, and Lundbeck A/S.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Women’s Mental Health
Rights and permissions
About this article
Cite this article
Comasco, E., Sundström-Poromaa, I. Neuroimaging the Menstrual Cycle and Premenstrual Dysphoric Disorder. Curr Psychiatry Rep 17, 77 (2015). https://doi.org/10.1007/s11920-015-0619-4
Published:
DOI: https://doi.org/10.1007/s11920-015-0619-4