Abstract
Psychiatric medications such as antidepressants, antipsychotics, and anticonvulsants are commonly prescribed by physicians for the off-label use of improving sleep. Reasons for preferential prescription of these medications over FDA-approved insomnia drugs may include a desire to treat concurrent sleep problems and psychiatric illness with a single medication, and/or an attempt to avoid hypnotic drugs due to their publicized side effects. However, there have been few large studies demonstrating the efficacy and safety of most off-label medications prescribed to treat insomnia. In addition, many of these medications have significant known side effect profiles themselves. Here we review the pertinent research studies published in recent years on antidepressant, antipsychotic, and anticonvulsant medications frequently prescribed for sleep difficulties. Although there have been few large-scale studies for most of these medications, some may be appropriate in the treatment of sleep issues in specific well-defined populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The off-label prescription of antidepressants, antipsychotics, and anticonvulsants for the treatment of sleep problems is a common practice among physicians. In fact, analyses in the past decades have found that certain off-label medications have been prescribed more commonly than FDA-approved medications for insomnia [1, 2]. One analysis of data from a national service tracking physician prescription activity in 2002 found that the number of prescriptions of antidepressants for insomnia had passed the use of FDA-approved hypnotics for insomnia, with 5.28 million prescriptions for antidepressants and 3.4 million prescriptions for insomnia medications that year. The most commonly prescribed medication of all was trazodone, which was prescribed 32 % more than the most widely prescribed insomnia drug [2].
A survey of 1273 members of the American Academy of Child and Adolescent Psychiatry in 2003–2004 found that trazodone was also the most commonly prescribed medication for the treatment of insomnia in children with concurrent mood and anxiety disorders, with other antidepressants, atypical antipsychotics, anticonvulsants, and short-acting hypnotics also being commonly prescribed for sleep complaints in children with mood disorders [3].
Some reasons for prescribing off-label medications over FDA-approved medications for insomnia include: (1) the benefit of using a single medication with sedating properties to manage both a psychiatric or medical disorder and concurrent insomnia; (2) using a medication with sedating properties to offset sleep difficulties caused by another medication; and (3) avoiding the use of hypnotics due to concerns about dependence and side effects. In children, the American Academy of Pediatrics and the National Sleep Foundation have stated that there are inadequate data to guide pharmacologic treatment of insomnia in children [4]. Thus, the physician who wishes to prescribe pharmacotherapy for insomnia in the child or adolescent must choose a medication without an approved indication or adequate research on the effects of these medications in this population.
In adults, the frequent prescription of sedating antidepressants, antipsychotics, and anticonvulsants for insomnia implies that prescribers believe these medications are more effective, or safer, or less prone to dependence or side effects when compared with hypnotic medications. It is true that until recently the FDA included a warning with Schedule-IV hypnotics that these medications not be taken for more than 2 consecutive weeks without reevaluation. Patients and physicians may also be concerned about using hypnotics such as zolpidem after much-publicized reports of sleep driving and other complex behaviors occurring with its use [5]. However, there also remains a paucity of research establishing the safety and efficacy of most antidepressants, antipsychotics, and anticonvulsants for the purpose of treating insomnia. Furthermore, many of these medications may be both expensive and associated with a significant known side effect profile. In the case of antidepressants, side effects may include sleep disturbances such as increased wakefulness after sleep onset (WASO), exacerbation of restless leg syndrome and increased periodic limb movements [6, 7].
FDA approval of new medications for insomnia requires at least 2 randomized, placebo-controlled trials in insomnia patients that show more effective induction and/or maintenance of sleep compared with placebo. Approval also requires evidence of this effectiveness using both objective measurement of sleep and subjective patient report. To a large extent, trials of this magnitude have not been conducted for many off-label prescriptions of these medications for insomnia. One notable exception is doxepin, a tricyclic antidepressant, which was approved by the FDA in 2010 for the treatment of insomnia after 3 large phase III trials demonstrated improved WASO, total sleep time (TST), and sleep efficiency (SE) compared with placebo [8]. The FDA does not prohibit the use of approved medications for off-label purposes; however, the decision to use a medication for a purpose other than its approved indication warrants discussion with the patient concerning the clinical rationale for choosing the medication, as well as documentation of the discussion in the patient’s medical record [9, 10].
The off-label prescription of medications for insomnia has been described extensively in the past [11••]. For the purposes of this article, we will briefly summarize previous research on the sleep effects of specific sedating antidepressants, antipsychotics, and anticonvulsants commonly prescribed for insomnia, with subsequent focus on more recent studies performed in the last 2 years.
Antidepressants
Trazodone
Background
Trazodone is a triazolopyridine antidepressant that blocks post-synaptic serotonin receptors 5-HT1A, 5-HT1C, and 5-HT2, as well as post-synaptic α1-adreneregic receptors. It is a relatively weak SSRI with an elimination half-life of 5–9 hours. Typical doses for depression are >150 mg daily.
Since its introduction in the United States in 1983, few studies have investigated the beneficial effects of trazodone on sleep in people with primary insomnia; however, it is one of the most prescribed off-label medications for sleep difficulties in both adults and children [2, 3, 12]. In small studies with primary insomniacs and normal sleepers, trazodone 50–200 mg has been found to increase slow wave sleep (SWS) over short periods of time, compared with placebo [13–15]. It may be noted that although the clinical significance of increased SWS is not entirely clear, it is often assumed to be a sign of improved sleep. Many more small studies examining the use of trazodone for sleep have been conducted in depressed patients, and in patients whose insomnia is depression-associated or antidepressant-induced. These studies also report increases in SWS and improvements in sleep quality; however, there is no clear trend of benefits in sleep continuity [16–18].
The most common side effects of small doses at bedtime are residual morning sedation and orthostatic hypotension from peripheral adrenergic blockade. Priapism, though often cited as a concerning side effect, is a relatively rare occurrence [19–22].
Recent Studies
There are still few studies on the efficacy and safety of trazodone for primary insomnia, despite its popularity among providers. One within-subjects, randomized, double-blind, placebo-controlled study administered 50 mg to 16 insomniacs 30 minutes before bedtime for 7 days, and found that trazodone produced small but significant impairments of short-term memory, verbal learning, equilibrium, and arm muscle endurance across time-points. Relative to placebo across test days, trazodone was associated with fewer night-time awakenings, minutes of Stage 1 sleep and self-reports of difficulty sleeping. On day 7 only, slow wave sleep was greater and objective measures of daytime sleepiness lower with trazodone than with placebo [23•].
Two recent studies have demonstrated improvement of both depression and insomnia with trazodone. Fourteen patients with primary insomnia and high Beck Depression Inventory (BDI) scores (>10), and 15 sex- and age-matched patients with primary insomnia and low BDI scores (≤10) were treated with trazodone CR 25–150 mg/d for 3 months and followed for 1 month after discontinuation of the medication. Significant improvements in subjective sleep time and several sleep rating scales occurred in both high and low BDI groups. No significant differences were found with actigraphic measurements of sleep [24]. In another double-blind study, 412 patients with major depressive disorder were randomized 1:1 to receive either Trazodone Contramid® OAD (150–375 mg) or placebo for 8 weeks. There was a statistically significant difference between trazodone and placebo on the mean 17-item Hamilton Depression Rating Scale score; secondary findings included improvements in quality of sleep as measured by self-report. This study did not include objective measures of sleep [25].
Trazodone has also been extensively studied in the treatment of fibromyalgia. One study with 66 fibromyalgia patients treated with flexibly dosed trazodone (50-300 mg/day) over 12 weeks found that trazodone significantly improved global fibromyalgia severity, sleep quality, and depression, as well as pain interference with daily activities although without showing a direct effect on bodily pain [26]. In another study, a flexible dose of trazodone (50–300 mg/day), was administered to 66 fibromyalgia patients for 12 weeks. The primary outcome measure was the Pittsburgh Sleep Quality Index (PSQI). Trazodone markedly improved sleep quality, with large effect sizes in total PSQI score as well on sleep quality, sleep duration and SE. Significant improvements, although with moderate effect sizes, were also observed in standardized fibromyalgia, anxiety, and depression rating scores, as well as pain interference with daily activities [27].
A retrospective study on sleep effects of trazodone in patients with dementia found that trazodone was among the antidepressants used with good tolerability in this sample, showing effectiveness in resolving sleep complaints and caregiver distress in 2/3 of patients. “Effectiveness” was defined as improvement of the sleep complaint and reduction in distress of the caregiver as rated on the Neuropsychiatric Inventory Scale (Nighttime Behavior items). One third terminated treatment with trazodone due to a lack of effectiveness but not due to adverse effects [28].
A study on 137 people receiving methadone who reported a Pittsburgh Sleep Quality Index (PSQI) score of 6 or higher found that trazodone did not improve subjective or objective sleep in this sample [29].
Summary
Trazodone may be effective in improving night-time awakenings, subjective sleep difficulties, and objective daytime sleepiness in patients with primary insomnia, but there is evidence that it may also produce significant cognitive and motor impairment. Research on the efficacy of trazodone for sleep difficulties in the last several years has focused on patients with depression and those with fibromyalgia. In these patient groups, significant improvements have been observed in both sleep and comorbid disorder, though without improvements in objective sleep parameters.
Amitriptyline
Background
Amitriptyline is a tricyclic antidepressant (TCA) that inhibits reuptake of serotonin and norepinephrine, with cholinergic, histaminergic, and α1-adreneregic receptor blockade. It has an elimination half-life of 20–30 hours. Typical antidepressant dosages are >75 mg.
Before the introduction of fluoxetine in the US in 1987, tricyclic antidepressants were first-line treatment for depression, and were commonly prescribed to improve sleep in that patient population. However, there have been no data on the effects of amitriptyline on sleep in patients with primary insomnia and little data on sleep effects in patients with depression. There is limited evidence that in depressed patients, amitriptyline may improve PSG sleep measures of TST, sleep latency (SL), early morning awakening, and total REM time; however, this research was performed without placebo comparison or patient self-report [30].
Recent Studies
We found no studies on the effects of amitriptyline on sleep in primary insomniacs in the last 3 years. One study with healthy male subjects investigated the impact of evening doses of 75 mg amitriptyline over 2 nights on PSG-recorded nocturnal sleep and day-time sleepiness measured by the multiple sleep latency test, in comparison to 10 mg escitalopram and placebo. While amitriptyline did reduce PSG-determined WASO, compared with placebo, it also was associated with greater rates of periodic limb movements (PLM) and a higher PLM-arousal index. In turn, amitriptyline was associated with increased daytime sleepiness compared with placebo, as reflected in shorter mean sleep latencies [31].
Amitriptyline has also been studied in sleep disturbance associated with fibromyalgia. A randomized, double-blind, active-control, equivalency crossover trial compared nabilone (0.5–1.0 mg before bedtime) to amitriptyline (10–20 mg before bedtime) in patients with fibromyalgia with chronic insomnia. Although sleep was improved by both amitriptyline and nabilone, nabilone was superior to amitriptyline as rated on the Insomnia Severity Index. No objective measure was reported [32].
Summary
There remains little data on the benefits of amitriptyline for the treatment of sleep difficulties, whether in insomnia or fibromyalgia. Large research efforts in recent years have focused on other TCAs such as doxepin, which has shown promise in the treatment of insomnia at low dosages with minimal side effects.
Doxepin
Background
Like amitriptyline, doxepin is a TCA that inhibits reuptake of serotonin and norepinephrine, with cholinergic, histaminergic, and α1-adreneregic receptor blockade. Typical antidepressant dosage is >75 mg daily. However, it is likely that at low doses under 10 mg, doxepin’s main pharmacologic effect is histaminergic blockade, with little effect on serotonergic or adrenergic receptors [8].
There has been a dramatic increase in research on the sleep effects of doxepin that has led to recent FDA approval in 2010 of doxepin as Silenor® (Somaxon Pharmaceuticals, San Diego, CA) in 3 mg and 6 mg doses for the treatment of insomnia characterized by difficulty with sleep maintenance. Although doxepin is thus no longer considered an off-label prescription for insomnia, we will include it here to illustrate the large research efforts that led to FDA approval of this medication.
Previously, studies on doxepin at lower doses than typically used for antidepressant effect (1, 3, and 6 mg) were found to improve sleep as measured by PSG and patient self-report. Side effects of low-dose doxepin in primary insomniacs are similar to placebo [33].
Recent Studies
FDA approval of Silenor occurred after 3 large phase III clinical trials in adult and elderly patients with chronic primary insomnia demonstrated that low-dose doxepin 3 mg or 6 mg once daily improved PSG-determined WASO, TST, and SE compared with placebo. Five weeks of nightly administration of DXP 3 mg and 6 mg to adults with chronic primary insomnia resulted in significant and sustained improvements in sleep maintenance and early morning awakenings. These sleep improvements were not accompanied by next-day residual effects or followed by rebound insomnia or withdrawal effects upon discontinuation [34••].
Two randomized, double-blind, placebo-controlled trials studied low-dose doxepin in elderly patients with primary insomnia. Elderly adults with primary insomnia were randomized to 4 weeks of nightly treatment with either doxepin 6 mg or placebo. Doxepin 6 mg produced significant improvements in patient-reported WASO, TST, and sleep quality endpoints that were sustained throughout the trial [35••]. Doxepin 1 mg and 3 mg administered nightly to elderly chronic insomnia patients for 12 weeks resulted in significant and sustained improvements in PSG-measured WASO, TST, SE, and WASO compared with placebo; they also noted improvement in patient-reported SOL, TST, and sleep quality. These improvements were not accompanied by evidence of next-day residual sedation or other significant adverse effects [36••].
Summary
The approval of doxepin for the management of insomnia characterized by difficulty in sleep maintenance introduces a medication that has a well-established mechanism of action and few side effects. Perhaps more importantly, it has been studied in geriatric patients, a population with common sleep complaints of early morning awakenings and fragmented sleep. The low anticholinergic effect of this dosage also makes it appropriate for the elderly population.
Mirtazapine
Background
Mirtazapine is a tetracyclic piperazino azepine with potent inhibition of 5-HT2, 5-HT3 and central α2-adrenergic receptors, with minimal monoamine uptake. It has a half-life of 22–40 hours, and typical antidepressant dosage is >15 mg daily.
There have been no placebo-controlled randomized clinical trials of mirtazapine in primary insomniacs. Mirtazapine has been shown to reduce PSG-measured SL and increase slow wave sleep and SE in normal sleepers [37, 38]. In depressed insomniacs, 8 weeks of treatment produced greater reductions in PSG SL and increased TST as compared with fluoxetine, with no patient report described. Antidepressants such as mirtazepine have also shown efficacy in treating disturbed sleep associated with hot flashes in perimenopausal women [39].
Side effects of bedtime mirtazapine 30 mg have been observed, include prolonged next-day motor reaction and impaired driving performance when compared with placebo, for acute but not chronic dosing [40]. Mirtazapine may also cause significant weight gain.
Recent Studies
No recent studies were performed in normal sleepers or primary insomniacs. Two studies tested the effects of mirtazapine in patients with depression. In one of the studies, 16 depressed patients experienced significant improvement of sleepiness and fatigue measures on subjective scales as well as the Multiple Sleep Latency Test (MSLT); there was no placebo comparison [41].
Previously noted side effects of motor impairment were revisited in another study in which 14 depressed patients took mirtazapine 30 mg at bedtime for 30 days. A computerized driving simulator test (DST) and the Maintenance of Wakefulness Test (MWT) were conducted at baseline and on days 2, 9, 16, and 30 after commencement of antidepressant use. Several driving safety measures improved with mirtazepine over time, and several were also superior compared with untreated patients. The authors observed greatest improvement in morning performance, and suggested this may related to the circadian pattern often observed in untreated depression, in which mood is lower in the morning [42].
A case series of 11 perimenopausal women with insomnia without depression found that treatment with mirtazapine 15 mg followed by prolonged-release melatonin add-on therapy significantly improved sleep quality as measured by PSQI scores [43].
Summary
Mirtazapine, as with other sedating antidepressants, may be effective for sleep difficulties in depressed patients, particularly those with a need for weight gain. These studies suggest that it may also improve next-day sleepiness and fatigue, possibly due to its antidepressant effect. Mirtazapine may also be effective in treating insomnia associated with hot flashes in perimenopausal women.
Antipsychotics
Quetiapine
Background
Quetiapine is an atypical antipsychotic with high affinity for 5-HT2A receptors and weak affinity for dopamine, muscarinic, and adrenergic receptors. It has a half-life of 2–3 hours, and a typical antipsychotic dose is 150–800 mg daily.
In small studies of patients with primary insomnia or dementia, quetiapine was previously found to increase PSG or actigraphic TST at doses starting at 25 mg [44–46]. Side effects of quetiapine include weight gain with potential glucose intolerance [47].
Recent Studies
The prescription of quetiapine for sleep difficulties in patients with psychiatric illness and dementia is commonly employed [2]. In 1 retrospective cross-sectional study on the use of quetiapine for sleep in demented patients between January 2007 and December 2009, authors found that 43 of the 101 patients included in the study were prescribed quetiapine, "probably for sleep" [48].
We found only 1 study evaluating the effect of quetiapine in primary insomnia in a randomized controlled trial. Quetiapine 25 mg at night led to nonsignificant improvement of self-reported TST and SOL in patients with primary insomnia [49].
In adolescents with autistic spectrum disorder and aggressive behavior, treatment with 25 mg twice a day (50 mg/d) for the first 4 days of treatment, titrated to a maximum of 150 mg/day based on physician judgment, significantly improved subjective sleep disturbances; a positive correlation was found between the improvements in aggression and sleep [50].
Quetiapine has also been recently studied in regards to generalized anxiety disorder (GAD). One prospectively planned pooled analysis of 3 10-week, randomized, double-blind, placebo-controlled studies evaluated the efficacy and tolerability of acute extended release quetiapine fumarate (quetiapine XR) monotherapy in GAD. Significant improvements vs placebo at Week 8 included Pittsburgh Sleep Quality Index global scores for all quetiapine XR doses (50, 150, and 300 mg/day) [51].
Two studies evaluated adjunctive quetiapine XR in patients with major depressive disorder (MDD) who demonstrated inadequate response to antidepressant treatment. Among the individual Montgomery–Åsberg Depression Rating Scale items, the greatest magnitude of improvement at Weeks 1 and 6 was observed in Item 4 (reduced sleep). Quetiapine XR was also associated with significant improvement in PSQI global score and HAM-D sleep disturbance factor scores at Week 6 [52].
Summary
Quetiapine has been most studied for the treatment of insomnia in disorders characterized by psychosis, frequently with symptoms of agitation. In recent years, a number of studies have suggested it may be useful for treating sleep difficulties in patients with a variety of disorders, including autism with aggressive behavior, GAD, and depression.
Anticonvulsants
Gabapentin
Background
Gabapentin is a GABA analogue that interferes with the influx of calcium into nerve terminals. It is excreted via the kidneys as an unchanged drug, and has a half-life of 5–7 hours. Initial dosing for epilepsy is >900 mg daily. For neuropathic pain, dosing upwards of 2400–3600 mg per day is typical.
Gabapentin has been shown to increase SWS in normal sleepers [53]. Much of the research on gabapentin sleep effects has been conducted in alcoholics, in whom FDA-approved hypnotics treatment for insomnia may not be recommended. Gabapentin has not been found to have significant abuse potential and does not affect hepatic function. It has been studied extensively in treating insomnia during alcohol abstinence, with findings that gabapentin may reduce insomnia as well as alcohol use and cravings [54, 55]. Gabapentin may also reduce sleep disturbance in pain-related disorders such as fibromyalgia, peripheral neuropathy, and traumatic nerve injury [56–60].
Recent Studies
One small, uncontrolled study with 18 primary insomniacs receiving gabapentin treatment for at least 4 weeks showed improved PSQI score, as well as increased PSG-measured SE and slow-wave sleep, decreased WASO, and spontaneous arousal index after gabapentin treatment [61].
A secondary analysis of data from a cohort of menopausal women participating in a randomized, double-blind, placebo-controlled trial of gabapentin 300 mg, 3 times daily (TID) for hot flashes saw gabapentin-associated improvement in the global PSQI score and SE factor score at 4 weeks [62].
Research also continues on the sleep effects of gabapentin in alcoholics. One hundred individuals seeking outpatient treatment of alcohol withdrawal with Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA-Ar) ratings ≥10 were randomized to double-blind treatment with 2 doses of gabapentin (900 mg tapering to 600 mg or 1200 tapering to 800 mg) or lorazepam (6 mg tapering to 4 mg) for 4 days. The Epworth Sleepiness scale was significantly lower in the high dose gabapentin vs lorazepam group during the randomized treatment, but not during follow-up. The authors note that symptoms of impaired sleep, mood instability, and anxiety play a role in alcohol relapse; however, they do not speculate on whether lower Epworth Sleepiness scale scores were due to improved sleep or decreased daytime sedation with gabapentin compared with lorazepam [63].
Summary
Gabapentin has been extensively studied in the treatment of sleep disturbance associated with pain disorders. In addition, it may improve insomnia associated with menopause and alcohol withdrawal. Additional placebo-controlled research in primary insomniacs may be helpful in establishing its effect in that population.
Pregabalin
Background
Pregabalin is closely related to gabapentin, with a similar mechanism of action. Its half-life is 5–6 hours and it is excreted by the kidneys. Pregabalin is FDA-approved for the treatment of fibromyalgia, epilepsy, neuropathic pain, and post-herpetic neuralgia. Dosing for pain syndromes is 150–600 mg per day.
Pregabalin has been shown to increase SWS in normal sleepers [64]. Many studies have been performed showing that treatment with pregabalin in pain-related syndromes reduces sleep disturbance [65–68].
Recent Studies
Much of the recent efforts on studying sleep effects of pregabalin have focused on treating sleep disturbance in fibromyalgia. One study published analyses of 2 randomized, double-blind, placebo-controlled trials of pregabalin (300, 450, and 600 mg daily) in adult fibromyalgia patients. Pregabalin significantly improved quality of sleep as measured by daily sleep diary and the Medical Outcomes Study Sleep Scale items for sleep disturbance, quantity of sleep, and sleep problems, relative to placebo. Mediation models indicated that 43 %–80 % of the benefits on sleep (vs placebo) were direct effects of pregabalin, with the remainder resulting from an indirect effect of treatment via pain relief [69].
Another international, multicenter, double-blind, placebo-controlled trial randomly assigned 747 patients with fibromyalgia to placebo or 300, 450, or 600 mg/day pregabalin twice daily for 14 weeks. All pregabalin doses demonstrated superiority to placebo on the Medical Outcomes Study-Sleep Scale Sleep Disturbance subscale and the Sleep Quality diary [70•].
Sleep effects of pregabalin were also studied in generalized anxiety patients. Data were analyzed from 6 double-blind, placebo-controlled, 4- to 6-week trials of outpatients with GAD with a minimum Hamilton Rating Scale for Anxiety (HAM-A) score = 18. Response was evaluated for 3 fixed-dose pregabalin groups (150, 300–450, 600 mg/day), and for a benzodiazepine group (alprazolam or lorazepam). In the “high-insomnia” subgroup (defined by a baseline HAM for Depression (HAM-D) insomnia factor score greater than “3”, treatment with the 2 higher doses of pregabalin (300–450 and 600 mg), and with alprazolam/lorazepam, was associated with significant endpoint improvement on the 3-item HAM-D insomnia factor score [71•].
Summary
Pregabalin, like gabapentin, is well-established in its subjective improvement of insomnia associated with pain disorders such as fibromyalgia. In addition, a number of studies have suggested it may improve sleep difficulties associated with GAD.
Conclusion
Off-label prescriptions for antidepressants, antipsychotics, and anticonvulsants continue to rival that of FDA-approved medications for the treatment of insomnia. The last several years have seen the approval of doxepin following placebo-controlled, randomized clinical trials demonstrating its efficacy and safety in adult and elderly patients with primary insomnia. Other medications are increasingly studied in the treatment of comorbid insomnia in special populations such as patients with fibromyalgia and generalized anxiety. Still other medications that were (and possibly still are) frequently prescribed for insomnia, such as amitriptyline, nortriptyline, valproic acid, and tiagabine, have had very little published research in recent years investigating their effects on sleep.
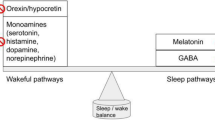
Although few of the studied medications have reached the level of research required for FDA approval, many of them do show sleep improvement within well-defined populations. For physicians treating these disorders, the ability to prescribe one medication for the patient’s underlying disorder and treat concurrent insomnia is an attractive quality. Many of these medications also enhance SWS, a characteristic not seen in most FDA-approved hypnotics [72, 73].
While off-label use of these medications may or may not be appropriate for primary insomnia, they may be useful in the special populations for whom the medications have been studied heavily, even without specific FDA approval. For many of these drugs, it is unclear whether the drug is directly treating the insomnia itself, or merely easing sleep difficulties secondary to an underlying psychiatric condition.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Walsh JK, Schweitzer PK. Ten-year trends in the pharmacological treatment of insomnia. Sleep. 1999;22:371–5.
Walsh JK. Drugs used to treat insomnia in 2002: regulatory-based rather than evidence-based medicine. Sleep. 2004;27:1441–2.
Owens J, Rosen C, Mindell J, et al. Use of pharmacotherapy for insomnia in child psychiatry practice: a national survey. Sleep Med. 2010;11:692–700.
Mindell J, Emslie G, Blumer L, et al. Pharmacologic management of insomnia in children and adolescents: consensus statement. Pediatrics. 2006;117:1223–32.
Poceta J. Zolpidem ingestion, automatisms, and sleep driving: a clinical and legal case series. J Clin Sleep Med. 2011;7:632–8.
Rottach K, Schaner BM, Kirch M. Restless leg syndrome as side effect of second generation antidepressants. J Psychiatr Res. 2008;43:70–5.
Schweitzer P, et al. Drugs that disturb sleep and wakefulness. In: Kryger M, Roth T, Dement, editors. Principles and practice of sleep medicine. 5th ed. St Louis: Elsevier Saunders; 2012. p. 542.
Weber J, Siddiqui M, Wagstaff A. Low-dose doxepin: in the treatment of insomnia. CNS Drugs. 2010;24:713–20.
Kuntz R. Off-label prescribing of antidepressants and anxiolytics: an attorney's guide to psychoactive drugs. J Psychiatry Law. 1998;26:519–32.
Kramer S, McCall V. Off-label prescribing: 7 steps for safer, more effective treatment. Curr Psychiatry. 2006;5:15–28.
•• McCall W. Off-label use of prescription medications for insomnia: sedating antidepressants, antipsychotics, anxiolytics, and anticonvulsants. In: Sateia M, Buysse D, editors. Insomnia: diagnosis and treatment. London: Informa Healthcare; 2010. p. 397–409. This chapter presents a comprehensive review of the literature regarding the off-label use of psychiatric medications in treating sleep difficulties.
Dording C, Mischoulon D, Petersen T, et al. The pharmacologic management of SSRI-induced side effects: a survey of psychiatrists. Ann Clin Psychiatry. 2002;14:143–7.
Montgomery I, Oswald I, Morgan K, et al. Trazodone enhances sleep in subjective quality but not in objective duration. Br J Clin Pharmacol. 1983;16:139–44.
Yamadera H, Nakamura S, Suzuki H, et al. Effects of trazodone hydrochloride and imipramine on polysomnography in healthy subjects. Psychiatry Clin Neurosci. 1998;52:439–43.
Ware JC, Pittard JT. Increased deep sleep after trazodone use: a double-blind placebo-controlled study in healthy young adults. J Clin Psychiatry. 1990;51:18–22.
Mendelson WB. A review of the evidence for the efficacy and safety of trazodone in insomnia. J Clin Psychiatry. 2005;66:469–76.
Haffmans PMJ. The effects of trazodone on sleep disturbances included by brofaromine. Eur Psychiatry. 1999;14:167–71.
Nierenberg A, Adler LA, Peselow E, et al. Trazodone for antidepressant-associated insomnia. Am J Psychiatry. 1994;151:1069–72.
Burns M, Hoskowitz H, Jaffe J. A comparison of the effects of trazodone and amitriptyline on skills performance by geriatric subjects. J Clin Psychiatry. 1986;47:252–4.
Warrington SJ, Ankier SI, Turner P. An evaluation of possible interactions between ethanol and trazodone or amitriptyline. Br J Clin Pharmacol. 1984;18:549–57.
Saletu-Zyhlarz G, Abu-Bakr M, Anderer P, et al. Insomnia related to dysthymia: polysomnographic and psychometric comparison with normal controls and acute therapeutic trials with trazodone. Neuropsychobiology. 2001;44:139–49.
James S, Mendelson W. The use of trazodone as a hypnotic: a critical review. J Clin Psychiatry. 2004;65:752–5.
• Roth A, McCall W, Vaughn, Liguori A. Cognitive, psychomotor and polysomnographic effects of trazodone in primary insomniacs. J Sleep Res. 2011;20:552–8. Although trazodone is one of the most frequently prescribed off-label medications for insomnia, few studies have investigated its efficacy and safety for this indication. In this study, trazodone 50 mg produced significant impairments of short-term memory, verbal learning, equilibrium, and arm muscle endurance across time-points. Relative to placebo, trazodone was associated with fewer night-time awakenings, minutes of Stage 1 sleep and self-reports of difficulty sleeping.
Wichniak A, Wierzbicka A, Jernajczyk W. Patinets with insomnia and subthreshold depression show marked worsening of insomnia after discontinuation of sleep promoting medication. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1671–6.
Sheehan D, Croft H, Gossen E, et al. Extended-release trazodone in major depressive disorder: a randomized, double-blind, placebo-controlled study. Psychiatry. 2009;6:20–33.
Calandre E, Morillas-Arques P, Molina-Barea R, et al. Trazodone plus pregabalin combination in the treatment of fibromyalgia: a 2-phase, 24-week, open-label uncontrolled study. BMC Musculoskelet Disord. 2011;12:95.
Morillas-Arques P, Rodriguez-Lopez C, Molina-Barea R, et al. Trazodone for the treatment of fibromyalgia: an open-label, 12-week study. BMC Musculoskelet Disord. 2010;11:204.
Camargos E, Pandolfi M, Freitas M, et al. Trazodone for the treatment of sleep disorders in dementia: an open-label, observational and review study. Arq Neuropsiquiatr. 2011;69:44–9.
Stein M, Kurth M, Sharkey K, et al. Trazodone for sleep disturbance during methadone maintenance: a double-blind, placebo-controlled trial. Drug Alcohol Depend. 2012;120:65–73.
Kupfer DJ, Spiker DG, Coble P, et al. Amitriptyline and EEG sleep in depressed patients: I. Drug effect Sleep. 1978;1:149–59.
Doerr J, Spiegelhalder K, Petzold F, et al. Impact of escitalopram on nocturnal sleep, day-time sleepiness, and performance compared to amitriptyline: a randomized, double-blind, placebo-controlled study in healthy male subjects. Pharmacopsychiatry. 2010;43:166–73.
Ware M, Fitzcharles M, Joseph L, et al. The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg. 2010;110:604–10.
Roth T, Rogowski R, Hull S, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in adults with primary insomnia. Sleep. 2007;30:1555–61.
•• Krystal A, Lankford A, Durrence HH, et al. Efficacy and safety of doxepin 3 and 6 mg in a 35-day sleep laboratory trial in adults with chronic primary insomnia. Sleep. 2011;34:1433–42. Five weeks of nightly administration of doxepin 3 mg and 6 mg to adults with chronic primary insomnia resulted in significant and sustained improvements in sleep maintenance and early morning awakenings.
•• Krystal A, Durrence HH, Scharf M. Efficacy and safety of doxepin 1 mg and 3 mg in a 12-week sleep laboratory and outpatient trial of elderly subjects with chronic primary insomnia. Sleep. 2010;33:1553–61. Doxepin 1 mg and 3 mg administered nightly to elderly chronic insomnia patients for 12 weeks resulted in significant and sustained improvements in most endpoints, without evidence of next-day residual sedation or other significant adverse effects. Doxepin also demonstrated improvements in both patient- and physician-based ratings of global insomnia outcome.
•• Lankford A, Rogowski R, Essink B, et al. Efficacy and safety of doxepin 6 mg in a 4-week outpatient trial of elderly adults with chronic primary insomnia. Sleep Med. 2012;13:133–8. Elderly adults meeting DSM-IV-TR criteria for primary insomnia were randomized to 4 weeks of nightly treatment with either doxepin 6 mg or placebo. Doxepin 6 mg produced significant improvements in sleep maintenance, sleep duration, and sleep quality endpoints that were sustained throughout the trial.
Ruigt GSF, Kemp B, Groenhout CM, et al. Effect of the antidepressant Org 3770 on human sleep. Eur J Clin Pharmacol. 1990;38:551–4.
Aslan S, Isik E, Cosar B. The effects of mirtazapine on sleep: a placebo controlled, double-blind study in young healthy volunteers. Sleep. 2002;25:677–9.
Perez D, Loprinzi D, Barton DL. Pilot evaluation of mirtazapine for the treatment of hot flashes. J Support Oncol. 2004;2:50–6.
Wingen M, Bothmer J, Langer S, et al. Actual driving performance and psychomotor function in healthy subjects after acute and subchronic treatment with escitalopram, mirtazapine, and placebo: a crossover trial. J Clin Psychiatry. 2005;66:436–43.
Shen J, Hossain N, Streiner D, et al. Excessive daytime sleepiness and fatigue in depressed patients and therapeutic response of a sedating antidepressant. J Affect Disord. 2011;134:421–6.
Shen J, Moller H, Wang X, et al. Mirtazapine, a sedating antidepressant, and improved driving safety in patients with major depressive disorder: a prospective, randomized trial of 28 patients. J Clin Psychiatry. 2009;70:370–7.
Dolev Z. Case series of perimenopausal women with insomnia treated with mirtazapine followed by prolonged-release melatonin add-on and monotherapy. Arch Womens Ment Health. 2011;14:269–73.
Cohrs S, Rodenbeck A, Guan Z, et al. Sleep-promoting properties of quetiapine in healthy subjects. Psychopharmacology. 2004;174:421–9.
Wiegand M, Landry F, Bruckner T, et al. Quetiapine in primary insomnia: a pilot study. Psychopharmacology. 2008;196:337–8.
Nanda F, Singer C. Placebo-Controlled Trial of Quetiapine for Sleep Disturbance in Dementia and MCI. 16 ed. 2008;A126.
Cates M, Jackson C, Feldman J, et al. Metabolic consequences of using low-dose quetiapine for insomnia in psychiatric patients. Community Ment Health J. 2009;45:251–4.
Dolder C, McKinsey J. Quetiapine for sleep in patients with dementia. Consult Pharm. 2010;25:676–9.
Tassniyom K, Paholpak S, Tassniyom S, et al. Quetiapine for primary insomnia: a double blind, randomized controlled trial. J Med Assoc Thai. 2010;93:729–34.
Golubchik P, Sever J, Weizman A. A low-dose quetiapine for adolescents with autistic spectrum disorder and aggressive behavior: open-label trial. Clin Neuropharmacol. 2011;34:216–9.
Stein D, Bandelow B, Merideth C, et al. Efficacy and tolerability of extended release quetiapine fumarate (quetiapine XR) monotherapy in patients with generalized anxiety disorder: an analysis of pooled data from 3 8-week placebo-controlled studies. Hum Psychopharmacol. 2011;26:614–28.
Bauer M, El-Khalili N, Datto C, et al. A pooled analysis of 2 randomized, placebo-controlled studies of extended release quetiapine fumarate adjunctive to antidepressant therapy in patients with major depressive disorder. J Affect Disord. 2010;127:19–30.
Foldvary-Schaefer N, De Leon Sanchez I, Karafa M, et al. Gabapentin increases slow-wave sleep in normal adults. Epilepsia. 2002;43:1493–7.
Karam-Hage M, Brower K. Open pilot study of gabapentin versus trazodone to treat insomnia in alcoholic outpatients. Psychiatry Clin Neurosci. 2003;57:542–4.
Furieri F, Nakamura-Placios E. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68:1691–700.
Arnold LM, Goldenberg D, Stanford S, et al. Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial. Arthritis Rheum. 2007;56:1336–44.
Hahn K, Arendt G, Braun J, et al. A placebo-controlled trial of gabapentin for painful HIV-associated sensory neuropathies. J Neurol. 2004;251:1260–6.
Rice A, Maton S, Postherpetic Neuralgia Study Group. Gabapentin in postherpetic neuralgia: a randomized, double blind, placebo controlled study. Pain. 2001;94:215–24.
Backonja M. Gabapentin monotherapy for the symptomatic treatment of painful neuropathy: a multicenter, double-blind, placebo-controlled trial in patients with diabetes mellitus. Epilepsia. 1990;40(Suppl):S57–9.
Gordh T, Stubhaug A, Jenson T, et al. Gabapentin in traumatic nerve injury pain: a randomized, double-blind, placebo-controlled, cross-over, multi-center study. Pain. 2008;138:255–66.
Lo H, Yang C, Lo H, et al. Treatment effects of gabapentin for primary insomnia. Clin Neuropharmacol. 2010;33:84–90.
Yurcheshen M, Guttuso TJ, McDermott M, et al. Effects of gabapentin on sleep in menopausal women with hot flashes as measured by a Pittsburgh sleep quality index factor scoring model. J Womens Health. 2009;18:1355–60.
Myrick H, Malcolm R, Randall P. A double-blind trial of gabapentin vs lorazepam in the treatment of alcohol withdrawal. Alcohol Clin Exp Res. 2009;33:1582–8.
Hindmarch I, Dawson J, Stanley N. A double-blind study in healthy volunteers to assess the effects on sleep of pregabalin compared with alprazolam and placebo. Sleep. 2005;28:187–93.
Arnold LM, Russell I, Diri E, et al. A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain. 2008;9:792–805.
Freeman R, Durso-Decruz E, Emir B. Efficacy, safety, and tolerability of pregabalin treatment for painful diabetic peripheral neuropathy: findings from 7 randomized, controlled trials across a range of doses. Diabetes Care. 2008;31:1448–54.
Mease P, Russell I, Arnold LM, et al. A randomized, double-blind, placebo-controlled, phase III trial of pregabalin in the treatment of patients with fibromyalgia. J Rheumatol. 2008;35:502–14.
Siddall P, Cousins M, Otte A, et al. Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial. Neurology. 2006;67:1792–800.
Russell I, Crofford L, Leon T. The effects of pregabalin on sleep disturbance symptoms among individuals with fibromyalgia syndrome. Sleep Med. 2009;10:604–10.
• Pauer L, Winkelmann A, Arsenault P, et al. An international, randomized, double-blind, placebo-controlled, phase III trial of pregabalin monotherapy in treatment of patients with fibromyalgia. J Rheumatol. 2011;38:2643–52. This international, multicenter, double-blind, placebo-controlled trial randomly assigned 747 patients with fibromyalgia to placebo or 300, 450, or 600 mg/day pregabalin twice daily for 14 weeks. All pregabalin doses demonstrated superiority to placebo on the Medical Outcomes Study-Sleep Scale Sleep Disturbance subscale and the Sleep Quality diary.
• Montgomery S, Herman B, Schweizer E, et al. The efficacy of pregabalin and benzodiazepines in generalized anxiety disorder presenting with high levels of insomnia. Int Clin Psychopharmacol. 2009;24:214–22. Pooled data from 6 double-blind, placebo-controlled, 4- to 6-week trials of outpatients with generalized anxiety disorder found that pregabalin was well tolerated and improved overall anxiety symptoms, while specifically improving insomnia in patients with generalized anxiety disorder presenting with high levels of concurrent insomnia.
Zammit GK, McNabb LJ, Caron J, et al. Efficacy and safety of eszopiclone across 6-weeks of treatment for primary insomnia. Curr Med Res Opin. 2004;20:1979–91.
Roth T, Soubrane C, Titeux L, et al. Efficacy and safety of zolpidem-MR: a double-blind, placebo-controlled study in adults with primary insomnia. Sleep Med. 2006;7:397–406.
Disclosure
C. McCall: none; W. V. McCall: consultant for Sunovion.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
McCall, C., McCall, W.V. What Is the Role of Sedating Antidepressants, Antipsychotics, and Anticonvulsants in the Management of Insomnia?. Curr Psychiatry Rep 14, 494–502 (2012). https://doi.org/10.1007/s11920-012-0302-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-012-0302-y