Abstract
Purpose of Review
Pseudotumor cerebri syndrome (PTCS) may affect both children and adults; however, the risk factors and clinical presentation vary greatly between these populations. This review aims to highlight the entity of PTCS in children and the unique considerations in this population; review the epidemiology and demographics; discuss the clinical presentation, revised diagnostic criteria, and approach to evaluation; review management strategies; and discuss the prognosis and long-term outcomes in children with PTCS.
Recent Findings
Clinical presentation can be variable in children and may be less obvious than in their adult counterparts. Papilledema can also be challenging to diagnose in this population. The upper limits for opening pressure on lumbar puncture differ in children, with a cut-off of 25 cm H20 (or 28 cm H2O in a sedated or obese child).
Summary
Morbidity related to visual loss, pain and reduced quality of life lends urgency towards accurately identifying, evaluating and managing children with PTCS. There are no randomised controlled studies to allow for evidence-based recommendations for the management of PTCS in children. Further studies are needed to clarify and consolidate management approaches in this population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pseudotumour cerebri syndrome (PTCS) is the umbrella term for a series of symptoms and signs reflecting increased intracranial pressure with normal brain parenchyma, which cannot be attributed to a space-occupying lesion, ventriculomegaly, malignancy or infection. When precipitated by an identifiable secondary cause, the nomenclature of secondary PTCS is preferred. In the absence of an identifiable secondary cause, primary PTCS is preferred. Some consider the older term idiopathic intracranial hypertension to be a subset of primary PTCS, in the absence of any known risk factors [1, 2••]. The term benign intracranial hypertension should be rejected; it is misleading and misrepresentative given the significant potential for vision loss and reduced quality of life that this condition carries.
PTCS may affect both children and adults. However, the risk factors and clinical presentation vary greatly between these populations, therefore PTCS in children merits distinct review. In this paper, we aim to highlight the entity of PTCS in children and the unique considerations in this population; review the epidemiology and demographics; discuss the clinical presentation, revised diagnostic criteria, and approach to evaluation; review management strategies; and discuss the prognosis and long-term outcomes in children with PTCS.
Epidemiology and Demographics
The annual incidence of PTCS in adults is estimated at 0.9–2.36/100,000 [3, 4]. In paediatric studies, the annual incidence is slightly lower, estimated at 0.6–0.71/100,000 [5,6,7].
Of importance in interpreting these epidemiological studies is the historic variability in the case definitions of PTCS. The diagnosis of PTCS, particularly in those without papilledema, remains a controversial topic. Prior diagnostic criteria did not specifically require papilledema, but rather included it among other “symptoms and signs” of high ICP such as headache, nausea or transient visual obscurations (TVOs)—with only one of these features required in order to meet that criterion [8]. The revised diagnostic criteria by Friedman et al., discussed further under Diagnostic Criteria and Evaluation, aimed to avoid over-diagnosis of PTCS by creating more restrictive diagnostic parameters. In the revised criteria, the authors categorise PTCS without papilledema as a distinct entity, but in the absence of papilledema require the presence of an objective physical finding, in addition to elevated CSF opening pressure [2••]. Further epidemiologic studies using the revised clinical criteria would be of interest.
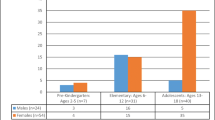
The typical adult patient with PTCS is an obese female of child-bearing age [3, 6, 9]. Conversely, in young children, there is an equal distribution between males and females [10, 11]. In children younger than age 12, weight does not seem to influence the development of primary PTCS, and younger boys especially tend to be thinner. Obesity separates as a risk factor beyond age 12, which may reflect the effect of pubertal status on the pathophysiology of primary PTCS [12,13,14,15]. Risk factors for the development of primary PTCS are detailed in Table 1.
Secondary PTCS likely represents a substantial amount of PTCS cases in children. Older published reports, which included obesity as a cause for secondary PTCS, suggested that up to 53–78% of PTCS cases in children were secondary [3, 16]. More recent studies excluding overweight and obesity suggested that these numbers may be overestimates, and found that only 21–30% of paediatric patients had a secondary aetiology for PTCS [15, 17•]. Nonetheless, this still represents a substantial percentage of children with PTCS; therefore, a thorough diagnostic evaluation for an identifiable secondary cause that may require aetiology-specific management remains of particular importance in this age group. Secondary causes include systemic conditions, genetic conditions, medication use (especially the tetracycline-class antibiotics) and cerebral venous abnormalities [2••]. Conditions associated with the development of secondary PTCS are detailed in Table 2.
Clinical Presentation
The clinical presentation of PTCS in children varies with age, and younger children may have less discernible symptoms. Abnormal findings may be picked up on routine examination, and up to 29% of children with PTCS remain asymptomatic early on [13, 14, 21]. This highlights the need for awareness of these less discernable symptoms and signs in order to ascertain this diagnosis in younger children.
Headache is the most common presenting symptoms of PTCS in children, present in 57–87% of paediatric patients [5, 6, 22•]. The above range in estimated percentage of children presenting with headache relates to whether papilledema was required for diagnosis in each study. In patients with papilledema, the initial presenting symptom may be headache or vision changes, whereas when papilledema is not required for diagnosis, headache is most likely to bring these patients to medical attention. In adult PTCS studies, headache was similarly common, affecting 84% of patients, with 51% reporting a daily or constant headache. In contrast, the characteristics of headache in paediatric PTCS are more widely variable. Headache in PTCS may be daily or constant but also may be entirely episodic, and the pain may be diffuse or focal [23, 24]. Headache in paediatric PTCS is more likely to involve the neck and shoulders, perhaps related to sensitivity towards distention of the spinal root dural sheaths with increased pressure [23]. Importantly, the “classic” high-pressure headache triad of (i) daily headache, (ii) worsening with Valsalva, and (iii) diffuse non-pulsating pain was found to be present in only 36.6% of children with PTCS [23, 25]. Consequently, at the risk of missing the diagnosis, the presence or absence of these “classic” headache features cannot be used as a reliable screen for PTCS in children.
Given the variability in headache phenotype in PTCS, the headache description in PTCS may mimic the primary headaches, especially migraine and tension-type headache. Conversely, these disorders can—and often commonly do—coexist with PTCS, which can further complicate the diagnostic formulation. Other symptoms which may be present in PTCS include nausea and vomiting (12.7–52%) [17•, 21, 25] and back and neck pain (4–8%) [5, 6]. Transient visual obscurations, referring to transient disturbances in binocular or monocular vision lasting < 30 s and often precipitated by position changes or Valsalva due to optic nerve ischemia [26], are slightly less common in paediatric PTCS (16–42.3%) compared with adult PTCS (up to 68%) [27, 28•]. Cranial nerve (CN) deficits can also be seen with PTCS. The most common CN deficit is an abducens (CN VI) palsy, which affects 10–17% of children [5, 22•, 29]. Oculomotor (CN III) and facial nerve (CN VII) palsy have also been reported [30]. Pulsatile tinnitus is reported in only 10% of children with PTCS, but this may be an underestimate, as children may not volunteer this symptom and may not know how to explain it [17•, 31]. Other symptoms reported in adult studies include cerebrospinal fluid (CSF) rhinorrhea, olfactory dysfunction and cognitive impairment [32].
The clinical and diagnostic importance of papilledema in PTCS has been a source of significant interest and controversy in the literature. Papilledema is best evaluated in dilated pupils by an experienced neurologist or ophthalmologist. While papilledema has traditionally been considered the best clinical indictor of increased intracranial hypertension if accurately confirmed, newer studies suggest that up to 18% of patients with symptoms and signs of intracranial hypertension with an elevated opening pressure on lumbar puncture will not have papilledema [11]. The entity of PTCS without papilledema, discussed further below, has been supported by several hypotheses. The threshold to develop papilledema may depend on individual characteristics; in patients with PTCS without papilledema, perhaps their individual threshold to develop papilledema is above their opening pressure. An additional observation put forward is that patients with papilledema tend to have a smaller cup-to-disc ratio. Equally, a larger cup-to-disc ratio may be protective and may offer more resistance to papilledema developing in these patients [24, 33, 34].
Diagnostic Criteria and Evaluation
Over the years there have been multiple different criteria for the diagnosis of PTCS. The modified Dandy criteria, which have been used for multiple studies, permitted the diagnosis of PTCS if either signs (i.e. papilledema) or symptoms (i.e. headache or visual changes) were present [8]. Diagnostic criteria for PTCS in adults and children were revised in 2013 by Friedman et al [2••]. With these criteria, both papilledema and elevated cerebrospinal fluid (CSF) pressure are required for the diagnosis of definite PTCS. Patients with papilledema but with normal opening pressure [35] may be given a diagnosis of probable PTCS, and patients with elevated opening pressure with CN VI palsy or specific imaging findings may be given the diagnosis of PTCS without papilledema [2••]. A diagnostic algorithm for PTCS based on the 2013 revised criteria is outlined in Fig. 1. The criteria do not confer a diagnosis of PTCS to patients with headache and increased CSF pressure who do not have papilledema or other objective signs. These patients are thought not to be at risk for vision loss given the absence of papilledema [25, 32]. However, whether they more closely resemble PTCS or non-PTCS headache disorders in their clinical features and treatment responsiveness is not known. In keeping with the more restrictive nature of the revised criteria, when Inger at al. applied these new criteria to a cohort of children previously diagnosed with PTCS, they found that 62% met criteria for definite PTCS; 20% met criteria for probable PTCS; and 18% did not meet criteria [36]. Gerstl et al. demonstrated similar findings in a paediatric population [37].
The International Classification of Headache Disorders (ICHD), 3rd Edition puts forward criteria for Headache attributed to intracranial hypertension, found under Part Two: The Secondary Headaches, categorised under Headache attributed to increased CSF pressure [38]. The ICHD-3 criteria require a new headache, or a significant worsening of a pre-existing headache, which has developed or significantly worsened in temporal relation to the intracranial hypertension or led to its discovery; and/or a headache accompanied by pulsatile tinnitus. These criteria are slightly different from the 2013 revised PTCS criteria from Friedman et al., in that the ICHD-3 requires elevated opening pressure but does not require papilledema. Improvement in headache following removal of CSF, while previously thought to be a specific sign for headache attributed to intracranial hypertension, is actually of variable sensitivity and specificity (sensitivity 72%; specificity 77%) for PTCS and may also been seen in 10–15% of patients with chronic migraine [25, 38, 39].
History and Examination
Evaluation of a child with suspected PTCS begins with a detailed history and examination. A fundoscopic examination should be performed to evaluate for papilledema. The funduscopic examination may be particularly challenging if not done by a neurologist or ophthalmologist with expertise in evaluating children. Due to the difficulty clinically differentiating between papilledema and pseudo-papilledema, and the high rate of pseudo-papilledema in children, papilledema is often over-diagnosed [30, 33, 40,41,42].
Visual Assessment
Orbital ultrasound and optical coherence tomography (OCT) are useful as ancillary diagnostic tools. OCT, which measures the retinal nerve fibre layer thickness, total retinal thickness and optic nerve head volume, has been shown in adult studies to correlate with the degree of papilledema [43,44,45]. In one paediatric study, OCT was confirmed to accurately identify signs of optic neuropathy and thereby aid in the identification of the patients who may be most vulnerable to long-term morbidity due to vision loss, and who may require more aggressive treatment to preserve vision [46]. In any child with suspected PTCS, a full ophthalmology assessment including perimetry and visual fields should be completed as part of the initial evaluation, to assess for any baseline deficits and identify any imminent risk of visual function [47]. On initial testing, papilledema may result in an enlarged blind spot, peripheral visual field deficits, constriction of the visual field, or nasal steps. Central visual acuity and colour vision become compromised as the papilledema progresses.
Neuroimaging
Neuroimaging is required to confirm normal brain parenchyma in patients with suspected PTCS. In the 2013 revised diagnostic criteria, the authors recommended contrast imaging with either magnetic resonance imaging (MRI) or computerised tomography (CT). MRI is preferable over CT in children to avoid exposure to radiation. Venous imaging is required for further evaluation in atypical cases. In practice, we recommend MRI including venous imaging (either by dedicated venogram or contrast-enhancement) in all males; all pre-adolescent children; and all non-obese adolescent females with suspected PTCS.
The presence of certain imaging features, together with normal parenchyma, can be supportive of a diagnosis of PTCS. In the absence of papilledema and CN VI palsy, the 2013 revised diagnostic criteria require the presence of these imaging features to make a diagnosis of suggested PTCS [2••]. These supportive features include (i) flattening of ocular globe (seen in 56–81%); (ii) distension of the peri-optic subarachnoid space (60–79%) without, or with (iii) tortuosity of the optic nerve (30–68%); (iv) empty sella (30–77%); and transverse venous sinus stenosis [2••, 26, 48, 49]. In children, the most specific of these may be the presence of transverse venous stenosis [50].
Lumbar Puncture
A lumbar puncture to confirm elevated opening pressure should be performed in all patients suspected to have PTCS who do not have a contraindication to the procedure. There has been some debate in the literature about the upper limit of opening pressure in children. In the 2013 revised criteria, the upper limit is considered to be > 28 cm H20 or > 25 cm of H2O in an unsedated or non-obese child [2••, 35]. Other authors have suggested incorporating a lower cut-off of 18 cm H2O for children under age 8 [12, 51]. As opening pressure represents a single measurement, in the context of diurnal and wide variation in cerebrospinal fluid pressure, if the measurement does not fit the clinical picture, it should be interpreted with caution [33, 44]. Additional considerations regarding lumbar puncture in PTCS include patient positioning, and patients should be positioned in the lateral decubitus position. Having the child’s legs flexed vs. extended likely does not make a material difference in influencing the accuracy of the opening pressure [52]. In sedated children, there should be normalisation of end-tidal CO2, as every increase of 1 kPa Co2 can result in a corresponding increase of 3.5–12 cm H20 in opening pressure [53].
For every 0.91 mL of CSF removed, ICP decreases by 1 cm H2O [54]; however, there has been no significant association found between closing pressure, amount of CSF removed, and time to resolution of papilledema in children with PTCS. This suggests that there is not any clear diagnostic or therapeutic value in measuring the closing pressure or maximising the volume of CSF removed when performing a lumbar puncture on a child with suspected PTCS [51, 55].
Other Testing
Other testing considered in the initial evaluation of a child with PTCS should include a complete blood count to exclude anaemia [47]. Additional bloodwork may be considered based on individual presentation (see Conditions Associated with Secondary PTCS, Table 2).
Management
There are no randomised controlled studies to allow for evidence-based recommendations for the management of PTCS in children. The main goals in management are to (i) prevent visual loss and (ii) relieve symptoms of increased pressure, such as headache. Any identifiable secondary cause or underlying risk factor should be addressed and treated. Beyond this, management should be tailored to the individual, and a multi-disciplinary approach is preferred.
Weight Loss
The only disease-modifying treatment for PTCS is weight loss [56]. In adult studies, loss of at least 6% of total body weight is needed for resolution of papilledema [57]. However, weight loss targets in children are likely different, as they are still growing and developing. Any weight loss in an overweight or obese child should be individualised and supported under medical supervision by a paediatrician [58].
Medication
There is a paucity of paediatric data to guide the use of medications in PTCS. In the Idiopathic Intracranial Hypertension Treatment Trial (IIHTT) in adults, acetazolamide was found to yield better visual outcomes and quality of life at 6 months as compared with placebo alone [59,59,61]. In the IIHTT, however, there was no effect of acetazolamide on headache. In a paediatric case series, Tovia et al. found a 76.7% response rate to acetazolamide, including improvement in reported headache [22•]. Side effects of acetazolamide include paresthesia, metallic taste, fatigue, decreased appetite and gastrointestinal upset. Metabolic acidosis has been reported with acetazolamide; however, this is usually mild and asymptomatic.
Adult studies have compared acetazolamide with topiramate using visual outcomes as the primary end point, with significant improvement found in both groups [62]. Topiramate is commonly used and well-tolerated in children for other headache disorders; therefore, it would seem to be a reasonable choice in PTCS, particularly if headache is a prominent feature. Other medications with limited evidence of benefit in PTCS include furosemide, zonisamide and spironolactone [63].
Surgical Interventions
Surgical interventions are considered when there is significant visual loss at onset or evidence of declining visual function. These interventions should be considered as part of the acute management and should not replace long-term management strategies such as weight loss or modification of underlying risk factors. Surgical options most commonly employed in PTCS include optic nerve sheath fenestration; the role of CSF shunting (lumboperitoneal or ventriculoperitoneal) and neurovascular (venous sinus) stenting has not yet been established in adults or children, and carries risk of significant morbidity [34, 64].
Management of Symptoms
In children with headache, the phenotype should be assessed, and treatments should be tailored towards best fitting the patient’s headache phenotype. Non-pharmacologic management strategies such as headache hygiene, lifestyle modifications and behavioural interventions should be optimised. A multi-disciplinary team approach yields best results in managing headaches in this population. Failing optimisation of non-pharmacologic strategies, early introduction of preventive treatments should be considered. Sometimes pressure-lowering medications such as acetazolamide or topiramate can treat the headache, but other times headache preventives are needed in addition to pressure-lowering meds. Caution should be used to avoid or closely monitor any medications that may contribute to weight gain (e.g. amitriptyline), especially if there is comorbid obesity. Education to avoid medication overuse (the use of simple analgesics more than 15 days per month or combined preparations or triptan more than 10 days per month for more than 3 months) can prevent potential worsening of headache as well as side effects. Opioids should be avoided uniformly.
Surveillance
Children with PTCS require close clinical follow-up and diligent visual monitoring. OCT has been used as a tool for monitoring papilledema and may be of additional value in visual surveillance [65]. The optimal duration of treatment for children with PTCS has not been fully established, but should be guided by resolution of papilledema and improvement in clinical symptoms.
Prognosis and Outcomes
The most feared outcome in PTCS is irreversible visual impairment. Permanent visual loss or visual field deficit may occur in up to 20% of children [66]. Visual compromise and severe papilledema at presentation is a predictor of poorer visual outcomes [67]. More favourable prognostic factors suggested in the paediatric literature include male sex, older age at diagnosis, primary PTCS and lack of headache as a clinical feature [68•]. Paediatric recurrence rates are estimated at 18–20% and may be associated with pubertal status. Recurrence with weight gain has been demonstrated in adult studies [69, 70]. This may be considered as a possible risk in children as well, pending further studies to clarify the relationship of weight gain and puberty with recurrence. Papilledema may not be present in recurrent PTCS due to gliotic changes in the retinal nerve fibre layer or subtle optic atrophy; therefore, the clinician should not rely on papilledema alone as a discriminating feature in evaluating a child suspected to have recurrent PTCS.
Conclusion
PTCS is a rare but important disease entity to be aware of in children, with some special considerations in this population. Clinical presentation can be variable in children and may be less obvious than in their adult counterparts. Papilledema can also be challenging to diagnose in this population. The upper limits for opening pressure on lumbar puncture differ in children, with a cut-off of 25 cm H20 (or 28 cm H2O in a sedated or obese child). Morbidity related to visual loss, pain and reduced quality of life lends urgency towards accurately identifying, evaluating and managing children with PTCS.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Friedman DI. The pseudotumor cerebri syndrome. Neurol Clin. 2014;32(2):363–96. https://doi.org/10.1016/j.ncl.2014.01.001.
•• Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–65. https://doi.org/10.1212/WNL.0b013e3182a55f17 The most reently revised diagnostic criteria for PTCS, including criteria for assessing children both with and without the presence of papilledema.
Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumour cerebri: population studies in Iowa and Louisiana. Arch Neurol. 1988;45:875–7.
McCluskey G, Mulholland DA, McCarron P, McCarron MO. Idiopathic Intracranial Hypertension in the Northwest of Northern Ireland: Epidemiology and Clinical Management. Neuroepidemiology. 2015;45(1):34–9. https://doi.org/10.1159/000435919.
Matthews YY, Dean F, Lim MJ, Mclachlan K, Rigby AS, Solanki GA, et al. Pseudotumor cerebri syndrome in childhood: incidence, clinical profile and risk factors in a national prospective population-based cohort study. Arch Dis Child. 2017;102(8):715–21. https://doi.org/10.1136/archdischild-2016-312238.
Gillson N, Jones C, Reem RE, Rogers DL, Zumberge N, Aylward SC. Incidence and Demographics of Pediatric Intracranial Hypertension. Pediatr Neurol. 2017;73:42–7. https://doi.org/10.1016/j.pediatrneurol.2017.04.021.
Bursztyn LL, Sharan S, Walsh L, LaRoche GR, Robitaille J, De Becker I. Has rising pediatric obesity increased the incidence of idiopathic intracranial hypertension? Can J Opthalmol. 2014;49(1):87–91. https://doi.org/10.1016/j.jcjo.2013.09.015.
Smith JL. Whence pseudotumor cerebri? J Clin Neuroophthalmol. 1985;5(1):55–6.
Sheldon CA, Paley GL, Xiao R, Kesler A, Eyal O, Ko MW, et al. Pediatric Idiopathic Intracranial Hypertension: Age, Gender, and Anthropometric Features at Diagnosis in a Large, Retrospective. Multisite Cohort. Ophthalmology. 2016;123(11):2424–31. https://doi.org/10.1016/j.ophtha.2016.08.004.
Standridge SM, O’Brien SH. Idiopathic intracranial hypertension in a pediatric population: a retrospective analysis of the initial imaging evaluation. J Child Neurol. 2008;23(11):1308–11. https://doi.org/10.1177/0883073808318056.
Aylward SC, Aronowitz C, Roach ES. Intracranial Hypertension Without Papilledema in Children. J Child Neurol. 2016a;31(2):177–83. https://doi.org/10.1177/0883073815587029.
Rangwala LM, Liu GT. Pediatric idiopathic intracranial hypertension. Surv Opthalmol. 2007;52(6):597–617.
Cinciripini GS, Donahue S, Borchert MS. Idiopathic intracranial hypertension in prepubertal pediatric patients: characteristics, treatment, and outcome. AM J Opthalmol. 1999;127(2):178–82.
Balcer LJ, Liu GT, Forman S, Pun K, Volpe NJ, Galetta SL, et al. Idiopathic intracranial hypertension: relation of age and obesity in children. Neurology. 1999;52(4):870–2.
Paley GL, Sheldon CA, Burrows EK, Chilutti MR, Liu GT, McCormack SE. Overweight and obesity in pediatric secondary pseudotumor cerebri syndrome. Am J Ophthalmol. 2015;159(2):344–52.e1. https://doi.org/10.1016/j.ajo.2014.11.003.
Phillips PH, Repka MX, Lambert SR. Pseudotumor cerebri in children. J AAPOS. 1998;2(1):33–8.
• Aylward SC, Waslo CS, Au JN, Tanne E. Manifestations of Pediatric Intracranial Hypertension From the Intracranial Hypertension Registry. Pediatr Neurol. 2016b;61:76–82. https://doi.org/10.1016/j.pediatrneurol.2016.04.007 A review of the demographics, clinical features, and interventions in from a large registry database of pediatric patients with PTCS.
Fernándes-García MÁ, Cantarín-Extremera V, Andíon-Catalán M, Duat-Rodríguez A, Jiménez- Echevarría S, Bermejo-Arndeo I, et al. Secondary Intracranial Hypertension in Pediatric Patients With Leukemia. Pediatr Neurol. 2017;77:48–53. https://doi.org/10.1016/j.pediatrneurol.2017.08.013.
Sussman J, leach M, Greaves M, Malia R, Davies-Jones GA. Potentially prothrombotic abnormalities of coagulation in benign intracranial hypertension. J Neurol Neurosurg Psychiatry. 1997;62(3):229–33.
Sodi M, Sheldon CA, Carleton B, Etminan M. Oral fluoroquinolones and risk of secondary pseudotumor cerebri syndrome: Nested case-control study. Neurology. 2017;89(8):792–5. https://doi.org/10.1212/WNL.0000000000004247.
Bassari H, Berkner L, Stolovitch C, Kesaler A. Asymptomatic idiopathic intracranial hypertension in children. Acta Neurol Scand. 2008;118(4):251–5. https://doi.org/10.1111/j.1600-0404.2008.01007.x.
• Tovia E, Reif S, Oren A, Mitelpunkt A, Fattal-Valevski A. Treatment Response in Pediatric Patients With Pseudotumor Cerebri Syndrome. J Neuroophthalmol. 2017;37(4):393–7. https://doi.org/10.1097/WNO.0000000000000516 A retrospective study of 60 pediatric PTCS cases, outlining demographics, clinical characteristics, and treatment outcomes.
Hamedani AG, Witonsky KFR, Cosico M, Rennie R, Xiao R, Sheldon CA, et al. Headache Characteristics in Children With Pseudotumor Cerebri Syndrome, Elevated Opening Pressure Without Papilledema, and Normal Opening Pressure: A Retrospective Cohort Study. Headache. 2018;58(9):1339–46. https://doi.org/10.1111/head.13362.
Moavero R, Sforza G, Papetti L, Battan B, Tarantino S, Vigevano F, et al. Clinical Features of Pediatric Idiopathic Intracranial Hypertension and Applicability of New ICHD-3 Criteria. Front Neurol. 2018;9:819. https://doi.org/10.3389/fneur.2018.00819.
Mathew NT, Ravishankar K, Sanin LC. Coexistence of migraine and idiopathic intracranial hypertension without papilledema. Neurology. 1996;46(5):1226–30.
Cleves-Bayon C. Idiopathic Intracranial Hypertension in Children and Adolescents: An Update. Headache. 2018;58(3):485–93. https://doi.org/10.1111/head.13236.
Dessardo NS, Dessardo S, Sasso A, Sarunic AV, Dezulovic MS. Pediatric idiopathic intracranial hypertension: clinical and demographic features. Coll Antropol. 2010;34(Suppl 2):217–21.
• Smith SV, Friedman DI. The idiopathic intracranial hypertension treatment trial: a review of the outcomes. Headache. 2017;57(8):1303–10. https://doi.org/10.1111/head.13144 A review of the literature and summary of all outcome results from the IIHTT, supporting the use of acetazolamide and weight loss to improve visual outcomes and quality of life in adults.
Reid JE, Reem RE, Aylward SC, Rogers DL. Sixth nerve palsy in paediatric intracranial hypertension. Neuroophthalmology. 2016;40(1):23–7.
Sachdeva V, Vasseneix C, Hage R, et al. Optic nerve head edema among patients presenting to the emergency department. Neurology. 2018;90(5):e373–9. https://doi.org/10.1212/WNL.0000000000004895.
Wall M, Kupersmith MJ, Kieburtz KD, Corbett JJ, Feldon SE, Friedman DI, et al. NORDIC Idiopathic Intracranial Hypertension Study Group. The idiopathic intracranial hypertension treatment trial: clinical profile at baseline. JAMA Neurol. 2014a;71(6):693–701. https://doi.org/10.1001/jamaneurol.2014.133.
Marcelis J, Silberstein SD. Idiopathic intracranial hypertension without papilledema. Arch Neurol. 1991;48(4):392–9.
Fisayo A, Bruce BB, Newman NJ, Biousse V. Overdiagnosis of idiopathic intracranial hypertension. Neurology. 2016;86(4):341–50. https://doi.org/10.1212/WNL.0000000000002318.
Aylward SC, Way AL. Pediatric Intracranial Hypertension: a Current Literature Review. Curr Pain Headache Rep. 2018;22(2):14. https://doi.org/10.1007/s11916-018-0665-9.
Avery RA, Shah SS, Licht DJ, Seiden JA, Huh JW, Boswinkel J, et al. Reference range for cerebrospinal fluid opening pressure in children. N Engl J Med. 2010a;363(9):891–3. https://doi.org/10.1056/NEJMc1004957.
Inger HE, Rogers DL, McGregor ML, Aylward SC, Reem RE. Diagnostic criteria in pediatric intracranial hypertension. J AAPOS. 2017;21(6):492–495.e2. https://doi.org/10.1016/j.jaapos.2017.08.003.
Gerstl L, Schoppe N, Albers L, Ertl-Wagner B, Alperin N, Ehrt O, et al. Pediatric idiopathic intracranial hypertension - Is the fixed threshold value of elevated LP opening pressure set too high? Eur J Paediatr Neurol. 2017;21(6):833–41. https://doi.org/10.1016/j.ejpn.2017.08.002.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. https://doi.org/10.1177/0333102417738202.
Vieira DS, Masruha MR, Goncalves AL, et al. Idiopathic intracranial hypertension with and without papilloedema in a consecutive series of patients with chronic migraine. Cephalalgia. 2008;28(6):609–13. https://doi.org/10.1111/j.1468-2982.2008.01564.x.
Aylward SC, Reem RE. Pediatric Intracranial Hypertension. Pediatr Neurol. 2017;66:32–43. https://doi.org/10.1016/j.pediatrneurol.2016.08.010.
Liu B, Murphy RK, Mercer D, Tychsen L, Smyth MD. Pseudopapilledema and association with idiopathic intracranial hypertension. Childs Nerv Syst. 2014;30(7):1197–200. https://doi.org/10.1007/s00381-014-2390-y.
Kovarik JJ, Doshi PN, Collinge JE, Plager DA. Outcome of pediatric patients referred for papilloedema. J AAPOS. 2015;19(4):344–8. https://doi.org/10.1016/j.jaapos.2015.05.007.
Gilbert AL, Heidary G. Update on the evaluation of pediatric idiopathic intracranial hypertension. Curr Opin Ophthalmol. 2016;27(6):493–7.
Lee YA, Tomsak RL, Sadikovic Z, Bahl R, Sivaswamy L. Use of Ocular Coherence Tomography in Children With Idiopathic Intracranial Hypertension-A Single-Center Experience. Pediatr Neurol. 2016;58:101–106.e1. https://doi.org/10.1016/j.pediatrneurol.2015.10.022.
Phillips PH, Sheldon CA. Pediatric Pseudotumor Cerebri Syndrome. J Neuroophthalmol. 2017;37(Suppl 1):S33–40. https://doi.org/10.1097/WNO.0000000000000548.
Chen JJ, Thurntell MJ, Longmuir RA, Garvin MK, Wang JK, Wall M, et al. Causes and prognosis of visual acuity loss at the time of initial presentation in idiopathic intracranial hypertension. Invest Opthalmol Vis Sci. 2015;56(6):3850–9. https://doi.org/10.1167/iovs.15-16450.
Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018;89(10):1088–100. https://doi.org/10.1136/jnnp-2017-317440.
Lim MJ, Pushparajah k JW, Jan W, Calver D, Lin JP. Magnetic resonance imaging changes in idiopathic intracranial hypertension in children. J Child Neurol. 2010;25(3):294–9. https://doi.org/10.1177/0883073809338874.
Görkem SB, Doğanay S, Canpolat M, Koc G, Dogan MS, Per H, et al. MR imaging findings in children with pseudotumor cerebri and comparison with healthy controls. Childs Nerv Syst. 2015;31(3):373–80. https://doi.org/10.1007/s00381-014-2579-0.
Kohli AA, Vossough A, Mallery R, Woo J, Sheldon CA, Paley GL, McCormack S, Liu G, Szperka CL. MRI Findings in Children with Pseudotumor Cerebri Syndrome (PTCS), Intracranial Hypertension, and Normal Opening Pressure without Papilledema. North American Neuro-Ophthalmology Society 42nd Annual Meetin (poster), Tucson, Arizona. February-March 2016.
Aylward SC. Pediatric idiopathic intracranial hypertension: a need for clarification. Pediatr Neurol. 2013;49(5):303–4. https://doi.org/10.1016/j.pediatrneurol.2013.05.019.
Avery RA, Mistry RD, Shah SS, Boswinkel J, Huh JW, Ruppe MD, et al. Patient position during lumbar puncture has no meaningful effect on cerebrospinal fluid opening pressure in children. J Child Neurol. 2010b;25(5):616–9. https://doi.org/10.1177/0883073809359198.
Lim MJ, Lin JP. The effects of carbon dioxide on measuring cerebral spinal fluid pressure. Child's Nerv Syst. 2009;25(7):783–4. https://doi.org/10.1007/s00381-009-0902-y.
McLaren SH, Monuteaux MC, Delaney AC, Landschaft A, Kimia AA. How Much Cerebrospinal Fluid Should We Remove Prior to Measuring a Closing Pressure? J Child Neurol. 2017;32(4):356–9. https://doi.org/10.1177/0883073816681352.
Beres SJ, Sheldon CA, Boisvert CJ, Szperka CL, Paley GL, Burrows EK, et al. Clinical and Prognostic Significance of Cerebrospinal Fluid Opening and Closing Pressures in Pediatric Pseudotumor Cerebri Syndrome. Pediatr Neurol. 2018;83:50–5. https://doi.org/10.1016/j.pediatrneurol.2018.02.011.
Sinclair AJ, Burdon MA, Nightingale PG, et al. Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: prospective cohort study. BMJ. 2010;341:c2701. https://doi.org/10.1136/bmj.c2701.
Johnson LN, Krohel GB, Madsen RW, March GA Jr. The role of weight loss and acetazolamide in the treatment of idiopathic intracranial hypertension (pseudotumor cerebri). Ophthalmology. 1998;105(12):23137. https://doi.org/10.1016/S0161-6420(98)91234-9.
Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S254–88.
Piper RJ, Kalyvas AV, Young AM, et al. Interventions for idiopathic intracranial hypertension. Cochrane Database Syst Rev 2015:CD003434. doi:https://doi.org/10.1002/14651858.CD003434.pub3
Wall M, McDermott MP, Kieburtz KD, et al. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss. J Am Med Assoc. 2014b;311(16):1641–51. https://doi.org/10.1001/jama.2014.3312.
Bruce BB, Digre KB, McDermott MP, et al. Quality of life at 6 months in the idiopathic intracranial hypertension treatment trial. Neurology. 2016;87:1871–7. https://doi.org/10.1212/WNL.0000000000003280.
Celebisoy N, Gokcay F, Sirin H, Aykyurekli O. Treatment of idiopathic intracranial hypertension: Topiramate vs acetazolamide, an open-label study. Acta Neurol Scand. 2007;116:322–7.
Sheldon CA, Paley GL, Beres SJ, McCormack SE, Liu GT. Pediatric Pseudotumor Cerebri Syndrome: Diagnosis, Classification, and Underlying Pathophysiology. Semin Pediatr Neurol. 2017;24(2):110–5. https://doi.org/10.1016/j.spen.2017.04.002.
Bersani TA, Meeker AR, Sismanis DN, Carruth BP. Pediatric and adult vision restoration after optic nerve sheath decompression for idiopathic intracranial hypertension. Orbit. 2016;35:132–9.
El-Dairi MA, Holgado S, O’Donnell T, et al. Optical coherence tomography as a tool for monitoring pediatric pseudotumor cerebri. J AAPOS. 2007;11:564–70.
Gospe SM 3rd, Bhatti MT, El-Dairi MA. Anatomic and visual function outcomes inpaediatric idiopathic intracranial hypertension. Br J Ophthalmol. 2016;100(4):505–9. https://doi.org/10.1136/bjophthalmol-2015-307043.
Agarwal A, Vibha D, Prasad K, Bhatia R, Singh MB, Garg A, et al. Predictors of poor visual outcome in patients with idiopathic intracranial hypertension (IIH): an ambispective cohort study. Clin Neurol Neurosurg. 2017;159:13–8. https://doi.org/10.1016/j.clineuro.2017.05.009.
• Ravid S, Shahar E, Schif A, Yehudian S. Visual outcome and recurrence rate in children with idiopathic intracranial hypertension. J Child Neurol. 2015;30(11):1448–52. https://doi.org/10.1177/0883073815569306 A retrospective study evaluating the visual outcome and recurrence rate of idiopathic intracranial hypertension in children and clinical predictors for poorer visual outcomes.
Wong R, Madill SA, Pandey P, Riordan-Eva P. Idiopathic intracranial hypertension: the association between weight loss and the requirement for systemic treatment. BMC Opthalmol. 2007;7:15.
Ko MW, Chang SC, Ridha MA, et al. Weight gain and recurrence in idiopathic intracranial hypertension: A case-control study. Neurology. 2011;76(18):1564–7. https://doi.org/10.1212/WNL.0b013e3182190f51.
Funding
Dr. Szperka receives research funding from the National Institute of Health (K23NS102521). There was no specific funding for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Barmherzig declares no conflict of interest. Dr. Szperka has received grant support from Pfizer. Allergan provides consulting payments for work done by Dr. Szperka to the CHOP Paediatric Headache Program.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Childhood and Adolescent Headache
Rights and permissions
About this article
Cite this article
Barmherzig, R., Szperka, C.L. Pseudotumor Cerebri Syndrome in Children. Curr Pain Headache Rep 23, 58 (2019). https://doi.org/10.1007/s11916-019-0795-8
Published:
DOI: https://doi.org/10.1007/s11916-019-0795-8