Abstract
Purpose of Review
Migraine is a disabling and prevalent neurological disease, commonly affecting women during their reproductive years. It is crucial for providers to be able to adequately counsel women who are pregnant, planning pregnancy, or nursing, regarding preventive and abortive treatment options for episodic migraine. This review will discuss (1) the expected course of migraine during pregnancy and the post-partum period, (2) recommended preventive therapies for migraine during pregnancy and lactation, and (3) recommended abortive medications for migraine during pregnancy and lactation.
Recent Findings
Recent research has indicated safety for triptan use during pregnancy and ibuprofen use during the first trimester of pregnancy. Considerations for use of emerging migraine-preventive treatment, such as non-invasive neurostimulators, are discussed.
Summary
For clinical decision-making and patient counseling, it is important to understand both the limitations in determining teratogenic effects in humans and the principles affecting medication transmission from mother to breast milk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 50% of all people with migraine report severe impairment [1]. The prevalence of migraine is more than 17% in women and is highest during ages 30–39, coinciding with reproductive years [1]. Therefore, understanding how to counsel and manage episodic migraine in women who are pregnant, planning pregnancy, or nursing is critical.
Shifts in hormone levels are thought to lead to changes in the number of migraine days experienced by women during pregnancy, the post-partum period, and lactation. A stable estrogen level has a protective effect against pain, which is thought to be secondary to its modulation of neurotransmitters such as serotonin, dopamine, and norepinephrine, as well as endorphins [2]. Rising estrogen levels have correlated with an increase in pain threshold [2]. Estrogen levels rise and stabilize during pregnancy and steeply fall following delivery. Prospective studies have supported the hypothesis that in correlation with increased and stable estrogen levels, migraine symptoms improve during pregnancy [3,4,5]. Other factors, such as avoidance of previously overused medications during pregnancy, may also play a role in migraine improvement [4].
Impact of Migraine During Pregnancy
Improvement in migraine frequency can occur in the first trimester; however, significant improvement typically occurs following the first trimester [3,4,5,6]. In a prospective study, improvement in migraine frequency occurred in up to 83% of women in the second trimester, with complete remission rate increasing from 53 to 79% from the second to third trimester [4]. Among those with migraine with aura, remission occurred in 59% in the second trimester and 66% in the third trimester [5]. The intensity of migraine experienced, as well as the duration of migraine exacerbation, can also improve over the course of pregnancy [4, 7]. Women whose migraine does not improve by the end of the first trimester may be more likely to continue to have migraine for the rest of the pregnancy [3]. About half of patients with headache during pregnancy will have worsening headache in subsequent pregnancies, while in the other half of cases, there will be no impact on headache development during subsequent pregnancies [6]. Parity has not consistently been shown to have any influence on migraine pattern [3, 7]. Fortunately, overall, migraine is not a risk factor for adverse events in pregnancy, labor, fetal survival, or malformations [6, 8••]; however, in comparison with the general population, pregnant women seeking treatment for migraine in an acute care setting have been shown to have a higher rate of preterm delivery and preeclampsia and deliver infants with lower birth weights [9••].
Patients therefore can be counseled that, generally, migraine should not affect their pregnancy or delivery, and that migraine will most likely improve in frequency or remit during pregnancy. Among women whose migraine does not improve by the end of the first trimester, or if they require acute setting care for migraine treatment, preventive treatment may be warranted. In addition, the current pregnancy may require closer surveillance for adverse birth outcomes, and future pregnancies should be monitored for possible worsened headache.
Impact of Migraine During the Post-Partum Period and Breastfeeding
Nearly 40% of all women experience some form of post-partum headache [10]. The post-partum period corresponds with a steep drop in estrogen levels and is characterized by maternal fatigue and stress, which may increase the risk of migraine exacerbation [7, 10]. A prior history of migraine is also a risk factor for post-partum headache ([10]. The prospective MIGRA study, which studied 208 pregnant women with migraine enrolled between 1997 and 1998, showed that there is, in fact, a spike in migraine intensity and duration 1 week post-partum [7]. However, following this time period, women typically return to the migraine frequency and pattern they had during pregnancy [7, 11]. While breastfeeding has been postulated as a protective agent against migraine recurrence, studies have shown that it may not actually have any impact [3, 4, 7, 11].
Therefore, patients can be counseled that while migraine may spike in the first week post-partum, they could expect a return to a pre-delivery migraine pattern. Nursing may or may not be a protective factor [3, 4, 7, 11].
Considerations for Pharmacological Treatment
Choosing a pharmacological option for treating episodic migraine in women who are pregnant, planning to become pregnant, or nursing is challenging. The major concern for pharmacologic treatment during pregnancy is teratogenicity or an exogenous agent’s impact on fetal development and contribution to birth defects. For women who are nursing, medications transmitted to breast milk can have adverse effects on a developing infant.
FDA Recommendations
To help gauge the risk of using a medication during pregnancy, the US Food and Drug Administration (FDA) developed categories delineating potential risk (see Table 1).
However, it should be noted that FDA recommendations are limited. Category labeling does not specify whether recommendations are based on data or lack of data; pregnancy categories also do not indicate at which time in gestation the recommendation should be applied. Studies have shown that FDA categories have little correlation to actual risk of teratogenicity [12, 13].
To improve this system, on June 30, 2015, the FDA implemented the Pregnancy Lactation Labeling Rule (PLLR), which replaces the pregnancy categories with a summary of product information and requires updates to the information [14]. The new labeling will include the following pregnancy risk information for each medication: (1) data on any current pregnancy registries including specific contact information; (2)risk information for the general population about systemic drug absorption based on existing human and animal studies; (3) optional clinical considerations such as recommended dose adjustments during pregnancy, risk of adverse events during labor and delivery, risk of maternal adverse events, or specific risks in the disease population; (4) comprehensive review of scientific literature to support the preceding risk recommendations. The new labeling includes the following lactation risk information for each medication: (1) risk summary regarding systemic absorption with specific information on the known presence of the mediation in breast milk, effects on a breast-fed infant, and effects on breast milk production; (2) optional clinical considerations for infant monitoring and minimizing exposure; and (3) data supporting the preceding recommendations. Examples of labeling following the PLLR can be found at www.fda.gov. The goal of this regulation is to improve counseling and decision-making for pregnant and nursing women. Medications approved after June 30, 2001 may still rely on the older pregnancy category system, although are expected to make labeling changes; however, products approved after June 30, 2015 will use this new system. Other resources are online-computerized teratogenic databases: Teratogen Information System (TERIS), Toxicology Data Network (TOXNET), or non-profit organizations such as the “MotherToBaby” website from the Organization of Teratology Information Specialists.
For clinical decision-making and patient counseling, it is important to understand both the limitations in determining teratogenicity in humans and the impact of when the exposure occurred in the relation to fetal development. Similarly, it is important to understand the principles of how medications are transferred to breast milk and how they may impact a developing infant.
Limitations in Determining Teratogenicity
The prevalence of congenital birth defects can be as high as 8%; 1% of infants have birth defects from drug-related teratogenic effects [15]. Teratogens are identified through animal and human studies; however, these studies have significant limitations, as follows. Given ethical considerations for human research on potential teratogens, results from animal studies are accepted for FDA drug approval. However, animal models are poor predictors of a drug’s teratogenic potential due to inter-species differences in (1) pharmacokinetic and pharmacodynamic profiles, (2) placentation and embryonic development, and (3) predisposition to congenital anomalies [16]. Non-human primates are better models for predicting human teratogenicity. Unfortunately, assessment of teratogenic effects on non-human primates is expensive and therefore occurs rarely. Most recommendations are thus extrapolated from non-primate animal models such as rodents, which are phylogenetically distant from humans [16].
Human studies include case reports and clinical series, as well as epidemiological studies [16]. These observations only take place after a recurrent pattern is identified following numerous exposures. Even then, observations can be limited by recall or reporting bias and misattribution of causality.
It is important to think critically about suspected human teratogens, as misattributing potentially helpful drugs as teratogens could lead to poor treatment of episodic migraine in pregnancy, false litigation, and termination of pregnancy, while false negatives could lead to unnecessary exposure. Teratogens among humans are identified with more certainty if epidemiological and experimental data show reproducibility, consistency, and biological plausibility [16].
Exposure Considerations During Pregnancy
When considering the impact of an exposure to a teratogen, it is also important to understand critical developmental time periods. The time from conception to the time of implantation (theoretically, the first week post-conception) is protected from drug effect, as the blastocyte does not yet have a vascular interface with the mother’s circulation [16]. However, during embryogenesis, which occurs from the time of implantation until about 8 weeks post-conception, teratogens can result in abnormal tissue development or spontaneous abortion [16]. Following this period, during fetal development, teratogenic effects include (1) organ or structural damage, (2) system damage, (3) growth retardation, and (4) fetal death or stillbirth [16]. The effects can occur concomitantly.
Exposure Considerations During Lactation
Human breast milk is recommended for human infants; however, the decision to treat episodic migraine during lactation may be affected by concerns regarding the amount of medication entering human breast milk. Although central nervous system (CNS) active medications can enter breast milk more frequently than non-CNS active medications, only rarely do these medications achieve clinically significant levels in breast milk [17••, 18]. Medications pass into breast milk by passive diffusion from maternal plasma through capillaries into lactocytes, which line the alveolus. By the end of the first week post-partum, medications must go through a bilayer lipid membrane of the alveolar cell in order to enter breast milk.
Therefore, in order to transfer to breast milk, a medication must have (1) a high maternal plasma concentration (the most important factor), (2) low molecular weight, and (3) low protein binding [17••, 18]. In order to have clinical impact on the infant, following passage to breast milk, the medication must still be orally bioavailable to the infant; the infant’s gut, gut wall, or liver can halt absorption of medications [17••, 18]. Of note, medications with longer half-lives can continually build up in an infant’s plasma over time.
To determine how much of a medication to which an infant is exposed, a relative infant dose (RID) can be calculated by dividing the infant’s dose from breast milk (mg/kg/day) by the mother’s medication dose in mg/kg/day. An acceptable range is when the RID is < 10% [17••, 18]. Premature and newborn infants are at greater risk for clinical effects even from small amounts of medications due to low metabolic capacity [17••, 18].
Preventive Treatment During Pregnancy
Lifestyle medications, including optimizing exercise, nutrition, and sleep hygiene, remain the cornerstone of preventive therapy in women with migraine who are pregnant or planning pregnancy [19]. Non-pharmacological approaches, such as relaxation therapy, biofeedback, and acupuncture have also been shown to be beneficial in episodic migraine prevention, without posing risk to fetal development [19].
Supplements and vitamins, or nutraceuticals, may be considered in the preventive treatment of migraine during pregnancy, although large-scale evidence regarding efficacy and safety is limited. Riboflavin (vitamin B2), coenzyme Q10, and magnesium are thought to improve mitochondrial energy metabolism, the dysfunction of which may play a role in migraine exacerbation [20, 21]. Randomized placebo-controlled trials have demonstrated that both riboflavin, at doses of 400 mg daily, and coenzyme Q10, at doses of 100 mg three times a day, taken over a 3-month duration, are more efficacious than placebo in preventing migraine [22, 23]. Both medications have excellent tolerability, with adverse events limited to polyuria, diarrhea, and cutaneous allergy [22, 23]. There are no adverse outcomes reported with coenzyme CoQ10 use during pregnancy; in fact, supplementation of 200 mg of CoQ10 daily during pregnancy has been shown to reduce the risk of developing pre-eclampsia [24]. High-dose riboflavin use however has not been studied during pregnancy, although no adverse events have been described. Studies using a 1-mg supplement of riboflavin, along with other vitamins, have shown a reduced risk of hematological issues such as anemia in pregnant women [25, 26]. Overall, there has not been enough high-quality evidence to determine if magnesium supplementation for the prevention of migraine is beneficial [27, 28]. In a Cochrane review, no increased risk of neonatal death was seen in pregnant women supplemented with magnesium after infants with major congenital abnormalities were excluded [29]. If considering nutraceutical options for migraine prevention during pregnancy, CoQ10 and riboflavin, ideally initiated 3 months prior to pregnancy, may be safe and effective.
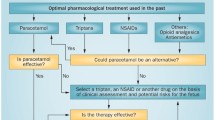
However, in cases of severe migraine during pregnancy or while planning pregnancy, one may need to consider a pharmacologic prophylactic agent. Table 2 reviews the FDA pregnancy categories for medications recommended for migraine prophylaxis [30].
Generally, medications from the anticonvulsant category, such a topiramate or valproic acid, should be avoided. Studies have suggested that anticonvulsants themselves contribute to an increase of congenital malformations seen in the offspring of women with epilepsy [31]. The most common congenital malformations include cleft lip and/or palate as well as congenital heart defects [16, 32]. Valproic acid use during pregnancy has been associated with lower IQ and risk for impaired fine motor development [33, 34].
There is no conclusive evidence that beta-blockers as a class have any adverse events on the fetal development, with the exception of atenolol, which has been associated with low birth weight when taken in the first trimester [35, 36]. If using beta-blocker therapy, the pregnancy should be closely monitored for development of fetal bradycardia, intrauterine growth retardation, respiratory issues, hypoglycemia, and jaundice [16].
There are no randomized placebo-controlled trials on the use of serotonin-norepinephrine reuptake inhibitors (SNRIs) or tricyclic antidepressants (TCAs) during pregnancy. However, a population-based cohort study, database studies, and meta-analysis have shown that SNRIs (venlafaxine and duloxetine) do not have any significant association with total fetal malformations or cardiac malformations [37]. Cohort studies on TCAs, on the other hand, have been associated with increase in total fetal malformations, including cardiac and craniofacial malformations [37]. Overall, during maternal use of antidepressants, the pregnancy should be monitored for fetal and neonatal side effects, including withdrawal symptoms [37, 38]. TCAs may also cause maternal hypotension and tachycardia [37, 38].
The most common recommendation for angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARB) is that they should be avoided in all women during pregnancy, especially during the second and third trimesters. Use of an ACEi or ARB in the second and third trimesters has been associated with fetal malformations, including renal, pulmonary, and skull malformations that can occur [39]. Evidence for malformation risk when this medication class is used during the first trimester is controversial [39].
Clonidine and guanfacine are alpha-2 adrenergic agonists. No large epidemiologic studies have been conducted to assess adverse fetal events resulting from use of these agents during pregnancy. One prospective trial did not show any maternal or fetal adverse events during clonidine use in pregnancy [40].
Cyproheptadine is a piperadine-derived anti-histamine with anticholinergic and antiserotoninergic properties. No human reports have shown adverse fetal events, although there are conflicting results from animal studies [16].
There are several emerging treatments for migraine prevention for which safety of use during pregnancy will need further investigation. The risk during pregnancy while using calcitonin gene-related peptide (CGRP) monoclonal antibodies for migraine prevention will need to be assessed. Notably, the CGRP system is thought to play a role in the maintenance of normal pregnancy, and specifically regulates uteroplacental blood flow and vasculature [41]. Non-invasive neurostimulation, such as vagus nerve stimulation (gammaCore), supraorbital stimulation (Cefaly), and single-pulse transcranial magnetic stimulation (SpringTMS), is another emerging modality of migraine prevention. Although the safety of use during pregnancy is not yet established, animal studies and limited open-label studies have not suggested reproducible adverse effects on fetal development [42•, 43•, 44•]. Memantine is an N-methyl-d-aspartate (NMDA) receptor antagonist that is worth noting given its potential efficacy in migraine prevention and safety during pregnancy. Although its use is limited by lack of FDA approval for migraine treatment and lack of evidence from large-scale studies, a 12-week trial using 10 mg/day memantine showed that it is effective in reducing migraine frequency compared to placebo [45]. Animal studies do not show any teratogenicity at doses that are equivalent to 6 and 21 times the maximum recommended human dose [46]. There is no maternal toxicity or decreased birth weight at doses two times the maximum recommended human dose [46].
Abortive Treatment During Pregnancy
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are commonly used as an abortive treatment for migraine. However, as prostaglandin synthetase inhibitors, they pose a risk for premature closure of the ductus arteriosus during use in the third trimester and are therefore contraindicated during that time. A recent large-scale database study found no adverse impact on pregnancy with first trimester use of ibuprofen [47••]. Of the neuroleptics, metoclopramide has been noted to be safe even during use in the first trimester of pregnancy for acute migraine treatment and is also effective for nausea and vomiting [48] . A recent randomized control trial showed that IV metoclopramide (combined with diphenhydramine for sedation and akathisia prevention) can be an effective option if acetaminophen has failed [49]. Triptans are migraine-specific abortive medications, which have recently been studied for use during pregnancy. A recent prospective observational cohort study of 432 pregnant women exposed to triptans showed no statistically significant adverse outcome on pregnancy or fetal development with triptan exposure during pregnancy [8••]. Of the triptans, sumatriptan had the largest number of studied exposures and is therefore the recommended option [8••]. Eletriptan and frovatriptan had too few exposures to draw conclusive results and require more study [8••].
Preventive Treatment During Lactation
There are several references assigning lactation risk for medications; the below discussion uses Hale’s Lactation Risk Categories from Medications and Mothers Milk (17th edition, last published in 2017). Lactation Risk Categories for drugs recommended for migraine prophylaxis are listed in Table 2 [30]. In addition, a comprehensive review by Hutchinson et al. (2013) compiles the recommendations of several resources regarding medication use for migraine during lactation [50••].
If anticonvulsants are used for migraine prophylaxis, infants may need monitoring for liver function and platelet levels, as well as for sedation [17••]. Breastfeeding is probably compatible with use of topiramate for migraine prophylaxis, although there has been a case report of recurrent watery diarrhea in an infant [51]. Maternal use of valproic acid during breastfeeding should be avoided if possible; there has been one case report of an infant presenting with thrombocytopenic purpura, anemia, and reticulocytosis, which improved following cessation of nursing [52]. Of the beta-blocker family, propranolol is preferred in lactating women, as maternal plasma levels of the medication are exceedingly low [17••]. Beta-blockers should be avoided in mothers or infants with asthma, and infants may need monitoring for bradycardia, hypotension, and weakness [17••]. Long-term exposure has not been studied [17••]. For tricyclic antidepressants, such as amitriptyline and venlafaxine, active metabolites are secreted into breast milk in small amounts [17••, 53]. Infants should be monitored for sedation, poor feeding, and anticholinergic side effects [17••]. ACEi and ARB in general do not transfer into human milk significantly; however, concerns regarding renal toxicity indicate that they should be used with caution in premature infants [17••]. Alpha-2 agonists, such as clonidine, may reduce prolactin secretion and therefore could theoretically reduce milk production [17••]. Cyproheptadine use during breastfeeding of newborns has been contraindicated by the manufacturer due to anti-histamine sensitivity.
Abortive Treatment During Lactation
Of the non-steroidal anti-inflammatory drugs (NSAIDs) studied, ibuprofen is an ideal analgesic as studies have demonstrated that ibuprofen concentrations in breast milk are very low, even at doses of 400 mg every 6 h [17••, 54]. Naproxen, on the other hand, has been associated with adverse effects on infants including drowsiness and vomiting [55]. Aspirin has been associated with Reye’s syndrome and should be avoided [50••]. Regarding commonly used phenothiazines (metoclopramide, procholperazine, and promethazine), there may be a risk of sedation and apnea with the latter two [17••]. Metoclopramide has sometimes been used in lactating women to increase breast milk production [17••].
In terms of triptan use, sumatriptan is the most well studied. Given its low RID (approximately 3.5% for a single dose), and low oral availability, it is not expected to reach clinically significant levels in infant circulation [17••]. Eletriptan also has low levels in breast milk [50••]. Ergotamines are contraindicated in breastfeeding [50••].
Conclusion
The 2015 implementation of the FDA Pregnancy Lactation Labeling Rule underscores the responsibility of providers in interpreting data for clinical decision-making and patient counseling regarding teratogenicity and lactation risk. It is important for clinicians to think critically about pharmacologic options, as medications misattributed as teratogens or as a lactation risk could lead to poor treatment of episodic migraine in pregnancy, while use of true teratogens could lead to unnecessary exposure. Considerations regarding recommended migraine prophylactic medications and selected abortive medication for use in pregnancy and lactation have been discussed above. The use of novel treatments for migraine prevention in pregnancy should accordingly be appraised critically; the emergence of non-invasive neurostimulators may be a promising venue of treatment. Continued research is needed to expand preventive and abortive treatment options available to pregnant and nursing women with episodic migraine.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States data from the American migraine study II. Headache. 2001;41:646–57.
Marcus DA. Interrelationships of neurochemicals, estrogen, and recurring headache. Pain. 1995;62:129–39.
Marcus DA, Scharff L, Turk D. Longitudinal prospective study of headache during pregnancy and postpartum. J Head Face Pain. 1999;39:625–32.
Sances G, Granella F, Nappi RE, Fignon A, Ghiotto N, Polatti F, et al. Course of migraine during pregnancy and postpartum: a prospective study. Cephalalgia. 2003;23:197–205.
Serva WA, Serva VM, de Fátima Costa Caminha M, Figueiroa JN, Albuquerque EC, Serva GB, et al. Course of migraine during pregnancy among migraine sufferers before pregnancy. Arq Neuropsiquiatr. 2011;69:613–9.
Maggioni F, Alessi C, Maggino T, Zanchin G. Headache during pregnancy. Cephalalgia. 1997;17:765–9.
Kvisvik EV, Stovner LJ, Helde G, Bovim G, Linde M. Headache and migraine during pregnancy and puerperium: the MIGRA-study. J Headache Pain. 2011;12:443–51.
•• Spielmann K, Kayser A, Beck E, Meister R, Schaefer C. Pregnancy outcome after anti-migraine triptan use: a prospective observational cohort study. Cephalalgia. 2018;38:1081–92. Importance: Recent study evaluating the teratogenicity of triptans.
• Grossman TB, Robbins MS, Govindappagari S, Dayal AK. Delivery outcomes of patients with acute migraine in pregnancy: a retrospective study. Headache. 2017;57:605–11. Importance: Novel study on pregnancy outcomes for women seeking acute treatment for migraine during pregnancy.
Goldszmidt E, Kern R, Chaput A, Macarthur A. The incidence and etiology of postpartum headaches: a prospective cohort study. Can J Anesth. 2005;52:971–7.
Scharff L, Marcus DA, Turk DC. Headache during pregnancy and in the postpartum: a prospective study. Headache. 1997;37:203–10.
Addis A, Sharabi S, Bonati M. Risk classification systems for drug use during pregnancy: are they a reliable source of information? Drug Saf. 2000;23:245–53.
Sannerstedt R, Lundborg P, Danielsson BR, Kihlström I, Alván G, Prame B, et al. Drugs during pregnancy: an issue of risk classification and information to prescribers. Drug Saf. 1996;14:69–77.
Whyte J. FDA implements new labeling for medications used during pregnancy and lactation. Am Fam Physician. 2016;94:12–3.
Baird PA, Anderson TW, Newcombe HB, Lowry RB. Genetic disorders in children and young adults: a population study. Am J Hum Genet. 1988;42:677–93.
Glistrap LC, Little BB. In: Gilstrap LC, Little BB, editors. Drugs and pregnancy. 2nd ed. New York: Chapman & Hall; 1998.
•• Hale T, Rowe HE. Medications and mothers’ milk. 17th ed. Danvers, MA: Springer Publishing Company, LLC; 2017. Importance: Comprehensive resource for assessing lactation risk for medications.
Hotham N, Hotham E. Drugs in breastfeeding. Aust Prescr. 2015;38:156–9.
Airola G, Allais G, Gabellari IC, Rolando S, Mana O, Benedetto C. Non-pharmacological management of migraine during pregnancy. Neurol Sci. 2010;31:63–5.
Welch KM, Levine SR, D’Andrea G, Schultz LR, Helpern JA. Preliminary observations on brain energy metabolism in migraine studied by in vivo phosphorus 31 NMR spectroscopy. Neurology. 1989;39:538–41.
Welch KMA, Ramadan NM. Mitochondria, magnesium and migraine. J Neurol Sci. 1995;134:9–14.
Schoenen J, Jacquy J, Lenaerts M. Effectiveness of high-dose riboflavin in migraine prophylaxis. A randomized controlled trial. Neurology. 1998;50:466–70.
Shults CW, Beal MF, Fontaine D, Nakano K, Haas RH, Magis D, et al. Absorption, tolerability, and effects on mitochondrial activity of oral coenzyme Q10 in parkinsonian patients. Neurology. 1998;50:793–5.
Teran E, Hernandez I, Nieto B, Tavara R, Ocampo JE, Calle A. Coenzyme Q10 supplementation during pregnancy reduces the risk of pre-eclampsia. Int J Gynecol Obstet Wiley-Blackwell. 2009;105:43–5.
Ma AG, Schouten EG, Zhang FZ, Kok FJ, Yang F, Jiang DC, et al. Retinol and riboflavin supplementation decreases the prevalence of anemia in Chinese pregnant women taking Iron and folic acid supplements. J Nutr Oxford University Press. 2008;138:1946–50.
Ma AG, Schouten EG, Ye Sun Y, Yang F, Xia Han X, Zhi Zhang F, et al. Supplementation of iron alone and combined with vitamins improves haematological status, erythrocyte membrane fluidity and oxidative stress in anaemic pregnant women. Br J Nutr. 2010;104:1655–61.
Teigen L, Boes CJ. An evidence-based review of oral magnesium supplementation in the preventive treatment of migraine. Cephalalgia. 2015;35:912–22.
Pfaffenrath V, Wessely P, Meyer C, Isler HR, Evers S, Grotemeyer KH, et al. Magnesium in the prophylaxis of migraine—a double-blind placebo-controlled study. Cephalalgia. 1996;16:436–40.
Makrides M, Crosby DD, Bain E, Crowther CA. Magnesium supplementation in pregnancy. Cochrane Database Syst Rev. 2014.
Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: table 1. Neurology. 2012;78:1337–45.
Meadow R. Anticonvulsants in pregnancy. Arch Dis Child. 1991;66:62–5.
Kelly TE, Rein M, Edwards P. Teratogenicity of anticonvulsant drugs. IV: the association of clefting and epilepsy. Am J Med Genet. 1984;19:451–8.
Veiby G, Engelsen BA, Gilhus NE. Early child development and exposure to antiepileptic drugs prenatally and through breastfeeding. JAMA Neurol. 2013;70:1367–74.
Meador KJ, Baker GA, Browning N, Cohen MJ, Bromley RL, Clayton-Smith J, et al. Breastfeeding in children of women taking antiepileptic drugs. JAMA Pediatr [Internet]. 2014 [cited 2018 May 19];168:729. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24934501
Bayliss H, Churchill D, Beevers M, Beevers DG. Anti-hypertensive drugs in pregnancy and fetal growth: evidence for “pharmacological programming” in the first trimester? Hypertens Pregnancy. 2002;21:161–74.
Abalos E, Duley L, Steyn DW. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2014;6:CD002252.
Lusskin SI, Khan SJ, Ernst C, Habib S, Fersh ME, Albertini ES. Pharmacotherapy for perinatal depression. Clin Obstet Gynecol [Internet]. 2018;00:1. Available from: https://doi.org/10.1097/GRF.0000000000000365
Miller LJ. Psychopharmacology during pregnancy. Prim Care Update Ob Gyns. 1996;3:79–86.
Quan A. Fetopathy associated with exposure to angiotensin converting enzyme inhibitors and angiotensin receptor antagonists. Early Hum Dev. 2006;82:23–8.
Horvath JS, Phippard A, Korda A, Henderson-Smart DJ, Child A, Tiller DJ. Clonidine hydrochloride—a safe and effective antihypertensive agent in pregnancy. Obstet Gynecol. 1985;66:634–8.
Yallampalli C, Chauhan M, Thota CS, Kondapaka S, Wimalawansa SJ. Calcitonin gene-related peptide in pregnancy and its emerging receptor heterogeneity. Trends Endocrinol Metab. 2002;13:263–9.
• Miller S, Sinclair AJ, Davies B, Matharu M. Neurostimulation in the treatment of primary headaches. Pract Neurol. 2016;16:362–75. Importance: Further reading on neurostimulation options for migraine treatment.
• Bhola R, Kinsella E, Giffin N, Lipscombe S, Ahmed F, Weatherall M, et al. Single-pulse transcranial magnetic stimulation (sTMS) for the acute treatment of migraine: evaluation of outcome data for the UK post market pilot program. J Headache Pain. 2015;16:535. Importance: Further reading on transcranial magnetic stimulation for migraine acute treatment.
• Judkins A, Johnson RL, Murray ST, Yellon SM, Wilson CG. Vagus nerve stimulation in pregnant rats and effects on inflammatory markers in the brainstem of neonates. Pediatr Res. 2018;83:514–9. Importance: Further reading on vagus nerve stimulation for migraine treatment during pregnancy.
Noruzzadeh R, Modabbernia A, Aghamollaii V, Ghaffarpour M, Harirchian MH, Salahi S, et al. Memantine for prophylactic treatment of migraine without aura: a randomized double-blind placebo-controlled study. Headache J Head Face Pain. 2016;56:95–103.
Namenda XR (memantine hydrochloride) capsules label. [cited 2018 Jul 23]; Available from: www.fda.gov/medwatch.
•• Dathe K, Fietz A-K, Pritchard LW, Padberg S, Hultzsch S, Meixner K, et al. No evidence of adverse pregnancy outcome after exposure to ibuprofen in the 1st trimester—evaluation of the national embryotox cohort. Reprod Toxicol. 2018;79:32–8. Importance: Recent study evaluating the teratogenicity of ibuprofen use during the first trimester.
Colman I, Brown MD, Innes GD, Grafstein E, Roberts TE, Rowe BH. Parenteral metoclopramide for acute migraine: meta-analysis of randomised controlled trials. BMJ. 2004;329:1369–73.
Childress KS, Dothager C, Gavard J, Lebovitz S, Mostello D. Metoclopramide and diphenhydramine: a randomized controlled trial of a treatment for headache in pregnancy when acetaminophen alone is ineffective (MAD headache study). Am J Obstet Gynecol [Internet]. 2014;210:S277. https://doi.org/10.1016/j.ajog.2013.10.597.
•• Hutchinson S, Marmura MJ, Calhoun A, Lucas S, Silberstein S, Peterlin BL. Use of common migraine treatments in breast-feeding women: a summary of recommendations. Headache. 2013;53:614–27 Importance: Comprehensive resource for assessing lactation risk for medications.
Westergren T, Hjelmeland K, Kristoffersen B, Johannessen SI, Kalikstad B. Probable topiramate-induced diarrhea in a 2-month-old breast-fed child—a case report. Epilepsy Behav Case Reports. 2014;2:22–3.
Stahl MM, Neiderud J, Vinge E. Thrombocytopenic purpura and anemia in a breast-fed infant whose mother was treated with valproic acid. J Pediatr. 1997;130:1001–3.
Ilett KF, Kristensen JH, Hackett LP, Paech M, Kohan R, Rampono J. Distribution of venlafaxine and its O-desmethyl metabolite in human milk and their effects in breastfed infants. Br J Clin Pharmacol. 2002;53:17–22.
Townsend RJ, Benedetti TJ, Erickson SH, Cengiz C, Gillespie WR, Gschwend J, et al. Excretion of ibuprofen into breast milk. Am J Obstet Gynecol. 1984;149:184–6.
Ito S, Blajchman A, Stephenson M, Eliopoulos C, Koren G. Prospective follow-up of adverse reactions in breast-fed infants exposed to maternal medication. Am J Obstet Gynecol. 1993;168:1393–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Simy K. Parikh declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Episodic Migraine
Rights and permissions
About this article
Cite this article
Parikh, S.K. Unique Populations with Episodic Migraine: Pregnant and Lactating Women. Curr Pain Headache Rep 22, 80 (2018). https://doi.org/10.1007/s11916-018-0737-x
Published:
DOI: https://doi.org/10.1007/s11916-018-0737-x