Abstract
Lidocaine and mexiletine are class 1B antiarrhythmic drugs that act on sodium channels. Lidocaine is also an important anesthetic and topical agent that is useful in the treatment of multiple pain disorders, and mexiletine is commonly used for neuropathic pain and myotonia. Both intravenous lidocaine and mexiletine are increasingly used to treat pain syndromes and appear to be particularly effective in neuropathic pain. This suggests a role for these agents in patients with headache disorders. This article describes the role of intravenous lidocaine and mexiletine in the management of headache and trigeminal autonomic cephalalgias based on the published literature to date and provides practical guidelines for their use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trigeminal autonomic cephalalgias (TACs) are characterized by frequent attacks of unilateral headaches with autonomic features [1]. Cluster headache (CH), short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT), and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA) are TACs that occasionally require emergency treatment. SUNCT and SUNA are especially refractory to treatment with acute analgesics, including opioids [2, 3], and may present with status-like frequency, requiring urgent treatment [4, 5]. Lidocaine and mexiletine are antiarrhythmic medications that appear safe and effective in the treatment of various pain disorders, including neuropathic pain. This article describes the use of intravenous (IV) lidocaine and mexiletine in the treatment of pain, headache, and TACs, such as SUNCT and SUNA, and provides practical guidelines for their use.
Intravenous Lidocaine and Mexiletine: An Overview
Lidocaine and mexiletine are class 1B antiarrhythmic agents and local anesthetics. Drugs in this class work by interfering with sodium channels, depressing phase 0 and shortening the duration of the cardiac action potential [6]. Mexiletine and tocainide, another class 1B drug, are both lidocaine derivatives. Phenytoin, a commonly used anticonvulsant, is also a class 1B medication at high doses, explaining the hypotension and arrhythmias occasionally seen with IV phenytoin infusion [7]. Lidocaine and mexiletine have also been used to treat seizures [8], although at toxic levels they are more likely to cause convulsions.
In the past, clinicians routinely used lidocaine and other antiarrhythmic agents after a myocardial infarction, hoping to suppress ventricular arrhythmias. Clinical trials, however, demonstrated increased mortality and risk of congestive heart failure with the prophylactic use of class 1 antiarrhythmics, including lidocaine, to treat non-life-threatening ectopy after a myocardial infarction [9–12]. No class of antiarrhythmic drugs has been proven to reduce mortality in atrial fibrillation [13], and class 1B agents should be reserved for severe, life-threatening arrhythmias [14]. Antiarrhythmic agents can also have proarrhythmic effects leading to ventricular arrhythmias that may be fatal, although they are relatively uncommon with class 1B drugs [15].
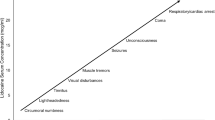
Lidocaine is the prototype class 1B drug, but it has minimal oral bioavailability. Lidocaine has a rapid onset of effect, with a half-life of 1 to 2 h. Lidocaine has hepatic metabolism via the CYP-450 system, and levels and toxicity may increase with potent enzyme inhibitors. β-Blockers, such as propranolol and metoprolol, may decrease clearance and increase toxicity [16]. Only 3% is excreted unchanged in the urine, making IV lidocaine relatively safe for patients with renal disease [17]. A therapeutic plasma level is from 1.5 to 6.0 µg/mL, with toxicity above 7.0 µg/mL. Common adverse events (AEs) include dizziness, bradycardia, paresthesias, perioral numbness, hypo-or hypertension, and tremor. Central nervous system (CNS) AEs, such as convulsions and visual disturbances (including hallucinations), usually occur with elevated plasma levels. Lidocaine produces psychiatric AEs, such as depression, euphoria, agitation with auditory or visual hallucinations, or paranoid ideation, in up to 50% of patients [18]. Allergic reactions, such as rash, are not rare. After IV lidocaine is discontinued, it is rapidly eliminated, with most of the drug gone in about 15 min [19].
Mexiletine is an antiarrhythmic agent that is structurally similar to lidocaine. Unlike lidocaine, it has a low first-pass metabolism, with a systemic bioavailability of about 90%. Peak drug levels occur at 2 to 3 h, and the half-life is 10 to 12 h. Mexiletine is metabolized in the liver via the CYP-450 system, specifically CYP2D6 and CYP1A2. Hepatic impairment, inhibitors of CYP2D6 (including duloxetine, bupropion, fluoxetine, and citalopram), and CYP1A2 inhibitors (eg, verapamil, fluvoxamine, and ciprofloxacin) may increase serum levels and toxicity. Mexiletine interacts with lidocaine by displacing lidocaine from binding sites, increasing levels and toxicity [20]. Metabolites of mexiletine have minimal antiarrhythmic activity [15]. As a local anesthetic, mexiletine is a more potent analgesic than lidocaine [21], but it is not commercially available as a topical agent. Renal disease only slightly increases half-life, as only 10% of the drug is renally excreted. The therapeutic range of mexiletine is 0.5 to 2.0 µg/mL, with toxicity occurring at levels greater than 2.0 µg/mL. Common CNS AEs include dizziness, tremor, incoordination, visual disturbances, and paresthesias. About 40% of patients experience nausea and heartburn [14, 22], and 1% to 2% of patients have elevated hepatic transaminases.
Lidocaine and Mexiletine in the Treatment of Pain
IV lidocaine and mexiletine have been used in the treatment of pain disorders for decades. The primary mechanism of action for both drugs is believed to be related to blocking of voltage-gated sodium channels [23], similar to many headache prophylactic medications that also alter sodium channels. Local anesthetics may have many other actions when given systemically, which can explain their effectiveness in pain. Anesthetics appear to act at opioid receptors [24] and may have synergistic effects when used with opioids [25]. Animal models of peripheral nerve injury suggest that the ectopic discharges that occur after injury and are conducted along sodium channels are suppressed with mexiletine and lidocaine, with no effect on normal nerve conduction [26, 27]. Other proposed actions include inhibiting pain transmission of capsaicin-sensitive afferents [28], inhibiting substance P and bradykinin [29], acting on glycine receptors in the spinal cord, modulating N-methyl-D-aspartic acid receptors [30], and reducing proinflammatory cytokine and complement levels [31]. In these models, lidocaine and mexiletine appear to be effective in treating both acute and chronic neuropathic pain [23].
Since the initial descriptions of IV lidocaine’s success in treating pain [32], it has become more widely used. The most common indication is neuropathic pain, for which IV lidocaine is often effective well beyond the time of infusion [33•]. Mexiletine and IV lidocaine appear effective in the treatment of diabetic neuropathy, including patients who have failed conventional treatments [34–36]. These medications appear especially useful for patients with allodynia [37, 38]. Other proposed uses of either mexiletine or IV lidocaine include the treatment of central pain syndrome [39], fibromyalgia [40], erythromelalgia [41], postoperative pain [42], and positive symptoms in multiple sclerosis [43]. Mexiletine and phenytoin are commonly used for symptomatic myotonia [44]. Although IV lidocaine and mexiletine are closely related medications, it is unclear if patients who respond to treatment with one agent will invariably respond to the other. Effective treatment with IV lidocaine, however, does appear to increase patient acceptance of chronic mexiletine therapy [45].
Intravenous Lidocaine and Mexiletine in Refractory Headache
IV lidocaine is an emerging treatment for refractory headache, but the optimal dose and length of treatment are unclear. Burke [46] reported successful treatment with IV lidocaine doses of 1 mg/kg after an infusion of 90 seconds. Reutens et al. [47] used 1 mg/kg for 2 min (13 patients) or a normal saline placebo (12 patients) for acute migraine. No significant change in pain intensity or nausea was seen at 10 or 20 min. Maciewicz et al. [48] described effective treatment of migraine and CH using a 100-mg injection of IV lidocaine. Jauslin et al. [49] reported that IV lidocaine is often effective in 48 h and may be combined with dihydroergotamine for the treatment of chronic daily headache. Kaube et al. [50] reported that lidocaine at a dose of 2 mg per minute for 2 days resulted in pain freedom for 26% of their patients with chronic daily headache and at least 50% improvement in another 42%. Williams and Stark [51] described the use of IV lidocaine in the treatment of 71 patients with chronic daily headache (usually transformed migraine) and medication overuse headache. The most commonly overused medications were opioids. Subjects received infusions of 2 mg per minute for a mean of 8.7 days, allowing 97% of patients to discontinue the offending medication. At discharge, 90% of patients experienced improvement, and daily headaches were improved in 76% 1 month after discharge. Rosen et al. [52•] reported successful outcomes in a group of 68 patients, including two with chronic CH, using doses ranging from 1 to 4 mg per minute for an average of 8.5 days. Most patients (82%) improved, including the two with CH. Postacoustic neuroma headache [53] and trigeminal neuralgia may also respond to IV lidocaine treatment.
Scott [54] reported using mexiletine for acute headache in a series of 10 patients. Each patient received an infusion of 0.5 to 1.0 mg/kg of lidocaine, followed by mexiletine 200 mg at the time of headache recurrence. All the lidocaine responders improved within 1 h of the mexiletine dose. A recent case series described nine patients with refractory chronic daily headache, including chronic migraine and new daily persistent headache, who responded to mexiletine at doses ranging from 600 to 1500 mg per day. This group included patients who had failed multiple standard headache preventive drugs and patients both with and without previous exposure to lidocaine. Many other patients, however, either did not improve or experienced intolerable AEs on mexiletine [55•]. This suggests that mexiletine is an alternative preventive agent for patients who are truly refractory or for whom IV lidocaine is not practical.
Intravenous Lidocaine in the Treatment of SUNCT and SUNA
SUNCT and SUNA are rare TACs characterized by sudden, short-lasting attacks, usually with a stabbing quality, lasting 5 to 240 seconds. Pain is usually localized to the ocular, periorbital, or temporal region. SUNCT requires the presence of both conjunctival injection and lacrimation, with or without other unilateral autonomic symptoms. Patients with SUNA may experience either conjunctival injection or lacrimation and must have at least one unilateral autonomic symptom [1]. SUNCT and SUNA attacks may consist of single stabs of pain, groups of stabbing pain, or continuous pain with superimposed stabs [56]. The attacks may be episodic with remissions [57] or chronic with no remission unless treated [56]. Interictal pain may occur [58]. Various activities, such as shaving, coughing, or talking, may trigger attacks but, unlike trigeminal neuralgia, most patients do not experience a refractory period [2]. Secondary headaches may mimic SUNCT or SUNA. Secondary causes are usually related to pathology in the posterior fossa or pituitary gland, such as brainstem infarction [59], multiple sclerosis [60], arteriovenous malformation [61], or prolactinoma.
SUNCT or SUNA may occasionally present with status-like exacerbations, with up to 60 attacks in an hour [4]. Occasionally, these patients will require hospitalization to control symptoms, which may prevent them from drinking or chewing. Because simple analgesics and opioids are usually ineffective and most preventive medications, such as lamotrigine, topiramate, or gabapentin, require slow titration, IV lidocaine is an attractive option for more rapid symptom relief.
Matharu et al. [62] described a series of four patients with SUNCT syndrome who had failed multiple preventive treatments but responded rapidly to treatment with IV lidocaine using doses of 2 to 3 mg per minute. Unlike most patients with chronic daily headache, these patients usually experienced complete attack cessation within minutes of an adequate dose. In a follow-up study, Cohen [63•] reviewed the effectiveness of different treatments in 52 patients, 43 with SUNCT and 9 with SUNA. Of the 11 patients with SUNCT and 4 with SUNA who received IV lidocaine, 100% had a moderate to excellent effect. The patients with SUNA remained pain-free for 2 days to 12 weeks after infusion. Williams and Broadley [64] gave lidocaine either as an infusion or subcutaneous injection for episodic and chronic SUNCT or SUNA. Thirteen of the 14 patients, including all 9 patients with chronic forms, had an excellent result, with most patients becoming attack-free. The mean infusion time was longer—6 days for the episodic patients and 8 for the chronic patients. Case reports of dramatic improvement in SUNCT and SUNA have led some to suggest that response to lidocaine can be a diagnostic tool in confirming the diagnosis [65].
Intravenous Lidocaine and Mexiletine: Practical Considerations
IV lidocaine and mexiletine are relatively safe treatments for headache, and IV lidocaine appears particularly effective in SUNCT/SUNA, suggesting an overlap with neuropathic pain syndromes. Due to the lack of other effective acute pain treatments, lidocaine may be the treatment of choice for the most acutely disabled SUNCT or SUNA patients. IV lidocaine is usually reserved for intractable headache in the hospital setting. When using IV lidocaine to treat pain, loading doses are usually not necessary. Obtain a baseline electrocardiogram, liver enzymes, and electrolyte panel before starting the infusion, and correct abnormalities such as hypokalemia.
Given that class 1B agents are relatively safe at these lower doses, the need for cardiac monitoring in patients with no known cardiac disease is uncertain. Some have advocated giving lidocaine as a home infusion [66], and oral mexiletine and phenytoin use does not require monitoring. In our experience, continuous cardiac monitoring is useful to monitor for bradycardia, tachycardia, or hypotension. This is especially important when increasing doses. For bothersome AEs, lower the dose and check the lidocaine level. For CNS AEs, such as hallucinations, discontinue the infusion for 10 to 15 min before restarting.
Mexiletine is typically started at doses of 400 to 600 mg per day in 2 to 3 divided doses every 8 to 12 h using 200-mg tablets. Increase daily doses as tolerated every 2 to 3 days up to 1200 mg per day. Increase more slowly in sensitive patients or those taking enzyme-inhibiting drugs. Mexiletine plasma levels are useful in determining the best daily dose. The dosing conversion from IV lidocaine to mexiletine is unclear, but patients who tolerate IV lidocaine well can probably take a higher mexiletine dose. Due to potential for significant interactions, including neurotoxicity, mexiletine should not be given to patients receiving IV lidocaine [20]. Taking mexiletine with food may reduce the incidence of nausea or heartburn, the most common AEs [22]. CNS AEs, such as visual disturbances or tremor, are often signs of toxicity, and patients should be instructed to hold the drug or reduce the dosage. Doses should initially be taken three times daily, but some patients can eventually dose twice daily, if they tolerate the medication, to improve compliance. Because mexiletine has a peak effect at 2 h, a patient who forgets a dose should not try to make it up by doubling the next dose. Because mexiletine has a narrow therapeutic index and may be difficult to tolerate, the best way to use mexiletine may be as a short-term preventive rescue drug. For patients with SUNCT or SUNA, consider using IV lidocaine or mexiletine on a short-term basis while initiating treatment with lamotrigine, gabapentin, or topiramate [67•].
Conclusions
Evidence has shown that continuous IV lidocaine infusion and oral mexiletine are safe and effective adjunctive medications in the treatment of neuropathic pain and chronic daily headache, including CH and medication overuse. IV lidocaine might be most helpful in CH patients with medication overuse or contraindications to dihydroergotamine. IV lidocaine appears especially useful in the treatment of SUNCT and SUNA and is a good acute treatment option for highly disabled patients with these conditions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 2nd edn. Cephalalgia 2004, 24(Suppl 1):44–54.
Matharu MS, Cohen AS, Boes CJ, Goadsby PJ: Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing syndrome: a review. Curr Pain Headache Rep 2003, 7:308–318.
Malik K, Rizvi S, Vaillancourt PD: The SUNCT syndrome: successfully treated with lamotrigine. Pain Med 2002, 3:167–168.
Montes E, Alberca R, Lozano P, et al.: Status-like SUNCT in two young women. Headache 2001, 41:826–829.
Pareja JA, Caballero V, Sjaastad O: SUNCT syndrome. Status-like pattern. Headache 1996, 36:622–624.
Carson IW, Lyons SM, Shanks RG: Anti-arrhythmic drugs. Br J Anaesth 1979, 51:659–670.
Singh SN, Patrick J, Patrick J: Antiarrhythmic drugs. Curr Treat Options Cardiovasc Med 2004, 6:357–364.
Mori K, Ito H, Toda Y, et al.: Successful management of intractable epilepsy with lidocaine tapes and continuous subcutaneous lidocaine infusion. Epilepsia 2004, 45:1287–1290.
Wyse DG, Morganroth J, Ledingham R, et al.: New insights into the definition and meaning of proarrhythmia during initiation of antiarrhythmic drug therapy from the Cardiac Arrhythmia Suppression Trial and its pilot study. The CAST and CAPS Investigators. J Am Coll Cardiol 1994, 23:1130–1140.
Alexander JH, Granger CB, Sadowski Z, et al.: Prophylactic lidocaine use in acute myocardial infarction: incidence and outcomes from two international trials. The GUSTO-I and GUSTO-IIb Investigators. Am Heart J 1999, 137:799–805.
Pharand C, Kluger J, O’Rangers E, et al.: Lidocaine prophylaxis for fatal ventricular arrhythmias after acute myocardial infarction. Clin Pharmacol Ther 1995, 57:471–478.
Sadowski ZP, Alexander JH, Skrabucha B, et al.: Multicenter randomized trial and a systematic overview of lidocaine in acute myocardial infarction. Am Heart J 1999, 137:792–798.
Nichol G, McAlister F, Pham B, et al.: Meta-analysis of randomized controlled trials of the effectiveness of antiarrhythmic agents at promoting sinus rhythm in patients with atrial fibrillation. Heart 2002, 87:535–543.
Fuster V, Rydén LE, Asinger RW, et al.: ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol 2001, 38:1231–1266.
Manolis AS, Deering TF, Cameron J, Estes NA 3rd: Mexiletine: pharmacology and therapeutic use. Clin Cardiol 1990, 13:349–359.
Ochs HR, Carstens G, Greenblatt DJ: Reduction in lidocaine clearance. Reduction in lidocaine clearance during continuous infusion and by coadministration of propranolol. N Engl J Med 1980, 303:373–377.
Collinsworth KA, Strong JM, Atkinson AJ Jr, et al.: Pharmacokinetics and metabolism of lidocaine in patients with renal failure. Clin Pharmacol Ther 1975, 18:59–64.
Gil-Gouveia R, Goadsby PJ: Neuropsychiatric side-effects of lidocaine: examples from the treatment of headache and a review. Cephalalgia 2009, 29:496–508.
Collinsworth KA, Kalman SM, Harrison DC: The clinical pharmacology of lidocaine as an antiarrhythmic drug. Circulation 1974, 50:1217–1230.
Maeda Y, Funakoshi S, Nakamura M, et al.: Possible mechanism for pharmacokinetic interaction between lidocaine and mexiletine. Clin Pharmacol Ther 2002, 71:389–397.
Tzeng JI, Cheng KI, Huang KL, et al.: The cutaneous analgesic effect of class I antiarrhythmic drugs. Anesth Analg 2007, 104:955–958.
Woosley RL, Wang T, Stone W, et al.: Pharmacology, electrophysiology, and pharmacokinetics of mexiletine. Am Heart J 1984, 107(5 Pt 2):1058–1065.
Mao J, Chen LL: Systemic lidocaine for neuropathic pain relief. Pain 2000, 87:7–17.
Hirota K, Okawa H, Appadu BL, et al.: Interaction of local anaesthetics with recombinant mu, kappa, and delta-opioid receptors expressed in Chinese hamster ovary cells. Br J Anaesth 2000, 85:740–746.
Tejwani GA, Rattan AK, McDonald JS: Role of spinal opioid receptors in the antinociceptive interactions between intrathecal morphine and bupivacaine. Anesth Analg 1992, 74:726–734.
Devor M, Wall PD, Catalan N: Systemic lidocaine silences ectopic neuroma and DRG discharge without blocking nerve conduction. Pain 1992, 48:261–268.
Chabal C, Jacobson L, Mariano A, et al.: The use of oral mexiletine for the treatment of pain after peripheral nerve injury. Anesthesiology 1992, 76:513–517.
Kamei J, Zushida K: Effect of mexiletine on thermal allodynia and hyperalgesia in diabetic mice. Jpn J Pharmacol 2000, 84:89–92.
Hitosugi H, Kashiwazaki T, Ohsawa M, Kamei J: Effects of mexiletine on algogenic mediator-induced nociceptive responses in mice. Methods Find Exp Clin Pharmacol 1999, 21:409–413.
Muth-Selbach U, Hermanns H, Stegmann JU, et al.: Antinociceptive effects of systemic lidocaine: involvement of the spinal glycinergic system. Eur J Pharmacol 2009, 613:68–73.
Herroeder S, Pecher S, Schönherr ME, et al.: Systemic lidocaine shortens length of hospital stay after colorectal surgery: a double-blinded, randomized, placebo-controlled trial. Ann Surg 2007, 246:192–200. (Published erratum appears in Ann Surg 2009, 249:701.)
Bartlettt EE, Hutserani O: Xylocaine for the relief of postoperative pain. Anesth Analg 1961, 40:296–304.
• Carroll I: Intravenous lidocaine for neuropathic pain: diagnostic utility and therapeutic efficacy. Curr Pain Headache Rep 2007, 11:20–24. This review discusses lidocaine in the treatment of chronic neuropathic pain.
Ackerman WE 3rd, Colclough GW, Juneja MM, Bellinger K: The management of oral mexiletine and intravenous lidocaine to treat chronic painful symmetrical distal diabetic neuropathy. J Ky Med Assoc 1991, 89:500–501.
Kastrup J, Petersen P, Dejgård A, et al.: Intravenous lidocaine infusion: a new treatment of chronic painful diabetic neuropathy? Pain 1987, 28:69–75.
Viola V, Newnham HH, Simpson RW: Treatment of intractable painful diabetic neuropathy with intravenous lignocaine. J Diabetes Complications 2006, 20:34–39.
Wallace MS, Magnuson S, Ridgeway B: Efficacy of oral mexiletine for neuropathic pain with allodynia: a double-blind, placebo-controlled, crossover study. Reg Anesth Pain Med 2000, 25:459–467.
Tremont-Lukats IW, Challapalli V, McNicol ED, et al.: Systemic administration of local anesthetics to relieve neuropathic pain: a systematic review and meta-analysis. Anesth Analg 2005, 101:1738–1749.
Attal N, Gaude V, Brasseur L, et al.: Intravenous lidocaine in central pain: a double-blind, placebo-controlled, psychophysical study. Neurology 2000, 54:564–574.
Schafranski MD, Malucelli T, Machado F, et al.: Intravenous lidocaine for fibromyalgia syndrome: an open trial. Clin Rheumatol 2009, 28:853.
Kuhnert SM, Phillips WJ, Davis MD: Lidocaine and mexiletine therapy for erythromelalgia. Arch Dermatol 1999, 135:1447–1449.
Fassoulaki A, Patris K, Sarantopoulos C, Hogan Q: The analgesic effect of gabapentin and mexiletine after breast surgery for cancer. Anesth Analg 2002, 95:985–991.
Sakurai M, Kanazawa I: Positive symptoms in multiple sclerosis: their treatment with sodium channel blockers, lidocaine and mexiletine. J Neurol Sci 1999, 162:162–168.
Cleland JC, Griggs RC: Treatment of neuromuscular channelopathies: current concepts and future prospects. Neurotherapeutics 2008, 5:607–612.
Carroll IR, Kaplan KM, Mackey SC: Mexiletine therapy for chronic pain: survival analysis identifies factors predicting clinical success. J Pain Symptom Manage 2008, 35:321–326.
Burke M: Intravenous lignocaine for migraine headache. Aust Fam Physician 1989,18:1559. (Published erratum appears in Aust Fam Physician 1990, 19:598.)
Reutens DC, Fatovich DM, Stewart-Wynne EG, Prentice DA: Is intravenous lidocaine clinically effective in acute migraine? Cephalalgia 1991, 11:245–247.
Maciewicz R, Chung RY, Strassman A, et al.: Relief of vascular headache with intravenous lidocaine: clinical observations and a proposed mechanism. Clin J Pain 1988, 4:11–16.
Jauslin P, Goadsby PJ, Lance JW: The hospital management of severe migrainous headache. Headache 1991, 31:658–660.
Kaube H, Hoskin KL, Goadsby PJ: Lignocaine and headache: an electrophysiological study in the cat with supporting clinical observations in man. J Neurol 1994, 241:415–420.
Williams DR, Stark RJ: Intravenous lignocaine (lidocaine) infusion for the treatment of chronic daily headache with substantial medication overuse. Cephalalgia 2003, 23:963–971.
• Rosen N, Marmura M, Abbas M, Silberstein S: Intravenous lidocaine in the treatment of refractory headache: a retrospective case series. Headache 2009, 49:286–291. (Published erratum appears in Headache 2009, 49:803.). This is a large review of IV lidocaine in the treatment of chronic daily headache, including CH.
Schere D, Silberstein SD: Intravenous lidocaine infusion for the treatment of post-acoustic neuroma resection headache: a case report. Headache 2009, 49:302–303.
Scott RM: Mexiletine and vascular headaches. N Z Med J 1981, 93:92–93.
• Marmura MJ, Passero FC Jr, Young WB: Mexiletine for refractory chronic daily headache: a report of nine cases. Headache 2008, 48:1506–1510. This is a practical review of mexiletine in the treatment of refractory headache in a tertiary headache clinic.
Cohen AS, Matharu MS, Goadsby PJ: Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) or cranial autonomic features (SUNA): a prospective clinical study of SUNCT and SUNA. Brain 2006, 129:2746–2760.
Pareja JA, Sjaastad O: SUNCT syndrome. A clinical review. Headache 1997, 37:195–202.
Pareja JA, Joubert, J, Sjaastad, O: SUNCT syndrome. Atypical temporal patterns. Headache 1996, 36:108–110.
Penart A, Firth M, Bowen JRC: Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT) following presumed dorsolateral brainstem infarction. Cephalalgia 2001, 21:236.
Vilisaar J, Constantinescu C: SUNCT in multiple sclerosis. Cephalalgia 2006, 26:891.
Bussone G, Leone M, Volta GD, et al.: Short-lasting unilateral neuralgiform headache attacks with tearing and conjunctival injection: the first symptomatic case. Cephalalgia 1991, 11:123.
Matharu MS, Cohen AS, Goadsby PJ: SUNCT syndrome responsive to intravenous lidocaine. Cephalalgia 2004, 24:985–992.
• Cohen AS: Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing. Cephalalgia 2007, 27:824. This is the largest case series of lidocaine to treat SUNCT and SUNA; it also includes an excellent overview of their clinical features.
Williams MH, Broadley SA: SUNCT and SUNA: clinical features and medical treatment. J Clin Neurosci 2008, 15:526–534.
Arroyo AM, Durán XR, Beldarrain MG, et al.: Response to intravenous lidocaine in a patient with SUNCT syndrome. Cephalalgia 2009 Apr 30 (Epub ahead of print).
Ferrini R, Paice JA: How to initiate and monitor infusional lidocaine for severe and/or neuropathic pain. J Support Oncol 2004, 2:90–94.
• Cohen AS, Matharu MS, Goadsby PJ: Trigeminal autonomic cephalalgias: current and future treatments. Headache 2007, 47:969–980. This excellent review of the treatment of TACs provides evidence for each modality.
Disclosure
Dr. Michael J. Marmura has received funding from Merck for clinical research and has received compensation from Cephalon for speaking fees.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marmura, M.J. Intravenous Lidocaine and Mexiletine in the Management of Trigeminal Autonomic Cephalalgias. Curr Pain Headache Rep 14, 145–150 (2010). https://doi.org/10.1007/s11916-010-0098-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-010-0098-6