Abstract
Although for the vast majority of patients with spontaneous intracranial hypotension knowledge of the exact site of the underlying spinal CSF leak is not necessary, it is for patients with recalcitrant symptoms. Such patients may require directed treatments such as percutaneous fibrin glue injections or surgery. A variety of MRI techniques have been shown to be able to detect CSF leaks as well and sometimes better than the “gold standard” – CT-myelography. For unusually rapid CSF leaks – particularly those ventral to the spinal cord – digital subtraction myelography or dynamic CT-myelography are indicated. Some patients with spontaneous intracranial hypotension verified by intracranial MRI are never found to have a spinal CSF leak using current techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spontaneous intracranial hypotension is an important and currently routinely diagnosed cause of new daily persistent headaches, particularly in young and middle-aged adults [1]. Children and the elderly, however, also can be afflicted [2, 3]. The most commonly diagnosed cause of spontaneous intracranial hypotension is a spontaneous spinal cerebrospinal fluid (CSF) leak, often in the setting of a generalized connective tissue disorder [1]. Alternative mechanisms include decreased CSF production, increased CSF absorption, pooling of CSF, and altered spinal dural elasticity. Importantly, there is no evidence to suggest any role of cranial base CSF leaks as the cause of spontaneous intracranial hypotension [4]. Although spontaneous intracranial hypotension is not a rare disorder and there has been a renewed interest in this cause of headaches since its MRI features were described in the early 1990s, an initial misdiagnosis remains common. The cardinal MRI features of spontaneous intracranial hypotension are sagging of the brain, enhancement of the pachymeninges, engorgement of venous structures, pituitary enlargement, and subdural fluid collections (mnemonic, SEEPS) (Table 1) [1]. The decrease of CSF volume in the subarachnoid spaces not only causes sagging of the brain but also manifests itself by a decreased diameter of the optic nerve sheath [5, 6]. Some patients with spontaneous intracranial hypotension have normal brain MRI findings, but the frequency of normal imaging is not really known, because the denominator is undetermined. In some series, as many as 20 % to 30 % of patients with SIH have a normal brain MRI [1].
Typically, a patient with spontaneous intracranial hypotension will present with an orthostatic headache. Associated symptoms are common, such as neck pain, nausea/emesis, hearing, or visual abnormalities, tinnitus, and cognitive abnormalities. Other, less common, manifestations include coma, Parkinsonism, dementia, and ataxia. Cerebellar hemosiderin deposits [7] and even superficial siderosis [8••] have been noted in some patients with spontaneous intracranial hypotension, particularly in patients with large intraspinal ventral CSF collections of long duration. Spinal manifestations, including myelopathy and radiculopathy, also have been reported and are generally due to compression by large intraspinal ventral CSF collections [9].
The spectrum of clinical and radiographic manifestations of spontaneous intracranial hypotension is unusually broad and many patients with documented spontaneous intracranial hypotension do not meet the diagnostic criteria according to the current International Classification of Headache Disorders (ICHD-2) [10]. Therefore, other sets of criteria have been developed to aid physicians with establishing the diagnosis of spontaneous intracranial hypotension [11, 12]. One area of controversy is the presence of spinal meningeal diverticula without associated CSF leak in patients with spontaneous intracranial hypotension. This was originally included as a criterion in a study published in 2008 [11] but this criterion has since been removed [12], because this finding is not specific to patients with spontaneous intracranial hypotension [13]. The presence of spinal meningeal diverticula also is not included in the new soon to be published criteria of the ICHD (ICHD-3). Kranz and colleagues [14] confirmed that meningeal diverticula are not rare in patients without spontaneous intracranial hypotension and reported diverticula in 44 % of controls vs 68 % in patients with spontaneous intracranial hypotension, while the mean number of diverticula was 2.2 in controls and 6.3 in patients with spontaneous intracranial hypotension. These differences were not statistically significant, but the small number of patients in this study (n = 19) makes a type II error likely.
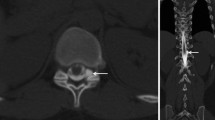
Although spontaneous resolution of spontaneous intracranial hypotension probably is frequent and placement of a lumbar epidural blood patch is a well-known and reasonably effective treatment for spontaneous intracranial hypotension [15, 16], the management of patients with spontaneous intracranial hypotension is not always that straightforward. A variety of treatments may be necessary to adequately control symptoms, such as multiple or directed epidural blood patching, intrathecal saline infusion, percutaneous placement of fibrin sealant, and surgical repair of the underlying CSF leak. Imaging of the spine is not necessary for most patients with spontaneous intracranial hypotension who are cured with routine lumbar epidural blood patching. However, for directed epidural blood patching, percutaneous fibrin glue placement, and surgical CSF leak repair it becomes imperative to image the spine and detect the exact site of the CSF leak.
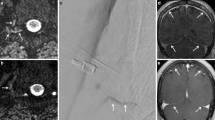
CT-myelography has long been considered to be the gold standard of CSF leak detection, especially compared with radionuclide cisternography and routine spine MRI. In 1 study, for example, only two-thirds of leaks detected on CT-myelography could be visualized on radionuclide cisternography or routine spine MRI [17]. However, heavily T2-weighted MRI (or, MR-myelography) has been shown to be an excellent noninvasive alternative to CT-myelography. Wang and colleagues [18] studied 19 patients with spontaneous intracranial hypotension using both modalities and CSF leaks were detected using CT-myelography in 13 patients. MR-myelography showed identical or very similar CSF leaks in these 13 patients but also identified a CSF leak in 2 (33 %) of 6 patients with normal CT-myelogram results. Intrathecal gadolinium-enhanced MRI (or, MR-myelography with intrathecal gadolinium) may also be superior to CT-myelography. Akbar and colleagues [19••] studied 24 patients with suspected spontaneous intracranial hypotension who had normal CT-myelogram results and detected a CSF leak in 5 patients (21 %) who underwent intrathecal gadolinium-enhanced MRI. Spinal subtraction MRI is a novel technique that shows promise in the evaluation of patients with spontaneous intracranial hypotension [20].
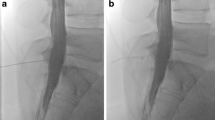
Rapid CSF leaks require specialized imaging because by the time CT or MRI is performed following intrathecal contrast administration, the contrast has already spread over many levels and the exact site of the dural tear remains unknown. On CT and MRI, these rapid CSF leaks usually manifests themselves as extensive longitudinal intraspinal extradural fluid collections, almost always ventral to the spinal cord in location. Digital subtraction myelography is the method of choice in detecting the exact level of the dural defect [21, 22, 23••] (Fig. 1). Hoxworth and colleagues have pioneered this technique for ventral CSF leaks [22, 23••]. Contrast is injected intrathecally and digital subtraction acquisition is performed at a rate of 3–6 frames per second. Resolution of these images is high, but susceptible to motion degradation. Dynamic CT-myelography [24], whereby the contrast is injected intrathecally in the CT scanner, is another technique to localize rapid CSF leaks, but I have found digital subtraction myelography to be superior in detecting the actual site of the dural defect.
Conclusions
Most patients with spontaneous intracranial hypotension do not need spinal imaging prior to treatment and for those who do, a variety of spinal MRI techniques are available. Rapid spinal CSF leaks, usually treated surgically, are best detected with digital subtraction myelography or dynamic CT-myelography.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;19:2286–96.
Schievink WI, Maya MM, Louy C, Moser FG, Sloninsky L. Spontaneous intracranial hypotension in childhood and adolescence. J Pediatr. 2013 (in press).
Schievink WI, Maya MM, Pikul BK, Louy C. Spontaneous spinal cerebrospinal fluid leaks as the cause of subdural hematomas in elderly patients on anticoagulation. J Neurosurg. 2010;112:295–9.
Schievink WI, Schwartz MS, Maya MM, Moser FG, Rozen TD. Lack of causal association between spontaneous intracranial hypotension and cranial cerebrospinal fluid leaks. J Neurosurg. 2012;116:749–54.
Rohr A, Jensen U, Riedel C, van Baalen A, Fruehauf MC, Bartsch T, et al. MR imaging of the optic nerve sheath in patients with craniospinal hypotension. Am J Neuroradiol. 2010;31:1752–7.
Takeuchi N, Horikoshi T, Kinouchi H, Watanabe A, Yagi T, Mitsuka K, et al. Diagnostic value of the optic nerve sheath subarachnoid space in patients with intracranial hypotension syndrome. J Neurosurg. 2012;117:372–7.
Schievink WI, Maya MM, Nuno M. Chronic cerebellar hemorrhage in spontaneous intracranial hypotension: association with ventral spinal cerebrospinal fluid leaks: clinical article. J Neurosurg Spine. 2011;15:433–40.
•• Kumar N. Beyond superficial siderosis: introducing “duraopathies.”. Neurology. 2012;78:1992–9. A superb overview of spinal CSF leaks related to superficial siderosis.
Schievink WI, Chu RM, Maya MM, Johnson JP, Cohen HC. Spinal manifestations of spontaneous intracranial hypotension. J Neurosurg Spine. 2013;18:96–101.
Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. 2nd ed. Cephalalgia 2004;24:1–160.
Schievink WI, Maya MM, Louy C, Moser FG, Tourje J. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. Am J Neuroradiol. 2008;29:853–6.
Schievink WI, Dodick DW, Mokri B, Silberstein S, Bousser MG, Goadsby PJ. Diagnostic criteria for headache due to spontaneous intracranial hypotension: a perspective. Headache. 2011;51:1442–4.
Albayram S, Ozer H, Kara B. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. Am J Neuroradiol. 2008;29:e94.
Kranz PG, Stinnett SS, Huang KT, Gray L. Spinal meningeal diverticula in spontaneous intracranial hypotension: analysis of prevalence and myelographic appearance. Am J Neuroradiol. 2012. [Epub ahead of print].
Sencakova D, Mokri B, McClelland RL. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001;57:1921–3.
Berroir S, Loisel B, Ducros A, et al. Early epidural blood patch in spontaneous intracranial hypotension. Neurology. 2004;63:1950–1.
Schievink WI, Meyer FB, Atkinson JL, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996;84:598–605.
Wang YF, Lirng JF, Fuh JL, Hseu SS, Wang SJ. Heavily T2-weighted MR myelography vs CT myelography in spontaneous intracranial hypotension. Neurology. 2009;73:1892–8.
•• Akbar JJ, Leutmer PH, Schwartz KM, Hunt CH, Diehn FE, Eckel LJ. The role of MR myelography with intrathecal gadolinium in localization of spinal CSF leaks in patients with spontaneous intracranial hypotension. Am J Neuroradiol. 2012;33:535–40. An excellent description of the Mayo Clinic experience with intrathecal gadolinium-enhanced MRI.
Bonetto N, Manara R, Citton V, Cagnin A. Spinal subtraction MRI for diagnosis of epidural leakage in SIH. Neurology. 2011;77:1873–6.
Phillips CD, Kaptain GJ, Razack N. Depiction of postoperative pseudomeningocele with digital subtraction myelography. Am J Neuroradiol. 2002;23:337–8.
Hoxworth JM, Patel AC, Bosch EP, Nelson KD. Localization of a rapid CSF leak with digital subtraction myelography. Am J Neuroradiol. 2009;30:516–9.
•• Hoxworth JM, Trentman TL, Kotsenas AL, Thielen KR, Nelson KD, Dodick DW. The role of digital subtraction myelography in the diagnosis and localization of spontaneous spinal CSF leaks. Am J Roentgenol. 2012;199:649–53. Must read article explaining the “ins and outs” of digital subtraction myelography.
Luetmer PH, Schwartz KM, Eckel LJ, Hunt CH, Carter RE, Diehn FE. When should I do dynamic CT myelography? Predicting fast spinal CSF leaks in patients with spontaneous intracranial hypotension. Am J Neuroradiol. 2012;33:690–4.
Compliance with Ethics Guidelines
Conflict of Interest
Wouter I. Schievink declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Headache
Rights and permissions
About this article
Cite this article
Schievink, W.I. Novel Neuroimaging Modalities in the Evaluation of Spontaneous Cerebrospinal Fluid Leaks. Curr Neurol Neurosci Rep 13, 358 (2013). https://doi.org/10.1007/s11910-013-0358-z
Published:
DOI: https://doi.org/10.1007/s11910-013-0358-z