Abstract
N-methyl-d-aspartate receptor (NMDAR) antibody encephalitis is a recently described immunotherapy-responsive panencephalitis with characteristic features that include a psychiatric onset and a later movement disorder. This entity was first described as a paraneoplastic phenomenon in young women with ovarian teratomata. However, more recently it has become clear that the majority of patients, particularly children, do not harbor a tumor and that males can also be affected. With the development of the NMDAR antibody assay, now available worldwide, a few patients with classical limbic encephalitis and early psychosis and epilepsy have also been found to harbor these antibodies. Early diagnosis followed by immunotherapies and tumor removal, when relevant, expedite recovery from the condition. Antibody levels correlate with the clinical severity of the disease in individual patients, and the antibodies have been shown to substantially reduce NMDA receptors on hippocampal neurons both in vitro and in vivo, supporting the likely direct pathogenicity of the NMDAR antibodies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has long been accepted that some neurologic syndromes are the results of the body’s immune response to a remote tumor—paraneoplastic neurologic syndromes. These conditions are associated with autoantibodies to onconeural antigens. The antibodies provide highly sensitive biomarkers for the associated tumors but are directed against intracellular antigens and do not predict a treatment-responsive, reversible syndrome. Over the past 10 years, however, antibody-mediated central nervous system (CNS) disorders have begun to be diagnosed by identification of antibodies binding to cell-surface neuronal proteins, principally antibodies to the voltage-gated potassium channel complex (VGKC complex) and to the N-methyl-d-aspartate receptor (NMDAR). This has opened up a new era of treatable autoimmune CNS disease.
Since the original description of autoantibodies to the NMDAR 3 years ago, the field has expanded rapidly with more than 600 patients now reported worldwide. NMDAR antibody encephalitis is associated with a wide demographic representation in a paraneoplastic and nonparaneoplastic context, although the majority of patients continue to be younger females. Many highly characteristic features of the typical NMDAR encephalitis are easily recognizable by the bedside, and clinical improvement follows tumor removal, when relevant, and immunosuppressive treatments.
Below, the core clinical features, the associated tumors, the expansion of the phenotypes associated with NMDAR antibodies, the data for mechanisms of direct antibody pathogenicity, and the current therapeutic implications and observations will be reviewed.
Paraneoplastic Origins
In 2007, 12 young (14–44 years of age, median 27 years) female patients were described with a characteristic encephalitis and teratomata [1•]. Features included a viral-like prodrome (headache and fever), prominent psychiatric symptoms, seizures, amnesia, frequent dyskinesias, dysautonomia, and central hypoventilation. The movement disorder is considered a highly characteristic feature with semi-repetitive orofacial and limb movements, opisthotonus, dystonic limb posturing, and oculogyric deviation. Interruption of corticostriatal pathways and disinhibition of brainstem pattern generators were proposed as a possible mechanism for the movements [2]. The dysautonomia causes lability of blood pressure/heart rate and patients have required cardiac pacemaker insertion for prolonged pauses. The sedation and ventilatory requirements of these patients means that many are usually managed in the intensive care unit [3•, 4]. This combination of clinical features should prompt early consideration of this diagnosis.
In Dalmau et al. [1•], the reported teratomata were ovarian in origin in 11 of 12 cases and expressed the NR2 subunit of the NMDA receptor within the neural components. Cerebrospinal fluid (CSF) lymphocytosis was identified in all patients (median 24 cells/μL) and only three patients had normal brain MRI. Eight patients showed improvement or full recovery after tumor resection or immunotherapy; two patients without resection died. It was subsequently reported that, even without tumor resection, protracted recovery was possible [5].
Within 1 year, 100 patients with NMDAR antibodies had been identified and characterized [6••]. All presented with memory or psychiatric symptoms, 54 of 58 cases with tumors had ovarian teratomata, and only 9% of cases were males. Early tumor removal, often with immunotherapy, offered the best outcomes. Serum NMDAR antibody titers were shown to fall in patients who showed clinical improvement. Other tumors have been noted in individual patients, including a teratoma of the mediastinum [1•], teratoma of the testicle [7], sex cord-stromal tumor [6••], Hodgkin’s lymphoma [8], small cell lung carcinoma [9], and neuroblastoma [10].
Nonparaneoplastic Spectrum of Disease and Temporal Progression of Features
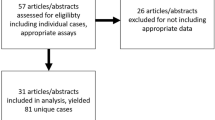
As other groups began to establish methods for NMDAR antibody determination, the spectrum of diseases associated with these antibodies began to expand. The Oxford group, in a consecutive collection of 44 NMDAR antibody-positive cases from the United Kingdom and Europe, found tumors were present in only nine patients (20%, ovarian teratomata in 8 cases). Moreover, they found that males accounted for 25% of all cases [11••]. Non-Caucasians appeared to be represented more frequently than would have been predicted.
A quantitative analysis of the time at onset of the clinical features showed a striking dichotomy observed in the majority of patients (Fig. 1). Neuropsychiatric features and seizures, with probable cortical localization, occurred at disease onset, whereas the features localizable to subcortical structures (movement disorder, dysautonomia, reduction in consciousness, and gaze deviation) occurred at a median of 10 to 20 days later. The time at onset of headache and fever, previously thought to occur prior to neuropsychiatric features, could be divided between a prodromal and a “subcortical” timing of onset. MRI changes were infrequent, seldom involved the temporal lobes, and were sometimes observed in white matter. The clinical observations correlated well with the paraclinical data: epileptiform activity and the rare cortical MRI findings preceded the onset of diffuse slow waves and subcortical white matter MRI changes, also by around 10 to 20 days. Interestingly, the early cortical phase of the disease was associated with CSF lymphocytosis and few oligoclonal bands, whereas later on the lymphocytosis became absent and oligoclonal bands appeared (Fig. 1) [11••]. These phases may correlate well with NMDAR antibodies altering the function of the cortical neurons, in conjunction with a CNS-lymphocyte influx, to produce downstream disinhibition of central pattern generators in the development of the movement disorder [2]. The development of oligoclonal bands during this later phase may represent the generation of multiple antibody specificities within the intrathecal space, but the specificity of the oligoclonal bands for either the NMDAR or other antigens has not yet been demonstrated.
An initial, likely cortical, stage of neuropsychiatric features and seizures, accompanied by electroencephalogram (EEG) spikes and cortical MRI changes is followed, after 10 to 20 days, by a subcortical stage of a movement disorder, dysautonomia, and reduction in consciousness with diffuse slowing on EEG and subcortical MRI changes. MRI changes are absent in around 70% of cases. When present, MRI changes are nonspecific most commonly including white matter T2 hyperintensities. Very few positron emission tomography studies have been reported; one found striatal hypermetabolism and cortical hypometabolism at the time of the extrapyramidal disorder [36]. Cerebrospinal fluid lymphocytosis and absence of oligoclonal bands occur early and these observations reverse later in the disease (data are presented within Irani et al. [11••]). Some patients have an infectious prodrome (headache and fever, usually), which has not been illustrated
It is also clear that many patients with NMDAR antibodies have a relapsing encephalitis. Estimates vary between 15% and 25% [6••, 11••] but patients with a tumor have fewer relapses. A retrospective analysis suggested that relapses occur almost exclusively in patients without adequate immunotherapies during their incident illness [11••]. Prospective studies are required to understand whether more aggressive and early immunotherapies prevent such relapses.
Children with NMDAR Antibodies
Since the original report, a large number of children have been identified with NMDAR encephalitis. Cases as young as 20 months have been reported [12], and over 100 cases under 18 years of age are now described in the literature [11••, 13, 14••]. Their disease is broadly similar to the adult phenotype, but of greatest importance fewer children harbor tumors [11••, 13, 14••, 15, 16]. In this cohort, and in the adult cases without tumors, further studies are required to understand the relative efficacy of available immunotherapies.
Assay Characteristics Used in the Detection of NMDAR Antibodies in CSF and Serum
Table 1 summarizes the main differences between the reported assays. All assays use human embryonic kidney cells, which are transiently transfected with the complementary DNAs encoding NR1 and NR2B subunits of the NMDA receptor, and subsequently incubated with patient sera. Contrary to the initial report [1•], the NR1 subunit is now considered the target subunit [6••, 11••] and commercial assays are being established (Table 1). As the antibodies bind the extracellular domain of the NMDAR, it is not necessary to permeabilize cells before serum incubation, although some laboratories do use permeabilized cells. The clinician needs to check with their immunology laboratory for advice regarding the requirements for the assay and technique used.
Nonpermeabilized cells allow a lower nonspecific background to the assay and the use of higher concentrations of serum (1:10–20 as opposed to 1:200). The lower serum concentrations used by Dalmau et al. (1:200) [6••] may account for the more consistent positivity of CSF samples in their hands. By comparison, the Oxford service usually finds serum (1:20) to give a slightly stronger binding than undiluted CSF, and know of only one of over 60 serum/CSF pairs in which serum was negative while CSF was weakly positive. The serum NMDAR-IgG concentration is consistently higher than the CSF NMDAR-IgG concentration [11••, 14••, 17]; however, there is substantial intrathecal synthesis of NMDAR-IgG with the ratio between serum NMDAR-IgG and CSF NMDAR-IgG being only 13 rather than the 400-fold difference that is found for total IgG [11••]. Thus, even in the nontumor patients, it seems that a peripheral immune response must be the initiating event. However, the relative importance of CSF and serum antibodies in the follow-up of individual patients needs to be determined systematically to judge which compartment is most important in the pathophysiology of the disease.
Broadening Phenotypes Associated with NMDAR Antibodies
As with novel phenotypes appearing in patients with VGKC-complex antibodies [18] and aquaporin-4 antibodies [19], the spectrum of diseases associated with an established autoantibody has expanded for NMDAR antibodies.
Psychosis
Neuropsychiatric features are an early and prominent feature of the NMDAR antibody encephalitis and some patients present directly to psychiatrists [6••, 11••]. More recently, NMDAR antibodies have been detected in a minority of patients with a first episode of psychosis [20•] and in patients with a purely neuropsychiatric disorder [21•]. One patient had a good response to plasma exchange [20•] and a response to electroconvulsive therapy has also been reported [22]. Even if these patients form a small percentage of cases with psychosis, they may represent a subset with an organic diagnosis and potential immunotherapy responsiveness.
Epilepsy
It has become clear that a few patients with a predominant, or pure, epileptic syndrome have NMDAR antibodies [11••, 23, 24]. Some of these patients may also have some subtle psychiatric features and often have a CSF lymphocytosis. Only one of these patients has had a tumor [23] and, interestingly, the four epileptic patients reported by Irani et al. [11••] did not have oligoclonal bands, suggesting a possible restriction of their illness to the early cortical stage of disease. It will be important to further understand whether immunotherapies may be of use in this setting.
Encephalitis Lethargica, Limbic Encephalitis, and Other Encephalitides
Encephalitis lethargica (EL) is a disease of great historical interest that has many features in common with NMDAR antibody encephalitis. One study examined the NMDAR antibody-positivity rate in 20 patients with a diagnosis of EL [14••]. This study found that half the cases had NMDAR antibodies. These were always found at higher concentrations in the serum than CSF. The features that differentiated NMDAR antibody-positive EL from NMDAR antibody-negative EL were early dyskinesias and seizures, both found in the NMDAR antibody-positive group. Although contemporary cases of EL have probably morphed from the classical (von Economo-like) descriptions, it is clear that NMDAR encephalitis is not a new clinical entity [25].
A few studies have reported cases with high medial temporal lobe signal and a clinical diagnosis of limbic encephalitis, in association with NMDAR antibodies [8, 9, 26]. However, VGKC-complex antibodies are much more common in this clinical context [27, 28].
Studies of unselected [29•] and selected [17] cohorts of patients with encephalitis have shown a substantial rate of NMDAR (and VGKC complex) antibody positivity. This furthers the assertion that the clinical entity is not a recent phenomenon and also supports the concept that many noninfectious encephalitides are likely to be of autoimmune origin. The future identification of further antibodies may account for a number of the remaining cases of encephalitis currently of unknown etiology. The fever and headache seen in patients with NMDA antibody encephalitis may create clinical diagnostic dilemma, which can only be resolved with use of the antibody testing. However, as both microbiological and autoantibody positivity can manifest in the same patient [3•], further studies may help identify clinical or laboratory features to determine relative sensitivity to microbiological or immunologic therapies.
Pathophysiology
Antibody Generation
Clinical and scientific evidence supports the likely pathogenicity of the autoantibody response to the NMDARs. Clinically, the presence of a tumor with neural components that express NMDARs provides evidence for a mechanism by which immunologic tolerance may be broken in the paraneoplastic patients, although the process by which this peripherally generated autoantibody accesses the CNS is not understood. Two plausible mechanisms include antibody or B cells traversing the blood–brain barrier. The disruption of the blood–brain barrier may be an initiating event, possibly mediated by the infectious prodrome seen in some patients. The presence of intrathecal NMDAR antibody-secreting plasma cells is supported by the marked intrathecal synthesis of antibody and it is possible that the cells reach the thecal compartment during the lymphocytosis that occurs early in the disease, possibly associated with initial antibody access and chemotactic complement activation. In the nonparaneoplastic patients, it may be there are other stimuli for antibody synthesis and one interesting report has recently suggested that subunits of the NMDAR are expressed by healthy ovaries, possibly explaining the predilection for females even in the nonparaneoplastic cohort [30]. Nevertheless, autoantibody generation at levels sufficient to cause disease may still require a second, currently unknown, stimulus.
Antibody Action
Brain histology has shown IgG deposition, microgliosis, and NR1 cluster depletion [31•, 32, 33]. There has consistently been an absence of complement deposition or expression of cytotoxic markers (eg, Fas/FasL, granzyme B, and perforin). The absence of complement deposition in a disease in which the majority of NMDAR-IgG are of the IgG1 subclass is surprising [11••, 31•]. However, these tissue samples are often taken late in the disease and after a number of potentially disease-modifying agents have been administered; their relevance to the in vivo situation remains unclear.
At a molecular level, there is good in vitro evidence that the NMDAR antibodies are capable of reducing the surface expression (downregulation) of the NMDAR on neurons [6••, 33]. This in vitro effect is reversible with removal of patient NMDAR-IgG. The downregulation may be mediated by the cross-linking of NMDARs by bivalent F(ab) IgG fragments: this mechanism has previously been shown to operate in myasthenia gravis. Interestingly, these antibodies do not mediate downregulation of other glutamate receptors, which are clustered with NMDARs at postsynaptic densities [33]. In vivo, rat hippocampus injections of NMDAR-IgG have been shown to produce a reduction in NMDAR expression [33] and a dose-dependent rise in extracellular glutamate concentrations [34]. The latter paper concluded that the antibodies induced an impairment of glutamatergic transmission. Although these studies now show that the NMDAR-IgG can elicit in vitro and in vivo modulation of molecules involved in excitatory neurotransmission, there are not yet detailed reports of behavioral correlates in rodent models. This finding will be the final proof of direct pathogenicity of NMDAR antibodies.
Treatments: Tumor Removal and Immunotherapies
NMDAR antibody concentrations correlate well with clinical states in individuals and relative changes across a cohort [6••, 11••]. Given this, and the animal and in vitro evidence of direct antibody pathogenicity, the major aim of therapies must be to reduce NMDAR antibody levels to avoid the significant potential mortality and morbidity of the untreated condition. In addition, a number of symptomatic therapies may be useful in the management of disease complications such as seizures, the hyperkinetic movement disorder, and cardiac asystole.
Reduction of NMDAR antibody levels may be achieved in paraneoplastic patients by tumor chemotherapies and removal. In addition, immunotherapies appear to hasten the response. Commonly used immunotherapies in the acute phase of the illness have included corticosteroids, intravenous immunoglobulins, plasma exchange, rituximab, and cyclophosphamide. Tumor removal, often with immunotherapies, produced a substantial reduction in NMDAR antibody levels, with early tumor removal showing the best outcomes [6••, 11••]. Delayed tumor removal may only have a beneficial effect after some months.
In the nonparaneoplastic cases, immunotherapies are administered using varying regimens by individual clinicians. However, more aggressive immunotherapies are required in the nonparaneoplastic cohort as their outcome is usually worse than the paraneoplastic cases [6••, 11••]. The one study to attempt to address the issue of immunotherapies systematically showed that late immunotherapy administration (after 40 days of symptom onset) has little advantage over no immunotherapies [11••]. This study also showed that among the patients administered early immunotherapies, there was a trend toward greater improvements in those given multiple immunotherapies [11••]. There are no established guidelines but attending clinicians have commonly used pulsed intravenous methylprednisolone (eg, 1 g for 3 days) followed by high-dose oral prednisolone, with addition of plasma exchange and/or intravenous immunoglobulins. If no improvement is seen in the subsequent weeks, rituximab and cyclophosphamide are considered. Once discharged from the hospital, high-dose prednisolone is tapered over 6 to 12 months. The concept of early and aggressive immunotherapy fits with the observational data regarding frequent relapses in patients offered limited immunotherapies [11••]. It may be that longer prednisolone regimens and azathioprine or methotrexate as long-term steroid-sparing agents reduce the frequency of relapses.
Conclusions
NMDAR antibodies are not an uncommon cause of encephalitis in younger adults. The disease is clinically distinctive with a psychiatric onset followed by orofacial/limb dyskinesias and dysautonomia, which may represent a cortical to subcortical transition in the disease localization. It is associated with a tumor in around one third of cases, often an ovarian teratoma that expresses the NMDAR. However, tumors are less common in children with the condition and in patients who have a relapsing course. The frequency of relapses and the poor outcomes from the condition are reduced with the use of immunotherapies. It is likely that early and aggressive immunotherapies offer better outcomes but these may have unacceptable side-effect profiles, particularly in the young female population often affected by the disease. With an expansion in the range of phenotypes associated with NMDAR antibodies, it has become clear that some cases of relatively pure epilepsy and psychosis may be immunotherapy-responsive. Although good in vitro evidence exists for NMDAR antibody pathogenicity, the definitive proof of a behavioral correlate in an animal model is still awaited.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Dalmau J, Tüzün E, Wu HY, et al.: Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007, 61:25-36. The original description of NMDAR antibodies in 12 young women with teratomata.
Kleinig TJ, Thompson PD, Matar W, et al. The distinctive movement disorder of ovarian teratoma-associated encephalitis. Mov Disord. 2008;23:1256–61.
• Davies G, Irani SR, Coltart C, et al.: Anti-N-methyl-D-aspartate receptor antibodies: a potentially treatable cause of encephalitis in the intensive care unit. Crit Care Med 2010, 38:679-82. NMDAR encephalitis is a frequent occurrence in a tertiary intensive care unit setting.
Varvat J, Lafond P, Page Y, et al. Acute psychiatric syndrome leading young patients to ICU: consider anti-NMDA-receptor antibodies. Anaesth Intensive Care. 2010;38:748–50.
Iizuka T, Sakai F, Ide T, et al. Anti-NMDA receptor encephalitis in Japan: long-term outcome without tumor removal. Neurology. 2008;70:504–11.
•• Dalmau J, Gleichman AJ, Hughes EG, et al.: Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008, 7:1091-8. This is a comprehensive clinical study of 100 cases with NMDAR antibodies confirming a predominantly paraneoplastic disease with a high rate of ovarian teratomata.
Eker A, Saka E, Dalmau J, et al. Testicular teratoma and anti-N-methyl-D-aspartate receptor-associated encephalitis. J Neurol Neurosurg Psychiatry. 2008;79:1082–3.
Zandi MS, Irani SR, Follows G, et al. Limbic encephalitis associated with antibodies to the NMDA receptor in Hodgkin lymphoma. Neurology. 2009;73:2039–40.
Graus F, Saiz A, Lai M, et al. Neuronal surface antigen antibodies in limbic encephalitis: clinical-immunologic associations. Neurology. 2008;71:930–6.
Lebas A, Husson B, Didelot A, et al. Expanding spectrum of encephalitis with NMDA receptor antibodies in young children. J Child Neurol. 2010;25:742–5.
•• Irani SR, Bera K, Waters P, et al.: N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 2010, 133:1655-67. This European study provided a temporal analysis of the clinical and paraclinical features of NMDAR encephalitis and showed that the majority of unselected cases were nonparaneoplastic.
Wong-Kisiel LC, Ji T, Renaud DL, et al. Response to immunotherapy in a 20-month-old boy with anti-NMDA receptor encephalitis. Neurology. 2010;74:1550–1.
Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66:11–8.
•• Dale RC, Irani SR, Brilot F, et al.: N-methyl-D-aspartate receptor antibodies in pediatric dyskinetic encephalitis lethargica. Ann Neurol 2009, 66:704-9. This is a study showing that 10 of 20 patients previously diagnosed with EL had NMDAR antibodies. The NMDAR-antibody patients were clinically different with higher rates of early dyskinesias and seizures.
Agrawal S, Vincent A, Jacobson L, et al. Successful treatment of antiN-methyl-d-aspartate receptor limbic encephalitis in a 22-monthold child with plasmapheresis and pharmacological immunomodulation. Arch Dis Child. 2010;95:312.
Biancheri R, Pessagno A, Baglietto MG, et al. Anti-N-methyl-D-aspartate-receptor encephalitis in a four-year-old girl. J Pediatr. 2010;156:332–4.
Prüss H, Dalmau J, Harms L, et al. Retrospective analysis of NMDA receptor antibodies in encephalitis of unknown origin. Neurology. 2010;75:1735–9.
Irani SR, Michell AW, Lang B, et al.: Faciobrachial dystonic seizures precede Lgi1-antibody limbic encephalitis. Ann Neurol 2011 (in press)
Wingerchuk DM, Lennon VA, Lucchinetti CF, et al. The spectrum of neuromyelitis optica. Lancet Neurol. 2007;6:805–15.
• Zandi MS, Irani SR, Lang B, et al.: Disease-relevant autoantibodies in first episode schizophrenia. J Neurol 2010 Oct 26. [Epub ahead of print] A minority of patients with first episode psychosis may have NMDA/VGKC complex antibodies.
• De Nayer AR, Myant N, Sindic CJ: A subacute behavioral disorder in a female adolescent. Autoimmune anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Biol Psychiatry 2009, 66:e13-4. NMDAR antibodies can associate with a pure neuropsychiatric syndrome.
Braakman HM, Moers-Hornikx VM, Arts BM, et al. Pearls & Oy-sters: electroconvulsive therapy in anti-NMDA receptor encephalitis. Neurology. 2010;75:e44–6.
Niehusmann P, Dalmau J, Rudlowski C, et al. Diagnostic value of N-methyl-D-aspartate receptor antibodies in women with new-onset epilepsy. Arch Neurol. 2009;66:458–64.
Vincent A, Irani SR, Lang B. The growing recognition of immunotherapy-responsive seizure disorders with autoantibodies to specific neuronal proteins. Curr Opin Neurol. 2010;23:144–50.
Tardieu M. Anti-N-Methyl-D-aspartate receptor encephalitis: a new entity? Dev Med Child Neurol. 2010;52:410–1.
Novillo-López ME, Rossi JE, Dalmau J, Masjuan J. Treatment-responsive subacute limbic encephalitis and NMDA receptor antibodies in a man. Neurology. 2008;70:728–9.
Vincent A, Buckley C, Schott JM, et al. Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain. 2004;127:701–12.
Irani SR, Alexander S, Waters P, et al. Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan's syndrome and acquired neuromyotonia. Brain. 2010;133:2734–48.
• Granerod J, Ambrose HE, Davies NW, et al; on behalf of the UK Health Protection Agency (HPA) Aetiology of Encephalitis Study Group: Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 2010, 10:835-844. A community-based study that showed autoimmune encephalitides are a common cause of encephalitis in the United Kingdom. VGKC-complex and NMDAR antibodies were the third most common cause of encephalitis.
Tachibana N, Shirakawa T, Ishii K, et al. Expression of various glutamate receptors including N-methyl-D-aspartate receptor (NMDAR) in an ovarian teratoma removed from a young woman with anti-NMDAR encephalitis. Intern Med 2010;49:2167–73.
• Tüzün E, Zhou L, Baehring JM, et al.: Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol 2009, Aug 14 [Epub ahead of print]. This is a histologic study of ovarian teratomata and brains from patients with NMDAR antibody encephalitis.
Camdessanché JP, Streichenberger N, Cavillon G, et al.: Brain immunohistopathological study in a patient with anti-NMDAR encephalitis. Eur J Neurol 2010 Aug 16. [Epub ahead of print]
Hughes EG, Peng X, Gleichman AJ, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci. 2010;30:5866–75.
Manto M, Dalmau J, Didelot A, et al. In vivo effects of antibodies from patients with anti-NMDA receptor encephalitis: further evidence of synaptic glutamatergic dysfunction. Orphanet J Rare Dis. 2010;5:31.
Wandinger KP, Saschenbrecker S, Stoecker W, Dalmau J: Anti-NMDA-receptor encephalitis: A severe, multistage, treatable disorder presenting with psychosis. J Neuroimmunol 2010, Oct 14. [Epub ahead of print]
Maeder-Ingvar M, Prior JO, Irani SR, et al.: FDG-PET hyperactivity in basal ganglia correlating with clinical course in anti-NDMA-R antibodies encephalitis. J Neurol Neurosurg Psychiatry. 2010 Oct 29. [Epub ahead of print]
Acknowledgment
S.R. Irani was supported by the National Institute of Health Research (NIHR), Department of Health, United Kingdom.
Disclosure
Conflicts of interest: S.R. Irani: royalties may be available in the future for Caspr2 and Lgi1 antibody testing; A. Vincent: has been a consultant for Athena Diagnostics, receives a part-time salary from University of Oxford and University College London, has received a grant from Euroimmun AG and from NIHR United Kingdom for development of antibody assays, and royalties may be available in the future for Caspr2 and Lgi1 antibody testing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Irani, S.R., Vincent, A. NMDA Receptor Antibody Encephalitis. Curr Neurol Neurosci Rep 11, 298–304 (2011). https://doi.org/10.1007/s11910-011-0186-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-011-0186-y