Abstract
Purpose of Review
The goal of this review is to provide an update on the epidemiology, diagnosis, and treatment of opportunistic fungal infections in patients with human immunodeficiency virus (HIV) infection including Cryptococcus spp., Histoplasma spp., Coccidioides spp., and Talaromyces marneffei, formerly Penicillium marneffei.
Recent Findings
In many settings, despite increasing roll out of antiretroviral therapy (ART), opportunistic invasive mycoses produce a substantial burden of disease. The prevalence of specific fungal pathogens depends on their endemicity. Viral suppression achieved by greater access to ART and increased the availability of point-of-care testing with rapid diagnostic tests (RDTs) aid to curtail the associated fungi morbidity. RDTs allow earlier screening to preemptively initiate treatment of opportunistic fungal pathogens. Identifying asymptomatic cryptococcal infection before starting ART is crucial in reducing the risk of the immune reconstitution inflammatory syndrome (IRIS).
Summary
There is an urgent need to decrease the burden of opportunistic invasive fungal infections in individuals with HIV/AIDS through different interventions: (a) continue to expand the deployment of ART to the most affected populations to achieve viral suppression; (b) ensure early diagnosis of fungal pathogen with point-of-care testing; (c) improve fungal diagnostic capacity in areas with the highest burden of AIDS-related mycoses; and (d) increased availability of existing antifungal drugs to optimally treat these infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungi comprise a vast and diverse group of microorganisms, but only a limited number of fungal species are considered human pathogens. Mycoses are usually acquired when these organisms or their spores are inhaled or implanted into skin wounds. Severe clinical manifestations or disseminated disease occur mostly among those with immunosuppression [1]. In this context, environmental exposure of endemic mycoses, due to their ubiquitous nature, plays a key role in the development of invasive fungal diseases in human immunodeficiency virus (HIV)-infected individuals [2]. The multifactorial interaction between HIV and the host 2 immune system is quite complex resulting in variable rates of progression to the acquired immunodeficiency syndrome (AIDS) [2]. All cell lines of immunity, including lymphocytes, antigen presenting cells, and natural killer cells, are affected. The progressive depletion of CD4 cells leads to the hallmark immunological failure that occurs in HIV [2]. As a result, infected individuals are at a significantly increased risk of developing a variety of opportunistic infections (OIs) including systemic invasive mycoses. Fungal colonization or latent infection prior to HIV infection may result in reactivation as HIV-induced immunosuppression progresses in the absence of ART [3]. Individuals may also become newly exposed to any of these fungal pathogens and develop primary progressive disease [3].
In this review, we provide an in-depth review of recent literature on opportunistic fungal infections in HIV-infected patients with emphasis on infections caused by Cryptococcus spp., Histoplasma spp., Coccidioides spp., and Talaromyces marneffei, formerly Penicillium marneffei (Table 1).
Epidemiology, Clinical Manifestations, and Treatment of Opportunistic Fungal Infections
HIV-infection was described with the identification of the epidemic of Pneumocystis jiroveci pneumonia (PCP) in the early 1980s among men who had sex with men (MSM) in major cities in North America [4, 5]. More than 30 years later, and in many settings, this fungal pathogen continues to impose a substantial burden of disease in HIV-infected individuals. Simultaneously, other AIDS-related mycoses including cryptococcosis, histoplasmosis, coccidiodomycosis, and talaromycosis also remain leading OIs in those with advanced HIV-immunosuppression (CD4 cell count < 100 cells/mm3) [6, 7]. Superficial and invasive Candida infections also contribute to a substantial burden of disease in HIV-infected persons [8••]. Emerging fungal pathogens may also produce disseminated disease in HIV-infected individuals including Emmonsia spp. in South Africa (recently renamed Emergomyces) which mimics disseminated histoplamosis or disseminated sporotrichosis caused by Sporothrix schenckii.
Despite advances in the treatment of HIV-infection with highly effective and safer antiretroviral therapy combinations and scale-up of ART [9], many individuals continue to progress to advanced HIV-associated immunosuppression [10•]. Invasive mycoses associated with HIV-infection pose two major surveillance challenges: the insidious natural history of disease reduces our ability to precisely define the epidemiology of AIDS-related mycoses and the limited diagnostic capacity in the most disease-stricken areas [10•, 11••]. Some recent estimates suggest that there are approximately one million cases of AIDS-associated invasive mycoses annually, with more than 500,000 deaths [10•, 11••]. There is increasing evidence that the major AIDS-related mycoses (cryptococcosis, pneumcystosis, histoplasmosis, and talaromycosis) contribute in some settings to mortality rates at nearly the same rate as those of tuberculosis [10•, 11••].
Cryptococcosis
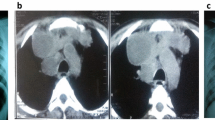
Cryptococcus neoformans and C. gattii are the two species capable of causing human disease in HIV-infected patients with advanced disease (CD4 cell count < 100 cells/mm3) [12, 13]. C. neoformans found throughout the world accounts for the majority of cases [14]. C. gattii has been isolated from a variety of plants in Australia, British Columbia, Canada, and the Pacific Northwest of the USA, but with recent expansion throughout the rest of the USA [15]. Inhalation of spores may result in pulmonary disease or disseminate via hematogenous route to the subarachnoid space and the Virchow-Robin space leading to meningitis or meningoencephalitis (Fig. 1) [12, 15]. Worldwide, one million cases of cryptococcal meningoencephalitis are diagnosed with more than 600,000 deaths annually [16]. Currently, cryptococcosis is considered an OI as prevalent, if no more prevalent, than tuberculosis in sub-Saharan Africa. Cryptococcosis substantially contributes to AIDS-associated deaths [10•, 11••, 16, 17].
Gram-staining of CSF of an HIV-infected individual with advanced immunosuppression (CD4 5 cells/mm3) demonstrating multiple encapsulated yeasts (oil inmersion 10 × 100) consistent with Cryptococcus spp. Culture yielded C. neoformans and the Cryptococcal antigen titer in cerebrospinal fluid were > 1:2240 dilutions
Due to the overwhelming burden of disease, attention has been placed on developing rapid diagnostic tests (RDTs) to improve prevention and treatment of cryptococcal disease in HIV-infected patients. Recently, researchers introduced a cryptococcal antigen (CrAg) test utilizing point-of-care lateral flow diagnostic assays (LFA) to detect cryptococcal capsular polysaccharide antigens, particularly glucuronoxylomannan (GXM). This test can be used on urine, blood, serum, or CSF samples [18]. CrAg LFA is comparable to cultures, latex agglutination, and enzyme-linked immunosorbent assay (ELISA) with sensitivity and specificity of 93–100% and 93–98%, respectively [19,20,21,22]. Identification of CrAg correlates with fungal burden and is detectable in serum for weeks to months prior to the development of meningoencephalitis, allowing for early detection and preemptive treatment with fluconazole [17, 23]. This intervention was associated with improved survival compared to CrAg-positive individuals who only received ART [24, 25]. Notably, the World Health Organization (WHO) and the US Department of Health and Human Services now endorse and recommend this strategy [26, 27]. Limitations to CrAg exist—although are minimal—as false-negative tests have been associated with low fungal burden, prozone reaction with high CrAg titers (> 1:256), immune complexes, inappropriate specimen handling, or infection with hypocapsular or acapsular strains of Cryptococcus spp. [28,29,30,31].
Treatment principles remain unchanged for cryptococcal meningoencephalitis including three sequential phases of antifungal therapy coupled with drainage of CSF via therapeutic lumbar punctures (LPs) or through the insertion of a lumbar drain or ventriculostomy (Table 2) [27]. An evaluation of combination therapy for cryptococcal meningoencephalitis recently found reduced mortality in patients treated with amphotericin B and flucytosine compared to those treated with amphotericin B alone (15 vs. 25 deaths by day 14; hazard ratio [HR], 0.57; 95% confidence interval [CI], 0.30 to 1.08; unadjusted P = 0.08; and 30 vs. 44 deaths by day 70; HR, 0.61; 95% CI, 0.39 to 0.97; unadjusted P = 0.04) [32 ]. Combination therapy with amphotericin B plus fluconazole did not improve survival compared to amphotericin B alone (HR for death by 14 days, 0.78; 95% CI, 0.44 to 1.41; P = 0.42; HR for death by 70 days, 0.71; 95% CI, 0.45 to 1.11; P = 0.13). Sterilization of CSF measured by rates of yeast clearance was significantly faster for patients treated with amphotericin B plus flucytosine. Despite fungicidal combination therapy, mortality remains approximately 30% at 10 weeks with many survivors experiencing substantial disability [32, 33]. Therefore, the standard of care for treating cryptococcal meningoencephalitis is amphotericin-B formulations and flucytosine (Table 2).
Extrapolated from the benefits observed with other CNS infections including tuberculous meningitis and acute bacterial meningitis caused by Streptococcus pneumoniae, investigators evaluated the effects of adjunctive dexamethasone for 6 weeks in HIV-associated cryptococcal meningitis [34]. Higher rates of adverse events and disability were observed in patients receiving dexamethasone compared to those receiving placebo, while mortality was similar, 47 and 41% (HR in the dexamethasone group, 1.11; 95% CI, 0.84 to 1.47; P = 0.45), respectively. One potential explanation for the lack of positive findings is the symptoms associated with CNS disease appear primarily related to intracranial hypertension secondary to CSF outflow obstruction rather than meningeal inflammation [35]. Aggressive management with therapeutic LPs should be pursued to decrease intracranial pressure (ICP), fungal burden, and inflammatory cytokines. Significant survival benefit was detected among patients with HIV-associated C. neoformans meningitis who received at least one therapeutic LP (adjusted relative risk of mortality 0.31, 95% CI 0.12–0.82) [36].
Up to one third of patients with cryptococcal meningitis experience immune reconstitution inflammatory syndrome (IRIS) weeks to months following initiation of ART, which appears to be associated with the fungal burden at the time of diagnosis [37, 38]. The resultant immune recovery may lead to overwhelming inflammation against the cryptococci and its polysaccharide capsule disrupting the delicate intracranial balance [17]. Time to initiation of ART in patients with cryptococcal meningitis remains to be fully defined [27, 39]. Higher mortality was observed at 6 months in patients with cryptococcal meningitis randomly assigned to receive ART within 1–2 weeks after initiating antifungal therapy compared to those with delayed initiation after 5 weeks, 45 vs. 30% (HR 1.73; 95% CI, 1.06 to 2.82), respectively [40]. Excess mortality was most prominent during days 8 to 30 (P = 0.007) but appears to be more closely related to cryptococcal meningitis rather than cryptococcal-associated IRIS. Therefore, initiation of ART should be individualized based on CSF pleocytosis, fungal burden, opening pressure at the time of diagnosis, CSF sterilization following induction therapy, and potential drug-drug interactions but deferred for at least 2–8 weeks. Our recommendation is to wait at least 5 weeks to initiate ART [35].
Histoplasma spp.
Histoplasmosis, caused by Histoplasma capsulatum var. capsulatum, endemic to the Ohio and Mississippi River Valleys, is found in soil contaminated with bird or bat excreta [41, 42]. H. capsulatum has also been identified in South and Central America and the Caribbean, Africa, Asia, and Australia [43]. H. capsulatum var. duboisi has been increasingly identified in some parts of Africa producing disseminated disease indistinguishable from cases caused by H. capsulatum [11]. Transmission is typically the result of inhalation of microconidia, which may disseminate due to lack of cell-mediated immunity. Although infrequent, histoplasmosis may occur in patients not residing in endemic areas as a result of reactivation of prior exposure. Disseminated disease occurred in up to 25% of HIV-infected patients, primarily those with CD4 cell counts < 150 cells/mm3 [41, 42]. Following the introduction of ART, annual incidence decreased to approximately 5% [44]. Host risk factors independently associated with histoplasmosis include CD4 cell count < 200 cells/mm3, nadir CD4 cell count < 50 cells/mm3, CD8 cell count < 650 cells/mm3, male gender, history of herpes simplex infection, and not currently receiving fluconazole or ART [45, 46].
Diagnosis of histoplasmosis includes direct microscopy visualization of budding yeast from tissues or body fluids, culture, serology, or antigen detection [47]. The sensitivity of identifying yeast is associated with severity of disease with positive results occurring in only 75% of patients, whereas isolation in culture may require up to 6 weeks, which must be done in a biosafety laboratory (BSL) level 2 or 3 [41]. Serologic testing is less sensitive in immunocompromised patients, and positive results lack the ability to differentiate between active and passive infection [48]. Antigen detection in urine or serum is sensitive for the identification of disseminated or acute pulmonary disease, but not chronic pulmonary histoplasmosis [48, 49]. The major limitation for utilizing antigen testing is the necessity that all specimens must be submitted to a reference laboratory, which may lead to delays in reporting and patient management [50]. An LFA platform to detect Histoplasma galactomannan in urine by ELISA was evaluated with positive and negative agreements of 82.3 and 100%, respectively, with 90% overall agreement compared to current urinary antigen testing methodologies. Serial antigen monitoring should be performed to evaluate response to therapy.
Primary prophylaxis may decrease the risk of histoplasmosis in HIV-infected patients with CD4 cell counts < 150 cells/mm3 living in endemic areas, but has not been shown to affect mortality [27, 49]. Itraconazole 200 mg per day may be considered in patients at risk of occupational exposure or those residing in high-risk areas, defined as > 10 cases per 100 patient-years. Primary prophylaxis can be safely discontinued with CD4 cell counts ≥ 150 cells/mm3 in patients receiving ART for at least 6 months, but should be restarted if the CD4 cell count declines to < 150 cells/mm3.
Treatment of disseminated histoplasmosis requires itraconazole monotherapy or in combination with amphotericin B for less severe disease and moderately severe to severe disease, respectively (Table 2) [27, 49]. Itraconazole formulations are not interchangeable. The liquid formulation is better absorbed, does not require an acidic environment, and should be administered on an empty stomach, while the capsule must be given with food. Serum itraconazole concentrations should be performed after 2 weeks of therapy to maintain concentrations greater than 1 mcg/mL. Relapse is common and can occur in 50–80% of patients with advanced HIV and histoplasmosis if suppressive therapy is not used (Table 2) [51].
ART should be started immediately following the initiation of antifungal therapy in HIV-infected patients with histoplasmosis [27, 49]. Although the risk of IRIS exists, it is uncommon and non-severe, typically presenting as unmasking and paradoxical disseminated histoplasmosis IRIS [52].
Coccidioides spp.
Coccidioides immitis and C. posadasii, the causative pathogens for coccidioidomycosis, are soil-dwelling dimorphic fungi endemic to the arid regions of southwestern USA, certain areas of Mexico, and Central and South America [53]. Although, recent reports have identified cases of coccidioidomycosis extending into eastern Washington state [54]. While most infections are the result of arthroconidium inhalation, these could be related to reactivation due to prior travel history to endemic areas [53, 55]. Analysis of soil samples suggests persistent colonization corresponding with expanding endemic area [55].
Typically, coccidioidomycosis is an asymptomatic, self-limiting disease in immunocompetent patients; clinical manifestations of symptomatic coccidioidomycosis correlate with cell-mediated immunity function, particularly in HIV-infected individuals with CD4 cell counts < 250 cells/mm3 [55]. Diffuse pulmonary disease and extrapulmonary dissemination to skin, joints, and bones, or meninges may occur [56]. Diagnosis can be confirmed by identification of Coccidioides spp. or spherules in clinical specimens or coccidioidal serologic tests, both of which are highly specific for active infection [52, 57,58,59]. Bimonthly ELISA for IgM and IgG or immunodiffusion may further increase the sensitivity for recently acquired or reactivated disease. Recently, an antigen assay was developed to detect antigen in urine, serum, and other body fluids with higher sensitivity and specificity—93 and 100%, respectively—compared to complement fixation and ELISA, particularly for diagnosis coccidioidal meningitis [58]. Routine CSF examination in patients without signs or symptoms of CNS disease is not clinically indicated [60].
Previously considered a major OI in HIV-infected patients, the overall incidence and severity of coccidiodomycosis have dramatically decreased following the introduction of ART [61]. Although primary prophylaxis in patients with negative serologic tests is not recommended, annual or biannual serologic testing and chest radiography are indicated for patients residing in or traveling to coccidioidal endemic areas [27]. A new positive test should prompt evaluation for active disease in patients with CD4 cell counts < 250 cells/mm3, but if active disease cannot be identified, fluconazole 400 mg per day should be initiated and continued until CD4 cell counts ≥ 250 cells/mm3 in the setting of ART and virologic suppression.
In patients with coccidioidal meningitis, fluconazole is at least as effective as amphotericin B and has become the preferred medication (Table 2) [27]. Alternatively, in severely ill patients with diffuse pulmonary involvement or extrapulmonary disease, amphotericin B with or without fluconazole is the preferred therapy. Continuation or transition to fluconazole monotherapy should occur once clinical improvement is noted, unless bone or joint involvement where itraconazole is preferred. Data are limited for the use of voriconazole, posaconazole, or isavuconazole for coccidioidomycosis, but are expected to have activity [27, 61, 62]. Therapeutic response can be assessed by monitoring complement fixation antibody titer every 12 weeks.
Therapy can be safely discontinued in patients with focal pneumonia or those with asymptomatic disease, and CD4 cell counts > 250 cells/mm3 after at least 6 months of therapy in the setting of ART with virologic suppression and immune reconstitution (Table 2) [27, 59]. Discontinuation in patients with diffuse pulmonary or nonmeningeal disseminated disease and coccidioidal meningitis is less clear. Due to relapse occurring in up to 33 and 80%, respectively—even in patients with CD4 cell counts ≥ 250 cells/mm3—antifungal should not be discontinued.
ART should not be delayed in patients with coccidioidomycosis as IRIS is rare, but selection of ART regimen should be done with caution due to the potential for complex drug-drug interactions with azole antifungals [27, 59]. Localized coccidioidomycosis in cervical lymph nodes or coccidioidomycosis presenting as atypical lymphocytic meningitis may occur after introduction of ART during the acute phase of immune recovery or may be delayed up to 1 year [63, 64].
Talaromyces marneffei (Penicillium marneffei)
T. marneffei, formerly P. marneffei, causes a disseminated fungal infection known as talaromycosis (previously penicilliosis) endemic to Southeast Asia, Northeastern India, and southern China, and Taiwan [65, 66]. Despite available antifungal therapies, mortality rates often exceed 50%, killing up to 1.5 million people annually [4, 6]. Acquisition and transmission of talaromycosis, either inhalation or direct inoculation, have not been fully elucidated, as the only known hosts are humans and bamboo rats: Cannomys and Rhizomys spp. [66]. Reactivation of latent infections may also occur in the absence of cell-mediated immunity, particularly in HIV-infected patients with CD4 cell counts < 100 cells/mm3 [67]. Incidence rates range from 4 to 14% with an associated mortality of 10–30%, and even up to 97% if therapy is delayed [67,68,69].
Dissemination typically occurs in immunocompromised patients and is responsible for the clinical manifestations of the disease, ranging from cutaneous skin lesions to multi-organ involvement with resultant cardiopulmonary failure [70, 71]. Patients typically present with fever, anorexia, skin lesions, hepatosplenomegaly, and lymphadenopathy. Laboratory abnormalities including anemia, transaminitis, and increased alkaline phosphatase are frequently observed. Diagnosis has traditionally been dependent on the identification of T. marneffei from clinical specimens but can take up to seven or more days to grow on culture media [27, 70]. Due to missed and delayed diagnosis, a monoclonal antibody-based ELISA was developed with high sensitivity and specificity, but clinical data is currently unavailable [72,73,74]. Initial treatment for talaromycosis should consist of amphotericin B. A randomized clinical trial demonstrated superior clinical response and fungicidal activity for amphotericin B compared to itraconazole [75].
Primary prophylaxis with itraconazole 200 mg or fluconazole 400 mg weekly is indicated in HIV-infected patients with CD4 cell counts < 100 cells/mm3 residing in endemic areas [71, 76]. Although data is lacking, prophylaxis can theoretically be discontinued in patients on ART with CD4 cell counts > 100 cells/mm3 for at least 6 months. Treatment of active disease should be followed by secondary prophylaxis (Table 2).
No data is currently available on optimal time to initiate ART in patients with talaromycosis [27]. ART should be initiated immediately after antifungal therapy in patients with CD4 cell counts ≤ 100 cells/mm3, whereas it may be reasonable to delay ART until induction therapy is complete. IRIS with T. marneffei has been associated with an unmasking of a previously latent infection [76, 77].
Conclusions
Despite the widespread deployment of ART, AIDS-related invasive mycoses continue to affect those not receiving ART and therefore progressing to advanced immunosuppression. Mortality rates are substantial despite effective antifungal therapy for Cryptococcus spp., Histoplasma spp., Coccidioides spp., and T. marneffei. Development and improvements in RDTs increase the ability to screen and diagnose patients that could benefit from preemptive therapy. Early institution of ART should be considered in patients diagnosed with any of the AIDS-related mycoses. However, the timing of initiation of ART in those with CNS cryptococcosis should be individualized. Additionally, there is an urgent need to increase the availability of antifungal drugs to optimally treat these fungal pathogens in many resource-limited settings. There is also an important need to improve surveillance activities by enhancing diagnostic fungal capacity in areas with the highest burden of AIDS-related mycoses.
References
Papers of particular interest, published recently, have been highlighted as: ● Of importance ●● Of major importance
Haddad NE, Powderly WG. The changing face of mycoses in patients with HIV/AIDS. AIDS Read. 2001;11(7):375–8.
Sm Okoye AA, Picker LJ. CD4(+) T-cell depletion in HIV infection: mechanisms of immunological failure. Immunol Rev. 2013 Jul;254(1):54–64. doi:10.1111/imr.12066.
Buchacz K, Lau B, Jing Y, Bosch R, Abraham AG, Gill MJ, et al. Incidence of AIDS-defining opportunistic infections in a multicohort analysis of HIV-infected persons in the United States and Canada, 2000–2010. J Infect Dis. 2016;214(6):8862–72.
Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:165rv113.
Masur H. HIV related opportunistic infections are still relevant in 2015. Top Antivir Med. 2015;23:116–9.
Brown GD, Denning DW, Levitz SM. Tackling human fungal infections. Science. 2012;336:647.
Ruhnke M. Mucosal and systemic fungal infections in patients with AIDS: prophylaxis and treatment. Drugs. 2004;64(11):1163–80.
•• Guarner J. Human immunodeficiency virus and fungal infections. Semin Diagn Pathol. 2017;34(4):313. doi:10.1053/j.semdp.2017.05.003. This article provides an excellent overview on the diagnosis of AIDS-related fungal mycoses.
Bowen LN, Smith B, Reich D, Quezado M, Nath A. HIV-associated opportunistic CNS infections: pathophysiology, diagnosis, and treatment. Nat Rev Neurol. 2016;12(11):662–74.
• Armstrong-James D, Bicanic T, Brown GD, Hoving JC, Meintjes G, Nielsen K, et al. AIDS-related mycoses: current progress in the field and future priorities. Trends Microbiol. 2017;25(6):428–30. This article provides a summary of advances in research in addressing AIDS-related mycoses and next steps needed to close the gap.
•• Armstrong-James D, Meintjes G, Brown GD. A neglected epidemic: fungal infections in HIV/AIDS. Trends Microbiol. 2014;22:120–7. This article summarizes the epidemiology, clinical aspects, and treatment of the major AIDS-related mycoses.
O’Meara TR, Alspaugh JA. The Cryptococcus neoformans capsule: a sword and a shield. Clin Microbiol Rev. 2012;25(3):387–408. doi:10.1128/CMR.00001-12.
Perfect JR, Bicanic T. Cryptococcosis diagnosis and treatment: what do we know now. Fungal Genet Biol. 2015;78:49–54. doi:10.1016/j.fgb.2014.10.003.
Lazera MS, Salmito Cavalcanti MA, Londero AT, Trilles L, Nishikawa MM, Wanke B. Possible primary ecological niche of Cryptococcus neoformans. Med Mycol. 2000;38(5):379–83.
Franco-Paredes C, Sellers B, Hayes A, Chane T, Patel K, Marr K. Management of Cryptococcus gattii meningoencephalitis. Lancet Infect Dis. 2014;15(3):348–55. doi:10.1016/S1473-3099(14)70945-4.
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–30.
French N, Gray K, Watera C, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS. 2002;16:1031–8.
Nalintya E, Kiggundu R, Meya D. Evolution of cryptococcal antigen testing: what is new? Curr Fungal Infect Rep. 2016;10(2):62–7.
Tanner DC, Weinstein MP, Fedorciw B, Joho KL, Thorpe JJ, Reller L. Comparison of commercial kits for detection of cryptococcal antigen. J Clin Microbiol. 1994;32(7):1680–4.
Jarvis JN, Percival A, Bauman S, Pelfrey J, Meintjes G, Williams GN, et al. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis. 2011;53(10):1019–23.
Boulware DR, Rolfes MA, Rajasingham R, von Hohenberg M, Qin Z, Taseera K, et al. Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast. Emerg Infect Dis. 2014;20(1):45–53.
Williams DA, Kiiza T, Kwizera R, et al. Evaluation of fingerstick cryptococcal antigen lateral flow assay in HIV-infected persons: a diagnostic accuracy study. Clin Infect Dis. 2015;61:464–7.
Meya D, Rajasingham R, Nalintya E, et al. Preventing cryptococcosis—shifting the paradigm in the era of highly active antiretroviral therapy. Curr Trop Med Rep. 2015;2:81–9.
Butler EK, Boulware DR, Bohjanen PR, Meya DB. Long term 5-year survival of persons with cryptococcal meningitis or asymptomatic subclinical antigenemia in Uganda. PLoS One. 2012;7(12):e51291.
Mfinanga S, Chanda D, Kivuyo SL, Guinness L, Bottomley C, REMSTART trial team, et al. Cryptococcal meningitis screening and community-based early adherence support in people with advanced HIV infection starting antiretroviral therapy in Tanzania and Zambia: an open-label, randomised controlled trial. Lancet. 2015;385(9983):2173–82.
World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Available at http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf?ua=1. Accessed April 28, 2017.
DHHS Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed April 28, 2017.
Farmer S, Komorowski R. Histologic response to capsule-deficient Cryptococcus neoformans. Arch Pathol. 1973;96:383–7.
Opota O, Desgraz B, Kenfak A, et al. Cryptococcus neoformans meningitis with negative cryptococcal antigen: evaluation of a new immunochromatographic detection assay. New Microbes New Infect. 2014;4:1–4.
Blevins LB, Fenn J, Segal H, Newcomb-Gayman P, Carroll KC. False-positive cryptococcal antigen latex agglutination caused by disinfectants and soaps. J Clin Microbiol. 1995;33(6):1674–5.
Wilson DA, Sholtis M, Parshall S, Hall GS, Procop GW. False-positive cryptococcal antigen test associated with use of BBL Port-a-cul transport vials. J Clin Microbiol. 2011;49(2):702–3.
Bratton EW, El Husseini N, Chastain CA, Lee MS, Poole C, Stürmer T, et al. Approaches to antifungal therapies and their effectiveness among patients with cryptococcosis. Antimicrob Agents Chemother. 2013;57(6):2485–95.
Day JN, Chau TTH, Wolbers M, et al. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368:1291–302.
Beardsley J, Wolbers M, Kibengo FM, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374(6):542–54.
Franco-Paredes C, Chastain DB, Rodriguez-Morales AJ, Marcos LA. Cryptococcal meningoencephalitis in HIV/AIDS: when to start antiretroviral therapy? Ann Clin Microbiol Antimicrob. 2017;16(1):9.
Rolfes MA, Hullsiek KH, Rhein J, Nabeta HW, Taseera K, Schutz C, et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014;59(11):1607–14.
Shelburne SA 3rd, Darcourt J, White AC Jr, et al. The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis. 2005;40(7):1049–52.
Muller M, Wandel S, Colebunders R, et al. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(4):251–61.
Günthard HF, Saag MS, Benson CA, et al. Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the international antiviral society-USA panel. JAMA. 2016;316(2):191–210.
Boulware DR, Meya DB, Muzoora C, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487–98.
Kauffman CA. Histoplasmosis: a clinical and laboratory update. Clin Microbiol Rev. 2007;20(1):115–32.
McKinsey DS, Spiegel RA, Hutwagner L, et al. Prospective study of histoplasmosis in patients infected with human immunodeficiency virus: incidence, risk factors, and pathophysiology. Clin Infect Dis. 1997;24(6):1195–203.
Adenis AA, Aznar C, Couppie P. Histoplasmosis in HIV-infected patients: a review of new developments and remaining gaps. Curr Trop Med Rep. 2014;1(2):119–28.
Baddley JW, Sankara IR, Rodriquez JM, Pappas PG, Many WJ Jr. Histoplasmosis in HIV-infected patients in a southern regional medical center: poor prognosis in the era of highly active antiretroviral therapy. Diagn Microbiol Infect Dis. 2008;62(2):151–6.
Nacher M, Adenis A, Blanchet D, Vantilcke V, Demar M, Basurko C, et al. Risk factors for disseminated histoplasmosis in a cohort of HIV-infected patients in French Guiana. PLoS Negl Trop Dis. 2014;8(1):e2638.
Hajjeh RA, Pappas PG, Henderson H, Lancaster D, Bamberger DM, Skahan KJ, et al. Multicenter case-control study of risk factors for histoplasmosis in human immunodeficiency virus-infected persons. Clin Infect Dis. 2001;32(8):1215–20.
Hage CA, Ribes JA, Wengenack NL, Baddour LM, Assi M, McKinsey DS, et al. A multicenter evaluation of tests for diagnosis of histoplasmosis. Clin Infect Dis. 2011;53(5):448–54.
Wheat LJ. Current diagnosis of histoplasmosis. Trends Microbiol. 2003;11(10):488–94.
Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, et al. Infectious Diseases Society of America. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(7):807–25.
Theel ES, Harrin JA, Dababneh AS, Rollins LO, Bestrom JE, Jespersen DJ. Reevaluation of commercial reagents for detection of Histoplasma capsulatum antigen in urine. J Clin Microb. 2015;53(4):1198–203.
Drew RH. Pharmacotherapy of disseminated histoplasmosis in patients with AIDS. Ann Pharmacother. 1993;27(12):1510–8.
Kiggundu R, Nabeta HW, Okia R, Rhein J, Lukande R. Unmasking histoplasmosis immune reconstitution inflammatory syndrome in a patient recently started on antiretroviral therapy. Autops Case Rep. 2016;6(4):27–33.
Nguyen C, Barker BM, Hoover S, Nix DE, Ampel NM, Frelinger JA, et al. Recent advances in our understanding of the environmental, epidemiological, immunological, and clinical dimensions of coccidioidomycosis. Clin Microbiol Rev. 2013;26(3):505–25.
Litvintseva AP, Marsden-Haug N, Hurst S, Hill H, Gade L, Driebe EM, et al. Valley fever: finding new places for an old disease: Coccidioides immitis found in Washington state soil associated with recent human infection. Clin Infect Dis. 2015;60(1):e1–3.
Saubolle MA, McKellar PP, Sussland D. Epidemiologic, clinical, and diagnostic aspects of coccidioidomycosis. J Clin Microbiol. 2007;45(1):26–30.
Ampel NM. Coccidioidomycosis in persons infected with HIV type 1. Clin Infect Dis. 2005;41(8):1174–8.
Kassis C, Zaidi S, Kuberski T, et al. Role of coccidioides antigen testing in the cerebrospinal fluid for the diagnosis of coccidioidal meningitis. Clin Infect Dis. 2015;61(10):1521–6.
Pappagianis D, Zimmer BL. Serology of coccidioidomycosis. Clin Microbiol Rev. 1990;3:247–68.
Galgiani JN, Ampel NM, Blair JE, Catanzaro A, Geertsma F, Hoover SE, et al. 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016;63(6):e112–46.
Thompson G 3rd, Wang S, Bercovitch R, Bolaris M, Van Den Akker D, Taylor S, et al. Routine CSF analysis in coccidioidomycosis is not required. PLoS One. 2013;8(5):e64249.
Thompson GR 3rd, Rendon A, Ribeiro Dos Santos R, Queiroz-Telles F, Ostrosky-Zeichner L, Azie N, et al. Isavuconazole treatment of cryptococcosis and dimorphic mycoses. Clin Infect Dis. 2016;63(3):356–62.
Schein R, Homans J, Larsen RA, Neely M. Posaconazole for chronic refractory coccidioidal meningitis. Clin Infect Dis. 2011;53(12):1252–4.
D'Avino A, Di Giambenedetto S, Fabbiani M, Farina S. Coccidioidomycosis of cervical lymph nodes in an HIV-infected patient with immunologic reconstitution on potent HAART: a rare observation in a nonendemic area. Diagn Microbiol Infect Dis. 2012;72(2):185–7.
Trible R, Edgerton N, Hayek S, Winkel D, Anderson AM. Antiretroviral therapy-associated coccidioidal meningitis. Emerg Infect Dis. 2013;19(1):163–5.
Le T, Wolbers M, Chi NH, Quang VM, Chinh NT, Lan NP, et al. Epidemiology, seasonality, and predictors of outcome of AIDS-associated Penicillium marneffei infection in Ho Chi Minh City, Viet Nam. Clin Infect Dis. 2011;52(7):945–52.
Gugnani H, Fisher MC, Paliwal-Johsi A, Vanittanakom N, Singh I, Yadav PS. Role of Cannomys badius as a natural animal host of Penicillium marneffei in India. J Clin Microbiol. 2004;42(11):5070–5.
Chariyalertsak S, Supparatpinyo K, Sirisanthana T, Nelson KE. A controlled trial of itraconazole as primary prophylaxis for systemic fungal infections in patients with advanced human immunodeficiency virus infection in Thailand. Clin Infect Dis. 2002;34(2):277–84.
Hu Y, Zhang J, Li X, et al. Penicillium marneffei infection: an emerging disease in mainland China. Mycopathologia. 2013;175:57–67.
Son VT, Khue PM, Strobel M. Penicilliosis and AIDS in Haiphong, Vietnam: evolution and predictive factors of death. Med Mal Infect. 2014;44:495–501.
Supparatpinyo K, Khamwan C, Baosoung V, Nelson KE, Sirisanthana T. Disseminated Penicillium marneffei infection in southeast Asia. Lancet. 1994;344(8915):110–3.
Ranjana KH, Priyokumar K, Singh TJ, et al. Disseminated Penicillium marneffei infection among HIV-infected patients in Manipur state, India. J Inf Secur. 2002;45(4):268–71.
Wang Y-F, Cai J-P, Wang Y-D, et al. Immunoassays based on Penicillium marneffei Mp1p derived from Pichia pastoris expression system for diagnosis of penicilliosis. PLoS One. 2011;6:e28796.
Prakit K, Nosanchuk JD, Pruksaphon K, et al. A novel inhibition ELISA for the detection and monitoring of Penicillium marneffei antigen in human serum. Eur J Clin Microbiol Infect Dis. 2016;35:647–56.
Wang Y-F, Xu H-F, Han Z-G, et al. Serological surveillance for Penicillium marneffei infection in HIV-infected patients during 2004–2011 in Guangzhou, China. Clin Microbiol Infect. 2015;21:484–9.
Le T, Kinh NV, Cuc NTK, Tung NLN, Lam NT, Thuy PTT, et al. A Trial of Itraconazole or Amphotericin B for HIV-Associated Talaromycosis. N Engl J Med. 2017;376(24):2329–40.
Manosuthi W, Chaovavanich A, Tansuphaswadikul S, et al. Incidence and risk factors of major opportunistic infections after initiation of antiretroviral therapy among advanced HIV-infected patients in a resource-limited setting. J Inf Secur. 2007;55(5):464–9.
Gupta S, Mathur P, Maskey D, Wig N, Singh S. Immune restoration syndrome with disseminated Penicillium marneffei and cytomegalovirus co-infections in an AIDS patient. AIDS Res Ther. 2007;4:21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
This article is part of the Topical Collection on HIV/AIDS
Rights and permissions
About this article
Cite this article
Chastain, D.B., Henao-Martínez, A.F. & Franco-Paredes, C. Opportunistic Invasive Mycoses in AIDS: Cryptococcosis, Histoplasmosis, Coccidiodomycosis, and Talaromycosis. Curr Infect Dis Rep 19, 36 (2017). https://doi.org/10.1007/s11908-017-0592-7
Published:
DOI: https://doi.org/10.1007/s11908-017-0592-7