Abstract
Coarctation of the aorta represents more than a simple obstructive lesion, as there is often evidence of hypertension and vascular dysfunction despite successful surgery at an early age. There are ample data showing that a large proportion of patients develop arterial hypertension, and this appears to increase with age. Our understanding of the pathogenesis of late hypertension is incomplete, and there is limited information on which drugs are most appropriate. Increased arterial rigidity is now well described in this patient group, although it is not known how this should influence therapy. The increase in afterload associated with this increased rigidity has been found to have an impact on the left ventricle at an early stage, and the interaction between the vascular dysfunction and the ventricle is an area of interest and active research. This article reviews some recent studies and highlights areas where research questions remain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term ‘coarctation of the aorta’ (CoA) has traditionally referred to narrowing of the thoracic aorta in the region of the ductus arteriosus. Clinical assessment, however, may be complicated by varying degrees of narrowing in the transverse arch. Our understanding of this lesion has evolved from that of a simple obstructive lesion to one where there is significant vascular dysfunction. Recurring or residual obstruction, aortic dilatation, and aortic valve problems may occur in patients who have undergone treatment for coarctation. This review will focus on issues primarily related to blood pressure. Abnormal blood pressure represents the most common clinical problem in the long-term follow-up of these patients, but the causes for this and the relation to vascular dysfunction are not completely understood.
Prevalence of Hypertension
Some data on blood pressure have been available for many years. The paper by Cohen et al. in 1989 [1] covers the initial experience with this operation (first carried out in 1944) by describing the results of 646 patients undergoing surgery for isolated coarctation of the aorta at the Mayo Clinic between 1946 and 1981. As in many other studies, there was a male preponderance (71 %), and it should be noted that the median age at operation was 16 years and median follow-up was 20 years (1.5–36 years) for the 571 patients with long-term follow-up. The majority of patients were clinically well, with 87 % in NYHA I, 10 % in NYHA II, and 3 % in NYHA III. Blood pressure was measured at clinic and using a diagnosis of hypertension as either a systolic blood pressure > 150 mm Hg or a diastolic pressure > 90 mm Hg, 25 % of patients in this cohort were hypertensive. Interestingly, the main risk factor noted for hypertension was age at operation, as demonstrated by the observation that those operated on in infancy had a 7 % prevalence of hypertension, whereas those operated on at over 4 years of age had a 33 % prevalence of hypertension, as defined above. Coronary artery disease was the most common cause of death in the long-term survivors.
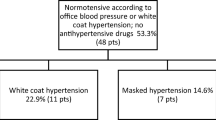
In the 1990s, therefore, the medical community was aware that even though coarctation surgery was very successful in terms of symptoms, there was a high incidence of late blood pressure problems and there was some evidence that this might be improved with earlier surgery. Unfortunately, the hope that earlier surgery would eliminate blood pressure as a clinical issue has not been realised. The report by Hager et al. [2] provides information on a cohort of 404 patients operated between 1974 and 1999, with follow-up on 273 patients. At up to 27 years post-surgery, 25 % of patients were on antihypertensive medication, 25 % were found to be hypertensive on ambulatory monitoring, and another 10 % had a hypertensive response to exercise.
Although the significance of an exaggerated blood pressure rise with exercise was previously undetermined [3], some recent studies present evidence that this is likely to be an important predictor of hypertension. This so-called hypertensive response to exercise is known to occur in a significant subset of patients who have had an anatomically satisfactory coarctation repair and who have normal resting blood pressure. In the study by Madueme et al. of patients with normal resting blood pressure following coarctation repair, 16 % could be classified as having an exaggerated response to exercise, at a mean age of 12.7 years [4•]. In another study [5••] in an older group of patients (median age 27 years), a hypertensive response to exercise was significantly associated with left ventricular mass and was therefore determined to be a marker of haemodynamic importance.
Overall, therefore, the prevalence of abnormal blood pressure in the cohort described by Hager was over 50 %, and the most important factor appears to be duration of follow-up. In that study, virtually all of the older patients were hypertensive. Increasingly, studies are showing that blood pressure abnormalities can be detected even during childhood. In a study from the northeast of England [6] approximately 30 % of the cohort operated on in infancy (median age of 0.2 months) had significantly elevated blood pressure, based on either casual or ambulatory readings, when followed up at a mean age of 12 years. This and other data suggest that even with satisfactory repair of the aortic arch, the ‘natural’ history is that blood pressure issues will develop with time, and this process is detectable in children.
The Role of Residual Obstruction
As stated above, hypertension is common even in the absence of significant obstruction. Gradients of around 20 mm Hg and less are usually regarded as mild. There is evidence of a significant relationship between systolic blood pressure and mild gradients on Doppler in children [6], but a study on adults [7] at a mean age of 34 years and varying degrees of residual obstruction suggested no significant relationship between residual gradient and late hypertension. With this uncertainty as to the physiological implications of mild gradients, the advisability of removing small residual gradients is unclear.
In the last decade, the placement of endovascular stents has become more feasible and provides a potentially non-surgical treatment for mild coarctation. There are a few studies available that address the value of treating mild gradients, but the numbers treated are relatively small. Eicken et al. [8] reported on 43 patients treated with a stent at a median age of 16.8 years and who had a median gradient (pre-procedure) of 22 mm Hg. They found that resting systolic blood pressure was significantly decreased at follow-up but that only 68 % of this relatively young group of patients could be classified as having normal blood pressure at a median follow-up of 30 months.
A similar finding was recently reported [9•] on 40 patients where the average age at the time of the procedure was 24.9 years and the peak systolic gradient under general anaesthesia was 24 mm Hg (mean) before stent placement. Thirteen of 39 patients (33 %) who were successfully treated had persistently elevated systolic BP (>140 mm Hg) at last follow-up. Of the 4 patients aged >40 years at the time of the procedure, 2 remain hypertensive (systolic BP >150 mm Hg). The number of antihypertensive agents administered before the procedure compared to most recent follow-up did not change significantly. Paired 24-hour BP recordings were taken before and after stent placement in 7 patients, and there was a similar magnitude of reduction in post-procedural systolic BP compared to paired clinic BP recordings (mean systolic BP before stent placement 141 mm Hg, reducing to 130 mm Hg after stent treatment, p < 0.005). Moltzer et al. [10] reported on a slightly older group of 24 patients who had stent implantation, including native coarctation and re-coarctation, at a median age of 36 years. Despite significant improvement in gradient, the proportion of cohort on treatment for hypertension did not decrease (79 % pre and 82 % post). There was no significant difference in 24-hour systolic blood pressure (on 22 patients) after a median follow-up of 27 months. The only significant difference was lower diastolic pressure on follow-up in the re-coarctation stented group.
It appears, therefore, that the elimination of mild–moderate coarctation with stents or surgery is associated with some medium-term reduction in systolic blood pressure and that the risk of intervention by stenting is relatively low. With regards to blood pressure, this procedure is not curative, and the prevalence of hypertension and need for medication remains significant. The long-term benefit from intervention on mild gradients has yet to be demonstrated. The data would seem to support a small but significant decrease in systolic pressure, which may be more obvious in younger patients. This must be balanced against the risk of the intervention, and for the time being, decisions should be individualised to each patient.
Vascular Dysfunction
As described above, hypertension may be the most clinically common and obvious issue in patients who have had coarctation repair, but there is strong evidence of vascular dysfunction in this patient population that may be of major importance in terms of long-term prognosis. This was first described in a study in 1985 [11], and our understanding of the pathophysiological process has been gradually evolving since then. That landmark study demonstrated abnormal forearm vascular reactivity and normal lower-limb (calf) vascular reactivity in patients following coarctation surgery, and postulated that these abnormalities were related to the prevalence of hypertension in this patient group.
These vascular issues can be arbitrarily divided into abnormal compliance (rigidity, stiffness) of the conduit arteries and endothelial dysfunction. The increased stiffness of the conduit arteries of the pre-coarctation site is now well established, but the implications in terms of causation and treatment are not completely understood. It was initially suggested that the subgroup operated at less than 4 months may have normal arterial stiffness [12], which would bode well for the increasing proportion of patients operated on as neonates. However, in a prospective longitudinal study in a group of children who had neonatal repair, Kuhn et al. [13] showed that after a mean follow-up of 2.9 years, the elasticity of the ascending aorta did not change significantly from the initial neonatal findings. The estimate of aortic distensibility was significantly different from the control group at age 2.9 years despite similar blood pressure and left ventricular measurements.
It has been recognised for some time that the intima-media thickness of the carotid artery of coarctation patients is increased in adults. Through the use of very high-resolution ultrasound, this can now be extended to the brachial and radial arteries [14••]. The precise anatomical basis for the observed functional abnormalities has been the subject of some animal studies. A number of years ago, Schested et al. [15] demonstrated that surgical specimens of 8 patients taken above and below the coarctation site at the time of operation showed increased collagen in the area a few cm above the main coarctation narrowing. A more recent study [16••] using an animal model has examined the expression of key smooth muscle contractile proteins and focal adhesion proteins both before and after coarctation repair. The study found increased proximal non-muscle myosin expression and decreased smooth muscle myosin expression in the animal model both before and after surgical correction of the coarctation. The researchers speculate that these alterations in smooth muscle phenotype may contribute to the structural and functional changes observed in the proximal arteries of patients who have undergone coarctation repair. Further studies are needed to determine the direct relevance to humans and how this may influence therapy.
A number of studies of flow and glyceryl trinitrate-mediated dilation have shown that endothelial function is altered post-coarctation repair. The initial studies [12, 17] showed that both of these parameters were abnormal. Further studies [18] reported similar findings and also described an increased level of adhesion molecules, the expression of which is increased in the presence of impaired endothelial function. This study [18] showed that the impaired distensibility in the carotid arteries was positively correlated with endothelial dysfunction, suggesting an association between the mechanical abnormalities and endothelial impairment in the large arteries.
Another factor that may be of importance is the shape of the arch [19]. A study of patients (mean age = 15 years) with a ‘Gothic’ arch (i.e., steeper angulation between ascending and descending aorta) demonstrated that this was associated with higher systolic blood pressure and increased arterial stiffness. There are a number of potential confounding factors. It is not known how the final shape of the arch interacts with surgical approach and technique and how these factors, as well as size of the transverse arch [20•], affect growth and eventual outcome. Overall, it can be stated that there are a number of vascular abnormalities at macroscopic, microscopic, and functional levels in this patient population. It is to be expected that there will be some interaction between these factors that will complicate analysis of studies.
Left Ventricle
There are a number of studies that document abnormalities in the left ventricle following coarctation repair. In view of the previously described high prevalence of blood pressure abnormalities in both the paediatric and adult age groups, one may expect left ventricular hypertrophy in this patient population. However, the extent of left ventricular problems appears to be disproportionate to the elevation in blood pressure. Some years ago, in a study using ambulatory blood pressure in a group of 20 children (mean age of 14 years), Leandro et al. [21] demonstrated that left ventricular mass was increased despite the absence of significant elevation in 24-hour blood pressure. A more recent study [22] in a group of 40 patients who could be classified as normotensive (mean age = 12 years) showed that there was a significant increase in left ventricular mass index in comparison to controls. This suggests that the observed increased in left ventricular mass cannot be attributed simply to elevated blood pressure. In a group of 52 older patients (mean age 21 years), Crepaz et al [23] demonstrated that left ventricular mass and mass-to-volume ratio were significantly increased compared to a control group, although systolic blood pressure was higher than controls in this study.
It is not surprising that more subtle left ventricular abnormalities are now increasingly described, even at a relatively early age. A study by Lombardi et al. [24••] reported that subtle abnormalities of ventricular function can be found in the absence of demonstrable left ventricular hypertrophy or elevation of blood pressure. Using matched controls, this retrospective study of 24 patients at a median age of 9 years, who had had early repair (median age at repair = 0.5 months) found evidence of left ventricular diastolic dysfunction.
In this context, it appears that left ventricular abnormalities can be demonstrated, at least initially, in the absence of definite blood pressure elevation and that these left ventricular abnormalities, as demonstrated by studies in children, probably evolve with time.
Ventricle Aortic Interaction
Distensibility and compliance are important properties of the arterial system, and are mainly determined by the elasticity of the proximal aorta and major arteries. Abnormalities of the proximal aorta will inevitably have an effect on ventricular function. A recent paper [25••] investigated the aortic wave reflection and relation to cardiac afterload and the effect on left ventricular mass. In this study of 20 patients under the age of 15 years (14 coarctation and 6 interrupted aortic arch) with no residual gradient, a pressure sensor-mounted catheter was placed in the ascending aorta, and an augmentation index was calculated for each patient using the pressure waveform. The corrected (for heart rate) augmentation index was significantly higher in patients who underwent aortic arch repair than the reference data. The degree of thickness of the left ventricular wall was correlated with the enhancement of pressure wave reflection. The study authors speculated that increase in wave reflection, as measured by the augmentation index, causes increase in afterload, and that this may be a significant factor in the above-mentioned ventricular abnormalities. The previously mentioned study by Lombardi et al. [24••] used echo-Doppler techniques to assess aortic distensibility, stiffness index, and strain, and reported significant differences in LV diastolic function and aortic elasticity measurements in comparison to the control group. This study shows that even at a young age (median age = 9 years), both aortic elasticity and LV diastolic function are impaired in children with satisfactory coarctation repair.
The increased wave reflection that will affect afterload [25••] and the evidence of a linear relation between proximal ascending aortic elasticity and diastolic function [24••], as shown in these studies, would support a direct relation between vascular abnormalities and ventricular function.
Pathophysiology of Hypertension After Coarctation Repair
Although an association between the well-documented abnormalities in vascular function and the left ventricle may be intuitive, the relationship of these parameters to hypertension remains to be fully elucidated. Studies in elderly populations have shown that age-related vascular stiffening is accompanied by changes in the left ventricle and have demonstrated increased end-systolic chamber stiffness. The study of the interplay between arterial stiffness and left ventricular ejection is difficult, as this generally requires catheters to be placed in the ventricle to construct pressure/area loops at different preloads. A catheter study [26] of a paediatric population (mean age 5.9 years) who had had coarctation repair documented an increase in arterial rigidity, but also reported increased left ventricular end-systolic elastance compared to controls. The authors reported that the increase in end-systolic elastance of the left ventricle was disproportionate and that there was no significant correlation with degree of left ventricular hypertrophy. They also showed increased left ventricular systolic and diastolic stiffness, which was likely in response to the increased vascular load. This combined ventricular-arterial stiffness has been termed ‘coupling’ disease, and has been implicated in problems with blood pressure regulation and cardiovascular reserve in the elderly population. Even though the stiffening of the heart and vessels observed in coarctation will have similarities with the aging process, there are likely important differences, as can be seen in the variable diastolic blood pressure reported in coarctation as opposed to the classically high pulse pressure in the elderly population. The area of the vascular bed involved and the presence of surgical sutures are other important distinguishing factors.
The role of the baroreceptor in the pathogenesis of hypertension is uncertain. Kenny et al. [27••] studied 31 patients between 14 and 18 years of age and measured 24-hour blood pressure, pulse wave velocity, and spontaneous baroreceptor sensitivity. They showed that the subgroup of coarctation patients who appeared to be normotensive had increased spontaneous baroreceptor sensitivity when compared to a control population. The subgroup in this study found to be hypertensive (n = 9) by ambulatory monitoring did not show this difference, and one could speculate that the spontaneous baroreceptor sensitivity is increased at a relatively early point, but appears to normalise as hypertension develops. It is possible that the ‘failing’ of the increased sensitivity may result in the observed hypertension. This study suggests that baroreceptor function differs from normal in this population, but whether this is cause or effect remains to be proven.
Bicuspid Aortic Valve
The high prevalence of bicuspid aortic valve (BAV) with aortic coarctation is well recognised. It has been shown that coarctation is associated mainly with the presence of an anterior-posterior commissure due to fusion of the left and right leaflets [28]. There is increasing attention to the different types of bileaflet aortic valve and the relation to aortopathy. Pees and Michel-Behnke [29••] studied subjects, without coarctation, who had bileaflet or trileaflet aortic valves (TAV); there were 48 children in both groups with a mean age of 11 years. They found that the aorta was bigger in BAV versus TAV and that the morphology of the BAV was important, with more dilation in the group where there was fusion of the right and non-coronary cusps. The aorta appeared to be stiffer in the group with fusion of the left and right leaflets. This may suggest that morphology of the aortic valve is another contributing factor to arterial stiffness observed in the coarctation patients, although the precise manner by which it contributes is not understood.
Drug Therapy
An improved understanding of pathophysiology may help to inform the choice of antihypertensive therapy. Ideally, such drugs would not only lower measured blood pressure but would also improve arterial stiffness, endothelial function, and ventricular stiffness. In 16 patients with successfully repaired coarctation of aorta (mean age = 29.9 years), Brili et al [18] reported that proinflammatory cytokines and adhesion molecules were higher in the coarctation group. In a subsequent 4-week randomised crossover trial [30], they demonstrated that the angiotensin-converting enzyme (ACE) inhibitor ramipril improved endothelial function and decreased the expression of pro-inflammatory cytokine IL-6 in patients who had coarctation repair. The study evaluated post-ischaemic hyperaemia as an index of endothelial function in the right forearm, and therapy with ramipril significantly improved maximum hyperemic forearm blood flow. Interestingly, however, it had no significant effect on diastolic blood pressure.
Giordano et al [31] reported on a study where 30 patients (mean age = 15 years) were treated with either a ß-Blocker (atenolol, n = 12), an angiotensin receptor blocker (ARB), candesartan, (n = 13), or both (n = 5). Good blood pressure control was achieved in 50 % of the ß blocker group and 75 % of the candesartan group. There were more side effects in the ß-blocker group. In a study on an older group of patients [32], candesartan was compared with metoprolol in an 8-week crossover study on 16 patients (mean age 37 years), and metoprolol was found to be more effective in reducing blood pressure. Disappointingly, neither agent had an effect on pulse wave velocity, although it should be noted that the duration of treatment was relatively short.
It would appear that both ß-blockers and drugs affecting the renin-angiotensin-aldosterone system can improve blood pressure control and that ACE inhibitors may be better tolerated in younger patients. Data demonstrating improved vascular function with either group is lacking.
Conclusions
Coarctation of the aorta remains an area of active research interest, as there are many unanswered questions. Some are very basic questions as to the causation of the vascular dysfunction. Is it predetermined from fetal life, or is it related to the surgical intervention necessary to relieve the obstruction? With regard to the vascular issues apparent with all surgical techniques, would the advent of biological stents offer a different mode of initial treatment that may have a different outcome in terms of vascular function and blood pressure? The relation of coarctation with the different types of bicuspid aortic valve is intriguing and may provide a model to investigate the importance of flow and genetic factors in the pathogenesis of vascular abnormalities.
We are uncertain as to the best therapy for blood pressure control in these patients, when to start treatment, and what parameters we should be measuring and monitoring, acknowledging that measurement of systolic blood pressure does not equate to all of the vascular pathology present. Finally, the importance of the diastolic pressure in this population, and the paediatric age group in particular, is not well-studied. It is not known if the clinical measurement of pulse pressure is of prognostic value in either the young or old post-coarctation repair population. As we approach the 70th anniversary of the first surgical resection for coarctation, it is clear that, despite relief of obstruction, related issues in this patient population will continue to pose many questions.
References
Papers of particular interest, published recently, have been highlighted: • Of importance •• Of major importance
Cohen M, Fuster V, Steele P, McGoon D. Coarctation of the aorta: Long term follow up and prediction of outcome after surgical correction. Circulation. 1989;80:840–5.
Hager A, Kanz S, Kaemmerer H, Schreiber C, Hess J. Coarctation long term follow up: significance of arterial hypertension in a cohort of 404 patients up to 27 years after surgical resection of isolated coarctation even in the absence of recordation and prosthetic material. J Thorac Cardiovasc Surg. 2007;134:738–45.
Swan L, Goyal S, Hsia C, Hechter S, Webb G, Gatzoulis M. Exercise systolic blood pressures are of questionable value in the assessment of the adult with a previous coarctation repair. Heart. 2003;89:189–92.
Madueme P, Khoury P, Urbina E, Kimball T. Predictors of exaggerated exercise induced systolic blood pressure in young patients after coarctation repair. Cardiol Young. 2013;23:416–22. Study showing that an exaggerated blood pressure response to exercise can be demonstrated at a relatively young age.
Krieger E, Clair M, Opotowsky A, Landzberg M, Rhodes J, Powell A, Colan S, Valente A. Correlation of exercise response in repaired coarctation o f the aorta to left ventricular mass and geometry. Am J Cardiol 2013; 111:406-411. Study relating exercise blood pressure to left ventricle mass/volume ratio; provides good evidence that this is an important measure of blood pressure
O’Sullivan J, Derrick G, Darnell. Prevalence of hypertension in children after early repair of coarctation of the aorta: a cohort study using casual and 24 hour blood pressure measurement. Heart. 2002;88:163–6.
Trojnarska O, Mizia-Stec K, Gabriel M, Szczepaniak-Chicheł L, Katarzyńska-Szymańska A, Grajek S, et al. Parameters of arterial function and structure in adult patients after coarctation repair. Heart Vessels. 2011;26:414–20.
Eicken A, Pensl U, Sebening W, Hager A, Genz T, Schreiber C, et al. The fate of systemic blood pressure in patients after effectively stented coarctation. Eur Heart J. 2006;27:1110–5.
Bentham J, English K, Ballard G, Thompson J. Effect of interventional stent treatment of native and recurrent coarctation of aorta on blood pressure. Am J Cardiol 2013; 111:731–736. Study showing that after placement of endovascular stents, a significant decrease in systolic blood pressure can be demonstrated, but many remain hypertensive
Moltzer E, Roos-Hesselink JW, Yap SC, Bogers AJ, de Jaegere PP, Witsenburg M. Endovascular stenting for aortic (re)coarctation in adults. Neth Heart J. 2010;18:430–6.
Gidding S, Rocchini A, Moorehead C, Schork M, Rosenthal A. Increased forearm vascular reactivity in patients with hypertension after repair of coarctation. Circulation. 1985;71:495–9.
De Divitiis M, Pilla C, Kattenhorn M, Donald A, Leeson P, Wallace S, et al. Vascular dysfunction after repair of coarctation of the aorta: impact of early surgery. Circulation. 2001;104:I-165–70.
Kuhn A, Baumgartner C, Horer J, Schreiber C, Hess J, Vogt M. Impaired elastic properties of the ascending aorta persist within the first three years of neonatal coarctation repair. Pediatr Cardiol. 2009;30:46–51.
Sarkola T, Redington A, Slorach C, Hui W, Jaeggi E. Assessment of vascular phenotype using a novel very high resolution ultrasound technique in adolescents after coarctation repair and/or stenting. Heart 2011; 97:1788-1793. Study using ultrasound of intima-media thickness in patients with coarctation repair, showing differences in brachial and radial arteries when compared with controls
Schested J, Baandrup U, Mikkelsen E. Different reactivity and structure of the prestenotic and poststenotic aorta in human coarctation. Circulation. 1982;65:1060–5.
Menon A, Eddinger T, Wang H, Wendell D, Toth J, LaDisa J. Altered haemodynamics, endothelial function and protein expression occur with aortic coarctation and persist after repair. Am J Physiol Heart Circ Physiol 2012; 303:1304-1318. Study of the expression of key smooth muscle contractile proteins that found that proximal nonmuscle myosin expression was increased and smooth muscle myosin expression decreased in the animal model both before and after surgical correction of the coarctation
Gardiner H, Celermajer D, Sorensen K, Georgakopoulos D, Robinson J, Thomas O, et al. Arterial reactivity is significantly impaired in normotensive young adults after successful repair of coarctation in childhood. Circulation. 1994;89:1745–50.
Brili S, Tousoulis D, Antoniades C, Aggeli C, Roubelakis A, Papathanasiu S, et al. Evidence of vascular dysfunction in young patients with successfully repaired coarctation of aorta. Atherosclerosis. 2005;182:97–103.
Ou P, Celermajer D, Mousseaux E, Giron A, Aggoun Y, Szezepanski I, et al. Vascular remodelling after successful repair of coarctation. J Am Coll Cardiol. 2007;49:883–90.
Lee M, Kowalski R, Galati J, Cheung M, Jones B, Koleff J, d’Udekem Y. Twenty four hour blood pressure monitoring detects a high prevalence of hypertension late after coarctation repair in patients with hypoplastic arches. J Thorac Cardiovasc Surg 2012; 44:1110-1118. Study relating exercise blood pressure to size of the arch
Leandro J, Smallhorn J, Benson L, Musewe N, Balfe J, Dyck J, et al. Ambulatory blood pressure monitoring and left ventricular mass and function after successful surgical repair of coarctation of the aorta. J Am Coll Cardiol. 1992;20:197–204.
Ou P, Celermajer D, Jolivet O, Buyens F, Herment A, Sidi D, et al. Increased central aortic stiffness and left ventricular mass in normotensive young subjects after successful coarctation repair. Am Heart J. 2008;155:187–93.
Crepaz R, Cemin R, Romeo C, Bonsante E, Gentili L, Trevisan D, et al. Factors affecting left ventricular re-modelling and mechanics in the long term follow-up after successful repair of coarctation of the aorta. Cardiol Young. 2005;15:160–7.
Lombardi K, Northrup V, McNamara R, Sugeng L, Weismann C. Aortic stiffness and left ventricular diastolic function in children following early repair of aortic coarctation. Am J Cardiol 2013; 112:1828-1833. Study showing how early changes can be detected in the left ventricle even after early repair
Murakami T, Takeda A, Yamazawa H, Tateno S, Kawasoe Y, Miwa K. Aortic pressure wave reflection in patients after successful aortic arch repair in early infancy. Hypertens Res 2013; 36:603-607. Study showing how wave reflection may increase ventricular afterload
Senzaki H, Iwamoto Y, Ishido H, Masutani S, Taketazu M, Kobayashi T, et al. Ventricular-Vascular stiffening in patients with repaired coarctation of the aorta. Circulation. 2008;118:191–8.
Kenny D, Polson J, Martin R, Caputo M, Wilson D, Cockcroft J, Paton J, Wolf A. Relationship of aortic pulse wave velocity and baroreceptor reflex sensitivity to blood pressure control in patients with repaired coarctation of the aorta. Am Heart J 2011;162:398-404. Study on the function of the baroreceptor, showing that there are differences when compared to controls
Fernandes S, Sanders S, Khairy P, Jenkins K, Gauvreau K, Lang P, et al. Morphology of bicuspid aortic valve in children and adolescents. J Am Coll Cardiol. 2004;44:1648–51.
Pees C and I Michel-Behnke. Morphology of the bicuspid aortic valve and elasticity of the adjacent aorta in children. Am J Cardiol 2012; 110:1354-1360. Study showing potentially important differences in elastic properties between subtypes of bicuspid aortic valve
Brili S, Tousoulis D, Antoniades C, Vasiliadou C, Karali M, Papageorgiou N, et al. Effects of Ramipril on endothelial function and the expression of proinflammatory cytokines and adhesion molecules in young normotensive subjects with successfully repaired coarctation of aorta. J Am Coll Cardiol. 2008;51:742–9.
Giordano U, Cifra B, Giannico S, Turchetta A, Calzolari A. Mid-term results and therapeutic management for patients suffering hypertension after surgical repair of aortic coarctation. Cardiol Young. 2009;19(5):451–5.
Moltzer E, Raso F, Karamermer Y, Boersma E, Webb G, Simoons M, et al. Comparison of Candesartan versus Metoprolol for treatment of systemic hypertension after repaired coarctation. Am J Cardiol. 2010;105:217–22.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
John O’Sullivan declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Hypertension
Rights and permissions
About this article
Cite this article
O’Sullivan, J. Late Hypertension in Patients with Repaired Aortic Coarctation. Curr Hypertens Rep 16, 421 (2014). https://doi.org/10.1007/s11906-014-0421-4
Published:
DOI: https://doi.org/10.1007/s11906-014-0421-4