Abstract
Life expectancy is longer in women compared to men, and cardiovascular events occur at a lower rate and at a later age in females than males. The impact of gender on the prevalence, the presentation, and the long-term outcome of cardiovascular disease has long been a topic of active research. Gender differences have been found in several studies but opposite findings also exist. The impact of gender in hypertension and antihypertensive therapy remains poorly clarified. The prevalence, awareness, treatment, and control rates of hypertension exhibit some differences between the two sexes, which are age-dependent. The female advantage in the cardiovascular risk of hypertensive patients might be attenuated by comorbidities and target organ damage. Another aspect of major clinical importance is whether gender differences exist on the effects of antihypertensive agents in blood pressure reduction and cardiovascular morbidity and mortality. The aim of this review is to critically evaluate recent data regarding gender differences in hypertension and incorporate new data into the body of existing knowledge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gender differences on the prevalence, presentation, symptoms and severity of cardiovascular complications of hypertension have long been under investigation. Gender differences have been described in several studies for cardiovascular risk factors and cardiovascular risk status, but results are at times conflicting. Table 1 summarizes the major differences between men and women with hypertension.
Life expectancy is longer in women and cardiovascular events occur at a lower rate and at a later age than men [1]. A vast amount of evidence from observational studies demonstrated that the risk for cardiovascular events is lower in women than in men [1], but the gap is narrowing with age possibly due to a survival effect of males reaching older age. Female patients are more likely to experience poor outcomes following a cardiovascular event or interventions [2]. Whether gender differences in long-term outcomes and prognosis represent a true phenomenon or result from differences in patient management, diagnostic approach, and therapeutic strategies is not yet clarified. For example, the data point towards increased early mortality after myocardial infarction in women than in men. This might be attributed to a worse risk profile on admission, lower utilization of invasive management or less compliance to therapy [3]. Naturally, the skeptics attribute some of the gender differences to “gender bias.” Women are not taken seriously when they present with chest pain, they are not treated as aggressively as men, or women at times may be deprived of state of the art procedures.
Women are significantly under-represented in large clinical trials within the cardiovascular disease arena. Female representation is about 30 %, while specific gender analysis is performed in only one out of three reports [4].
This review aims to describe gender differences in the epidemiology and pathophysiology of hypertension, to present the impact of gender on cardiovascular risk, target organ damage and comorbidities, and to discuss potential gender differences on the effects of antihypertensive agents in blood pressure reduction and cardiovascular morbidity and mortality.
Prevalence – Awareness – Treatment- Control
Hypertension affects 1 out of 3 US adults for an estimated number of 77.9 million patients suffering from high blood pressure [5••]. The prevalence of hypertension does not present significant gender differences overall: 33.6 % (37.2 million) for males and 32.2 % (40.7 million) for females. Significant gender differences exist however within different age groups. The prevalence of hypertension is higher among males until the age of 45, the prevalence is nearly equal between the two genders from 45 to 64 years of age, and after that hypertension becomes more prevalent among women.
Recent data from the NHANES 2007–2010 survey reveal that 81.5 % of hypertensive patients were aware of the disease, 74.9 % were receiving antihypertensive therapy, and blood pressure was controlled in 52.5 % of them [5••]. Significant differences exist however between males and females. Until recently (NHANES 1988–2008) awareness and treatment of hypertension was greater in women than in men, while control rates were greater in men, suggesting that hypertension in females is relatively ‘resistant’ to antihypertensive therapy and several hypotheses to explain this issue have been proposed [6]. However, the most recent data from the 2007–2010 NHANES survey reveal that awareness, treatment, and control rates are significantly higher in women than men, and this is apparent for all races. Gender disparity is more pronounced in African-American and Mexican-American patients and less pronounced in Caucasian patients. For example, in African-Americans, awareness rates are 7.8 % higher, treatment rates 11.6 % higher, and control rates 12.4 % higher in women than in men, while the corresponding differences in Caucasian patients are 4.6 %, 6.8 %, and 3.8 %, respectively [5••].
In a recently published study from the Department of Veterans Affairs, blood pressure control was examined over a 10-year period (2000 to 2010). Overall blood pressure control improved from 45 % in 2000 to 76 % in 2010, control rates lagged behind among black patients, but there was no difference in control rates among men and women [7].
Among older adults (>65 years), control rates were significantly lower in women than in men at the NHANES 1999–2004 survey [8]. Whether this gender disparity is still apparent or has improved nowadays is currently not known. A recent study of more than 150,000 hypertensive patients participating in the Cardiovascular Research Network in the US showed higher control rates in women than in men (45.7 % versus 41.2 %) [9]. However, control rates were significantly affected by age, with better control among women in young and middle age, and better control among men in older age (>65 years), suggesting that further efforts are needed to alleviate gender disparity in control rates in the elderly.
Data from other parts of the world are also available. A recent analysis of data from more than 26 million Canadians revealed that the prevalence of hypertension was higher in older (60 years) women than in men [10]. Similar findings were observed in a recent large population study in developing countries (India, China, and Latin America) [11]. In the Canadian Health Measures Survey it was found that female patients were more likely to be aware of having hypertension, since only 14 % of women were unaware compared to 21 % of their male counterparts [12]. On the other hand, women were less likely to have their blood pressure controlled, especially at advanced age (>60 years), with uncontrolled rates being 34 % for women and 18.1 % for men.
Pathophysiologic Mechanisms
The pathophysiologic mechanisms underlying the age-dependent disparity in blood pressure levels between the two sexes are poorly defined, although many hypotheses have been proposed with the hormonal component being the prevailing.
Experimental and clinical data suggest that estrogen exert a variety of beneficial cardiovascular effects, including vasorelaxation, sympathoinhibition, prevention of vascular remodeling, and renoprotection [13]. Increased estrogen levels in premenopausal women induce vasorelaxation and subsequently decreased aortic stiffness via actions on the endothelium and smooth muscle cells. Estrogen levels fall abruptly in postmenopausal women, leading to the attenuation of beneficial effects and finally to increased cardiovascular risk. A recent report from the Multi-Ethnic Study of Atherosclerosis shows that incident hypertension is positively associated with testosterone, estradiol, and dehydroepiandrosterone levels and inversely associated with sex-hormone binding globulin levels [14•].
However, the observed increase of blood pressure after menopause cannot be evaluated independently of the potential confounding effects of aging and comorbidities. In fact, it seems that aging is responsible for the majority of effects that have traditionally been attributed to menopause [15].
Sex steroids seem to significantly affect sympathetic nervous system activity exerting opposing effects. Progesterone is associated with sympathoexcitation, while estradiol is associated with sympathoinhibition. The dynamic interaction between estradiol and progesterone levels during the luteal phase has been proposed to explain the sympathoexcitation during the mid-luteal phase of ovarian cycle [16]. Recent data indicates that the interaction of sex steroids, including testosterone, with the sympathetic system during menopause is affected by several factors, including nitric oxide and b-adrenergic receptor sensitivity [17, 18]. A positive relationship between sympathetic overactivity and peripheral vascular resistance that was not altered by beta-blockers was reported, suggesting that beta-blockade does not attenuate sympathetic vasoconstriction in postmenopausal women.
Sympathetic activity recently attracted wide scientific interest in another ‘female disease’, the polycystic ovary syndrome [19]. The polycystic ovary syndrome is associated with menses abnormalities, insulin resistance, hypertension and sympathetic overactivity. Attenuation of sympathetic overactivity through renal nerve ablation resulted not only in blood pressure reduction but also in glucose metabolism improvements [20••]. More impressively, reoccurrence of menses was observed in one patient with long-lasting amenorrhea, suggesting that sympathetic overactivity is implicated not only in blood pressure elevation and insulin resistance but in the pathogenesis of the syndrome itself as well.
Sex hormones seem to affect the activity of the renin–angiotensin system. Experimental data point towards a sexual dimorphism in salt-sensitive hypertension mediated by enhanced intrarenal activity of the renin-angiotensin system in male compared to female rats [21]. Sex hormones seem to affect sodium handling, since blood pressure is salt-resistant in premenopausal women and becomes salt-sensitive after menopause [22], explaining the significant benefits of salt restriction in postmenopausal women that were recently reported [23].
Endothelin-1 actions in the kidney seem to be gender-related. Experimental data suggests that male animals have higher endothelin-1 mRNA expression in the kidneys and enhanced vasoconstriction through type A receptors, while gonadectomy attenuates these effects [24]. In contrast, female animals are relatively protected from high blood pressure through increased diuresis and natriuresis mediated by type B receptors [25].
Apart from this hormonal component, several other gender differences exist in the cardiovascular system. A recent longitudinal study from Framingham revealed that pulse pressure increments with age and higher body mass index are more pronounced in women than in men [26]. Moreover, women have higher heart rate and lower cardiac output than men, partly due to their lower height and size. Shorter height results in premature arrival of the reflected wave, earlier in systole, leading to reduced pulse amplification and augmentation index.
Gender differences in the atherosclerotic process have been recently described. The number of thrombotic plaques, the necrotic area and the hemorrhagic extension were significantly lower in women than men undergoing surgical carotid endarterectomy [27]. Moreover, inflammation (as assessed by various indices) was less pronounced in women than in men. Similar findings were observed using magnetic resonance imaging in patients with carotid atherosclerosis [28]. A recent review reported that carotid plaques were more stable in women than men affecting the outcome of carotid endarterectomy [29].
Comorbidities
The prevalence of traditional cardiovascular risk factors like central obesity and hypercholesterolemia was higher in women than in men with hypertension in the 1999–2004 NHANES survey [30].
Although the prevalence of obesity is not significantly different between female and male individuals (35.6 % versus 33.6 %), significant gender divergence is observed in African-Americans (53.9 % versus 37.9 %) [31]. The association of hypertension with obesity seems to be gender and age-related, and the prevalence of hypertension and obesity is lower in premenopausal women than in men [32]. A recent observational study in almost 30,000 young Japanese individuals reported a strong association of obesity with hypertension and prehypertension, which was significantly stronger in women than in men [33]. Sex differences in the association between abdominal and total obesity with hypertension have also been reported. A large cross-sectional study of more than 25,000 Chinese individuals reported that hypertension was associated more with abdominal than total adiposity in men over the age of 45 years, while the opposite association (with total obesity) was evident for women of all ages [34].
The prevalence of hypercholesterolemia is significantly higher in females than in males: 44.9 % versus 41.3 % for total cholesterol levels above 200 mg/dl, and 14.7 % versus 12.7 % for total cholesterol levels above 240 mg/dl. In contrast, HDL-cholestrol levels are consistently higher in women than in men and the prevalence of low HDL-cholesterol (<40 mg/dl) is 12.3 % for women versus 31.8 % for men [35]. Mean triglyceride levels are significantly higher among males (141.7 mg/dl) than females (119.1 mg/dl), while no significant gender differences are noted for LDL-cholesterol levels. It is clinically significant that LDL-cholesterol control rates remain disappointingly low, especially for men (22.6 %) versus women (26.9 %) [35].
A recent analysis of more than 10,000 patients from the ARIC, CARDIA, and the Framingham Heart Study revealed that incident diabetes mellitus type 2 was directly associated with baseline blood pressure levels [36•]. Hypertensive patients were at increased risk to develop diabetes than prehypertensive and normotensive individuals. In addition, race and gender differences were observed: (1) diabetes incidence rates were higher among African-Americans than Caucasians, and (2) incidence rates were higher in women than men in hypertensive African-Americans, while the opposite was observed in hypertensive Caucasians.
An association between hypertension and cancer has been previously suggested but available data is controversial. In a large prospective observational study of seven European cohorts from Norway, Austria, and Sweden with more than half a million participants, significant gender-based differences were reported, since blood pressure increment by 10 mmHg was significantly associated to total incident cancer in men but not in women [37•]. Moreover, gender differences were observed by cancer site: increased blood pressure was associated with cancer of oropharynx, colon, rectum, lung, bladder, kidney, and skin (melanoma and non-melanoma) in men; cancer of the liver, pancreas, cervix, uterine corpus, and melanoma in women. In our opinion, the relationship of hypertension with cancer is intriguing but should be examined with skepticism and great caution, until a definite association and gender differences are proved.
Target Organ Damage
A recent review of 26 studies with more than 12,000 patients showed that the prevalence of left ventricular hypertrophy (assessed by electrocardiography) was gender-related affecting 16 % of women and 24 % of men with hypertension [38•]. Gender differences in echocardiographically assessed left ventricular hypertrophy have been also described, however contradictory results are available in the literature. Regression of left ventricular hypertrophy was less pronounced in women than in men in the LIFE study, even after adjustments for confounders [39].
A sexual dimorphism in left ventricular structural and functional alterations induced by hypertension has been reported. Hypertension-induced left ventricular hypertrophy is different in female and male patients, since hypertensive women are more likely to develop concentric hypertrophy while eccentric hypertrophy is more common among men [40]. Left ventricular hypertrophy is common in hypertensive women and increases with age, achieving a prevalence of 80 % among nonagenarians [41].
Gender differences in left ventricular diastolic function are less clear, since contradictory data exists. A recent report using cutting-edge technology (magnetic resonance tissue phase mapping of myocardial motion) showed that diastolic function was enhanced in women compared to men at a younger age, while this association was reversed at the older age and the loss of function was greater in women than in men [42].
Heart failure appears either with reduced or preserved ejection fraction in approximately equal frequency. Although it is still unclarified whether these two forms are completely distinct or simply ends of a same continuum, heart failure with preserved ejection fraction is without any doubt significantly more common in female patients, as women outnumber men by a 2:1 ratio [43]. Heart failure with preserved ejection fraction is currently attributed to a global limitation in cardiovascular reserve affecting multiple functional domains. In particular, vascular, endothelial, and chronotropic impairments act synergistically and result in heart failure symptoms [44]. Gender differences in any of these factors may account for the observed inequality in prevalence. Indeed, a study from the Framingham project showed that flow-mediated dilatation abnormalities are more prevalent in older women than men (38 % versus 20 % respectively) [45].
Abnormalities in dynamic ventricular-vascular coupling are more frequent in hypertensive women than men both at rest and during exercise [46]. Arterial stiffening is enhanced with aging and hypertension resulting in faster transmission of antegrade and reflected waves. Arterial stiffness becomes more pronounced in postmenopausal women than men [47], leading to greater pulsatile afterload and subsequent diastolic dysfunction. This gender difference has been highlighted in a recent study, in which arterial stiffness was inversely related to diastolic function only in women [48].
Carotid media thickness is considered an independent predictor of cardiovascular events. Significant differences among male and female individuals were observed in almost 5,000 individuals participating in the Gutenberg Heart Study, for a median intima-media thickness of 0.67 mm in hypertensive women versus 0.69 mm in hypertensive men [49]. Similarly, carotid plaques were more common in hypertensive men than women (57 % versus 45.3 %).
Males have a faster decline of renal function with age than females; however, this gender association is reversed in older age and postmenopausal women experience a more rapid deterioration of renal function than male individuals [50]. Estrogen seems to exert beneficial actions on renal function. Postmenopausal women have higher levels of fibroblast groth factor-23 (a predictor of renal disease progression) compared to men or women who are on replacement therapy [51]. Experimental data support the renoprotective effect of estrogens, since the progression of glomerulosclerosis is accelerated in estrogen-deficient mice [52].
Contradictory findings exist in the literature regarding the impact of gender on the prevalence of chronic kidney disease. The prevalence of chronic kidney disease in women was found lower, similar, or higher than in men in different population cohorts. In a recent Italian study of about 3,500 hypertensive patients attending specialized centers, it was found that the prevalence of microalbuminuria was lower in women than in men, while the prevalence of reduced eGFR was higher in women [53].
Cardiovascular Risk
A voluminous amount of evidence indicates that women are at a lower cardiovascular risk than men before menopause, while the risk for cardiovascular events increases significantly after menopause so that female cardiovascular risk eclipses male in late life. The 1999–2004 NHANES survey demonstrated a higher cardiovascular risk profile in women than in men, since at least three risk factors were identified in more women than men (53 % versus 41 %). In a recent report from the Nurses Health Study it was found that incident hypertension can be prevented in a significant percentage of individuals through lifestyle and dietary intervention [24].
About one in three adults do not engage in leisure-time physical activity. Females are more prone than males to be physically inactive at all ages (33.2 % versus 29.9 %) and physical inactivity advances with age; its prevalence increases from 26 % in younger age to 52 % in older age (>75 years) [54]. A recent report from Australia suggests that 76 % of women are not adequately active compared to 68 % of men [55]. The corresponding US rates were 54.5 % for women and 47.3 % for men [54]. Gender differences also exist in individuals achieving the 2008 Federal physical activity guidelines (17 % females, 25 % males). However, these data are based on questionnaires. When objective assessments with accelerometers are used, a dramatic drop in rates of adequate physical activity is observed, achieving levels of 2–3 %. Indeed, a recent systematic review found that self-reported physical activity was significantly greater than the objectively measured activity by 138 % in women and by 44 % in men [56].
Gender differences in all-cause mortality according to salt-sensitivity have been recently reported. Increased salt sensitivity was strongly associated with all-cause mortality in men, while no association was found in women [57]. However, salt-sensitivity was assessed indirectly by using ambulatory blood pressure and heart rate indices, limiting the validity of study findings.
Pulse pressure amplification, i.e., the consistently higher blood pressure in peripheral than central arteries, is a result of arterial stiffening and is particularly increased in post-menopausal women [58]. Recently, pulse pressure amplification (expressed as branchial to carotid pulse pressure ratio) was found to be independently associated with cardiovascular and all-cause mortality in a large cohort of more than 120,000 French individuals [59•]. This association was significantly stronger in women than in men, and more importantly was markedly enhanced with aging only in women and not in men. This finding highlights the alterations in arterial elasticity that take place after menopause due to estrogen loss.
Visit-to-visit blood pressure variability has been recently introduced as a strong independent predictor of cardiovascular morbidity and mortality in hypertensive patients [60, 61]. It has to be kept in mind however that these were findings from post hoc analyses of randomized studies carrying the inherent limitations of such analyses. A recent report of almost 3,000 participants in the Flemish population study failed to show any association between visit-to-visit blood pressure variability and cardiovascular outcomes, except for women in whom blood pressure variability was an independent predictor of cardiovascular events [62]. Another recent report from a large population study in England of more than 20,000 patients with a follow-up period of 29 years revealed that transiently high readings of diastolic blood pressure (suggesting higher blood pressure variability) were strongly associated with cardiovascular and all-cause mortality only in women and not in men [63]. In our opinion, the abovementioned data suggests that the concept of visit-to-visit variability remains controversial and future studies are needed to prove this concept, clarify its clinical significance, and evaluate whether gender differences truly exist.
Cardiovascular Risk Assessment
Middle-aged women have a substantial lifetime risk for cardiovascular disease. The presence of comorbidities increases the 30-year cardiovascular risk to 42 % in women at the age of 45 [64].
Gender differences in the management of hypertensive patients seem to exist. A recent study among French cardiologists treating about 3,500 hypertensive patients revealed that significantly fewer tests have been performed in women than in men to assess for myocardial ischemia (gender bias) [65]. Female patients are less likely to receive optimal evidence-based therapy and appropriate diagnostic procedures (gender bias) [66].
A very large study of over 9,000 patients undergoing ambulatory blood pressure monitoring found that the proportion of preventable cardiovascular complications is greater in women than in men, despite a lower absolute cardiovascular risk [67•]. In this study, a steeper relationship between blood pressure and cardiovascular events was observed in female compared to male participants. The impact of nighttime blood pressure on cardiovascular outcomes was higher in women than in men. Despite a lower absolute cardiovascular risk in women, the preventable cardiovascular risk is significantly higher (by 30 %-100 %) in women. The clinical significance of this observation for cardiovascular risk prediction remains to be elucidated.
Hypertension in pregnancy emerged as a significant risk factor for future hypertension and cardiovascular events. Preeclampsia is associated with a fourfold increased risk for chronic hypertension, a threefold increased risk for diabetes mellitus, and a twofold increased risk for stroke and coronary heart disease [68–70]. In addition, risk increments observed with preeclampsia are significantly enhanced by the concomitant presence of other abnormalities, such as preterm birth [71]. The importance of a hypertensive disorder during pregnancy in female cardiovascular risk prediction has been acknowledged in the latest guidelines of the American Heart Association [72]. However, this opportunity is frequently missed in everyday clinical practice, since most obstetricians are not aware of the association between the future sequelae of preeclampsia [73•].
Significant gender differences in estimated lifetime medical expenditures for hypertensive men and women have been reported, with an estimated expenditure of about $250,000 for a 20-year-old hypertensive woman compared to about $190,000 for a hypertensive man of the same age [74], possibly due to greater longevity among women. However, the hypertension-attributable lifetime expenditure was more than double in men than in women, suggesting that diagnostic and therapeutic approaches vary significantly among the two genders.
Morbidity and Mortality
It has been estimated that the overall life expectancy for 50 years old individuals is 4.9 years shorter for hypertensive women and 5.1 years shorter for hypertensive men compared to normotensive individuals of the same age [75].
A recent analysis of stroke mortality in 39 countries of Europe and Central Asia revealed a disproportional toll among women, who largely outnumbered stroke deaths compared to men (739,000 versus 487,000 deaths, respectively) [76]. Stroke rates followed an age-dependent pattern, with lower rates at younger age and higher rates at older age. Since the vast majority of stroke deaths occur in the elderly, the greater longevity of women seems to account for this difference along with a potential ‘survivor effect’ among men reaching older ages.
Gender differences in the prognosis of heart failure patients have been described, however not universally identified in randomized and observational studies. A recent meta-analysis of 31 studies with more than 40,000 patients with heart failure demonstrated that mortality was lower in women than in men, irrespective of the ejection fraction [77]. The female survival benefit was also evident in hypertensive women who comprised about half of studied patients. Of note, lower mortality rates in women were observed despite lower prescription rates of renin–angiotensin system inhibitors.
A recent report evaluated the trends in cardiovascular and all-cause mortality among hypertensive and normotensive individuals, using the 1971–1975 and the 1988–-1994 NHANES surveys [78]. Mortality rates were higher in hypertensive than normotensive individuals, and in hypertensive men compared to women in both surveys. A significant reduction in mortality rates was observed in the second survey; however, the reduction was much more pronounced in hypertensive men than women. This subpar reduction is worrisome and if confirmed in recent surveys calls for intense public health efforts to attenuate this gender disparity. A similar trend was observed in stroke incidence rates in the Netherlands, with a substantial reduction (34 %) in men between the 1990 and 2000 cohorts compared to no change in women [79]. Mortality trajectories in hypertensive patients are influenced by the other traditional risk factors (smoking, obesity, diabetes mellitus, dyslipidemia), which may significantly affect mortality along with other existing comorbidities.
History of hypertension is identified in the vast majority of patients experiencing stroke, heart attack, and congestive heart failure [80]. Recently, a large study of more than 170,000 US patients with incident hypertension was published [81]. Women compared to men with incident hypertension were significantly less likely to suffer from myocardial infarction and stroke or die from any cause, while they were significantly more likely to develop chronic kidney disease. Despite the large number of study participants, several limitations need to be noted. First, significant differences in baseline characteristics existed which might have influenced the outcome. Then, information about the use of antihypertensive medication was not provided. Gender-related dissimilarities in prescription of the various antihypertensive drug classes due to either physicians’ habits or based on existing differences in patients’ profile and comorbidities might significantly affect the outcome. Finally, gender-related differences on the effects of antihypertensive drugs might also be implicated. The latter two speculations are addressed in the next chapter.
Antihypertensive Therapy
The impact of lifestyle and dietary factors in the development of hypertension is imperative. Normal weight, physical activity, and adoption of a healthy diet was associated with a significantly lower risk for incident hypertension in the second Nurses’ Health Study [24].
Data from some small clinical studies suggest that gender differences in blood pressure response might exist. For example, a prospective study comparing the effects of amlodipine monotherapy in men and women suggested that diastolic blood pressure reduction was greater in women than in men, and blood pressure control was achieved in more women than men [82]. Similarly, greater blood pressure reductions were recently observed in women using the combination of angiotensin receptor blockers with hydrochlorothiazide [83, 84].
No significant differences in blood pressure reduction between men and women were observed in almost all large, prospective, randomized trials in the hypertension arena. However, some minor differences might be identified. In the ALLHAT study, blood pressure reduction was greater with amlodipine than with lisinopril, and was associated with reduced stroke rates [85]. In the VALUE trial, cardiovascular morbidity and mortality was greater with valsartan compared to amlodipine in women but not in men [86]. It has to be noted however that these findings are not convincing and should probably be disregarded since in the vast majority of prospective, randomized, large clinical trials gender differences in blood pressure control have not been observed.
Gender differences in the long-term cardiovascular benefits of antihypertensive therapy have been also described. In two older studies (Heart Attack Trial and Hypertension Care Computing Project), beta blockers were associated with reduced mortality only in men and not in women [87, 88]. The Second Australian National Blood Pressure study raised a lot of concerns about the efficacy of ACE-inhibitors in women [89]. A significant reduction in cardiovascular events was demonstrated in men using ACE-inhibitors when compared to diuretic use, while there were no differences in cardiovascular outcomes between the two drugs in women despite a similar blood pressure reduction in both sexes.
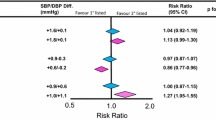
The impact of gender on the benefits of antihypertensive therapy has been the subject of a large meta-analysis by the Blood Pressure Lowering Treatment Trialists’ Collaboration, which included 31 randomized trials with about 100,000 men and 90,000 women with hypertension [90]. No significant differences in cardiovascular outcomes between men and women were observed. Moreover, there was no convincing sign that the various antihypertensive drug classes exert gender-related blood pressure lowering effects or cardiovascular protection. These findings provide strong evidence that the efficacy of antihypertensive drugs is similar in men and women, regarding both blood pressure reduction and long-term cardiovascular risk reduction.
Although this meta-analysis established the absence of any significant impact of gender on blood pressure response to antihypertensive therapy and on cardiovascular outcomes, a closer look unveils some minor differences. For example, calcium antagonists offered greater benefits in stroke prevention than ACE-inhibitors in women when compared to men, while calcium antagonists compared to placebo reduced all-cause mortality in males but not in females. However, these gender differences might be attributed to chance given the significant number of performed comparisons.
An analysis of more than 12,000 visits in primary care providers revealed that diuretics were more frequently used in women (20.9 % versus 16.9 %), while ACE-inhibitors were more frequently used in men (28.7 % versus 20.9 %) [91]. The more frequent use of diuretics in women might be attributed to the observed effects of diuretics in reducing hip fractures in older women [92].
Adverse effects of antihypertensive therapy were twice as frequent in women as in men in the TOMHS study [93]. A similar greater frequency of adverse effects in women was observed in the LIFE study, however serious adverse effects were more common among men [94]. Dry cough is more common in women than men; genetic polymorphisms in ABO have been recently proposed as candidate mediators of ACE-inhibitors induced cough [95], but further studies are needed to establish the clinical significance of this observation. A higher incidence of edema with calcium antagonists is observed in women than in men, which is frequently associated with a greater therapeutic response [82]. Diuretic-induced adverse drug effects are more frequently experienced by women than men. Women are more likely to experience hypokalemia and hyponatremia and less likely to experience gout with diuretics [96].
Sexual dysfunction is more common among hypertensive women than men and is significantly related to beta blockers in female patients [97]. Antihypertensive drugs seem to exert different effects on sexual function with older drugs (beta blockers, diuretics, centrally acting) being detrimental, and newer agents being either neutral (calcium antagonists, ACE-inhibitors) or even beneficial (angiotensin receptor blockers, nebivolol) [98].
Conclusions
Awareness, treatment, and control rates of hypertension are higher among women than men; however control rates are lower in older hypertensive women. The pathophysiologic mechanisms underlying the age-dependent differences between the two genders are poorly defined, with hormonal and mechanical factors being the prevailing candidates. Gender differences exist in target organ damage and comorbidities in hypertensive patients affecting the overall cardiovascular risk. Cardiovascular morbidity and mortality present some differences between male and female hypertensive patients. Data from large clinical trials and a meta-analysis offer strong evidence that the effects of antihypertensive therapy are similar between men and women regarding the reduction in both blood pressure levels and cardiovascular events.
Further intense clinical research is needed to uncover potential gender differences in hypertension and antihypertensive therapy not only in the general population but also in specific subgroups, such as patients with concomitant diabetes, overt cardiovascular disease, chronic kidney disease, and the very elderly. Moreover, further basic research is of paramount importance to uncover the biological plausibility and the mechanisms mediating potential gender differences in hypertension and associated cardiovascular disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kannel WB, Schwartz MJ, McNamara PM. Blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Chest. 1969;56:43–51.
Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care and outcomes. Lancet Neurol. 2008;7:915–26.
Wong C, Froelicher E, Bacchetti P, et al. In a managed care setting, are there sex differences in the use of coronary angiography after acute myocardial infarction? Am Heart J. 1998;135:435–42.
Melloni C, Berger JS, Wang TY, et al. Representation of women in randomized clinical trials of cardiovascular disease prevention. Circulation. 2010;3:135–42.
•• Go A, Mozaffarian D, Roger V, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e77–86. A very significant annual report showing higher awareness, treatment, and control rates among women compared to men. Control rates were consistently higher in men for decades and this trend was reversed for the first time.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–50.
Fletcher RD, Amdur RL, Kolodner R, et al. Blood pressure control among US veterans: a large multiyear analysis of blood pressure data from the Veterans Administration health data repository. Circulation. 2012;125:2462–8.
McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A Biol Sci Med Sci. 2009;64:256–63.
Daugherty SL, Masoudi FA, Ellis JL, et al. Age-dependent gender differences in hypertension management. J Hypertens. 2011;29:1005–11.
Robitaille C, Dai S, Waters C, et al. Diagnosed hypertension in Canada: incidence, prevalence and associated mortality. CMAJ. 2012;184:E49–56.
Prince M, Ebrahim S, Acosta D, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2011;30:177–87.
Gee M, Bienek A, McAlister F, et al. Factors associated with lack of awareness and uncontrolled high blood pressure among Canadian adults with hypertension. Can J Cardiol. 2012;28:375–82.
Orshal JM, Khalil RA. Gender, sex hormones, and vascular tone. Am J Physiol Regul Integr Comp Physiol. 2004;286:R233–49.
• Wang L, Szklo M, Folsom A, et al. Endogenous sex hormones, blood pressure change, and risk of hypertension in post-menopausal women: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2012;224:228–34. An important study that uncovers the role of sex hormones in blood pressure elevation in post-menopausal women.
Casiglia E, Tikhonoff V, Caffi S, et al. Menopause does not affect blood pressure and risk profile, and menopausal women do not become similar to men. J Hypertens. 2008;26:1983–92.
Carter J, Fu Q, Minson C, Joyner M. Ovarian cycle and sympathoexcitation in premenopausal women. Hypertension. 2013;61:395–9.
Tsuda K. Roles of sex steroid hormones and nitric oxide in the regulation of sympathetic nerve activity in women. Hypertension. 2013;61:e36.
Hart E, Charkoudian N, Wallin B, et al. Sex and ageing differences in resting arterial pressure regulation: the role of b-adrenergic receptors. J Physiol (London). 2011;589:5285–97.
Doumas M, Faselis C, Papademetriou V. Renal sympathetic denervation in hypertension. Curr Opin Nephrol Hypertens. 2011;20:647–53.
•• Schlaich M, Straznicky N, Grima M, et al. Renal denervation: a potential new treatment modality for polycystic ovary syndrome? J Hypertens. 2011;29:991–6. A very significant proof-of-concept study which highlighted the role of sympathetic nervous system in the pathogenesis of polycystic ovary syndrome. Renal sympathetic denervation not only reduced blood pressure but also improved the severity of the disease itself.
Rands V, Dale M, Kobori H, Prieto M. Sexual dimorphism in urinary angiotensinogen excretion during chronic angiotensin II-salt hypertension. Gend Med. 2012;9:207–18.
Perchere-Bertschi A, Burnier M. Female sex hormones, salt, and blood pressure regulation. Am J Hypertens. 2004;17:994–1001.
Forman J, Stampfer M, Curhan G. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–11.
Kittikulsuth W, Sullivan J, Pollock D. ET-1 actions in the kidney: evidence for sex differences. Br J Pharmacol. 2013;168:318–26.
Kittikulsuth W, Pollock J, Pollock D. Sex differences in renal medullary endothelin receptor function in angiotensin II hypertensive rats. Hypertension. 2011;58:212–8.
Cheng S, Xanthakis V, Sullivan L, Vasan R. Blood pressure tracking over the adult life course. Hypertension. 2012;60:1393–9.
Sangiorgi G, Roversi S, Biondi-Zoccai G, et al. Sex-related differences in carotid plaque features and inflammation. J Vasc Surg. 2013;57:338–44.
Ota H, Reeves M, Zhu D, et al. Sex differences in patients with asymptomatic carotid atherosclerotic plaque. In vivo 3.0-T magnetic resonance study. Stroke. 2010;41:1630–5.
Den Harrog A, Algra A, Moll F, de Borst G. Mechanisms of gender-related outcome differences after carotid endarterectomy. J Vasc Surg. 2010;52:1062–71.
Ong K, Tso A, Lam K, Cheung B. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008;51:1142–8.
Go A, Mozaffarian D, Roger V, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e59–67.
Yanes L, Reckelhoff J. Postmenopausal hypertension. Am J Hypertens. 2011;24:740–9.
Wakabayashi I. Stronger associations of obesity with prehypertension and hypertension in young women than in young men. J Hypertens. 2012;30:1423–9.
Deng WW, Wang J, Liu MM, et al. Body mass index compared with abdominal obesity indicators in relation to prehypertension and hypertension in adults: the CHPSNE study. Am J Hypertens. 2013;26:58–67.
Go A, Mozaffarian D, Roger V, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e72–6.
• Wei G, Coady S, Goff D, et al. Blood pressure and the risk of developing diabetes in African American and Whites. Diabetes Care. 2011;34:873–9. An important analysis of data from three large studies (ARIC, CARDIA, Framingham) revealing that the development of diabetes depends on baseline blood pressure and incident diabetes among hypertensive patients is more frequent in female African-Americans and male Caucasians.
• Stocks T, van Hemelrijck M, Manjer J, et al. Blood pressure and risk of cancer incidence and mortality in the metabolic syndrome and cancer project. Hypertension. 2012;59:802–10. A significant study suggesting that hypertension might be associated with cancer in women but not in men. However, further research is needed in this field before jumping to definite conclusions.
• Cuspidi C, Rescaldani M, Sala C, et al. Prevalence of electrocardiographic left ventricular hypertrophy in human hypertension: an updated review. J Hypertens. 2012;30:2066–73. A valuable meta-analysis showing that left ventricular hypertrophy, as assessed by electrocardiography, is more prevalent in men than in women with hypertension.
Okin P, Gerdts E, Kjeldsen S, et al. Gender difference in regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy. Hypertension. 2008;52:100–6.
Piro M, Della Bona R, Abbate A, et al. Sex-related differences in myocardial remodeling. J Am Coll Cardiol. 2010;55:1057–65.
Koster NK, Reddy YM, Schima SM, Almeida NJ. Gender-specific echocardiographic findings in nonagenarians with cardiovascular disease. Am J Cardiol. 2010;105:273–6.
Foll D, Jung B, Schilli E, et al. Magnetic resonance tissue phase mapping of myocardial motion: new insight in age and gender. Circ Cardiovasc Imaging. 2010;3:54–64.
Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–14.
Borlaug BA, Olson TP, Lam CS, et al. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J Am Coll Cardiol. 2010;56:845–54.
Hamburg NM, Palmisano J, Larson MG, et al. Relation of brachial and digital measures of vascular function in the community: the Framingham heart study. Hypertension. 2011;57:390–6.
Chantler PD, Melenovsky V, Schulman SP, et al. The sex-specific impact of systolic hypertension and systolic blood pressure on arterial-ventricular coupling at rest and during exercise. Am J Physiol. 2008;295:H145–53.
Rossi P, Frances Y, Kingwell BA, Ahimastos AA. Gender differences in artery wall biomechanical properties throughout life. J Hypertens. 2011;29:1023–33.
Shim CY, Park S, Choi D, et al. Sex differences in central hemodynamics and their relationship to left ventricular diastolic function. J Am Coll Cardiol. 2011;57:1226–33.
Sinning C, Wild P, Echevarria F, et al. Sex differences in early carotid atherosclerosis (from the community-based Gutenberg-Heart study). Am J Cardiol. 2011;107:1841–7.
Neugarten J, Acharaya A, Silbiger S. Effect of gender on the progression of nondiabetic renal disease: a meta-analysis. J Am Soc Nephrol. 2000;11:319–29.
Ix J, Chonchol M, Laughlin G, Shlipak M, Whooley M. Relation of sex and estrogen therapy to serum fibroblast growth factor 23, serum phosphorus, and urine phosphorus: the Heart and Soul study. Am J Kidney Dis. 2011;58:737–45.
Doublier S, Lupia E, Catanuto P, Elliot S. Estrogens and progression of diabetic kidney damage. Curr Diabetes Rev. 2011;7:28–34.
Mueisan M, Ambrosioni E, Costa F, et al. Sex differences in hypertension-related renal and cardiovascular diseases in Italy: the I-DEMAND study. J Hypertens. 2012;30:2378–86.
Schiller J, Lucas J, Peregoy J. Summary health statistics for US adults: National Health Interview Survey 2010. Vital Health Stat. 2012;252:1–207.
AIHW. Women and heart disease: cardiovascular profile of women in Australia. Report. Cardiovascular disease series no 33. Cat no CVD 49. 2010.
Prince S, Adamo K, Hamel M, et al. A comparison of direct versus self-reported measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56–67.
Bursztyn M, Ben-Dov I. Sex differences in salt-sensitivity risk approximated from ambulatory blood pressure monitoring and mortality. J Hypertens. 2013;31:900–5.
Benetos A, Thomas A, Joly L, et al. Pulse pressure amplification, a mechanical biomarker of cardiovascular risk. J Am Coll Cardiol. 2010;55:1032–7.
• Regnault V, Thomas F, Safar M, et al. Sex difference in cardiovascular risk: role of pulse pressure amplification. J Am Coll Cardiol. 2012;59:1771–7. An important study proposing pulse pressure amplification as a novel potential predictor of cardiovascular risk.
Rothwell P, Howard S, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905.
Rothwell P, Howard S, Dolan E, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–80.
Schutte R, Thijs L, Liu YP, et al. Within-subject blood pressure level – not variability – predicts fatal and nonfatal outcomes in a general population. Hypertension. 2012;60:1138–47.
Peters R, Wells F, Bulpitt C, Beckett N. Impact of transiently elevated diastolic pressure on cause of death: 29-year follow-up from the General Practice Hypertension Study Group. J Hypertens. 2013;31:71–6.
Pencina M, D’Agostino R, Larson M, Massaro J, Vasan R. Predicting the 30-year risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:3078–84.
Mounier-Vehier C, Simon T, Guedj-Meynier D, et al. Gender-related differences in the management of hypertension by cardiologists: the PARITE study. Arch Cardiovasc Dis. 2012;105:271–80.
Ciambrone G, Kaski J. The importance of gender differences in the diagnosis and management of cardiovascular disease. Curr Pharm Des. 2011;17:1079–81.
• Boggia J, Thijs L, Hansen T, et al. Ambulatory blood pressure monitoring in 9357 subjects from 11 populations highlights missed opportunities for cardiovascular prevention in women. Hypertension. 2011;57:397–405. This significant clinical study in a large number of patients showed that the preventable cardiovascular risk is significantly higher in women than in men.
Lykke J, Langhoff-Roos J, Sibai B, et al. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–51.
McDonald S, Malinowski A, Zhou Q, Yusuf S, Devereaux P. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156:918–30.
Bellamy L, Casas J, Hingorani A, Williams D. Preeclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974–86.
Mongraw-Chaffin M, Cirillo P, Cohn B. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 2010;56:166–71.
Mosca L, Benjamin E, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women – 2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243–62.
• Schmittdiel J, Selby J, Swain B, et al. Missed opportunities in cardiovascular disease prevention? Low rates of hypertension recognition for women at medicine and obstetrics-gynecology clinics. Hypertension. 2011;57:717–22. This significant report highlights missed opportunities in everyday clinical practice for female cardiovascular risk prevention due to physicians’ lack of familiarity with the future cardiovascular sequelae of preeclampsia.
Basu R, Krueger P, Lairson D, Franzini L. Lifetime medical expenditures among hypertensive men and women in the United States. Women Health Issues. 2011;21:246–53.
Franco O, Peeters A, Bonneux L, de Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–6.
Redon J, Olsen M, Cooper R, et al. Stroke mortality and trends from 1990 to 2006 in 39 countries from Europe and Central Asia: implications for control of high blood pressure. Eur Heart J. 2011;32:1424–31.
Martinez-Selles M, Doughty R, Poppe K, et al. Gender and survival in patients with heart failure: interactions with diabetes and aetiology. Results from the MAGGIC individual patient meta-analysis. Eur J Heart Fail. 2012;14:473–9.
Ford E. Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation. 2011;123:1737–44.
Wieberdink R, Ikram M, Hofman A, Koudstaal P, Breteler M. Trends in stroke incidence rates and stroke risk factors in Rotterdam, the Netherlands from 1990 to 2008. Eur J Epidemiol. 2012;27:287–95.
Go A, Mozaffarian D, Roger V, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e109–21.
Daugherty S, Masoudi F, Zeng C, et al. Sex differences in cardiovascular outcomes in patients with incident hypertension. J Hypertens. 2013;31:271–7.
Kloner R, Sowers J, DiBona G, et al. Sex- and age-related antihypertensive effects of amlodipine. The Amlodipine Cardiovascular Community Trial Study Group. Am J Cardiol. 1996;77:713–22.
Saunders E, Cable G, Neutel J. Predictors of blood pressure response to angiotensin receptor blocker/diuretic combination therapy: a secondary analysis of the irbesartan/hydrochlorothiazide blood pressure reductions in diverse patient populations (INCLUSIVE) study. J Clin Hypertens (Greenwich). 2008;10:27–33.
Everett BM, Glynn RJ, Danielson E, Ridker PM. Combination therapy versus monotherapy as initial treatment for stage 2 hypertension: a prespecified subgroup analysis of a community-based, randomized, open-label trial. Clin Ther. 2008;30:661–72.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981–97.
Zanchetti A, Julius S, Kjeldsen S, et al. Outcomes in subgroups of hypertensive patients treated with regimens based on valsartan and amlodipine: an analysis of findings from the VALUE trial. J Hypertens. 2006;24:2163–8.
b-Blocker Heart Attack Trial Research Group. A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA. 1982;247:1707–14.
Fletcher A, Beevers DG, Bulpitt C, et al. Beta adrenoceptor blockade is associated with increased survival in male but not female hypertensive patients: a report from the DHSS Hypertension Care Computing Project (DHCCP). J Hum Hypertens. 1988;2:219–27.
Wing L, Reid C, Ryan P, et al. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348:583–92.
Turnbull F, Woodward M, Neal B, et al. Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J. 2008;29:2669–80.
Keyhani S, Scobie JV, Hebert PL, McLaughlin MA. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension. 2008;51:1149–55.
Schoofs MW, van der Klift M, Hofman A, et al. Thiazide diuretics and the risk for hip fracture. Ann Intern Med. 2003;139:476–82.
Lewis CE, Grandits A, Flack J, McDonald R, Elmer PJ. Efficacy and tolerance of antihypertensive treatment in men and women with stage 1 diastolic hypertension. Results of the Treatment of Mild Hypertension Study. Arch Intern Med. 1996;156:377–85.
Os I, Franco V, Kjeldsen SE, et al. Effects of losartan in women with hypertension and left ventricular hypertrophy: results from the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension. 2008;51:1103–8.
Mas S, Gasso P, Alvarez S, et al. Pharmacogenetic predictors of angiotensin-converting enzyme inhibitor-induced cough: the role of ACE, ABO, and BDKRB2 genes. Pharmacogenet Genomics. 2011;21:531–8.
Pemu PI, Ofili E. Hypertension in women—part I. J Clin Hypertens (Greenwich). 2008;10:406–10.
Manolis A, Doumas M. Antihypertensive treatment and sexual dysfunction. Curr Hypertens Rep. 2012;14:285–92.
Viigimaa M, Doumas M, Vlachopoulos C, et al. Hypertension and sexual dysfunction: time to act. J Hypertens. 2011;29:403–7.
Conflict of Interest
Michael Doumas declares that he has no conflict of interest
Vasilios Papademetriou declares that he has no conflict of interest
Charles Faselis declares that he has no conflict of interest
Peter Kokkinos declares that he has no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doumas, M., Papademetriou, V., Faselis, C. et al. Gender Differences in Hypertension: Myths and Reality. Curr Hypertens Rep 15, 321–330 (2013). https://doi.org/10.1007/s11906-013-0359-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-013-0359-y