Abstract
Hypertension is a common clinical problem and a major risk factor for cardiovascular disease and stroke. Elevated heart rate is associated with elevated blood pressure, increased risk for hypertension, and, among hypertensives, increased risk for cardiovascular disease. Despite these important relationships, heart rate is generally not a major consideration in choosing antihypertensive medications. In part, this is due to a lack of evidence supporting heart rate lowering as a therapeutic strategy in hypertension. Additionally, while there is a positive correlation between heart rate and peripheral blood pressure, there is an inverse relationship between heart rate and central blood pressure. The use of antihypertensive medications, specifically medications that affect heart rate, may not reliably reduce central blood pressure to a similar extent as observed peripherally. We review the relationship between heart rate and peripheral and central blood pressure, with a focus on the implications for chronotropic therapy in hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is a major public health problem and a known independent risk factor to cardiovascular disease. In the United States, recent data from the National Health and Nutrition Examination Survey (NHANES) report a prevalence of 30.5 % among men and 28.5 % among women [1]. For the calendar year of 2010, cost estimates attributed to hypertension have surpassed 90 billion dollars [2]. There is a continuous relationship between increasing blood pressure and cardiovascular disease, stroke, and end stage kidney disease (ESKD) [3, 4]. Management of hypertension is a significant focus of both primary care providers and hypertension specialists.
Numerous therapeutic options exist for the treatment of hypertension. Clinical situations for which certain classes of antihypertensive medications are specifically recommended include diabetes, proteinuric kidney diseases, and comorbid conditions, such as coronary artery disease (CAD) and congestive heart failure (CHF) [5]. Among patients with diabetes and nephropathy, treatment with angiotensin receptor blockers (ARBs) is recommended to reduce progression of kidney dysfunction and decrease rates of ESKD [6, 7]. Similarly, treating patients with heart failure with beta-blockers reduces all-cause mortality [8]. Absolute blood pressure is also a consideration in the treatment of hypertension; initiation of treatment with two drugs is recommended for patients with significantly elevated blood pressure [5]. Interestingly, the guidelines do not consider heart rate in choice of antihypertensive medications, despite the link between heart rate and development of hypertension and adverse cardiovascular outcomes. Herein, we review the link between heart rate and peripheral and central blood pressure, and the effect of chronotropic medications on blood pressures and adverse clinical outcomes.
Heart Rate, Blood Pressure, and Hypertension—Location, Location, Location
One rationale for consideration of heart rate in choosing antihypertensive medications comes from the observation that increased heart rate is a common feature in hypertensive patients and elevated heart rate is associated with development of hypertension [9••]. In the HARVEST study, 15 % of hypertensive patients had a resting heart rate > 85 beats per minute, and approximately 27 % had a heart rate > 80 beats per minute [9••]. Additionally, sustained elevations in heart rate over the course of the study were a strong predictor of developing hypertension necessitating pharmacologic therapy [10]. In a large general population cohort in France, heart rate was associated with blood pressure; hypertensive subjects had higher heart rates than normotensive subjects, with the greatest increase seen in those with moderate-severe hypertension [11]. In addition to elevated blood pressure, heart rate is also associated with other cardiovascular risk factors. Results from the Atherosclerosis Risk in Communities (ARIC) study demonstrate that a higher heart rate and lower heart rate variability were associated with an increased risk of incident diabetes, even when controlled for body mass index and physical activity [12]. Among patients at high cardiovascular risk in the VALUE trial, elevated baseline and in-trial heart rates were associated with increased risk for cardiovascular events and all-cause mortality, independent of achieved blood pressure [13•]. Finally, patients defined as “prehypertensive” with a heart rate ≥ 80 beats per minute were found to have a 50 % increase in all-cause mortality [14]. In summary, elevated heart rate is associated with elevated blood pressure, increased risk for development of hypertension (and diabetes), and all-cause mortality.
However, the relationship between heart rate and blood pressure is more complicated when both central and peripheral blood pressures are considered. The studies mentioned above measured blood pressure peripherally. Recent investigations have revealed the importance of central blood pressures and the conduction properties of the vasculature in relation to adverse outcomes. Typical office blood pressure measurement is obtained peripherally, usually from the brachial artery. Unfortunately, this measurement does not account for marked variability in vascular compliance, leading to differences of up to 20 mmHg between central and peripheral pressure measurements [15]. These marked differences have led to increased interest in detection of the central blood pressure profile as an important clinical marker for increased cardiovascular risk.
Assessment of the central pressure and pulse wave velocities (PWV) may provide insight into the vascular network and aortic stiffness. Measure of the carotid-femoral PWV is a validated, noninvasive technique that is accepted as the most simple, robust and reproducible method to determine arterial stiffness [16]. Risk factors for increased aortic PWV include increasing age, presence of diabetes, male gender, African American ethnicity, and hypertension [17••]. Additionally, in a cohort of subjects with chronic kidney disease (CKD), estimated glomerular filtration rate (GFR) was inversely related to PWV [17••]. PWV is an independent predictor of all-cause and cardiovascular mortality in the general population and CKD progression in patients with stage 4 and stage 5 CKD [18, 19]. On one hand, increased PWV may simply be a marker of cardiovascular and renal risk; however, increased PWV may contribute to increased risk by increasing central blood pressures.
The methods for measuring and the physiology of central blood pressure have recently been reviewed [20, 21]. Central blood pressure is typically calculated using a transfer function based on applanation tonometry measurements at the radial artery [16]. The central arterial pressure is a summation of forward pressure waves from ventricular contraction and backward reflection from the periphery [21]. The increase in central systolic pressure due to the reflected wave, the augmentation pressure, is often referred to as the augmentation index (augmentation pressure/central pulse pressure) [16]. As central arteries stiffen, PWV increases and reflected waves return earlier to the central aorta and “augment” the forward waves to increase central pressures [22, 23]. Not all studies have demonstrated a consistent relationship between PWV and augmentation index [24]. As with PWV, central blood pressures are independent predictors of cardiovascular outcomes and all-cause mortality [25]. In fact, central pulse pressure may be a more significant risk factor for clinical events than brachial pulse pressure [25]. In the Strong Heart Study, central pulse pressure was more strongly associated with cardiovascular outcomes than peripheral pulse pressure, which was not a significant predictor of events after adjustment for central pulse pressure [26].
The relationship between heart rate and blood pressure is location-dependent. As discussed above, there is a direct relationship between heart rate and peripheral blood pressure. However, a number of studies have demonstrated an inverse relationship between heart rate and central blood pressures. Among the offspring of patients with familial hypertension, heart rate was inversely related to the augmentation index [27]. Investigators have also evaluated the effect of increasing heart rate via pacing or pharmacologically. Wilkinson et al. demonstrated that increasing heart rate by pacing decreases augmentation index and central systolic blood pressure [28, 29]. Similarly, increasing heart rate via isoprenaline infusion was associated with a decrease in augmentation index [30]. The relationship between heart rate and augmentation index may be stronger in subjects with increased PWV [23]. In summary, while elevated heart rate is associated with increasing peripheral blood pressure, there appears to be an inverse relationship between heart rate, central blood pressure, and augmentation index. These varying relationships may have important therapeutic implications when considering antihypertensive medications that affect heart rate.
Effect of Beta-Blockade on Heart Rate and Blood Pressure
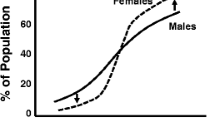
Currently, beta-blockers are recommended as a major therapeutic option in hypertensive patients in the setting of comorbidities, such as coronary artery disease and heart failure [5]. These therapies target a lower heart rate and decreased myocardial oxygen demand, in addition to lowering blood pressure. However, as might be expected from the previous discussion, studies consistently indicate that while traditional beta-blockers may reduce peripheral blood pressure, they are less effective at lowering central blood pressure. Compared to fosinopril, atenolol was equally efficacious at lowering peripheral blood pressure but not as effective at lowering augmentation index [31]. In a crossover study of 32 patients, atenolol was less effective at lowering aortic systolic blood pressure and augmentation pressure than angiotensin converting enzyme inhibitors (ACEi), calcium channel blockers, and diuretics [32]. A study of 393 patients with essential hypertension uncontrolled with 5 mg amlodipine compared the combination of amlodipine-valsartan to amlodipine-atenolol. After 24 weeks, central systolic blood pressure was lower in the amlodipine-valsartan group (P = 0.013) as was augmentation index (P < 0.001). There was no difference in brachial blood pressure or PWV [33••]. These studies indicate that while traditional beta-blockers lower heart rate and peripheral blood pressure, they are less effective at lowering central blood pressure. The lack of effectiveness at lowering central blood pressure may be exacerbated in patients with elevated PWV [23]. This interaction may explain the increased risk for stroke associated with beta-blockers in the elderly, a group with elevated PWV, and the opposite effect in younger subjects with normal PWV (Fig. 1) [34]. Recent studies indicate that newer beta-blockers with vasodilating properties might lower heart rate and both peripheral and central blood pressure, as well as augmentation index.
Relative risk for adverse outcomes associated with beta-blockers compared to other antihypertensive agents by age—a meta-analysis. Reprinted from J Am Coll Cardiol, 52, Bangalore S, Wild D, Parkar S, et al., Beta-blockers for primary prevention of heart failure in patients with hypertension. Insights from a meta-analysis, 1062–72, 2008, with permission from Elsevier.
Shah et al. demonstrated that carvedilol, a vasodilating beta-blocker, reduced augmentation index to a greater extent than beta-selective therapy with atenolol, which was actually associated with an increase in augmentation index (carvedilol −0.68 % vs. atenolol 4.47 %; P = 0.04) [35•]. Brachial blood pressure reductions were not significantly different between the two groups [35•]. Similar results were seen in a study that compared the use of nebivolol, a vasodilating beta-blocker, with metoprolol in 80 patients with hypertension [36••]. Results after one year demonstrated no difference in brachial blood pressure reduction but a greater decrease in central systolic blood pressure (P = 0.07) and central pulse pressure (P = 0.004) in subjects treated with nebivolol [36••]. A reduction in left ventricular mass was observed in the nebivolol arm although no comparison was made with the metoprolol arm; there was no difference in the augmentation index between the two arms of the study [36••]. Another study demonstrated reductions in the augmentation pressure and augmentation index with nebivolol versus atenolol [37]. In that study, change in heart rate was inversely related to augmentation pressure (r = −0.56, P < 0.001) and augmentation index. The mechanism for decreased central BP and augmentation index with vasodilating beta-blockers is unknown, but may be related to reduced pulse wave reflection via their effects on small arteries.
Heart Rate Lowering - Explanation for Clinical Trial Results?
Insight from short-term studies of the impact of beta-blockers and reduction in heart rate on central blood pressure and augmentation may provide an explanation of differing results from long-term clinical trials that include beta-blockers. As a result of effects on central blood pressure, studies may be more likely to report similar outcomes when beta-blockers are compared to antihypertensives that also lower heart rate. On the other hand, beta-blockers may have increased cardiovascular event rates when compared to antihypertensive regimens that do not lower heart rate. In the INVEST trial, over 20,000 patients with coronary artery disease were randomized to verapamil or atenolol based therapy [38]. At 24 months, there was no difference in blood pressure control or the rate of the primary cardiovascular composite [38]. It is noted that despite verapamil’s negative chronotropic effects, heart rate was lower at 24 months in the atenolol arm (69.2/min vs. 72.8/min, P < 0.01) [38]. Similar results were seen in the NORDIL study, in which there was no difference in the composite of stroke, myocardial infarction, or cardiovascular death among patients assigned to diltiazem or atenolol-thiazide based treatments [39]. It’s possible that the results in these trials comparing beta-blockade and calcium channel blockade are due to relatively similar effects of both classes on heart rate and peripheral and central blood pressure.
On the other hand, when beta-blockers are compared to agents that do not lower heart rate such as angiotensin receptors blockers, diuretics, and dihydropyridine calcium channel blockers, beta-blockers have been associated with increased rates of cardiovascular events. A few of these trials will be reviewed here. The LIFE trial evaluated the effect of losartan versus atenolol in 9,193 patients with hypertension, and demonstrated decreased rates of cardiovascular disease and stroke in subjects randomized to losartan [40]. The Medical Research Council (MRC) trial assigned hypertensive patients with a diastolic blood pressure < 115 mmHg to a diuretic, atenolol, or placebo [41]. Compared to placebo, treatment with a diuretic was associated with decreased risk for stroke, coronary heart disease, cardiovascular events, and cardiovascular death. No differences were observed between the atenolol and placebo groups [41]. In the ASCOT trial, lower rates of the primary cardiovascular outcome (stroke, cardiovascular events and procedures, and all-cause mortality) were observed in the amlodipine adding perindopril arm versus the atenolol adding a diuretic arm [42•]. The lower rate of adverse outcomes with amlodipine was independent of baseline heart rate indicating that, based on ASCOT, an elevated heart rate is not an indication for choosing a beta-blocker for management of hypertension [42•]. The ASCOT evaluation of central blood pressure provides a potential explanation for these results, and is reviewed below. The increased rate of cardiovascular events in the atenolol arms of the LIFE, MRC, and ASCOT trials may be due to lowering of heart rate, which may increase augmentation pressure and central blood pressure [43]. However, it is worth stating again that the beta-blocker used was atenolol, which is known to have an adverse side effect and metabolic profile [44].
The effect of atenolol on central blood pressure was addressed through the work of Williams et al. in the Conduit Artery Function Evaluation (CAFÉ) study, a sub-study of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) [45]. Both arms within the study contained protocols for titration of medications with additional therapies added to achieve a target blood pressure of < 140/90 mmHg for those without diabetes and < 130/80 mmHg for those with diabetes. In the CAFÉ subset of 2,073 patients in the ASCOT trial, radial applanation tonometry to calculate central pressure was performed [45]. There was no difference in brachial blood pressure or pulse pressure between the treatment arms, but atenolol was associated with lower heart rate and elevated central blood pressure and pulse pressure as well as augmentation index [45]. Lower heart rate was associated with increased central systolic blood pressure and pulse pressure [46•]. Central pulse pressure and augmentation were independent predictors of a composite of cardiovascular events and renal impairment [45]. While this is only one study, there does appear to be a direct link between heart rate lowering with atenolol, increased central blood pressure, and adverse outcomes.
Heart Rate, Blood Pressure, and Chronic Kidney Disease
The issues of heart rate reduction and hypertension control are magnified in patients with CKD. Decreased renal function is associated with elevated heart rate, hypertension, and significantly increased risk for cardiovascular disease [47–49]. In patients with CKD, elevated heart rate is associated with increased risk for cardiovascular disease [47]. Among 2,531 subjects in the Chronic Renal Insufficiency Cohort (CRIC) study, estimated GFR was associated with central pulse pressure on bivariate analyses, but was not retained as a predictor of central pulse pressure in multivariate models [50]. Treatment of patients with CKD with beta-blockade has been evaluated in one large study, the African American Study of Kidney Disease (AASK). In AASK, total GFR decline was slower in both ramipril and amlodipine compared to metoprolol [51]. The primary composite of a decline in GFR, ESKD or death was reduced in the ramipril arm compared to the metoprolol and amlodipine arms. No difference was observed in rates of cardiovascular mortality or cardiovascular events [51]. Further research in CKD patients is needed to evaluate the impact of heart rate lowering, preferably with newer vasodilatory beta-blockers, on renal and cardiovascular events in this high-risk population.
Beyond Heart Rate to Heart Rate Variability
Measurement of the time intervals from one ventricular contraction to the next allows for calculation of more than just the absolute heart rate. The beat-to-beat variability in heart rate can be measured in the time and frequency domains, is a measure of parasympathetic and sympathetic function, and is referred to as heart rate variability [52]. Low heart rate variability is associated with hypertension, CKD, and increased risk for all-cause mortality and ESKD [53–55]. Low heart rate variability is modifiable. Physical therapy improved heart rate variability in dialysis patients and patients after myocardial infarction [56, 57]. Finally, a small study of type 1 diabetic patients demonstrated an increase in heart rate variability with atenolol [58]. Whether changes in heart rate variability related to physical activity and different antihypertensive regimens modify blood pressure and clinical outcomes is unknown.
Conclusion
For a number of reasons, heart rate is considered an integral part of the assessment of the hypertensive patient. Elevated heart rate is associated with increased peripheral blood pressure, increased risk for cardiovascular disease, and is modifiable. However, in the absence of heart failure or coronary artery disease, treating hypertensive patients with heart rate lowering medications has not been shown to reduce adverse events when compared to active control. One possible explanation may be the increase in central blood pressure with the use of older beta-blockers. Newer vasodilatory beta-blockers do not appear to increase central blood pressure to the same extent, and may be effective antihypertensive agents with the potential to reduce rates of cardiovascular disease. Long-term, randomized controlled trials are needed to evaluate this hypothesis. The assessment of heart rate in hypertensive patients may be appropriate to evaluate adherence [59]. However, choosing antihypertensive medications based on heart rate or targeting a low heart rate in hypertensive patients cannot be recommended based on the current evidence.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599–606.
Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44.
Klag MJ, Whelton PK, Randall BL, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–8.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13.
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52.
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–9.
Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–60.
Dulin BR, Haas SJ, Abraham WT, Krum H. Do elderly systolic heart failure patients benefit from beta blockers to the same extent as the non-elderly? Meta-analysis of > 12,000 patients in large-scale clinical trials. Am J Cardiol. 2005;95(7):896–8.
•• Palatini P. Role of elevated heart rate in the development of cardiovascular disease in hypertension. Hypertension. 2011;58(5):745–50. This article provides a comprehensive review of the current literature regarding heart rate as a risk factor for cardiovascular disease in patients with hypertension.
Palatini P, Dorigatti F, Zaetta V, et al. Heart rate as a predictor of development of sustained hypertension in subjects screened for stage 1 hypertension: the HARVEST Study. J Hypertens. 2006;24(9):1873–80.
Morcet JF, Safar M, Thomas F, Guize L, Benetos A. Associations between heart rate and other risk factors in a large French population. J Hypertens. 1999;17(12 Pt 1):1671–6.
Carnethon MR, Golden SH, Folsom AR, Haskell W, Liao D. Prospective investigation of autonomic nervous system function and the development of type 2 diabetes: the atherosclerosis risk in communities study, 1987–1998. Circulation. 2003;107(17):2190–5.
• Julius S, Palatini P, Kjeldsen SE, et al. Usefulness of heart rate to predict cardiac events in treated patients with high-risk systemic hypertension. Am J Cardiol. 2012;109:685–92. A secondary analysis of the VALUE trial indicates that baseline and in-trial heart rate are risk factors for cardiovascular events and all-cause mortality. The findings are consistent in subjects with controlled and uncontrolled blood pressure.
King DE, Everett CJ, Mainous 3rd AG, Liszka HA. Long-term prognostic value of resting heart rate in subjects with prehypertension. Am J Hypertens. 2006;19(8):796–800.
Kavanagh-Gray D. Comparison of central aortic and peripheral artery pressure curves. Can Med Assoc J. 1964;90:1468–71.
Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27(21):2588–605.
•• Townsend RR, Wimmer NJ, Chirinos JA, et al. Aortic PWV in chronic kidney disease: a CRIC ancillary study. Am J Hypertens. 2010;23(3):282–9. In 2564 subjects in CRIC, increased aortic PWV was found to be associated with older age, elevated blood pressure, and lower eGFR.
Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37(5):1236–41.
Taal MW, Sigrist MK, Fakis A, Fluck RJ, McIntyre CW. Markers of arterial stiffness are risk factors for progression to end-stage renal disease among patients with chronic kidney disease stages 4 and 5. Nephron Clin Pract. 2007;107(4):c177–81.
Miyashita H. Clinical assessment of central blood pressure. Curr Hypertens Rev. 2012;8(2):80–90.
Cohen DL, Townsend RR. Central blood pressure and chronic kidney disease progression. Int J Nephrol. 2011;2011:407801.
London G, Guerin A, Pannier B, et al. Increased systolic pressure in chronic uremia. Role of arterial wave reflections. Hypertension. 1992;20(1):10–9.
Papaioannou TG, Vlachopoulos CV, Alexopoulos NA, et al. The effect of heart rate on wave reflections may be determined by the level of aortic stiffness: clinical and technical implications. Am J Hypertens. 2008;21(3):334–40.
Protogerou AD, Safar ME. Dissociation between central augmentation index and carotid-femoral pulse-wave velocity: when and why? Am J Hypertens. 2007;20(6):648–9.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, et al. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31(15):1865–71.
Roman MJ, Devereux RB, Kizer JR, et al. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension. 2007;50(1):197–203.
Yasmin, Brown MJ. Similarities and differences between augmentation index and pulse wave velocity in the assessment of arterial stiffness. QJM. 1999;92(10):595–600.
Wilkinson IB, Mohammad NH, Tyrrell S, et al. Heart rate dependency of pulse pressure amplification and arterial stiffness. Am J Hypertens. 2002;15(1 Pt 1):24–30.
Wilkinson IB, MacCallum H, Flint L, et al. The influence of heart rate on augmentation index and central arterial pressure in humans. J Physiol. 2000;525(Pt 1):263–70.
Lemogoum D, Flores G, Van den Abeele W, et al. Validity of pulse pressure and augmentation index as surrogate measures of arterial stiffness during beta-adrenergic stimulation. J Hypertens. 2004;22(3):511–7.
Chen CH, Ting CT, Lin SJ, et al. Different effects of fosinopril and atenolol on wave reflections in hypertensive patients. Hypertension. 1995;25(5):1034–41.
Morgan T, Lauri J, Bertram D, Anderson A. Effect of different antihypertensive drug classes on central aortic pressure. Am J Hypertens. 2004;17(2):118–23.
•• Boutouyrie P, Achouba A, Trunet P, Laurent S. Amlodipine-valsartan combination decreases central systolic blood pressure more effectively than the amlodipine-atenolol combination: the EXPLOR study. Hypertension. 2010;55(6):1314–22. Among patients already on amlodipine, a larger decrease in aortic systolic blood pressure, central pulse pressure, and augmentation index was observed with the addition of valsartan compared to atenolol. Brachial blood pressure reduction was similar in both arms.
Bangalore S, Wild D, Parkar S, et al. Beta-blockers for primary prevention of heart failure in patients with hypertension. Insights from a meta-analysis. J Am Coll Cardiol. 2008;52:1062–72.
• Shah NK, Smith SM, Nichols WW, et al. Carvedilol reduces aortic wave reflection and improves left ventricular/vascular coupling: a comparison with atenolol (CENTRAL Study). J Clin Hypertens (Greenwich). 2011;13(12):917–24. The authors demonstrated an increase in augmentation pressure and augmentation index in atenolol treated patients compared to those treated with carvedilol after 4 weeks of therapy. Reductions in central blood pressure and brachial pressures were similar in both groups.
•• Kampus P, Serg M, Kals J, et al. Differential effects of nebivolol and metoprolol on central aortic pressure and left ventricular wall thickness. Hypertension. 2011;57(6):1122–8. Randomized controlled trial of 80 patients comparing the vasodilating beta-blocker nebivolol to metoprolol. Both agents similarly reduced brachial blood pressure and heart rate; however reductions in central blood pressure and pulse pressure were seen in the nebivolol arm.
Mahmud A, Feely J. Beta-blockers reduce aortic stiffness in hypertension but nebivolol, not atenolol, reduces wave reflection. Am J Hypertens. 2008;21(6):663–7.
Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805–16.
Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356(9227):359–65.
Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan intervention for endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995–1003.
Medical Research Council trial of treatment of hypertension in older adults: principal results. MRC Working Party. BMJ. 1992;304(6824):405–12.
• Poulter NR, Dobson JE, Sever PS, et al. Baseline heart rate, antihypertensive treatment, and prevention of cardiovascular outcomes in ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial). J Am Coll Cardiol. 2009;54(13):1154–61. This large sub-study of the ASCOT trial analyzed the effect of heart rate in hypertensive patients without CVD. The authors compared amlodipine-based antihypertensive regimens to atenolol-based antihypertensive regimens and demonstrated a reduction in cardiovascular events in the amlodipine arms at all levels of heart rate.
Bangalore S, Sawhney S, Messerli FH. Relation of beta-blocker-induced heart rate lowering and cardioprotection in hypertension. J Am Coll Cardiol. 2008;52(18):1482–9.
Kalaitzidis R, Bakris G. Should nephrologists use beta-blockers? A perspective. Nephrol Dial Transplant. 2009;24(3):701–2.
Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–25.
• Williams B, Lacy PS. Impact of heart rate on central aortic pressures and hemodynamics: analysis from the CAFE (Conduit Artery Function Evaluation) study: CAFE-Heart Rate. J Am Coll Cardiol. 2009;54(8):705–13. Results of this study demonstrate an inverse relationship between heart rate and central aortic pressures, whereas lowering heart rate with treatment for hypertension resulted in elevated central aortic pressure.
Beddhu S, Nigwekar SU, Ma X, Greene T. Associations of resting heart rate with insulin resistance, cardiovascular events and mortality in chronic kidney disease. Nephrol Dial Transplant. 2009;24(8):2482–8.
Muntner P, Anderson A, Charleston J, et al. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2010;55(3):441–51.
Rahman M, Pressel S, Davis BR, et al. Cardiovascular outcomes in high-risk hypertensive patients stratified by baseline glomerular filtration rate. Ann Intern Med. 2006;144(3):172–80.
Townsend RR, Chirinos JA, Parsa A, et al. Central pulse pressure in chronic kidney disease: a chronic renal insufficiency cohort ancillary study. Hypertension. 2010;56(3):518–24.
Wright Jr JT, Bakris G, Greene T, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA. 2002;288(19):2421–31.
Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93(5):1043–65.
Brotman DJ, Bash LD, Qayyum R, et al. Heart rate variability predicts ESRD and CKD-related hospitalization. J Am Soc Nephrol. 2010;21(9):1560–70.
Burger AJ, D’Elia JA, Weinrauch LA, Lerman I, Gaur A. Marked abnormalities in heart rate variability are associated with progressive deterioration of renal function in type I diabetic patients with overt nephropathy. Int J Cardiol. 2002;86(2–3):281–7.
Dekker JM, Crow RS, Folsom AR, et al. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Atherosclerosis Risk In Communities. Circulation. 2000;102(11):1239–44.
Deligiannis A, Kouidi E, Tourkantonis A. Effects of physical training on heart rate variability in patients on hemodialysis. Am J Cardiol. 1999;84(2):197–202.
Malfatto G, Facchini M, Sala L, et al. Effects of cardiac rehabilitation and beta-blocker therapy on heart rate variability after first acute myocardial infarction. Am J Cardiol. 1998;81(7):834–40.
Lanza GA, Pitocco D, Navarese EP, et al. Association between cardiac autonomic dysfunction and inflammation in type 1 diabetic patients: effect of beta-blockade. Eur Heart J. 2007;28(7):814–20.
Fodor GJ, Kotrec M, Bacskai K, et al. Is interview a reliable method to verify the compliance with antihypertensive therapy? An international central-European study. J Hypertens. 2005;23(6):1261–6.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reule, S., Drawz, P.E. Heart Rate and Blood Pressure: Any Possible Implications for Management of Hypertension?. Curr Hypertens Rep 14, 478–484 (2012). https://doi.org/10.1007/s11906-012-0306-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-012-0306-3