Abstract
Purpose of Review
Highly effective, well-tolerated interferon-free direct-acting antivirals (DAA) have revolutionised hepatitis C virus (HCV) therapeutics, with the opportunity for broad treatment scale-up among marginalised or “high-risk” populations, including people who inject drugs (PWID) and people with HIV/HCV coinfection.
Recent Findings
Concern that HCV reinfection may compromise HCV treatment outcomes is sometimes cited as a reason for not offering treatment to current and former PWID. However, the incidence of reinfection following interferon-based treatment for chronic HCV is low among PWID. Reinfection rates in HIV-positive men-who-have-sex-with-men (MSM) are varied, with high incidence reported in some cohorts. Mathematical modelling suggests that substantial reductions in HCV incidence and prevalence could be achieved with targeted DAA therapy among those at the highest risk of ongoing transmission.
Summary
This review will summarise the recent literature on DAA efficacy in PWID and people with HIV/HCV coinfection, discuss the individual- and population-level impact of DAA treatment scale-up and reinfection, and highlight ongoing and future research questions in expanding HCV care and treatment to those populations at high risk of ongoing HCV transmission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Highly effective, well-tolerated interferon-free direct-acting antivirals (DAA) have revolutionised hepatitis C virus (HCV) therapeutics [1], with daily fixed-dose combination DAA regimens providing cure in greater than 95% of individuals with chronic infection [2,3,4]. The availability of DAA therapy has given rise to significant therapeutic optimism, providing an opportunity for broad treatment scale-up with the potential for HCV elimination among marginalised or “high-risk” populations, including people who inject drugs (PWID) and people with HIV/HCV coinfection [5,6,7,8].
One challenge in achieving HCV elimination is reinfection. There is concern that HCV reinfection may compromise HCV treatment outcomes in populations with ongoing risk behaviour, with the risk of reinfection cited as a reason for not offering treatment to PWID [9, 10]. However, the incidence of reinfection following interferon-based treatment for chronic HCV is low among lifetime PWID [11••, 12]. Reinfection rates in HIV-positive men-who-have-sex-with-men (MSM) are varied, with high incidence reported in some cohorts [13,14,15]. Mathematical modelling suggests that substantial reductions in HCV incidence and prevalence could be achieved with targeted DAA therapy among those at the highest risk of ongoing transmission [6, 16].
This review will summarise the recent literature on interferon-free DAA efficacy in PWID and people with HIV/HCV coinfection, discuss the individual- and population-level impact of DAA treatment scale-up and reinfection among PWID and HIV-positive MSM, and highlight ongoing and future research questions in expanding HCV care and treatment to those populations deemed at high risk of ongoing HCV transmission.
Who Is “High-Risk”? Defining the Population of Interest
When assessing suitability for interferon-based HCV therapy, certain populations, including PWID, people who are incarcerated, people with HIV/HCV coinfection, and MSM, had been considered “high-risk”, based on concerns regarding efficacy, toxicity, adherence, and particularly, the potential for reinfection [11••]. However, these populations are heterogeneous with different levels of reinfection risk attributable to specific subgroups.
Subpopulations of PWID include those who report injecting an illicit drug at least once (lifetime PWID), those who have ceased injecting drug use (former PWID), and those who continue to inject drugs (recent PWID, with definitions of “recent” varying between 1 and 12 months) [17]. Among lifetime PWID, there also exists a group of people receiving opioid substitution therapy (OST), some of whom may be recent PWID. Understanding the definitions for different PWID populations is crucial to accurately define outcomes and reinfection risk following DAA therapy.
Similarly, not all people with HIV/HCV coinfection demonstrate contemporary behaviours placing them at “high risk”. The higher HCV reinfection incidence reported in some studies among people with HIV/HCV coinfection, as compared to HCV mono-infection, has been driven by cohorts of acute HCV infection in HIV-positive MSM [11••]. Caution should be taken not to extrapolate these reinfection rates to general HIV/HCV coinfected populations. While similar risk behaviours are observed in HIV-positive and HIV-negative MSM [18], HCV incidence is significantly higher among HIV-positive MSM [19]. As DAA treatment scale-up occurs, a better understanding of drug use and sexual behaviours which pose a risk of reinfection is required.
DAA Efficacy Among People With HIV/HCV Coinfection and People Who Inject Drugs
Evidence From Clinical Trials
Phase II and III interferon-free DAA clinical trials have been undertaken in various populations, previously deemed “high-risk”, including PWID, people receiving OST, and people with HIV/HCV coinfection (Table 1). Overall efficacy and safety data have been similar to that seen in general populations.
HIV/HCV Coinfection
In contrast to results achieved with interferon-based therapy, HIV coinfection does not appear to compromise DAA efficacy. Phase III trials have demonstrated high sustained virological response at 12 weeks post-treatment (SVR12), equivalent to that observed in HCV mono-infection [3, 23, 24, 26, 27]. Following 12 weeks of interferon-free, ribavirin-free DAA therapy, SVR12 was achieved in greater than 95% of HIV/HCV coinfected participants receiving sofosbuvir/ledipasvir [3], sofosbuvir plus daclatasvir [23], grazoprevir/elbasvir [26], and sofosbuvir/velpatasvir [27].
However, the generalisability of these clinical trial results has been questioned, in large part due to the exclusion criteria pertaining to antiretroviral therapy, active drug use, CD4 T cell count, and detectable HIV RNA. Saeed et al. [33] reviewed phase III DAA clinical trial eligibility and compared this with the demographic, behavioural, and clinical characteristics of patients within the Canadian coinfection cohort (n = 874). They demonstrated that a minority (6–10%) of HIV/HCV coinfected patients would have been eligible for enrolment in the majority of HIV/HCV phase III trials, largely related to prescription of specific antiretroviral agents (drug–drug interactions) and active drug use. ALLY-2 [23], which assessed the efficacy and safety of sofosbuvir and daclatasvir, was the exception, with 43% of HIV/HCV coinfected patients potentially eligible for inclusion. Drug and alcohol use per se was not an exclusion criteria, with “active substance abuse” only regarded as exclusionary if the investigator deemed it “inappropriate”. The study by Saeed et al. [33] is important in highlighting the potential gap between clinical trial-based efficacy and “real-world” impact.
People Who Inject Drugs
Evidence from clinical trials with interferon-containing regimens indicated that recent drug use did not compromise HCV treatment outcomes [12]. Phase II and III trials of DAA therapy have demonstrated similar high efficacy among people receiving OST as compared with people not receiving OST [28,29,30,31]. However, in large part, these individuals have been stable on OST and people reporting recent drug use have been excluded, either by time since the last reported drug use or by urine drug screen.
A post hoc analysis of treatment efficacy and safety was performed among people who use drugs (PWUD) while receiving treatment in the ION-1 studies, in which participants with chronic HCV genotype 1 received sofosbuvir/ledipasvir (with or without ribavirin) for 8–24 weeks. As a positive urine drug test at screening was exclusionary, in order to assess drug use on treatment, stored samples were retrieved and tested retrospectively. Drug use during therapy was seen in 23% (n = 70), with the majority of positive samples detecting cannabinoids (19%). Use of opiates (1%), cocaine (1%), or amphetamine/methamphetamine (<1%) was demonstrated in a minority. High treatment efficacy and adherence were seen, regardless of on-treatment drug use (any drug use on-treatment: SVR12 97%, 68/70; no drug use on-treatment: SVR12 99%, 652/657).
In the C-EDGE COSTAR trial, the efficacy and safety of grazoprevir/elbasvir for 12 weeks in chronic HCV genotypes 1, 4, and 6 were assessed among people receiving OST (n = 301), the majority of whom had ongoing drug use during treatment and follow-up [32••]. Active drug use was assessed by regular urine drug screen; 58% had a positive urine drug screen at treatment initiation with stable patterns of drug use throughout treatment. At treatment initiation in the immediate treatment group, active use of benzodiazepines, opiates, cocaine, or amphetamines/methamphetamines was seen in 25, 22, 10, and 5%, respectively. Overall SVR12 was 92%, with similar treatment adherence and efficacy to the other C-EDGE phase III studies that excluded people with recent drug use [26, 34].
Evidence From “Real-World” Cohorts
Observational cohorts that have evaluated DAA regimens among broader populations in the “real world” have generally shown favourable treatment outcomes [35,36,37,38,39,40,41,42]. In the large US Veterans Affairs (VA) cohort [35], a high proportion of people with chronic HCV genotypes 1–4 achieved SVR (91%) following, predominately sofosbuvir-containing, DAA therapy initiated between January 2014 and June 2015. The VA cohort included individuals with a history of substance use disorder (37%), history of alcohol use disorder (44%), and HIV coinfection (4%). A history of “alcohol use disorder” did not impact SVR. HIV coinfection and history of substance use disorder were not included in the model.
The “real-world” efficacy of DAA therapy among people with HIV/HCV coinfection appears to be comparable to clinical trial efficacy [38,39,40,41, 43]. In a population traditionally designated difficult to treat, given poor outcomes with pegylated interferon and ribavirin (SVR ≤ 30%) [44, 45], high SVR12 (93%) was demonstrated among people with HIV/HCV coinfection and cirrhosis enrolled in the French National Agency for Research on AIDS and Viral Hepatitis (ANRS) CO13 HEPAVIH cohort [40]. Of 189 treated (75% male, 58% HCV genotype 1, 16% Child-Pugh class B or C), the vast majority received 24 weeks of sofosbuvir in combination with an NS5A inhibitor, daclatasvir (65%), or ledipasvir (12%), with or without ribavirin.
Similarly, high SVR has been reported in cohorts of PWUD. In a single-centre US cohort of PWUD (defined as people receiving OST, people reporting recent drug use, or people with a positive urine drug screen) treated with interferon-free DAA therapy, SVR12 was 96% (44/46), compared with 95% (41/43) in non-PWUD [46]. Most of the cohort reported recent drug use (65%) and receipt of OST (78%). In a small single-centre Austrian cohort of active PWID (n = 15), directly observed DAA therapy was initiated in concert with OST [47]. SVR12 was achieved in 100%, with excellent adherence (100%). While encouraging, further research is required to determine the feasibility and efficacy of DAA therapy in broader populations of recent PWID.
Reinfection Following HCV Treatment
There is concern that HCV reinfection may compromise the individual- and population-level benefits of HCV treatment in some populations [10]. In a recent meta-analysis, Simmons et al. [11••] examined the risk of HCV recurrence following interferon-based treatment-induced SVR in three different populations, defined by their perceived risk of reinfection—HCV mono-infected “low risk” (no recognised risk factors for reinfection), HCV mono-infected “high risk” (recognised risk factors for reinfection: former or recent injecting drug use, incarceration, MSM), and HIV/HCV coinfection. Reinfection incidence was 0.0 per 100 py (95% 0.0, 0.0) in those deemed “low risk”, 1.9 per 100 py (95% CI 1.1, 2.8) in those deemed “high risk”, and 3.2 per 100 py (95% CI 0.0, 12.3) in those with HIV/HCV coinfection. Regardless of risk category, reinfection incidence was low. However, it was unclear what proportion of those included in the “high-risk” group continued to demonstrate behaviours following SVR which posed a risk for HCV reinfection. Despite being included in the definition, no studies of MSM were included in the “high-risk” analysis. Also noteworthy, the higher reinfection incidence in the group with HIV/HCV coinfection was primarily driven by a single study of acute HCV infection in HIV-positive MSM [14].
A summary of primary studies and meta-analyses assessing HCV reinfection incidence following treatment in PWID and people with HIV/HCV coinfection is presented in Table 2, with the primary studies divided by duration of HCV infection. In general, HCV reinfection incidence in cohorts of acute or recent HCV infection is higher than that in cohorts of chronic HCV infection, presumably given contemporary risk behaviours for HCV transmission in acute HCV cohorts.
HCV Reinfection Among People Who Inject Drugs
The risk of reinfection is cited as a reason for not offering treatment to PWID [9]. However, the incidence of reinfection following interferon-based treatment for chronic HCV is generally low among people who have ever injected drugs (lifetime PWID, reinfection incidence 0–5 per 100 py) [11••, 12] (Table 2).
The risk of HCV reinfection is significantly higher in people treated for chronic HCV infection who report ongoing risk behaviour, with reinfection incidence in those reporting injecting drug use post-treatment ranging between 0.0 and 33.0 per 100 py [12, 49, 50, 56, 60, 62,63,64]. In a meta-analysis examining reinfection incidence among PWUD (recent and lifetime), overall reinfection incidence was 2.4 per 100 py (95% CI 0.9, 6.1), rising to 6.4 per 100 py (95% CI 2.5, 16.7) in those who reported injecting drug use post-SVR [12].
Several recent studies have demonstrated the impact of ongoing injecting drug use following treatment on reinfection incidence. Midgard et al. [49] followed “former” PWID for up to 7 years after successful treatment with pegylated interferon and ribavirin in Norway (n = 94). One of the inclusion criteria for initial study entry and interferon-based treatment was abstinence from injecting for more than 6 months; 39% reported injecting drug use during follow-up. In this cohort, 12 cases of reinfection were identified for an overall reinfection incidence of 2.0 per 100 py (95% CI 1.0, 3.5). Reinfection incidence rose to 5.8 per 100 py (95% CI 3.0, 10.2) among participants reporting injecting drug use post-treatment. Similarly, Weir et al. [50] examined reinfection incidence among lifetime PWID following SVR in Scotland (n = 277), with seven cases of reinfection identified and an overall reinfection incidence of 1.7 per 100 py (95% CI 0.7, 3.5). Among PWID who had been hospitalised for an opiate- or injection-related cause post-SVR (11%, n = 29), the risk of HCV reinfection was significantly higher (adjusted hazard ratio 12.9, 95% CI 2.2, 76.0, p = 0.002) with an increase in reinfection incidence to 5.7 per 100 py (95% CI 1.8, 13.3).
Evidence is being to emerge regarding reinfection following treatment with DAA therapy. In the C-EDGE COSTAR trial among people receiving OST, six cases of reinfection were identified at or prior to post-treatment week 24, with five cases of reinfection detected at post-treatment week 8. Reinfection incidence was 4.6 per 100 py (95% CI 1.7, 10.0) [32••]. Urine drug screen was positive both during and following treatment in five of the six cases. Of noted, reinfection cleared spontaneously in three of the six cases. Reinfection occurring soon after completion of treatment highlights that, in the era of interferon-free therapy, reinfection incidence will need to be calculated from end of treatment and sequencing used to accurately determine the aetiology of post-treatment HCV RNA recurrence to avoid misclassification. No cases of reinfection were identified up to 24 weeks post-treatment in the ION-1 or ASTRAL 1–3 trials [30, 31].
HCV Reinfection Among HIV-Positive MSM
An increase in HCV incidence and prevalence has been reported in HIV-positive MSM over the last decade [48•, 65], although the burden of disease remains significantly lower than among PWID. In the Swiss Cohort Study, HCV incidence increased 18-fold in MSM between 1998 and 2011, while it declined in PWID and remained <1 per 100 py in heterosexuals [66]. In a recent meta-analysis examining HCV incidence in HIV-positive MSM who denied ever injecting drugs, estimated annual HCV incidence rates rose from 0.4 per 100 py in 1991 (95% CI 0.2, 0.8) to 1.3 per 100 py in 2012 (95% CI 0.8, 2.4) [48•]. The increase in HCV incidence has been associated with a reported increase in sexual risk behaviour and recreational drug use [48•]. Risk factors for HCV acquisition in HIV-positive MSM include condomless traumatic anal intercourse, higher number of sexual partners, group sex, ulcerative sexually transmitted diseases, and sexual acts that involve trauma and bleeding [48•, 66,67,68,69,70,71]. However, HIV-positive MSM who inject drugs remain at significantly higher risk of HCV acquisition than HIV-positive MSM who do not inject drugs [65, 72].
Reinfection rates in HIV-positive MSM following primary HCV infection are varied, with high incidence reported in acute HCV cohorts [13,14,15] (Table 2). A meta-analysis examining reinfection HCV incidence among HIV-positive MSM who denied injecting drug use reported a reinfection incidence of 11.4 per 100 py (95% CI 7.4, 17.7) [48•], though results were pooled from only two retrospective acute HCV cohorts in Europe [13, 14]. Ingiliz et al. [15] analysed reinfection incidence in a large cohort of HIV-positive MSM in western Europe (n = 552), with 143 reinfections demonstrated over 1952 py of follow-up. Overall reinfection incidence was 7.3 per 100 py (95% CI 6.2, 8.6) with 25% reinfected at 3 years. Multiple reinfections were noted in some individuals (second reinfection, n = 69; third reinfection, n = 13) for a secondary reinfection incidence of 18.8 per 100 py (95% CI 12.9, 27.5). Importantly, the results combined two different populations at risk for reinfection, those with treatment-induced clearance and those with spontaneous clearance. Individuals with acute HCV infection and spontaneous clearance appear to be at higher risk of reinfection [73,74,75] than those with chronic HCV infection and treatment-induced SVR, indicative of different rates of ongoing risk behaviour [11••].
Reinfection has been documented in phase II and III DAA trials among people with HIV/HCV coinfection, in some cases prior to the primary endpoint of the study (SVR12). In TURQUOISE-I [24], two cases of reinfection were detected after the participants achieved SVR12; high-risk sexual behaviour was reported. In C-EDGE COINFECTION [26], two cases of reinfection were documented prior to SVR12; risk factors for reinfection were not reported.
Populations at high risk of reinfection, such as PWID and HIV-positive MSM, are not mutually exclusive. While often discussed as separate cohorts, it is important to remember that there is significant overlap [76]. Among a cohort of HIV/HCV coinfected individuals (of whom 86% reported ever injecting drugs), overall reinfection incidence was 1.2 per 100 py (95% CI 0.3, 3.1) [51]. Reinfection incidence in those individuals who used heroin and/or cocaine during follow-up was 8.7 per 100 py (95% CI 4.8, 23.7). In an Australian and New Zealand cohort of individuals treated for recent HCV infection (duration of HCV infection <18 months), ten cases of reinfection were identified in the population at risk (n = 120) [61]. Of the ten participants (seven HIV-positive MSM) with reinfection, eight reported injecting drug use during follow-up. The remaining two cases occurred in HIV-positive MSM who denied ever injecting drugs. Overall reinfection incidence was 7.4 per 100 py (95% CI 4.0, 13.8), rising to 15.5 per 100 py (95% CI 7.8, 31.1) in those who reported injecting drug use at end of or post-treatment. On adjusted analysis, reinfection was associated with injecting drug use during follow-up. Among PWID (including HIV-positive MSM), HCV reinfection was specifically associated with use of unsterile needles and syringes during follow-up. High reinfection incidence following treatment for HCV infection in individuals with ongoing high-risk behaviour emphasises the need for post-treatment surveillance, harm reduction strategies, and education.
Mathematical Modelling: Treatment-as-Prevention and the Impact of Reinfection
The burden of disease attributed to HCV is high among PWID and is increasing among HIV-infected MSM. Mathematical modelling suggests that substantial reductions in HCV incidence and prevalence could be achieved by targeted DAA treatment scale-up among those at the highest risk of ongoing transmission [6, 16, 77, 78]. Using HCV treatment uptake data from seven sites in the UK, Martin et al. demonstrated that treating 26 per 1000 HCV-infected PWID per annum with DAA therapy could achieve a 15–50% decrease in chronic HCV prevalence within 10 years [78]. Despite the high cost of DAA therapy, treating recent PWID and HIV-positive MSM with early liver disease appears to be cost-effective compared to delaying until cirrhosis, given the reduction in liver-related complications and additional benefit of averting secondary infections [7, 8, 79]. Modelling estimates support broad access to DAA therapy, without limitations based on disease stage or drug use, to gain the greatest individual- and population-level benefits.
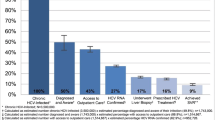
The potential for broad access to highly effective, well-tolerated interferon-free DAA regimens has stimulated discussion around HCV treatment-as-prevention (TasP). HCV treatment scale-up will have a population-level prevention benefit by reducing the size of the HCV viraemic reservoir. However, ongoing risk behaviour following successful HCV therapy will contribute to reinfection. As shown in Fig. 1, rapid scale-up of DAA therapy (>8% per year) among PWID markedly increases the aviraemic proportion and as such increases the proportion susceptible to HCV reinfection [80]. While initially this leads to an increase in the number of people with HCV reinfection, as the viraemic prevalence decreases overall, the number of people with reinfection also decreases. A slower scale-up of DAA therapy (≤4% per year) has more limited impact on the viraemic prevalence and reinfection.
Rate of HCV reinfection following HCV treatment scale-up assuming various rates of treatment uptake. Each line represents the expected number of individuals with HCV reinfection (left axis) in subsequent years based on an assumed annual treatment rate scenario. Permission to reproduce the image has been obtained from the author [80]
Ongoing risk behaviours associated with HCV transmission and high HCV reinfection rates may compromise the population-level benefits of TasP among recent PWID and HIV-positive MSM commencing DAA therapy. For PWID, access to interventions known to prevent HCV infection, including OST and high-coverage needle and syringe access programs [81,82,83,84,85], is crucial. Education regarding the potential for reinfection by health providers, peer-support workers, and community drug user organisations should be offered.
Using data from the UK Collaborative HIV Cohort (UK CHIC), mathematical modelling predicted that over the next decade, 94% of HCV infections in HIV-positive MSM would occur among high-risk individuals. As such, the greatest impact on HCV incidence and prevalence would be achieved if DAA treatment scale-up was prioritised to those with recently diagnosed (<1 year) HCV infection and occurred in combination with behavioural interventions [6]. Similarly, modelling within the Swiss HIV Cohort Study (SHCS) suggested that DAA treatment scale-up will need to occur in concert with behavioural risk reduction or stabilisation to achieve reductions in HCV incidence and prevalence [86]. Stabilisation of rates of high-risk behaviour combined with increased treatment uptake and the use of DAAs was predicted to reduce HCV incidence by 77% (from 2.2 per 100 py in 2015 to 0.5 per 100 py in 2030) and prevalence by 81% (from 4.8% in 2015 to 0.9% in 2030). However, most importantly, the model highlighted that a decrease in high-risk behaviour alone could rapidly reduce HCV incidence, independent of treatment uptake or efficacy. With serosorting of sexual partners by HIV status and increasing use of pre-exposure prophylaxis to prevent HIV transmission in HIV-negative MSM, there is the potential for increased sexual risk behaviour and transmission of HCV among MSM populations [71, 87, 88].
Prioritising treatment to those at risk of HCV transmission, including recent PWID and HIV-positive MSM engaging in high-risk behaviour, is consistent with international guidelines [89,90,91,92]. However, while there is evidence supporting interventions for HCV prevention among PWID [81,82,83,84,85], evidence supporting sexual behavioural interventions for HCV prevention among MSM is lacking. If reinfection does occur, retreatment should be made available.
Future Directions
To date, clinical trials have largely excluded those at the highest risk of ongoing transmission, including those with recent HCV infection, those reporting recent injecting drug use, and those who are incarcerated. Further evidence is required in these populations to assess DAA efficacy, long-term outcomes, and crucially, reinfection incidence. A 3-year post-treatment extension of the C-EDGE COSTAR study is underway, evaluating drug use behaviours and the incidence of HCV reinfection (NCT02105688).
Among recent PWID (defined as injecting drug use within 3 or 6 months of enrolment), ongoing clinical trials assessing the efficacy of sofosbuvir/velpatasvir include HERO (NCT02824640) and SIMPLIFY (NCT02336139). Among people receiving OST and reporting recent injecting drug use (defined as injecting drug use within 6 months of enrolment), D3FEAT (NCT02498015) is examining the efficacy of paritaprevir/ritonavir/ombitasvir and dasabuvir (with or without ribavirin). Among people who are incarcerated, large trials are being conducted in Australia (STOP-C; NCT02064049) and Spain (JAILFREE-C; NCT02768961). In those with recent HCV infection (duration of HCV infection 4–12 months), the efficacy and feasibility of short-duration (6–8 weeks) DAA therapy are being assessed (DAHHS-2, NCT02600325; REACT, NCT02625909; SWIFT-C, NCT02128217; TARGET3D, NCT02634008).
Among HIV-positive MSM in the Swiss Cohort Study, a comprehensive approach to HCV care involving the combination of treatment and behavioural intervention is being trialled (“The Swiss HCVfree trial”, NCT02785666). The treatment intervention includes grazoprevir/elbasvir for those with HCV GT 1 or 4 and the behavioural intervention involves targeted counselling about sexual risk behaviour and recreational drug use in participants reporting inconsistent condom use with casual male partners. All participants will receive “standard of care” (written and oral) information regarding the risk of HCV reinfection following successful treatment.
In an effort to expand access, different models of care are being assessed. In Scotland, a cluster randomised trial is assessing the impact of pharmacy-led directly observed HCV DAA therapy versus conventional nurse-led HCV therapy for people receiving OST (SuperDOT-C, NCT 02706223). In Melbourne, Australia, the TAP study (NCT02363517) is assessing a social network-based approach (“bring a friend”) to HCV treatment among PWID. In a multicentre randomised US study, the feasibility and acceptability of a patient-led model of care are being compared with directly observed therapy in active PWID (HERO; NCT02824640).
Conclusions
The treatment paradigm for individuals with HCV infection is evolving rapidly [2,3,4, 26]. High interferon-free DAA efficacy demonstrated in clinical trials appears to be translating into the “real world”, even among populations considered “high risk”.
The incidence of HCV reinfection following DAA-based treatment is unknown and needs careful evaluation as access to treatment among populations at risk of ongoing transmission increases. There is some uncertainty around current reinfection estimates following interferon-based therapy given small sample sizes, retrospective study designs, exclusion of recent PWID from clinical trials, varied definitions for recent injecting drug use and time at risk for reinfection, and the inability to accurately distinguish relapse from reinfection. Particularly in the setting of interferon-based therapy, there may have been considerable selection bias in those PWID deemed suitable, or willing, for treatment. While injecting risk behaviour among PWID appeared to decline during and after interferon-based treatment [93], it is possible that expanded HCV treatment access and DAA therapeutic optimism may be associated with increased risk behaviour, as seen among MSM following the introduction of HIV combination antiretroviral therapy [94].
With DAA treatment scale-up among traditionally marginalised or “high-risk” populations, implementation and evaluation of novel prevention strategies should be a priority. Populations at high risk of HCV transmission, such as PWID and HIV-positive MSM, are not mutually exclusive, with implications for public health strategies. Treatment should occur in concert with education and harm minimisation. Good-quality evidence supporting interventions for HIV and HCV prevention including needle and syringe access programs, OST, and supervised injection facilities exists [81,82,83,84,85]; broad implementation of these interventions is required. Similarly, education regarding high-risk sexual practices and behavioural risk reduction consistent with currently recommended HIV prevention strategies is warranted, although evidence supporting the success of these strategies in limiting HCV transmission is lacking [95]. Screening protocols for acute HCV in PWID and HIV-positive MSM should be employed to enhance early HCV diagnosis, linkage to care, and access to treatment [89,90,91,92]. Future research should evaluate the incidence of reinfection following DAA therapy and the feasibility of HCV prevention and retreatment strategies.
Ultimately, the population-level impact of DAA therapy will relate to facilitating global access to HCV screening, care, and treatment. Overcoming barriers imposed by high drug pricing, drug use, and liver disease stage restrictions and stigma will be central to this [96]. The risk of HCV reinfection following treatment in individuals with ongoing risk behaviour emphasises the need for post-treatment surveillance, harm reduction strategies, and education, but must not be considered an impediment to treatment, if HCV elimination is to be achieved.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dore GJ, Feld JJ. Hepatitis C virus therapeutic development: in pursuit of “perfectovir”. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2015;60(12):1829–36.
Feld JJ, Jacobson IM, Hezode C, Asselah T, Ruane PJ, Gruener N, et al. Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N Engl J Med. 2015;373(27):2599–607.
Naggie S, Cooper C, Saag M, Workowski K, Ruane P, Towner WJ, et al. Ledipasvir and sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med. 2015;373(8):705–13.
Gane EJ, Schwabe C, Hyland RH, Yang Y, Svarovskaia E, Stamm LM, et al. Efficacy of the combination of sofosbuvir, velpatasvir, and the NS3/4A protease inhibitor GS-9857 in treatment-naive or previously treated patients with hepatitis C virus genotype 1 or 3 infections. Gastroenterology. 2016;
Cousien A, Tran VC, Deuffic-Burban S, Jauffret-Roustide M, Dhersin JS, Yazdanpanah Y. Hepatitis C treatment as prevention of viral transmission and liver-related morbidity in persons who inject drugs. Hepatology. 2016;63(4):1090–101.
Martin NK, Thornton A, Hickman M, Sabin C, Nelson M, Cooke GS, et al. Can hepatitis C virus (HCV) direct-acting antiviral treatment as prevention reverse the HCV epidemic among men who have sex with men in the United Kingdom? Epidemiological and modeling insights. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62(9):1072–80.
Martin NK, Vickerman P, Dore GJ, Grebely J, Miners A, Cairns J, et al. Prioritization of HCV treatment in the direct-acting antiviral era: an economic evaluation. J Hepatol. 2016;65(1):17–25.
Scott N, McBryde ES, Thompson A, Doyle JS, Hellard ME. Treatment scale-up to achieve global HCV incidence and mortality elimination targets: a cost-effectiveness model. Gut. 2016;
Asher AK, Portillo CJ, Cooper BA, Dawson-Rose C, Vlahov D, Page KA. Clinicians’ views of hepatitis C virus treatment candidacy with direct-acting antiviral regimens for people who inject drugs. Substance use & misuse. 2016;51(9):1218–23.
Cunningham EB, Applegate TL, Lloyd AR, Dore GJ, Grebely J. Mixed HCV infection and reinfection in people who inject drugs—impact on therapy. Nat Rev Gastroenterol Hepatol. 2015;12(4):218–30.
•• Simmons B, Saleem J, Hill A, Riley RD, Cooke GS. Risk of late relapse or reinfection with hepatitis C virus after achieving a sustained virological response: a systematic review and meta-analysis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62(6):683–94. Meta-analysis of HCV recurrence, both late relapse and reinfection, following treatment-induced SVR in three different populations, defined by their risk of reinfection.
Aspinall EJ, Corson S, Doyle JS, Grebely J, Hutchinson SJ, Dore GJ, et al. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2013;57(Suppl 2):S80–9.
Lambers FA, Prins M, Thomas X, Molenkamp R, Kwa D, Brinkman K, et al. Alarming incidence of hepatitis C virus re-infection after treatment of sexually acquired acute hepatitis C virus infection in HIV-infected MSM. AIDS (London, England). 2011;25(17):F21–7.
Martin TC, Martin NK, Hickman M, Vickerman P, Page EE, Everett R, et al. Hepatitis C virus reinfection incidence and treatment outcome among HIV-positive MSM. AIDS. 2013;27(16):2551–7.
Ingiliz P, Martin TC, Rodger A, Stellbrink HJ, Mauss S, Boesecke C, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in western Europe. J Hepatol. 2016;
Martin NK, Hickman M, Hutchinson SJ, Goldberg DJ, Vickerman P. Combination interventions to prevent HCV transmission among people who inject drugs: modeling the impact of antiviral treatment, needle and syringe programs, and opiate substitution therapy. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2013;57(Suppl 2):S39–45.
Larney S, Grebely J, Hickman M, De Angelis D, Dore GJ, Degenhardt L. Defining populations and injecting parameters among people who inject drugs: implications for the assessment of hepatitis C treatment programs. The International journal on drug policy. 2015;26(10):950–7.
Ward C, Lee V. Experience of acute hepatitis C and HIV co-infection in an inner city clinic in the UK. J Int AIDS Soc. 2014;17(4 Suppl 3):19639.
Yaphe S, Bozinoff N, Kyle R, Shivkumar S, Pai NP, Klein M. Incidence of acute hepatitis C virus infection among men who have sex with men with and without HIV infection: a systematic review. Sex Transm Infect. 2012;88(7):558–64.
Sulkowski MS, Naggie S, Lalezari J, Fessel WJ, Mounzer K, Shuhart M, et al. Sofosbuvir and ribavirin for hepatitis C in patients with HIV coinfection. JAMA: the Journal of the American Medical Association. 2014;312(4):353–61.
Molina JM, Orkin C, Iser DM, Zamora FX, Nelson M, Stephan C, et al. Sofosbuvir plus ribavirin for treatment of hepatitis C virus in patients co-infected with HIV (PHOTON-2): a multicentre, open-label, non-randomised, phase 3 study. Lancet. 2015;385(9973):1098–106.
Osinusi A, Townsend K, Kohli A, Nelson A, Seamon C, Meissner EG, et al. Virologic response following combined ledipasvir and sofosbuvir administration in patients with HCV genotype 1 and HIV co-infection. JAMA: the journal of the American Medical Association. 2015;313(12):1232–9.
Wyles DL, Ruane PJ, Sulkowski MS, Dieterich D, Luetkemeyer A, Morgan TR, et al. Daclatasvir plus sofosbuvir for HCV in patients coinfected with HIV-1. N Engl J Med. 2015;373(8):714–25.
Sulkowski MS, Eron JJ, Wyles D, Trinh R, Lalezari J, Wang C, et al. Ombitasvir, paritaprevir co-dosed with ritonavir, dasabuvir, and ribavirin for hepatitis C in patients co-infected with HIV-1: a randomized trial. JAMA: the journal of the American Medical Association. 2015;313(12):1223–31.
Sulkowski M, Hezode C, Gerstoft J, Vierling JM, Mallolas J, Pol S, et al. Efficacy and safety of 8 weeks versus 12 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin in patients with hepatitis C virus genotype 1 mono-infection and HIV/hepatitis C virus co-infection (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385(9973):1087–97.
Rockstroh JK, Nelson M, Katlama C, Lalezari J, Mallolas J, Bloch M, et al. Efficacy and safety of grazoprevir (MK-5172) and elbasvir (MK-8742) in patients with hepatitis C virus and HIV co-infection (C-EDGE CO-INFECTION): a non-randomised, open-label trial. The lancet HIV. 2015;2(8):e319–27.
Wyles D, Brau N, Kottilil S, Daar ES, Ruane P, Workowski K, Luetkemeyer A, et al. Sofosbuvir and Velpatasvir for the Treatment of HCV in Patients Coinfected with HIV-1: an Open-Label, Phase 3 Study. Clin Infect Dis 2017.
Puoti M, Cooper C, Sulkowski MS, Foster GR, Berg T, Villa E, et al. ABT-450/r/ombitasvir plus dasabuvir with or without ribavirin in HCV genotype 1-infected patients receiving stable opioid substitution treatment: pooled analysis of efficacy and safety in phase 2 and phase 3 trials. Hepatology. 2014;60:1135a–6a.
Lalezari J, Sullivan JG, Varunok P, Galen E, Kowdley KV, Rustgi V, et al. Ombitasvir/paritaprevir/r and dasabuvir plus ribavirin in HCV genotype 1-infected patients on methadone or buprenorphine. J Hepatol. 2015;63(2):364–9.
Grebely J, Mauss S, Brown A, Bronowicki JP, Puoti M, Wyles D, et al. Efficacy and safety of ledipasvir/sofosbuvir with and without ribavirin in patients with chronic HCV genotype 1 infection receiving opioid substitution therapy: analysis of phase 3 ION trials. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;
Grebely J, Dore GJ, Zeuzem S, Aspinall RJ, Fox R, Han L, et al. Efficacy and safety of sofosbuvir/velpatasvir in patients with chronic hepatitis C virus infection receiving opioid substitution therapy: analysis of phase 3 ASTRAL trials. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;
•• Dore GJ, Altice F, Litwin AH, Dalgard O, Gane EJ, Shibolet O, et al. Elbasvir–grazoprevir to treat hepatitis C virus infection in persons receiving opioid agonist therapy. Annals of internal medicine. 2016. Phase III trial of elbasvir/grazoprevir in people receiving opioid agonist therapy, the majority of whom had evidence of ongoing drug use. High adherence, efficacy, and safety demonstrated regardless of on-treatment drug use.
Saeed S, Strumpf EC, Walmsley SL, Rollet-Kurhajec K, Pick N, Martel-Laferriere V, et al. How generalizable are the results from trials of direct antiviral agents to people coinfected with HIV/HCV in the real world? Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62(7):919–26.
Zeuzem S, Ghalib R, Reddy KR, Pockros PJ, Ben Ari Z, Zhao Y, et al. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 infection: a randomized trial. Ann Intern Med. 2015;163(1):1–13.
Ioannou GN, Beste LA, Chang MF, Green PK, Lowey E, Tsui JI, et al. Effectiveness of sofosbuvir, ledipasvir/sofosbuvir, or paritaprevir/ritonavir/ombitasvir and dasabuvir regimens for treatment of patients with hepatitis C in the Veterans Affairs National Health Care System. Gastroenterology. 2016.
Afdhal NH, Bacon B, Dieterich D, Flamm SL, Kowdley KV, Lee Y, et al. Failure with all-oral DAA regimens: real-world experience from the TRIO network [LB-17]. San Francisco: AASLD The Liver Meeting; 2015.
Sulkowski MS, Vargas HE, Di Bisceglie AM, Kuo A, Reddy KR, Lim JK, et al. Effectiveness of simeprevir plus sofosbuvir, with or without ribavirin, in real-world patients with HCV genotype 1 infection. Gastroenterology. 2016;150(2):419–29.
Christensen S, Mauss S, Hueppe D, Schewe K, Lutz T, Rockstroh JK, et al. Sofosbuvir and ledipasvir for eight weeks (SL8) in patients with hepatitis C virus (HCV) non-infection and human immunodeficiency virus (HIV)-HCV co-infection with genotype (GT)1 and 4 in clinical practice—results from the German hepatitis C cohort (GECCO) [ABSTRACT 1081]. Hepatology. 2015;62(1 (suppl)):740A.
Hawkins C, Grant J, Ammerman LR, Palella F, McLaughlin M, Green R. et al. High rates of hepatitis C virus (HCV) cure using direct-acting antivirals in HIV/HCV-coinfected patients: a real-world perspective. J Antimicrob Chemother. 2016;
Sogni P, Gilbert C, Lacombe K, Piroth L, Rosenthal E, Miailhes P, et al. All-oral direct-acting antiviral regimens in HIV/hepatitis C virus-coinfected patients with cirrhosis are efficient and safe: real-life results from the prospective ANRS CO13-HEPAVIH cohort. Clin Infect Dis Off Publ Infect Dis Soc Am. 2016;
Milazzo L, Lai A, Calvi E, Ronzi P, Micheli V, Binda F, et al. Direct-acting antivirals in hepatitis C virus (HCV)-infected and HCV/HIV-coinfected patients: real-life safety and efficacy. HIV Med. 2016;
Afdhal NH, Serfaty L. Cohort studies and registries in the treatment of hepatitis C virus: the impact of real-life effectiveness. Gastroenterology. 2016;
Del Bello D, Cha A, Sorbera M, Bichoupan K, Levine C, Doyle E, et al. Real-world sustained virologic response rates of sofosbuvir-containing regimens in patients coinfected with hepatitis C and HIV. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2016;62(12):1497–504.
Monje-Agudo P, Castro-Iglesias A, Rivero-Juárez A, Martínez-Marcos F, Ortega-González E, Real LM, et al. Impact of HIV infection on sustained virological response to treatment against hepatitis C virus with pegylated interferon plus ribavirin. Eur J Clin Microbiol Infect Dis. 2015;34(10):1929–36.
Carrat F, Bani-Sadr F, Pol S, Rosenthal E, Lunel-Fabiani F, Benzekri A, et al. Pegylated interferon alfa-2b vs standard interferon alfa-2b, plus ribavirin, for chronic hepatitis C in HIV-infected patients: a randomized controlled trial. JAMA: the journal of the American Medical Association. 2004;292(23):2839–48.
Norton BL, Fleming J, Steinman M, Yu K, Deluca J, Cunningham CO, et al. High HCV cure rates for drug users treated with DAAs at an urban primary care clinic conference on retroviruses and opportunisitic infections. Boston; 2016.
Schitz A, Moser S, Marchart K, Haltmayer H, Gschwantler M. Direct observed therapy of chronic hepatitis C with interferon-free all-oral regimens at a low-threshold drug treatment facility—a new concept for treatment of patients with borderline compliance receiving opioid substitution therapy. Am J Gastroenterol. 2016;111(6):903–5.
• Hagan H, Jordan AE, Neurer J, Cleland CM. Incidence of sexually transmitted hepatitis C virus infection in HIV-positive men who have sex with men. AIDS (London, England). 2015;29(17):2335–45. Meta-analysis of HCV incidence and reinfection in HIV-positive MSM who deny lifetime injecting drug use. Demonstrates high reinfection incidence in this population, but analysis pooled from only 2 retrospective acute HCV cohorts.
Midgard H, Bjoro B, Maeland A, Konopski Z, Kileng H, Damas JK, et al. Hepatitis C reinfection after sustained virological response. J Hepatol. 2016;64(5):1020–6.
Weir A, McLeod A, Innes H, Valerio H, Aspinall EJ, Goldberg DJ, et al. Hepatitis C reinfection following treatment induced viral clearance among people who have injected drugs. Drug Alcohol Depend. 2016;165:53–60.
Pineda JA, Nunez-Torres R, Tellez F, Mancebo M, Garcia F, Merchante N, et al. Hepatitis C virus reinfection after sustained virological response in HIV-infected patients with chronic hepatitis C. The Journal of infection. 2015;71(5):571–7.
Conway B, Wang J, Wong L, Alenezi O, Tossonian H. HCV reinfection in high-risk illicit drug users. Vancouver: 3rd International Symposium on Hepatitis Care in Substance Users; 2013.
Deshaies L. Treatment of hepatitis C in active intravenous drug users (IDUS): re-infection rate in TACTIC cohort. Suchtmed. 2013;15(4):262–3.
Edlin BR, Carden MR, Getter EV, Talal AH, Aden B, Goli S, et al. Hepatitis C treatment in active injection drug users [ABSTRACT]. Hepatology. 2013;58(S1):1091A–168A.
Hilsden RJ, Macphail G, Grebely J, Conway B, Lee SS. Directly observed pegylated interferon plus self-administered ribavirin for the treatment of hepatitis C virus infection in people actively using drugs: a randomized controlled trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2013;57(Suppl 2):S90–6.
Marco A, Esteban JI, Sole C, da Silva A, Ortiz J, Roget M, et al. Hepatitis C virus reinfection among prisoners with sustained virological response after treatment for chronic hepatitis C. J Hepatol. 2013;59(1):45–51.
Ruzić M, Fabri M, Preveden T, Kiralj K, Mikić S, Vukadinov T. Treatment of chronic hepatitis C in injecting drug users—a 5-year follow-up. Vojnosanit Pregl. 2013;70(8):723–7.
Grady BP, Vanhommerig JW, Schinkel J, Weegink CJ, Bruisten SM, Lindenburg CE, et al. Low incidence of reinfection with the hepatitis C virus following treatment in active drug users in Amsterdam. Eur J Gastroenterol Hepatol. 2012;24(11):1302–7.
Manolakopoulos S, Kranidioti H, Karatapanis S, Tsirogianni E, Goulis J, Deutsch M, et al. Hepatitis C virus reinfection following sustained virological response in intravenous drug users [ABSTRACT]. J Hepatol. 2012;56:S532.
Grebely J, Pham ST, Matthews GV, Petoumenos K, Bull RA, Yeung B, et al. Hepatitis C virus reinfection and superinfection among treated and untreated participants with recent infection. Hepatology. 2012;55(4):1058–69.
Martinello M, Grebely J, Petoumenos K, Gane E, Hellard M, Shaw D, Sasadeusz J, et al. HCV reinfection incidence among individuals treated for recent infection. J Viral Hepat 2016. doi:10.1111/jvh.12666.
Backmund M, Meyer K, Edlin BR. Infrequent reinfection after successful treatment for hepatitis C virus infection in injection drug users. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2004;39(10):1540–3.
Grebely J, Knight E, Ngai T, Genoway KA, Raffa JD, Storms M, et al. Reinfection with hepatitis C virus following sustained virological response in injection drug users. J Gastroenterol Hepatol. 2010;25(7):1281–4.
Currie SL, Ryan JC, Tracy D, Wright TL, George S, McQuaid R, et al. A prospective study to examine persistent HCV reinfection in injection drug users who have previously cleared the virus. Drug Alcohol Depend. 2008;93(1–2):148–54.
Jordan AE, Perlman DC, Neurer J, Smith DJ, Des Jarlais DC, Hagan H. Prevalence of hepatitis C virus infection among HIV+ men who have sex with men: a systematic review and meta-analysis. International journal of STD & AIDS. 2016. Meta-analysis of HCV incidence and reinfection in HIV-positive MSM who deny lifetime injecting drug use. Demonstrates high reinfection incidence in this population, but analysis pooled from only two retrospective acute HCV cohorts.
Wandeler G, Gsponer T, Bregenzer A, Gunthard HF, Clerc O, Calmy A, et al. Hepatitis C virus infections in the Swiss HIV cohort study: a rapidly evolving epidemic. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2012;55(10):1408–16.
Danta M, Brown D, Bhagani S, Pybus OG, Sabin CA, Nelson M, et al. Recent epidemic of acute hepatitis C virus in HIV-positive men who have sex with men linked to high-risk sexual behaviours. AIDS (London, England). 2007;21(8):983–91.
Gambotti L, Batisse D, Colin-de-Verdiere N, Delaroque-Astagneau E, Desenclos JC, Dominguez S, et al. Acute hepatitis C infection in HIV positive men who have sex with men in Paris, France, 2001-2004. Euro surveillance: bulletin Europeen sur les maladies transmissibles. European communicable disease bulletin. 2005;10(5):115–7.
Hasse B, Ledergerber B, Hirschel B, Vernazza P, Glass TR, Jeannin A, et al. Frequency and determinants of unprotected sex among HIV-infected persons: the Swiss HIV cohort study. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2010;51(11):1314–22.
Breskin A, Drobnik A, Pathela P, Chan C, Braunstein S, Bornschlegel K, et al. Factors associated with hepatitis C infection among HIV-infected men who have sex with men with no reported injection drug use in New York City, 2000-2010. Sex Transm Dis. 2015;42(7):382–6.
Apers L, Vanden Berghe W, De Wit S, Kabeya K, Callens S, Buyze J, et al. Risk factors for HCV acquisition among HIV-positive MSM in Belgium. J Acquir Immune Defic Syndr. 2015;68(5):585–93.
Gamage DG, Read TR, Bradshaw CS, Hocking JS, Howley K, Chen MY, et al. Incidence of hepatitis-C among HIV infected men who have sex with men (MSM) attending a sexual health service: a cohort study. BMC Infect Dis. 2011;11:39.
Sacks-Davis R, Aitken CK, Higgs P, Spelman T, Pedrana AE, Bowden S, et al. High rates of hepatitis C virus reinfection and spontaneous clearance of reinfection in people who inject drugs: a prospective cohort study. PLoS One. 2013;8(11):e80216.
Page K, Hahn JA, Evans J, Shiboski S, Lum P, Delwart E, et al. Acute hepatitis C virus infection in young adult injection drug users: a prospective study of incident infection, resolution, and reinfection. The Journal of infectious diseases. 2009;200(8):1216–26.
McDonald SA, Hutchinson SJ, Cameron SO, Innes HA, McLeod A, Goldberg DJ. Examination of the risk of reinfection with hepatitis C among injecting drug users who have been tested in Glasgow. The International journal on drug policy. 2012;23(5):353–7.
Matthews GV, Pham ST, Hellard M, Grebely J, Zhang L, Oon A, et al. Patterns and characteristics of hepatitis C transmission clusters among HIV-positive and HIV-negative individuals in the Australian trial in acute hepatitis C. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2011;52(6):803–11.
Hickman M, De Angelis D, Vickerman P, Hutchinson S, Martin NK. Hepatitis C virus treatment as prevention in people who inject drugs: testing the evidence. Curr Opin Infect Dis. 2015;28(6):576–82.
Martin NK, Foster GR, Vilar J, Ryder S, Cramp ME, Gordon F, et al. HCV treatment rates and sustained viral response among people who inject drugs in seven UK sites: real world results and modelling of treatment impact. J Viral Hepat. 2015;22(4):399–408.
Zahnd C, Salazar-Vizcaya L, Dufour JF, Mullhaupt B, Wandeler G, Kouyos R, et al. Modelling the impact of deferring HCV treatment on liver-related complications in HIV coinfected men who have sex with men. J Hepatol. 2016;65(1):26–32.
Razavi H. Reducing a country’s HCV-disease burden. Sydney: The 4th International Symposium on Hepatitis in Substance Users (INHSU 2015); 2015.
White B, Dore GJ, Lloyd AR, Rawlinson WD, Maher L. Opioid substitution therapy protects against hepatitis C virus acquisition in people who inject drugs: the HITS-c study. Med J Aust. 2014;201(6):326–9.
Nolan S, Dias Lima V, Fairbairn N, Kerr T, Montaner J, Grebely J, et al. The impact of methadone maintenance therapy on hepatitis C incidence among illicit drug users. Addiction. 2014;109(12):2053–9.
Tsui JI, Evans JL, Lum PJ, Hahn JA, Page K. Association of opioid agonist therapy with lower incidence of hepatitis C virus infection in young adult injection drug users. JAMA Intern Med. 2014;174(12):1974–81.
Turner KM, Hutchinson S, Vickerman P, Hope V, Craine N, Palmateer N, et al. The impact of needle and syringe provision and opiate substitution therapy on the incidence of hepatitis C virus in injecting drug users: pooling of UK evidence. Addiction. 2011;106(11):1978–88.
Coffin PO, Rowe C, Santos GM. Novel interventions to prevent HIV and HCV among persons who inject drugs. Curr HIV/AIDS Rep. 2015;12(1):145–63.
Salazar-Vizcaya L, Kouyos RD, Zahnd C, Wandeler G, Battegay M, Darling KE, et al. Hepatitis C virus transmission among HIV-infected men who have sex with men: modeling the effect of behavioral and treatment interventions. Hepatology. 2016;
Golub SA, Kowalczyk W, Weinberger CL, Parsons JT. Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J Acquir Immune Defic Syndr. 2010;54(5):548–55.
McFaul K, Maghlaoui A, Nzuruba M, Farnworth S, Foxton M, Anderson M, et al. Acute hepatitis C infection in HIV-negative men who have sex with men. J Viral Hepat. 2015;22(6):535–8.
AASLD/IDSA. Recommendations for testing, managing, and treating hepatitis C. Available from: www.hcvguidelines.org. 2015.
European Association for Study of L. EASL recommendations on treatment of hepatitis C 2015. J Hepatol. 2015;63(1):199–236.
Grebely J, Robaeys G, Bruggmann P, Aghemo A, Backmund M, Bruneau J, et al. Recommendations for the management of hepatitis C virus infection among people who inject drugs. The International journal on drug policy. 2015;26(10):1028–38.
WHO. Guidelines for the screening, care and treatment of persons with hepatitis C infection. Geneva, Switzerland; 2014.
Alavi M, Spelman T, Matthews GV, Haber PS, Day C, van Beek I, et al. Injecting risk behaviours following treatment for hepatitis C virus infection among people who inject drugs: the Australian trial in acute hepatitis C. The International journal on drug policy. 2015;26(10):976–83.
Dukers NH, Goudsmit J, de Wit JB, Prins M, Weverling GJ, Coutinho RA. Sexual risk behaviour relates to the virological and immunological improvements during highly active antiretroviral therapy in HIV-1 infection. AIDS (London, England). 2001;15(3):369–78.
Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. The Cochrane database of systematic reviews. 2008;3:CD001230.
Barua S, Greenwald R, Grebely J, Dore GJ, Swan T, Taylor LE. Restrictions for Medicaid reimbursement of sofosbuvir for the treatment of hepatitis C virus infection in the United States. Ann Intern Med. 2015;163(3):215–23.
Acknowledgements
The Kirby Institute is funded by the Australian Government Department of Health and Ageing. The views expressed in this publication do not necessarily represent the position of the Australian Government. The content is solely the responsibility of the authors. None of the authors has commercial relationships that might pose a conflict of interest in connection with this manuscript. Behzad Hajarizadeh is supported through NHMRC Early Career Fellowship. Jason Grebely and Gail Matthews are supported through NHMRC Career Development Fellowships. Gregory Dore is supported through NHMRC Practitioner Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Marianne Martinello has received speaker payments from Abbvie.
Behzad Hajarizadeh declared no conflicts of interest.
Jason Grebely is a consultant for and has received research grants from Abbvie, Bristol-Myers Squibb, Gilead Sciences Inc., and Merck.
Gregory J. Dore is an advisory board member and has received honoraria from Roche, Merck, Janssen, Gilead, Bristol-Myers Squibb, and Abbvie; has received research grant funding from Roche, Merck, Janssen, Gilead, Bristol-Myers Squibb, Vertex, Boeringher Ingelheim, and Abbvie; and travel sponsorship from Roche, Merck, Janssen, Gilead, and Bristol-Myers Squibb.
Gail V. Matthews has received research funding, advisory board payments, and speaker payments from Gilead; and research funding and speaker payments from Janssen.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Co-infections and Comorbidity
Rights and permissions
About this article
Cite this article
Martinello, M., Hajarizadeh, B., Grebely, J. et al. HCV Cure and Reinfection Among People With HIV/HCV Coinfection and People Who Inject Drugs. Curr HIV/AIDS Rep 14, 110–121 (2017). https://doi.org/10.1007/s11904-017-0358-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-017-0358-8