Abstract
A critical factor for understanding negative health outcomes is acknowledging the synergistic quality that clusters of health problems create. An important step in addressing clusters of health problems involves gaining an awareness of the contextual factors that connect them. This paper considers the intersection of 3 mutually reinforcing health problems: alcohol use, interpersonal violence (IPV), and HIV infection among pregnant women residing in South Africa. We explore how SAVA (substance abuse, violence and AIDS) - a syndemics related theory - underscores the dire need to intervene in various areas of psycho-social health and general well-being. Based on World Health Organization data, we highlight the remarkably high rates of alcohol use, IPV, and HIV infection among South African women compared with women residing in other countries around the world. We conclude by highlighting the need for improved recognition of the intersection of these epidemics and for improved surveillance of the prevalence of alcohol use among pregnant women. Finally, based on the literature reviewed, we provide recommendations for future interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction - The Impact of Intersecting Risks
The co-occurrence of risk factors is a topic of study across multiple fields in public health. We have long recognized patterns of co-occurring mental health diagnoses (particularly depression, anxiety, and substance use) and patterns of co-occurring medical diagnoses as age increases (eg, cardiovascular disease and hypertension). Furthermore, research has highlighted the interplay between clusters of both mental health and physical health diagnoses. Patients coming to terms with a diagnosis of a chronic illness like HIV, for example, face an increased risk of depression [1•, 2]. Moreover, individuals struggling with depression are more likely to self-medicate through substance use, including alcohol consumption, and are more likely to engage in other risk taking behavior [3]. This additive effect of negative health statuses may be further complicated by a sociocultural context that supports potentially harmful behaviors. For example, there is evidence that individuals residing in communities with elevated rates of substance use, and increased poverty and assault rates are more likely to experience multiple negative health outcomes compared with relatively safer communities [4, 5]. In short, the negative health outcomes an individual may face are complex as they often result from a chain of events situated in environments that foster such outcomes.
The recognition that the accumulation of physical and mental illnesses is more than just additive, ie, that the total burden of illness is greater than the sum of each negative health outcome, is referred to in the public health literature as a syndemic. The term syndemic was introduced by Singer [6] to address the relationships between health problems and the contextual (ie, social, political, historical, and environmental) influences that shape them [7]. One of the key goals in considering syndemics is understanding how the intersections of health problems unfold and, ultimately, affect general well-being. Syndemics occur in populations situated in particular locations, anchored in specific moments in time; hence, the recognition and prevention of syndemics requires an awareness of the contextual factors that connect each disease outcome [8].
This paper considers the intersection of 3 epidemics: Alcohol use, interpersonal violence (IPV), and HIV infection. In particular, we focus on how these epidemics intersect among pregnant women in South Africa. We chose to concentrate on these epidemics among these women as rates of alcohol use, IPV, and HIV among South Africa women are, on the whole, among the highest rates in the world. Furthermore, rates of fetal alcohol syndrome (FAS) among South African children are also among the highest in the world. And finally, the presence of these epidemics is consistent with the synergy of disease, social context, and behavioral patterns that Singer [6] initially presented as forming a syndemic; one which he refers to as SAVA – Substance Abuse, Violence, and AIDS. A recent review of the SAVA syndemic in American samples confirms that the impact of substance use and IPV are synergistic -- in particular, among studies focused on women, the SAVA syndemic emerges as a stable pattern: there are powerful relationships between substance use, the impact of IPV, poor decision making, and risk taking behavior [9•].
There is great need for context-sensitive interventions, particularly for the world’s most vulnerable populations. The development of context-sensitive interventions for pregnant women is urgently needed to improve not only the health of pregnant women but to create environments most advantageous for their infants. When pregnant women live in contexts that place them at a socio-economic disadvantage, support risk-taking behaviors, and normalize negative health outcomes, (ie, IPV) health consequences are compounded, each enhancing the next, thus amplifying the harmful effects for both the mother and, potentially, her unborn child.
Critical Intersecting Epidemics Among Pregnant Women
The Impact of Alcohol Use
With regards to world regions, we observe the overall highest rates of heavy episodic alcohol consumption among men and women living in sub-Saharan Africa [10]. Although Africa has a per capita consumption rate consistent with world averages, men and women in this region report high rates of abstaining from alcohol use, therefore, alcohol consumption among those who do drink is alarmingly high [11]. Similarly, the proportion of South Africans who drink alcohol is fairly low (in a national household survey just 39% of men and 16% of women reported alcohol use in the past year), however, South Africa has one of the highest per-capita rates of alcohol consumption in the world among those who do consume alcohol [12, 13••]. Heavy alcohol use in informal drinking establishments or shebeens (informal drinking venues) and taverns within many townships in South Africa occurs frequently [14–20]. Furthermore, South Africa has high rates of hazardous drinking and patterns of detrimental alcohol use tend to be more severe in South Africa [21–23], compared with other parts of the world [12].
It is widely believed that heavy drinking among poorer South Africans, particularly Coloureds (see belowFootnote 1), is deeply-rooted in the legacy of the ‘dop’ system. The dop system, named after the colloquial Afrikaans word which means an alcoholic drink, has a long history dating back to European colonialism. In the Western Cape province (where some of the highest rates of FAS have been recorded worldwide), the agricultural economy centered on grape and wine production. Within this system, the payment of farm workers in part with crude wine considered unfit to drink was established [24]. This system allowed farmers to get rid of surplus wine, and kept workers dependent and loyal due to their alcoholism. The dop system played an important role in farm workers’ dependency on alcohol and in the social control exercised over the indigenous people of the Cape region. Indigenous people were enticed to work on farms with the promise of payment in the form of tobacco, bread, and wine [25]. Under this system, farm workers were well controlled [26], but the shackles of their addiction had far reaching effects. In particular, since women did not refrain from alcohol use during pregnancy, the greatest impact has been on mothers and the children born to them [24].
The dop system was officially banned in 1960 but continued under apartheid; the ban was only enforced in the 1990s following South Africa’s democracy. Despite this change, there have been claims since then that the dop system is still active. However, in 2007 The Black Association of the Wine and Spirits Industry (BAWSI) called for the establishment of an industry fund to change people’s attitudes about drinking alcohol and to set up institutions to treat alcoholism. This effort led to judicial action in order to fight against the agricultural industry and, ultimately, to encourage government to address the outcomes of the dop system [27]. Some argue that farmers are still practicing the dop system today but the pattern of remuneration by means of cheap wine is cloaked under the pretence of farmers providing workers with a ‘gift’. The amendment of the 1928 liquor act in 1961 did not address the provision of free wine as a gift to farm workers, which left a loophole through which the practice continues [25].
Perhaps more devastating than the possibility of the currently functioning dop system practiced by farmers have been the claims that farm workers across the Western Cape have created their own dop system since the official system was outlawed [28]. In a newspaper article published in 2012, Prof Viljoen (founder of the Foundation for Alcohol Related Research, FARR), was quoted as stating that the dop system has been replaced by shebeens and on farms far from shebeens or from the bottle stores (spirit shops) found in townships, there now exist mobile shebeens. Trucks (locally called bakkies) stocked with alcohol travel to farms and communities to sell alcohol and will even sell alcohol on credit [29]. A cycle of drinking and paying off drinking debt persists to the extent that farm workers themselves have expressed concerns about the operation of mobile shebeens [30]. Therefore, despite the abolishment of the dop system, dependence on alcohol continues to play a role in enmeshing farm workers in a cycle of poverty and dependence [25] and beyond the rural areas in the townships of urban areas, regular, and heavy alcohol consumption persists.
During apartheid, illegal shebeens in black and coloured townships played an important role in the lives of the oppressed [26]; today, shebeens continue to thrive in impoverished environments. The legacy of excessive drinking continues to afflict these communities, causing widespread social damage and can only be addressed by changing the pattern of drinking in South Africa -- a shift which has been argued as essential if the alcohol-related burden is to be reduced [26].
The Impact of Interpersonal Violence (IPV)
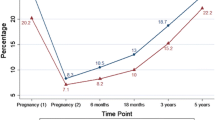
Women of childbearing age (15–49 years of age) are at the greatest risk of experiencing IPV across the lifespan [31]. The World Health Organization’s [32] multi-country study of Women’s Health and Domestic Violence found prevalence rates for IPV as high as 28%; it is noteworthy that among the 10 countries included in the survey, the 2 African countries (Namibia and the United Republic of Tanzania) hold the highest rates of IPV. This international study also reports that women who experience IPV are more likely to categorize their health as poor or very poor compared with women who have not experienced IPV. The negative outcomes of IPV during pregnancy pose particular risks to mother and child including increased risk of sexually transmitted infections/HIV, miscarriage, preterm labor, induced abortions, pregnancy complications, hypertension, delivering at a low birth weight, physical injuries, stress, and, in extreme cases, is associated with maternal death (see Fig. 1) [33–35].
Worldwide, rates of IPV are highest within impoverished communities and women with less education and fewer financial resources are at an increased risk for victimization. Efforts to improve employment and education rates can be obstructed by IPV, as assault and the fear of violence contribute to reduced school enrollment for girls [36]. Gender inequalities like these are common in many African cultures, which tend to organize social power around patriarchal systems, and underpin generational cycles of IPV [37••]. Substance use -- and alcohol use in particular -- is also highly correlated with IPV [38]. Cultural attitudes that condone violence against women, in combination with attitudes that minimize the risks of the consumption of drugs and alcohol, create a context wherein violence against women is normalized, resulting in exceptionally high rates of IPV. Remarkably, estimates of IPV during pregnancy among women in Africa range from 23%–49% and these rates have been identified as among the highest reported globally. Major risk factors for IPV among African pregnant women include being HIV infected, and having a history of violence, and alcohol and drug use [39••]. This high prevalence rate may be unique to pregnancy because expecting a child is likely to put increased demands on limited family resources and on relationship dynamics as individuals adjust during the transition to parenthood [40]. In South Africa, violence is the second leading cause of premature death and homicide accounts for more than half of all fatal injuries among 15–34 year-olds [41].
South Africa’s epidemic of community and personal level violence is fueled, in part, by alcohol use and attitudes condoning violence against women. More than half of female homicide victims are killed by their relationship partners, and both perpetrators and victims of violence often have high blood alcohol content [42]. Reviews across results from over 80 IPV studies have identified alcohol use as a significant predictor of violence perpetration -- in particular, that there is a significant and large correlation between attitudes condoning violence and violence perpetration [43]. In South Africa, IPV history has been linked to an increased chance of problematic alcohol use for men and women [37••], and drinking has been associated with greater odds of men perpetrating IPV and sexual assault [31, 43]. These results combined suggest the relationship is cyclic; IPV histories increase alcohol use, and alcohol consumption contributes to IPV -- this relationship most likely occurs through the process of lowering inhibitions, and increasing impulsive and risk-taking behavior. Indeed, research suggests that IPV victimization and perpetration are both better predicted by past IPV trauma histories than by substance use histories or any demographic variable [37••, 44]. “In South Africa, exposure to violence in childhood is as ubiquitous as it is in adulthood” [37••] and, overall, reports of IPV demonstrate its remarkably high prevalence in South Africa: between 25% and 42% of study respondents report currently being in a violent partnership [45–48].
The Impact of HIV Transmission
The burden of HIV infection disproportionately affects women in Africa; it is estimated that 60% of the individuals who are living with HIV in Africa are girls and women. Furthermore, in sub-Saharan Africa young women are 8 times more likely to be HIV infected than men. In all of sub-Saharan Africa, 40% of women living with HIV reside in South Africa [49, 50]. Efforts to prevent maternal-to-child transmission have expanded globally with an estimated 53% of HIV positive pregnant women receiving PMTCT (preventing mother to child transmission) treatment. However, only 15% of HIV positive pregnant women accessing maternal health clinics are receiving antiretroviral therapy for their own health [49, 50].
The limited care available for many HIV positive pregnant women in sub-Saharan Africa is consistent with the lack of services accessible for these same women who are using and abusing substances. Although options for HIV positive pregnant women who abuse substances are limited, it is well known that substance use during pregnancy is a major concern in multiple sub-Saharan countries [51]. Recently, work completed by Chersich et al. [52] has outlined the intricate relationships between alcohol use, HIV transmission, and unintended pregnancies. Cherisch focuses on the detrimental influence of alcohol in the role of secondary HIV transmission and unintended pregnancies, arguing for a focus on the broader context these behaviors occur in. Similarly, Rotheram-Borus [53••] has developed a community-level, behavioral intervention around addressing the role of HIV infection, alcohol use, and pregnancy in the Cape Town, South Africa area. This work has paved the way for defining approaches to delivering intervention content relating to complex risk and is delivered by lay health care workers residing within the community where they are working.
Recent studies focusing specifically on the use of alcohol among HIV positive pregnant women are limited in sub-Saharan Africa. However, available research suggests that the role of alcohol likely varies considerably across cultures, with studies from South Africa [54] and Nigeria [55] highlighting the different influences of alcohol among HIV positive pregnant women. Desmong et al. [54] notes that alcohol use among HIV positive South African pregnant women varies greatly, with those residing in the KwaZulu-Natal area reporting relatively lower of rates of alcohol use than other areas, yet women who do consume alcohol report high rates of alcohol consumption. However, Etukumana et al. [55] notes a lack of association between testing HIV positive and alcohol abuse. Overall, the impact of HIV on South African communities continues to bolster the presence of a syndemic among pregnant women in South Africa. Without considerable advances in access to HIV prevention education and tools, and without improved options for HIV treatment, the presence of a syndemic is likely to remain a key factor influencing the overall health outcomes of pregnant women.
Synergistic Co-occurrence
Taken independently, each of the epidemics of alcohol use, IPV and HIV transmission are a noteworthy and formidable threat to the health of pregnant women. When public efforts broaden to a global view (see Fig. 1), it is clear that threats to maternal and child wellbeing are synergistic. Their combination results in an alarming set of circumstances for South African women in particular. As depicted in Fig. 1, HIV prevalence rates are greatest in Africa, with Southern Africa experiencing the highest prevalence of HIV infection compared with any other region of the world. Likewise, maternal mortality ratios are the highest in Africa, with central Africa being most affected. Furthermore, heavy episodic alcohol consumption among women is greatest in Southern Africa, including South Africa. On the whole, as is evidenced by Fig. 1, South Africa represents the intersection of the highest rates of the aforementioned epidemics, a scenario characterized as a syndemic. By taking this broader view, prevention strategies can begin to address the bio-social context in which this syndemic is sustained.
Moreover, Fig. 1 depicts a public health scenario for Southern Africa that leaves little doubt that improvements in maternal child health are desperately needed. However, what we understand about the health of pregnant women in Southern Africa is also greatly limited. The information on maternal fatalities does not break down cause of death to distinguish between disease mechanisms and inflicted injuries (although greater than 50% of female homicide victims in South Africa are the result of IPV, as noted earlier), nor can we present reliable information on the rates of alcohol consumption among women who are pregnant specifically. Indeed, the lack of national-level data with much detail is an obstacle to forming timely, relevant, and effective intervention strategies. Remarkably, we were unable to identify any database containing FAS information: There appears to be no prevalence data on FAS for any of the 57 African countries. Sources have extrapolated estimates for FAS prevalence using North American incidence rates (ie, [56]), but these seem vastly under-informed given the clear differences in health and human service resources available on each continent. The limited data available exists within single or specific regions within single nations (ie, Cape Town Province of South Africa), and these numbers indicate on a national level the potential for each generation to be suffering disturbingly high FAS morbidity burdens [28]. In the absence of more detailed information, first steps towards improving maternal-child welfare outcomes must be informed by what is at hand. Thus, it is imperative that we prioritize improvements in the understanding of various maternal and child health outcomes, and that we make efforts to assess the prevalence of FAS in developing countries.
Prioritizing Goals for Future Prevention Efforts
Meeting the needs of HIV positive pregnant women is challenging in resource limited settings. However, there are potentially multiple entry points into care, or during ongoing care, where intervention around substance use and HIV transmission risk behaviors can be prioritized. For example, recent work by Peltzer [57], lays out the framework needed to address reasons that pregnant women do not receive HIV testing or HIV test results. Although, in this work, a majority of pregnant women received their results (81.2%), a significant minority did not, and, importantly, reasons for not receiving results may be addressable through counseling. Basic concerns around fear of learning one’s results and confidentiality were most commonly reported. In fact, in a meta-analysis of 5 recent studies [39••], IPV increased when a woman’s HIV status was positive; hence some of the reluctance to engage in testing may center around basic safety concerns. “We need to understand how HIV status operates in a culture where female subordination is the norm and how together with other factors it increases pregnant women’s risk for violence” [39••].
In our evaluation of available services for both HIV positive and negative pregnant women residing in informal settlements around the Cape Town, South Africa area, we suggest that relatively basic interventions could possibility have a profound effect on improved health outcomes. These interventions include: transportation to substance use treatment centers, social support groups for people actively engaging in substance abuse, the addition of non-alcoholic beverages at shebeens and greater accessibility to pregnancy tests for early detection. Moreover, safe places for women and families to reside who are exposed to IPV could serve as important options for breaking the cycle of violence.
Conclusion
Development of community-based and therefore contextually-grounded interventions for vulnerable populations are desperately needed in Southern Africa. Ideally, these interventions should be informed by thorough needs assessments and through reliable estimates of the scope of risk behavior. This process will allow for targeting and addressing factors that support the HIV, alcohol use, and IPV syndemic (a syndemic that perhaps is most dire for mothers and their unborn children). While the most effective and enduring strategies will be those that challenge attitudes that condone violence against women, educate the community about the risks of substance use, particularly during pregnancy, and create an environment of support and treatment for HIV positive individuals, these cultural shifts will likely take decades. Positive steps to improve maternal-child health outcomes, however, can be taken in the immediate future. For example, efforts to estimate the scope of each epidemic can be extended beyond the few regions currently collecting incidence and prevalence data. Moreover, structural interventions that provide access to community-based support for both HIV treatment and substance use recovery -- both with an eye towards IPV screenings -- can serve as safe havens and provide much needed health education resources. Screening and brief interventions delivered in prenatal services may help improve access to substance use interventions for pregnant women, thus preventing FAS and other negative consequences of substance use during pregnancy.
Notes
The terms “white,” “black,” and “coloured” in South Africa, refer to demographic markers and do not signify inherent characteristics. They refer to people of European, African and mixed (African, European and/or Asian) ancestry, respectively. The continued use of these markers in South Africa is important for monitoring improvements in health and socio-economic disparities, identifying vulnerable sections of the population, and planning effective prevention and intervention programs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Joyner K, Mash R. Recognizing intimate partner violence in primary care: Western Cape, South Africa. PLoS One. 2012;7:e29540. Provides information on incidence and measurement of IPV in community settings.
Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food insecurity, depression, and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74:2012–9.
Wong FY, Huang ZJ, DiGangi JA. Gender differences in intimate partner violence on substance abuse, sexual risks, and depression among a sample of South Africans in Cape Town, South Africa. AIDS Educ Prev. 2008;20:56–64.
Alio AP, Clayton HB, Garba M. Spousal concordance in attitudes toward violence and reported physical abuse in African couples. J Interpers Violence. 2011;26:2790–810.
Laisser RM, Nyström L, Lugina HI. Community perceptions of intimate partner violence–a qualitative study from urban Tanzania. BMC Women’s Health. 2011;18:11–3.
Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol. 1996;24:99–110.
Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17:423–41.
Millstein B. Introduction to the syndemics prevention network. Atlanta: Centers for Disease Control; 2001.
Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Women’s Health. 2011;20:991–1006. Includes information on the study of syndemics and of the SAVA syndemic in particular. Measurement of IPV in community settings.
WHO. Global status report on alcohol and health; 2011.
Hahn JA, Woolf-King SE, Muyindike W. Adding fuel to the fire: alcohol’s effect on the HIV epidemic in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2011;8:172–80.
Rehm J, Rehn N, Room R, Monteiro M, Gmel G, Jernigan D, et al. The global distribution of average volume of alcohol consumption and patterns of drinking. Eur Addict Res. 2003;9:147–56.
Parry CD. Alcohol policy in South Africa: a review of policy development processes between 1994 and 2009. Addiction. 2010;105:1340–5. Includes information on the study of syndemics and of the SAVA syndemic in particular. Measurement of IPV in community settings.
Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci. 2008;9:55–62.
Suliman S, Seedat S, Williams DR, Stein DJ. Predictors of transitions across stages of alcohol use and alcohol-use disorders in South Africa. J Stud Alcohol Drugs. 2010;71:695–703.
Schneider M, Norman R, Parry C, Bradshaw D, Plüddemann A, the South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. S Afr Med J. 2007;97:664–72.
Kalichman SC, Simbayi L, Jooste S, Cain D, Vermaak R. Sensation seeking and alcohol use predict HIV transmission risks: prospective study of sexually transmitted infection clinic patients, Cape Town, South Africa. Addict Behav. 2008;33:1630–3.
Kalichman SC, Simbayi LC, Vermaak R, Cain D, Smith G, Mthebu J, et al. Randomized trial of a community-based alcohol-related HIV risk-reduction intervention for men and women in Cape Town South Africa. Ann Behav Med. 2008;36:270–9.
Kalichman SC, Simbayi LC, Cain D, Jooste S. Alcohol expectancies and risky drinking among men and women at high-risk for HIV infection in Cape Town South Africa. Addict Behav. 2007;32:2304–10.
Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in Cape Town, South Africa. Am J Drug Alcohol Abuse. 2007;33:687–98.
Rehm J, Sempos CT, Trevisan M. Alcohol and cardiovascular disease–more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease–a review. J Cardiovasc Risk. 2003;10:15–20.
Gruenewald PJ, Russell M, Light J, Lipton R, Searles J, Johnson F, et al. One drink to a lifetime of drinking: temporal structures of drinking patterns. Alcohol Clin Exp Res. 2002;26:916–25.
Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–28.
McKinstry J. Using the past to step forward: fetal alcohol syndrome in the Western Cape province of South Africa. Am J Public Health. 2005;95:1097–9.
London L. The ‘dop’ system, alcohol abuse and social control amongst farm workers in South Africa: a public health challenge. Soc Sci Med. 1999;48:1407–14.
Schneider M, Norman R, Parry CDL, Bradshaw D, Plüddemann A. Estimating the burden of alcohol abuse in South Africa in 2000. Methodological note. Cape Town: S Afr Med Res. 2007;97:664–72.
Johns, L. “Taking Western Cape’s deadly dop system to court”. IOL News. 2007. Available at: http://www.iol.co.za/news/south-africa/taking-w-cape-s-deadly-dop-system-to-court-1.362932. Accessed 15 September 2012.
Crafford, A. “Abused from the womb”. Mail & Guardian online. 2009. Available at: http://mg.co.za/print/2009-06-26-abused-from-the-womb. Accessed 15 September 2012.
Stassen, W. “How De Aar is beating curse of alcohol”. Sunday Independent. 2012. Available at: http://www.iol.co.za/sundayindependent/how-de-aar-is-beating-curse-of-alcohol-1.1347367. Accessed 15 September 2012.
Koyana, X. “Bitter legacy of dop system stalks farms”. Cape Times. 2011 Available at: http://www.iol.co.za/capetimes/bitter-legacy-of-dop-system-stalks-farms-1.1138132. Accessed 15 September 2012.
Taillieu TL, Brownridge DA. Violence against pregnant women: prevalence, patterns, risk factors, theories, and directions for future research. Aggress Violent Behav. 2010;15:14–35.
WHO. WHO Multi-country study on women’s health and domestic violence against women: initial results on prevalence, health outcomes, and women’s responses. 2005.
WHO. Heavy episodic drinkers among drinkers, females, 2004. 2011. Available at: http://gamapserver.who.int/mapLibrary/Files/Maps/Global_episodic_drinkers_2004_females.png. Accessed 15 September 2012.
WHO. Maternal mortality ratio (per 100 000 live births), 2010. 2012. Available at: http://gamapserver.who.int/mapLibrary/app/searchResults.aspx. Accessed 15 September 2012.
WHO. A global view of HIV infection 39.5 million people living with HIV in 2006. 2007. Available at: http://gamapserver.who.int/mapLibrary/Files/Maps/HIVPrevalenceGlobal2006.png. Accessed 15 September 2012.
Garcia-Moreno C, Watts C. Violence against women: an urgent public health priority. Bull World Health Organ. 2011;89:2.
Gass JD, Stein DJ, Williams DR, Seedet S. Gender differences in risk for intimate partner violence among South African adults. J Interpersonal Violence. 2011;26:2764–89. This study has information on the gender-based experience of IPV in South Africa, including the role of alcohol consumption in IPV incidence.
Chersich MF, Rees HV. Causal links between binge drinking patterns, unsafe sex, and HIV in South Africa: It’s time to intervene. Int J STD AIDS. 2010;21:2–7.
Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One. 2011;6:e17591. Includes information on the IPV experiences of pregnant African women in a review of the literature.
WHO. Intimate partner violence during pregnancy. 2011.
Doolan K, Ehrlich R, Myer L. Experience of violence and socioeconomic position in South Africa: a national study. PLoS One. 2007;2:e1290.
Seedat M, Van Niekerk A, Jewks R, Suffla S, Ratele K. Violence and injuries in South Africa: prioritizing an agenda for prevention. Lancet. 2009;374:1011–22.
Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. J Stud Alcohol. 2004;65:434–42.
Gil-Gonzalez D, Vives-Cases C, Ruiz MT, Carrasco-Portino M, Alverez-Dardet C. Childhood experiences of violence in perpetrators as a risk factor of intimate partner violence: a systematic review. J Public Health. 2007;30:14–22.
Eaton LA, Kalichman SC, Sikkema KJ, Skinner D, Watt MH, Pieterse D. Pregnancy, alcohol intake, and intimate partner violence among men and women attending drinking establishments in a Cape Town, South Africa township. J Community Health. 2012;37:208–16.
Townsend L, Jewkes R, Matthews C, Johnston LG, Flisher AJ, Zembe Y, et al. HIV risk behaviors and their relationship to intimate partner violence (IPV) among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Behav. 2011;15:132–41.
Abrahams N, Jewkes R, Laubscher R, Hoffman M. Intimate partner violence: prevalence and risk factors for men in Cape Town, South Africa. Violence Vict. 2006;21:247–64.
Dunkle KL, Jewkes RK, Nduna M, Levin J, Jama N, Khuzwayo N, et al. Perpetration of partner violence and HIV risk behavior among young men in the rural Eastern Cape, South Africa. AIDS. 2006;20:2107–14.
UNAIDS. AIDS at 30: Nations on the crossroads. 2011.
UNAIDS. Report on the Global AIDS Epidemic. 2010.
Rosenthal J, Christianson A, Cordero J. Fetal alcohol syndrome prevention in South Africa and other low-resource countries. Am J Public Health. 2005;95:1099–101.
Chersich MF, Rees HV, Scorgie F, Martin G. Enhancing global control of alcohol to reduce unsafe sex and HIV in sub-Saharan Africa. Glob Heal. 2009;5:16.
Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, et al. Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants’ outcomes. Prev Sci. 2011;12:372–88. Article with information on prevention strategies for pregnant women.
Desmond K, Milburn N, Richter L, Tomlinson M, Greco E, van Heerden A, et al. Alcohol consumption among HIV-positive pregnant women in KwaZulu-Natal, South Africa: prevalence and correlates. Drug Alcohol Depend. 2012;120:113–8.
Etukumana EA, Thacher TD, Sagay AS. HIV risk factors among pregnant women in a rural Nigerian hospital. West Indian Med J. 2010;59:424–8.
Right Diagnosis. Statistics by Country for Fetal alcohol syndrome. 2012. Available at: http://www.rightdiagnosis.com/f/fetal_alcohol_syndrome/stats-country.htm. Accessed 15 September 2012.
Peltzer K, Mlambo G, Phaweni K. Factors determining prenatal HIV testing for prevention of mother to child transmission of HIV in Mpumalanga, South Africa. AIDS Behav. 2010;14:1115–23.
Acknowledgement
This project was supported in part by National Institute of Mental Health grant R01 MH094230.
Disclosure
B.S. Russell: none; L.A. Eaton: grant from National Institutes of Health (NIH).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Russell, B.S., Eaton, L.A. & Petersen-Williams, P. Intersecting Epidemics Among Pregnant Women: Alcohol Use, Interpersonal Violence, and HIV Infection in South Africa. Curr HIV/AIDS Rep 10, 103–110 (2013). https://doi.org/10.1007/s11904-012-0145-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-012-0145-5